Abstract
BACKGROUND
Telehealth technologies are increasing health care access for patients in the home, community, and rural and underserved areas. Older adults may be challenged to use new technologies due to aging related changes, lack of experience, and different attitudes toward its use. This pilot study evaluated potential issues in training/instructions and use of a telemonitoring application. The feedback from this study will be used to adapt the application and training to support dementia caregivers.
METHODS
Seven cognitively intact older adults attended a one-on-one training session for using a telemonitoring application on an iPad Mini or iPod Touch device. They returned one week after training to demonstrate actual use of the telemonitoring application. The demonstration session was video-recorded. Behavioral coding of the videos was used to determine which steps were problematic, and to identify modifications needed in the application and training. Use of telemonitoring application involved ten steps: turn on device, get to the App screen, open the App, position/reposition the device to record, change front-back camera setting, record, view recording, upload, delete, and return to start screen. The following challenges (errors) were coded; ask question, refer to manual, pause, ineffective tap, express frustration, cueing by the research assistant, and mistake. Participants also completed an ease of use questionnaire.
ANALYSIS
Descriptive analysis of the video recordings and the questionnaire identified usability challenges.
RESULTS
The actual use return demonstration session took an average of 50 minutes. All participants referred to the instruction manual. Participants varied in the number of challenges to completing the task but had an average of 19 coded errors or challenges to complete the process. This information was used to revise training materials and to work with the developer to improve the application.
CONCLUSIONS
Older adults may benefit from specific adaptations and training to use new health care technologies. Behavioral coding is an effective way to evaluate the user interface for new technologies with older adults.
Keywords: Telehealth, technology, older adults
New developments in health care and advances in technology are creating new telemedicine opportunities for enhanced care that can be delivered to patients in home and community settings, increasing access to care for persons of all ages. Telemedicine and e-health services are promising care delivery modes and interventional modalities designed to meet the needs of a variety of patient populations. Technology can extend the reach of expert practitioners to patients and families in the community and the home and in rural and isolated populations. Though there are barriers to address (Bossen, Kim, Williams, Steinhoff, & Strieker, 2015; Wu, Damnee, Kerherve, Ware, & Rigaud, 2015), virtual care in the community delivered via technology-based approaches is able to overcome the limitations of face-to-face delivery, namely time constraints, geographic limitations, and transportation issues (Lewis, Hobday, & Hepburn, 2010; White & Dorman, 2001). With the advent of the Affordable Care Act, industry projections include an increase in the use of telehealth technology in the United States by 500% by 2017 (Roashan, 2014).
New telehealth technologies that were initially developed for use in younger populations are now available for adaptation to help older persons. One such project is adapting a telemonitoring system originally designed to assist parents and teachers of children with autism, to the growing population of persons with Alzheimer’s disease and other dementias. The Behavior Imaging Solutions © developed Behavior Capture (a secure application to collect and upload video recordings) and Behavior Connect (a secure cloud-based site where practitioners can access and review submitted videos to provide feedback). This telemonitoring application works by capturing video recordings of challenging situations and behaviors that the caregiver and patient are involved in and caregiver’s strategies to manage them, with a buffer that captures footage prior to the trigger for recording. Videos of behavior situations are then uploaded for clinical expert review, and feedback and training in behavior management is provided to caregiver participants. Because we planned to use this technology to assist caregivers of older adults with dementia, we identified that a large proportion of the target caregivers would be adults and older adults (spouses and adult children) who may face barriers to adopting this technology. Thus, we designed a pilot study to inform our project.
Background
Telehealth is one of a number of available technologies to assist older adults, including those with Alzheimer’s disease and other dementias to remain living in the community (Bossen et al., 2015; Godwin, Mills, Anderson, & Kunik, 2013). New technology is meeting the needs of persons with early stage dementia through memory aides, cognitive stimulation, wayfinding, and information resources on the internet. Family members who care for persons with dementia living in the community are also supported by new technology. This provides a valuable resource as the number of persons experiencing dementia is projected to increase to 16 million by 2050, while the number of available caregivers for those afflicted will decline (Alzheimer's Association, 2014). Support for family caregivers, who experience a number of negative physical and psychological effects from the stress and burden of caregiving, has now been identified as a growing public health crisis (Talley & Crews, 2007). Technology currently supports family caregivers of persons with dementia through information and support resources available online, monitoring of movement, vital signs, and ambient and environmental conditions, tracking systems, and telemedicine and ehealth services (Bossen et al., 2015; Godwin et al., 2013).
Technology is growing in use by middle-aged and older adults. Over 50% of adults 65 and over use computers and other electronic devices daily to access the Internet for medical information and social support (Fox & Brenner, 2012). Surveys of family caregivers reveal that 80% to 95% request mobile systems and find that interactive features assist in caregiving. 66% of technology–using family caregivers in the US use a mobile wireless device and 69% of those find them helpful for caregiving. Mobile technology features such as mobile text messaging, personal medical recording, and visual communication with healthcare providers meet specific user needs (Fox & Brenner, 2012; National Alliance for Caregiving, 2011). Despite these estimates and growing recognition of the potential benefits to older adults from internet technologies that support their personal fulfillment, health preservation, social connectedness, functional capability and activity, and caregiver support (Baker, 2013) there is still concern about the abilities and attitudes of older adults in adopting new technology (D'Ambrosio & Mehler, 2014; Chaiwoo Lee, 2014).
Barriers limiting technology use by older adults caring for someone with dementia include (1) ethical considerations, (2) user perspectives and attitudes toward technology, (3) access to and reimbursement for technology, and (4) privacy. Privacy is a major concern, because video and audio sensitive care situations are utilized, with a risk of exposing sensitive, personally identifiable data. Although technology is intended to support independent living, unnecessary and too frequent use of technologies can diminish independence of choice and actions. Instead of being helpful, extremely advanced technology beyond of user’s capacity can become frustrating and dehumanizing (van Hoof, Kort, Rutten, & Duijnstee, 2011; Zwijsen, Niemeijer, & Hertogh, 2011).
There is also concern that technology use may replace human contact and lead to isolation. Health care providers need to acknowledge these cohort concerns with technology and assure human as well as technology contact. Families living in rural areas or with low incomes may have limited Internet access. Although, the number of persons 65 and older with high-speed Internet connections has increased to 39% today from 19% in 2008, there is still far to go to achieve universal access (Baker & Seegert, 2013). Insurance coverage for new technology to support dementia care is also lagging. Consumers must be able to afford these services as many emerging technologies are not covered by personal health insurance, Medicare, or Medicaid (Lee, 2013).
A critical factor in the acceptance of technology is ease of use (Kramer, 2013). This is especially pertinent for dementia caregivers who experience daily stress and burden from their role, are themselves experiencing cognitive and physical changes of aging, and may have limited experience and different attitudes toward technology. Normal aging changes including reduced processing speed, less manual dexterity, and low visual acuity may add to the challenge of learning and using new technologies. A pilot study was developed to evaluate the ability of older adults to utilize the new telemonitoring technology to be used in our larger research study and to evaluate our training materials and instructions. While longitudinal designs and comparison to younger adults would be helpful in our understanding of potential aging and cohort effects, this focus of this study was limited to evaluating one specific user-technology interface for older adults.
Pilot Study
A pilot study was completed in June 2014 to evaluate how difficult it would be for older adults (dementia caregives) to use a telemonitoring app, originally designed for parents of children with autism. We recruited and consented 7 volunteers from the local senior center, as approved by our University Institutional Review Board for Protection of Human Subjects. They ranged in age from 70–86. Five were male. All had at least a college degree and worked prior to retirement in teaching, medicine, and as college faculty. All had some familiarity with computers and used email at least daily. All participants used cell phones. No evaluation of cognitive status was done, though all were able to read and understand the consent forms.
Participants were trained in a one-hour session either in a private room in the Senior Center or in their home to use the Behavior Capture Application. Participants could choose which device to use; the iPod Touch that is the size of a cell phone or the iPad Mini that is a small tablet. During the session, a research assistant trained the older adult to use the telemonitoring application to complete a video capture and upload sequence. Our research team used an illustrated instruction manual that we developed to provide step by step instructions. The upload settings were preset and additional device settings were used to simplify the process (i.e. large font, assistive touch, App icon on a separate screen).
On the return visit, the older adult was asked to demonstrate actual use of the device to capture, upload, and delete videos with access to the instruction manual. This visit was video recorded. At the end of each visit, the participants completed the System Usability Scale (Bangor, Kortum, & Miller, 2009) to evaluate their perceived ease of use of the technology. Participants each received a $20 gift card at the end of each session.
Videos recording the return visits were behaviorally coded, using the Noldus Observer program (Noldus Information Technologies Inc., Leesburg, Virginia, 2003), to determine the biggest challenges. Behavioral coding can be readily adapted to identify specific behaviors and temporal relationships between behaviors in live and video recorded observations. We adapted several coding protocols used in our prior research (Williams, 2011; Williams, Herman, Gajewski, & Wilson, 2009).
Based on initial review of two videos, we divided the process involved in using the application into ten steps: Turn on Device, Get to the App screen, Open the App, Position/reposition the device to record, Change front-back camera setting, Record, View recording, Upload, Delete, and Return to start screen. Based on the initial coding of two videos, we identified the following behavioral events that indicated challenges (errors) in performance: Ask question, Refer to manual, Pause, Ineffective tap, Express frustration, Cueing by the research assistant, and Mistake. Definitions of the error terms are provided in Table 1. Two videos were coded by two individual coders, compared, and discussed, until coding agreement reached 90%.
Table 1.
Definitions of Error Codes
| Error Term | Definition |
|---|---|
| Ask Question | Participant had to ask a question to complete the step. |
| Refer to Manual | Participant was unable to proceed with a step without looking at the illustrated instruction manual. |
| Pause | Participant stopped during the demonstration for at least 15 seconds. |
| Ineffective Tap | Participant failed to trigger an icon to initiate actions (such as opening the app). May have been to brief or prolonged of a touch. |
| Express Frustration | Participant vocally expressed that they were challenged. |
| Cueing by the Research Assistant | Participant requested direction from the research assistant. |
| Mistake | Participant pressed a wrong icon or navigated to an incorrect screen. |
Results
All participants completed both the initial and return visits as part of the study. All of the participants elected to use the larger iPad Mini, reportedly due to its greater ease in visualizing and manipulating the device.
Survey results
Mean scores for the usability survey rating ease of use are provided in Table 2. In general, participants found the system easy to use and expressed confidence in their ability to learn the system. Most scores were at the top or bottom of the possible range, with the exception of item 7, “I would imagine that most people would learn to use this system very quickly” (mean scores were midrange).
Table 2.
System Usability Scale Results (based on a Likert scale with 1 = strongly disagree to 5 = strongly agree).
| First Visit | Return Visit | |
|---|---|---|
| 1. I think that I would like to use this system frequently |
4.29 | 4.29 |
| 2. I found the system unnecessarily Complex |
1.57 | 1.71 |
| 3. I thought the system was easy to use |
4.43 | 4.71 |
| 4. I think that I would need the support of a technical person to be able to use this system |
1.43 | 1.71 |
| 5. I found the various functions in this system were well integrated |
4.71 | 4.71 |
| 6. I thought there was too much inconsistency in this system |
1.43 | 1.14 |
| 7. I would imagine that most people would learn to use this system very quickly |
3.29 | 3.71 |
| 8. I found the system very cumbersome to use |
1.29 | 1.14 |
| 9. I felt very confident using the | 3.43 | 4.43 |
| 10. I needed to learn a lot of things before I could get going with this system |
2.0 | 1.29 |
Return Demonstration
The total return demonstration procedure took an average of 50 minutes. All participants reviewed the instruction manual for directions. Table 3 shows the average and range of times to complete each of the ten procedural steps and the total number of errors that occurred for each of the 7 participants (one was a husband-wife pair who worked together). For example, in step one, turning on the device, participant 2 had no errors, while participant 5 had 6 errors. The final column in Table 3 shows the average number of challenges across participants in each of the steps. Participants varied in the number of challenges to completing the task but all had at least 6 and an average of 19 coded challenges to complete a recording/upload/delete process. The most frequent errors occurred during turning on the device (M = 3.67) and in the uploading step (M = 3.17). The most common type of error was pausing during uploading, or requiring a cue to delete the video. There was variability in the number and type of mistakes by participants for each step in the process. The number of specific mistakes by each step is documented for the total population in Table 4. The uploading step, followed by the delete step had the most errors.
Table 3.
Time (in seconds) to Complete and Errors for Each Step of Return Demonstration
| STEPS | Mean Time |
Min Time |
Max Time |
Errors Subject 1 |
Errors Subject 2 |
Errors Subject 3 |
Errors Subject 4 |
Errors Subject 5 |
Errors Subject 6 |
Mean Errors |
|---|---|---|---|---|---|---|---|---|---|---|
| Turn On Device |
51.74 | 20.89 | 132.16 | 3 | 0 | 8 | 3 | 6 | 2 | 3.67 |
| Get to App Screen |
47.17 | 2.94 | 103.57 | 0 | 4 | 5 | 3 | 1 | 0 | 2.17 |
| Open App | 28.34 | 2.37 | 97.76 | 0 | 4 | 0 | 11 | 1 | 0 | 2.67 |
| Position/ reposition |
41.21 | 4 | 98.63 | 0 | 0 | 1 | 1 | 3 | 1.00 | |
| Front-Back camera |
16.33 | 8.61 | 24.06 | 1 | 0 | 0.50 | ||||
| Record | 49.11 | 15.45 | 124.42 | 0 | 0 | 1 | 4 | 2 | 3 | 1.67 |
| View Recording |
44.89 | 12.98 | 110.98 | 0 | 1 | 7 | 0 | 2.00 | ||
| Upload | 101.09 | 17.45 | 392.05 | 1 | 0 | 5 | 1 | 0 | 12 | 3.17 |
| Delete | 57.06 | 27.76 | 118.75 | 2 | 7 | 3 | 1 | 1 | 1 | 2.50 |
| Set New Recording |
54.24 | 8.04 | 141.71 | 0 | 0 | 2 | 2 | 1.00 | ||
| Totals | 6 | 16 | 22 | 34 | 12 | 23 | 19 |
Table 4.
Mistakes During Steps of the Procedure (totals for all participants)
| RECORD | VIEW | UPLOAD | DELETE | START OVER |
|
|---|---|---|---|---|---|
| Refer to Manual | 2 | 3 | 3 | 0 | 1 |
| Ask Question | 3 | 1 | 3 | 0 | 1 |
| Cueing | 1 | 1 | 4 | 5 | 1 |
| Mistake | 0 | 0 | 0 | 4 | 0 |
| Frustration | 3 | 3 | 4 | 1 | 2 |
| Ineffective Tap | 1 | 1 | 0 | 0 | 0 |
| Pause | 0 | 0 | 5 | 2 | 0 |
| Total | 10 | 9 | 19 | 12 | 5 |
Suggested Modifications/Implications
In collaboration with our research team, which includes a human factors engineer, we reviewed our results and developed modifications for our training protocols and reference manual as well as for the application developer. We determined that the iPad Mini should be used due to the larger screen and button size that was easier for participants to see and manipulate. Suggestions were made for identifying recorded videos by date and time, reducing the need for users to change between screens during various steps in the process (reviewing, uploading, and deleting videos), to reduce the number of steps for deleting videos, and to improve the labeling to be larger and more distinct.
There were edits and additions that needed to be made to the instruction manual for clarity (i.e. font size, labeling steps, including a problem solving page). For example, to simplify the process, the instructions were modified to leave the device on (and periodically plugged in for charging) and set to record (this eliminates the first 3 steps although if the app is closed, these first steps will need to be completed).
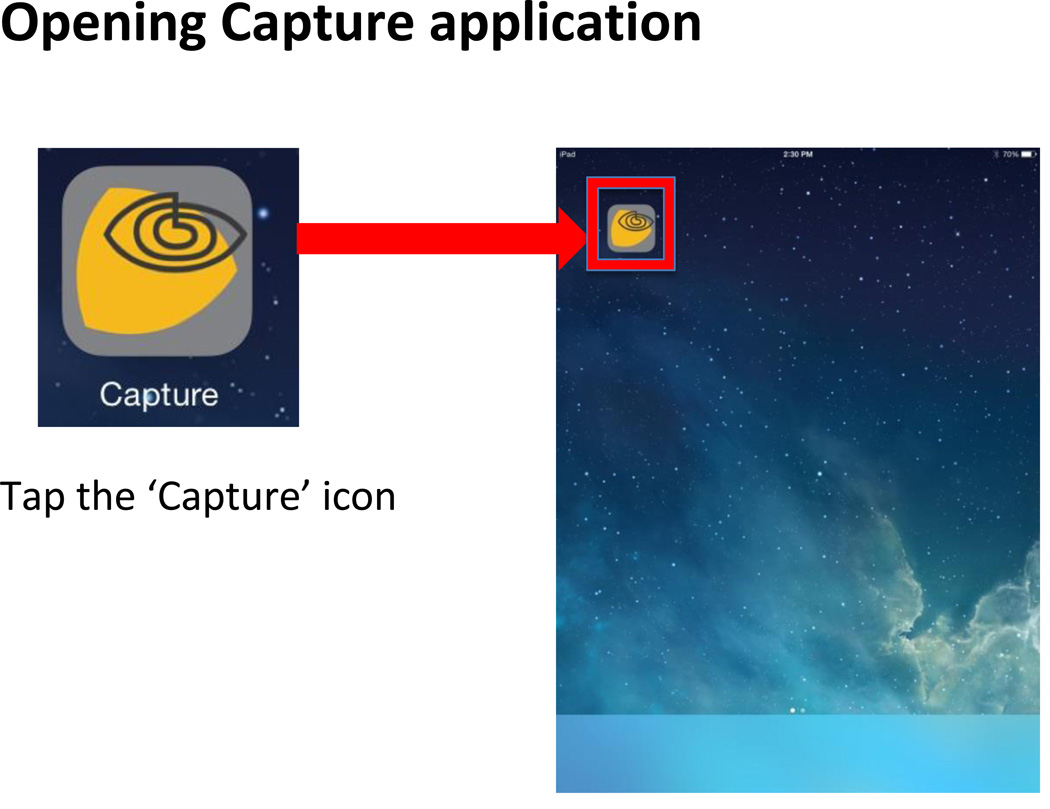
Following the pilot, the step by step instruction manual was modified to include larger text with clearly labeled screen shots with directions for performing steps, with breakdown of each step into small parts. An example of a page from the manual is provided in Figure 1.
Figure 1.
Sample Instruction
NOTE: You may need to press firmly on the icon, but do not hold.
Discussion
Survey results did not correspond to actual performance coded in the video recordings (the duration of the return demonstration and number of errors encountered). The older adults in our sample may have been overly confident or more tech-savvy than most other older adults. This may be due in part to the sampling for the study. All participants volunteered for the study and thus many who were less confident or had negative attitudes toward technology may have opted not to participate.
Responses to the useablity survey indicated that participants thought a human support person would be important if they were to use this technology routinely. This emphasizes the need for human support in using advancing technologies.
Modifications to improve user interface for older adults related to changes that occur in aging (cognitive and sensory) as well as cohort characteristics such as experience and attitudes toward technology. The instruction manual for using the system was simplified and training plan modified to accommodate the older adults. Additional application modifications will enhance the ability for older adults to use this technology.
Our modifications of the device settings and app to simplify the user interface may have helped the participants succeed in learning the technology, no matter what their background. They were open to participation without the tie to having a real use for the technology (in improving the care of a family member). Family members and caregivers may be more open to learning this technology (that we have simplified) given long term implications.
This study was limited by the size and characteristics of our sample. We utilized a convenience sample of highly educated older adults who were technology adopters. Thus, the results of our pilot study are not generalizable to all older adults. While longitudinal designs could have provided the opportunity to examine age-related changes over time, and comparison to a sample of younger persons would provide evidence of cohort effects, the focus of this pilot was limited to evaluating the user interface for our specific application and device. Expanded research such as studies comparing strategies for training adults both young and old (Hickman, Rogers, & Fisk, 2007) are important to inform the future preparation for the use of technology in across age groups.
The more devices are used and demonstrate that technology can improve older adults’ ability to live independently and not cause isolation or violation of privacy, greater acceptance and changes in attitudes toward technology use will improve. Additional functions for high tech devices (such as medication reminders) could also be programmed into the app. This would make the technology even more useful; however, complexity would also increase.
Conclusions
Older adults may not admit or realize challenges in learning to use new technology; the survey responses were very positive, compared to the length of time and number of errors encountered in our observation-based measurements. Despite the challenges encountered by our older adult participants, each was able (some with cueing) to complete the demonstration on the return visit. Although some expressed frustration, none abandoned the task. Although our participants were daily technology users, this suggests that with support, older adults have the motivation and ability to learn to use new technologies.
Behavioral coding is a strategy for identifying performance on technological steps and where challenges occur in adapting technology for use by older adults. Our results reinforced the importance of considering aging changes (normal as well as abnormal) that older adults may experience that challenge learning and using new technology (Czaja et al., 2006). Sensory changes, such reduced vision and reduced manual dexterity may present challenges to seeing and pressing touch screen areas as required by many apps. Adequate time must be allowed for training and ongoing support may be needed (many of our participants required cueing during the 1 week return demonstration visit). Training materials must be explicit, clear for those with reduced vision, and broken into minute steps.
Teams including clinicians and researchers are important to adapt technology for use by older adults. For example, the developer may do some data collection in the development of an application. However, researchers actually using the app in research and clinical settings face additional challenges. It is critical that developers and real world users establish a communication and feedback mechanisms to support good use of new technologies. In addition, having a human factors engineer as part of the research team is critical for facilitating these adaptations and should be considered as telehealth and other technologies are advanced.
Ongoing research is needed to evaluate how modifications such as these may improve ease of learning and using new technologies to extend health care to older adults. It is also important to include elders in the design of new products (Lee, 2013) as well as in adapting current products for use in this population. Acceptance of technology may also involve attitudinal change about technology as being a support for aging in place instead of a negative concept (D'Ambrosio & Mehler, 2014; Pew Research Center, 2014). These changes may take time and as cohorts mature, the evolving population of older adults may be enthusiastic about technology.
As health care transitions to include more virtual care, health care providers will need to be educated in how to most effectively intervene using technology, and how to balance the use of technology with human contact (Coughlin, 2014; Zwijsen et al., 2011). This will support ongoing acceptance and success with telehealth technology for older adults in home and community settings.
Contributor Information
Kristine Williams, Gerontological Nursing, University of Iowa College of Nursing, 446 CNB, 50 Newton Road, Iowa City, IA 52242, USA, kristine-n-williams@uiowa.edu, Telephone: (+1) 319-335-3103.
Priya Pennathur, Department of Mechanical and Industrial Engineering, College of Engineering, University of Iowa, 3131 Seamans Center for the Engineering Arts and Sciences, Iowa City, Iowa 52242, priyadarshini-pennathur@uiowa.edu, Telephone: (+1) 319-335-5683.
Ann Bossen, University of Iowa College of Nursing, CNB, 50 Newton Road, Iowa City, IA 52242, USA, ann-bossen@uiowa.edu, Telephone: (+1) 319- 335-3488.
Alexander Gloeckner, GE Healthcare, 1714 E Irving Pl. 3, Milwaukee, WI 53202.
REFERENCES
- Alzheimer's Association. 2014 Alzheimer's Disease Facts and Figures: Alzheimer's Association International. 2014 [Google Scholar]
- Baker C. Insitgy on the Issues. Vol. 79. AARP Public Policy Institute; 2013. A Connection for all ages: Enabling the benefits of high-speed internet access for older adults. [Google Scholar]
- Baker C, Seegert L. Insight on the Issues. Vol. 84. AARP Public Policy Institute; 2013. A Platform for Aging in Place: The Increasing Potential of High-speed Internet Connectivity. [Google Scholar]
- Bangor A, Kortum P, Miller J. Determinin what individual SUS Scores Mean: Adding an adjective rating scale. Journal of Usability Studies. 2009;4(3):114–123. [Google Scholar]
- Bossen A, Kim H, Williams K, Steinhoff A, Strieker M. Emerging roles for telemedicine and smart technologies in dementia care. Smart Homecare Technology and TeleHealth, 2015. 2015;3:49–57. doi: 10.2147/SHTT.S59500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin JF. Technology, Innovation, and Developing a NexGen Aging Services Workforce. Public Policy & Aging Report. 2014;24(1):6–9. [Google Scholar]
- Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, Sharit J. Factors predicting the use of technology: Findings from the center for research and education on aging and technology enhancement (create) Psychology and Aging. 2006;21(2):333–352. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Ambrosio LA, Mehler AC. Three Things Policymakers Should Know About Technology and Older Adults. Public Policy & Aging Report. 2014;24(1):10–13. [Google Scholar]
- Fox S, Brenner J. Family Caregivers Online. PewResearch Internet Project. 2012 [Google Scholar]
- Godwin KM, Mills WL, Anderson JA, Kunik ME. Technology-driven interventions for caregivers of persons with dementia: a systematic review. Am J Alzheimers Dis Other Demen. 2013;28(3):216–222. doi: 10.1177/1533317513481091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickman JM, Rogers WA, Fisk AD. Training Older Adults To Use New Technology. The Journals of Gerontology Series B. Psychological Sciences and Social Sciences. 2007;62(Special Issue 1):77–84. doi: 10.1093/geronb/62.special_issue_1.77. [DOI] [PubMed] [Google Scholar]
- Kramer B. Dementia Caregivers in Germany and Their Acceptance of New Technologies for Care: The Information Gap. Public Policy & Aging Report. 2013;24(1):32–34. [Google Scholar]
- Lee C. Adoption of Smart Technology Among Older Adults: Challenges and Issues. Public Policy & Aging Report. 2013;24(1):14–17. [Google Scholar]
- Lee C. Adoption of Smart Technology Among Older Adults: Challenges and Issues. Public Policy & Aging Report. 2014;24(1):14–17. [Google Scholar]
- Lewis ML, Hobday JV, Hepburn KW. Internet-based program for dementia caregivers. Am J Alzheimers Dis Other Demen. 2010;25(8):674–679. doi: 10.1177/1533317510385812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving. e-Connected Family Caregiver: Bringing Caregiving into the 21st Century. 2011 http://www.caregiving.org/data/FINAL_eConnected_Family_Caregiver_Study_Jan 2011.pdf. [Google Scholar]
- Pew Research Center. Numbers, Facts and Trends Shaping the World. Pew Research Center; 2014. Older adults and technology use. [Google Scholar]
- Roashan R. Telehealth Report-2014: IHS Abstract (Medical Devices & Healthcare) 2014 [Google Scholar]
- Talley RC, Crews JE. Framing the public health of caregiving. American Journal of Public Health. 2007;97(2):224–228. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hoof J, Kort HS, Rutten PG, Duijnstee MS. Ageing-in-place with the use of ambient intelligence technology: perspectives of older users. Int J Med Inform. 2011;80(5):310–331. doi: 10.1016/j.ijmedinf.2011.02.010. [DOI] [PubMed] [Google Scholar]
- White M, Dorman SM. Receiving social support online: implications for health education. Health Education Research. 2001;16(6):693–707. doi: 10.1093/her/16.6.693. [DOI] [PubMed] [Google Scholar]
- Williams K. Linking resident behavior to dementia care communication: effects of emotional tone. Behav Ther. 2011;42(1):42–46. doi: 10.1016/j.beth.2010.03.003. 10.1016/j.beth.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Herman R, Gajewski B, Wilson K. Elderspeak communication: Impact on dementia care. American Journal of Alzheimer’s Disease and Other Dementias. 2009;24:11–20. doi: 10.1177/1533317508318472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu YH, Damnee S, Kerherve H, Ware C, Rigaud A-S. Bridging the digital divide in older adults: A study from an initiative to inform older adults about new technologies. Clinical Intervnentions in Aging. 2015;10:193–201. doi: 10.2147/CIA.S72399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwijsen SA, Niemeijer AR, Hertogh CM. Ethics of using assistive technology in the care for community-dwelling elderly people: an overview of the literature. Aging Ment Health. 2011;15(4):419–427. doi: 10.1080/13607863.2010.543662. [DOI] [PubMed] [Google Scholar]