Abstract
Clinical studies have shown that bismuth-containing quadruple therapy given twice a day for 10 to 14 days is effective and safe in the treatment of Helicobacter pylori infection in Sardinia. However, bismuth is no longer available in Italy.
To report the effectiveness and tolerability of pantoprazole 20 mg, tetracycline 500 mg, and metronidazole 500 mg given b.i.d. (with the midday and evening meals) for 10 days supplemented with Lactobacillus reuteri (DSM 17938) 108 cfu/tablet once a day for 20 days in patients treated in a routine daily practice setting.
H pylori infection was defined as a positive gastric histopathology and/or 13C-Urea Breath Test (UBT) and/or stool antigen testing. Successful eradication was documented by 13C-UBT, and/or stool antigen assay at least 4 weeks post-therapy. Compliance and side effects were recorded after completing treatment.
A total of 45 patients (10 men, 35 women; mean age 52.6 years) have completed the treatment regimen with the success rate of 93% (95% confidence interval = 85–99%). Compliance was excellent. Side effects were absent or generally mild.
Proton pump inhibitor-tetracycline-metronidazole-L reuteri therapy provided high eradication rates with few side effects and therefore can safely replace bismuth in H pylori treatment. Further studies are needed that include susceptibility testing.
INTRODUCTION
Treatment failure of antimicrobial therapy for Helicobacter pylori infection is frequent and most often related to the presence of resistant bacteria or poor patient compliance. In Sardinia, the overall cure rates of legacy triple therapies have been demonstrated to be poor.1 However, omeprazole, 20 mg bid, plus metronidazole, 500 mg bid, plus tetracycline, 500 mg qid (OMT) was previously shown to be successful (e.g., cure rate of 91%; 95% confidence interval [CI] 80.4–97%).1 We previously showed that twice a day bismuth-containing quadruple therapy given at the evening and midday meals for 14 days provided excellent H pylori eradication as a primary therapy.2 In that study, the per protocol (PP) treatment success was 98% and the intention to treat (ITT) success was 95% despite smoking status, clinical diagnosis, and prior treatment failure.2 The regimen was subsequently evaluated in terms of duration (14 days vs 10 days) in a randomized trial of 417 patients.3 Bismuth-containing quadruple therapy remained highly effective although a reduced duration from 14 to 10 days with a success rate of ≥95% by PP and > 90% by ITT analysis.3 In the last year, bismuth has become unavailable in Italy.
Probiotics have been used in the treatment of H pylori infection and have proven useful in reducing side effects of traditional antimicrobial therapy and for enhancing patient compliance.4 Strains of L reuteri have previously been shown to inhibit colonization of human gastric mucosa by H pylori.5 In addition, L reuteri is able to produce reuterin, a broad spectrum antibiotic active against H pylori.6 Taking into account these results, a potential role of L reuteri in H pylori eradication therapy appeared likely. For this reason, in an intervention study, L reuteri (DSM 17938) 108 cfu plus pantoprazole 20 mg twice a day for 8 weeks was used to treat H pylori infection.7 The regimen cured 13.6% (3/22; 95% CI 2.9–34.9%) of patients with H pylori infection by ITT analysis and 14.2% (3/21; 95% CI 3.0–36%) by PP analysis.7 According to our previous experience, we examined whether substitution of L reuteri for bismuth, a modified OMT therapy would be effective for H pylori eradication in clinical practice. In this case series, we report the preliminary results of this highly effective novel regimen.
METHODS
Clinical Setting
Consecutive patients who underwent upper endoscopy at our Gastroenterology Unit between April, 2014, and November, 2015, and found positive for H pylori were treated for the infection. The majority of patients were referred to the endoscopy by family physicians and/or specialists from Northern Sardinia for dyspeptic and/or reflux symptoms. Demographic data including age, gender, cigarette smoking, and the height and weight were collected for each patient. Body mass index (BMI; weight in kilograms divided by height in square meters) was calculated using the formula Wt (kg)/Ht(m)2.
At baseline, patients were evaluated for symptoms, history of allergy to any of the drugs used, and for prior treatment for H pylori infection. Pretreatment culture of biopsy specimens and antibiotic susceptibility tests were not done. Thereafter, patients were evaluated to assess the eradication of H pylori infection and occurrence of adverse events as usual in clinical practice.
H pylori Status
Pretreatment H pylori infection was defined as the presence of H pylori on histological examination of gastric biopsies (2 from the antrum, 1 from the angulus, and 1 from the gastric corpus) or a positive 13C-UBT or antigen stool test. Post-treatment success was defined by a negative 13C-UBT or a negative H pylori antigen stool assay at least 30 days after therapy.
Treatment Regimen
Patients were treated with a modified regimen consisting of pantoprazole 20 mg, plus metronidazole 500 mg, and tetracycline 500 mg, all twice daily with the midday and evening meals for a total of 10 days, supplemented with L reuteri (DSM 17938, 108 cfu/tablet) (Reuflor®, BioGaia AB, Sweden) once a day for 20 days given at least 3 hours after breakfast. The duration of 20 days probiotics treatment (which started with H pylori therapy) was arbitrarily chosen in order to reduce the direct costs for the patient (20 lozenges for pack: € 15.2). Clear written instructions about when and how to take the pills were given to the patients.
There was no pharmaceutical sponsor for this study and no pharmaceutical company participation in any phase.
Enrolled patients have given their consent forms to publish our collected data according to the hospital regulations.
RESULTS
Patients
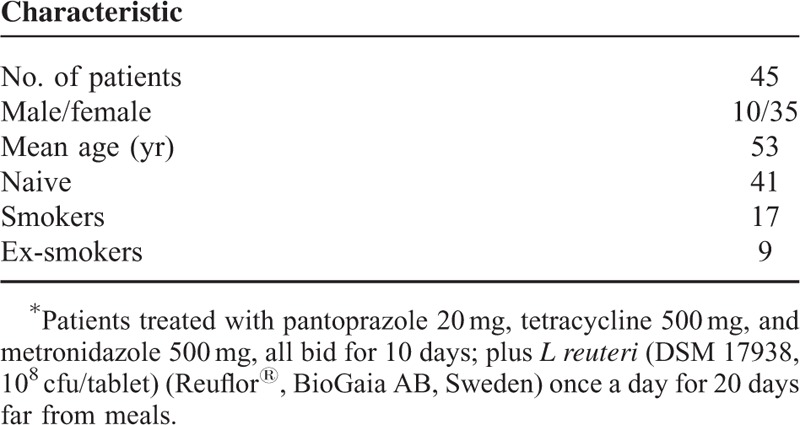
Our study showed that the number of patients who have completed the therapy was 45 (M: 10; F: 35) with a mean age of 53 years (Table 1). The cure rate was 42/45 (93.3 %; 95% CI = 85–99 %) and the treatment was effective in all men. Among the treated patients, 4 were previously treated for H pylori (1 patient with PPI-amoxicillin and clarithromycin bid for 7 days and the other one with several different regimens; 2 patients ignored the previous treatment). However, among the treatment failures, the modified therapy was effective in 50% (2/4). Demographic data of the patients are shown in Table 1. Peptic ulcer disease was present in 4.4% of patients (2/45) in the treated group. There was no correlation between BMI and cure rate.
TABLE 1.
Baseline Characteristics of Treated Patients∗
Patient Compliance and Side Effects
The overall tolerability was good. Excellent compliance (>95 % of medicines) was reported by all patients with the exception of one who took 80% of doses. Side effects were not recorded by using a standardized questionnaire. However, the major complaints were available in all studied patients. The most common side effects were mild diarrhea for 2 to 3 days reported in 5 patients (11 %) or abdominal discomfort presented in 3 patients.
DISCUSSION
There have been many attempts to develop a reliably effective treatment protocol to cure H pylori infection worldwide. As with other bacterial infections, the mainstay of therapy is the use of antimicrobials. However, the most effective treatment regimens are complicated requiring administration of many different drugs at multiple intervals and for a longer time (14 days).8 Three or 4 drug therapies appear necessary to achieve maximum cure rates. The original therapy with a high success rate in eradicating H pylori was developed by Borody et al in 1989.9 That regimen involved 3 drugs, bismuth, metronidazole, and tetracycline: BMT triple therapy. Bismuth salts have been used in medicine for >200 years,10 for example, to treat syphilis before the antibiotics era and more recently to prevent Escherichia coli travelers’ diarrhea.11 Ultrastructural examination shows that bismuth is directly bactericidal to H pylori leading to cell lysis with a marked reduction in bacterial colonies.10,11 Short-term bismuth use has an excellent safety record. The original BMT therapy consisted of bismuth (525 mg 4 times daily), and 2 antibiotics (e.g., metronidazole 250 mg 4 times daily and tetracycline 500 mg 4 times daily) given for 10 to 14 days without a PPI.9 The subsequent addition of a PPI and increasing the dose of metronidazole to 1500 or 1600 mg improved cure rates despite metronidazole resistance.12 Legacy clarithromycin-containing triple therapy currently provides miserable eradication rates in Sardinia explained, in part, by pretreatment antibiotic-resistant strains including to amoxicillin.1,13 However, triple therapy consisting of omeprazole, 20 mg bid, plus metronidazole, 500 mg bid, plus tetracycline, 500 mg qid (OMT) appeared promising because of the high success rate with metronidazole-resistant H pylori.1 In order to enhance efficacy, bismuth (colloidal bismuth subcitrate 240 mg bid) was added to that regimen (BTM-PPI).2 Moreover, to reduce the complexity, we attempted twice a day therapy to lower drug administrations.2 Exploratory studies confirmed the efficacy of such treatment regimens in adult and elderly infected patients with high eradication rates as a first-line regimen2,14,15 and as a salvage therapy.2,14 The regimen was associated with mild side effects. In addition, twice-a-day BMT-PPI therapy in a randomized trial of 10 and 14 days remained highly effective when given for 10 days (i.e., ≥95% PP and > 90% ITT).3
A pilot study conducted in Sardinia showed that L reuteri may have a potential role in H pylori eradication. More specifically, L reuteri plus pantoprazole bid was able to cure 13.6% (3/22; 95% CI 2.9–34.9%) of patients positive for H pylori infection by ITT analysis and 14.2% (3/21; 95% CI 3.0–36%) by PP analysis.7 Recently, bismuth was removed from the Italian market. For this reason, the modified low-dose PMT regimen supplemented with a probiotics was empirically utilized to take advantage of the potential topical action by L reuteri in the gastric mucosa.
One limitation of this series is that pretreatment susceptibility tests were not performed. For that reason we were not able to compare treatment efficacy of the novel protocol against sensitive and resistant metronidazole H pylori strains. Moreover, pretreatment measures of compliance and side effects were not defined. Nevertheless the excellent results with the novel protocol regimen suggested that twice a day, noon and evening meal, low-dose PMT therapy supplemented with L reuteri might potentially replace bismuth. Subsequent studies comparing the triple therapy (PPI, metronidazole, tetracycline) with or without L reuteri are planned along with assessment of antimicrobial susceptibility to fully characterize the therapy and understand the role of the different components.
Footnotes
Abbreviations: BMI = body mass index, CFU = colony forming unit, CI = confidence interval, Ht = body height, ITT = intention to treat, OMT = omeprazole + metronidazole + tetracycline, OR = odds ratio, PP = per protocol, PPI = proton pump inhibitors, UBT = urea breath test, Wt = weight.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Realdi G, Dore MP, Piana A, et al. Pretreatment antibiotic resistance in Helicobacter pylori infection: results of three randomized controlled studies. Helicobacter 1999; 4:106–112. [DOI] [PubMed] [Google Scholar]
- 2.Dore MP, Graham DY, Mele R, et al. Colloidal bismuth subcitrate-containing twice-a-day quadruple therapy as primary or salvage therapy for Helicobacter pylori infection. Am J Gastroenterol 2002; 97:857–860. [DOI] [PubMed] [Google Scholar]
- 3.Dore MP, Farina V, Cuccu M, et al. Twice-a-day bismuth-containing quadruple therapy for Helicobacter pylori eradication: a randomized trial of 10 and 14 days. Helicobacter 2011; 16:295–300. [DOI] [PubMed] [Google Scholar]
- 4.Dore MP, Goni E, Di Mario F. Is there a role for probiotics in Helicobacter pylori therapy? Gastroenterol Clin North Am 2015; 44:565–575. [DOI] [PubMed] [Google Scholar]
- 5.Mukai T, Asasaka T, Sato E, et al. Inhibition of binding of Helicobacter pylori to the glycolipid receptors by probiotic Lactobacillus reuteri. FEMS Immunol Med Microbiol 2002; 32:105–110. [DOI] [PubMed] [Google Scholar]
- 6.Chung T, Axelsson S. In vitro studies on reuterin synthesis by Lactobacillus reuteri. Microb Ecol Health Dis 1989; 2:137–144. [Google Scholar]
- 7.Dore MP, Cuccu M, Pes GM, et al. Lactobacillus reuteri in the treatment of Helicobacter pylori infection. Intern Emerg Med 2014; 9:649–654. [DOI] [PubMed] [Google Scholar]
- 8.Graham DY. Hp-normogram (normo-graham) for assessing the outcome of H. pylori therapy: effect of resistance, duration, and CYP2C19 genotype. Helicobacter 2016; 21:85–90. [DOI] [PubMed] [Google Scholar]
- 9.Borody TJ, Cole P, Noonan S, et al. Recurrence of duodenal ulcer and Campylobacter pylori infection after eradication. Med J Aust 1989; 151:431–435. [DOI] [PubMed] [Google Scholar]
- 10.Marshall BJ. The use of bismuth in gastroenterology. The ACG Committee on FDA-Related Matters. American College of Gastroenterology. Am J Gastroenterol 1991; 86:16–25. [PubMed] [Google Scholar]
- 11.Graham DY, Evans DG. Prevention of diarrhea caused by enterotoxigenic Escherichia coli: lessons learned with volunteers. Rev Infect Dis 1990; 12 Suppl 1:S68–S72. [DOI] [PubMed] [Google Scholar]
- 12.van der Hulst RWM, Keller JJ, Rauws EA, et al. Treatment of Helicobacter pylori infection in humans: a review of the world literature. Helicobacter 1996; 1:6–19. [DOI] [PubMed] [Google Scholar]
- 13.Dore MP, Piana A, Carta M, et al. Amoxycillin resistance is one reason for failure of amoxycillin-omeprazole treatment of Helicobacter pylori infection. Aliment Pharmacol Ther 1998; 12:635–639. [DOI] [PubMed] [Google Scholar]
- 14.Dore MP, Marras L, Maragkoudakis E, et al. Salvage therapy after two or more prior Helicobacter pylori treatment failures: the super salvage regimen. Helicobacter 2003; 8:307–309. [DOI] [PubMed] [Google Scholar]
- 15.Dore MP, Maragkoudakis E, Pironti A, et al. Twice-a-day quadruple therapy for eradication of Helicobacter pylori in the elderly. Helicobacter 2006; 11:52–55. [DOI] [PubMed] [Google Scholar]


