Abstract
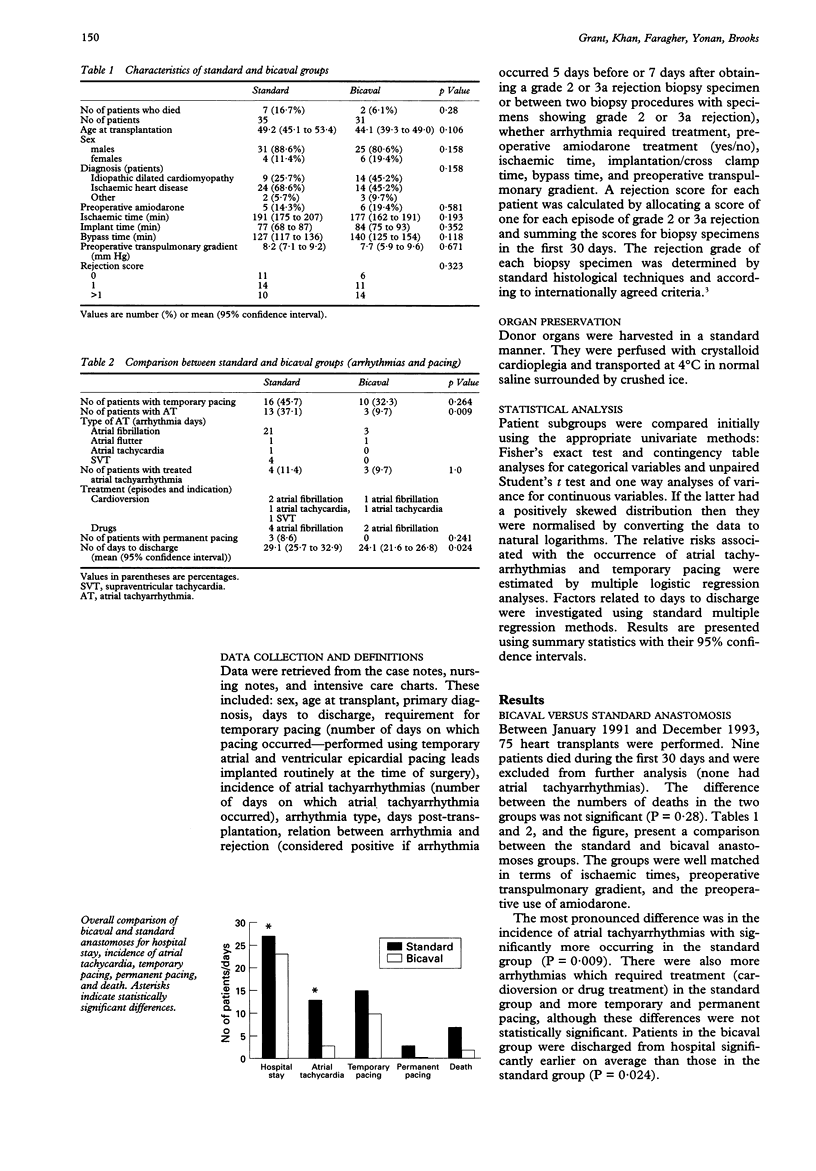
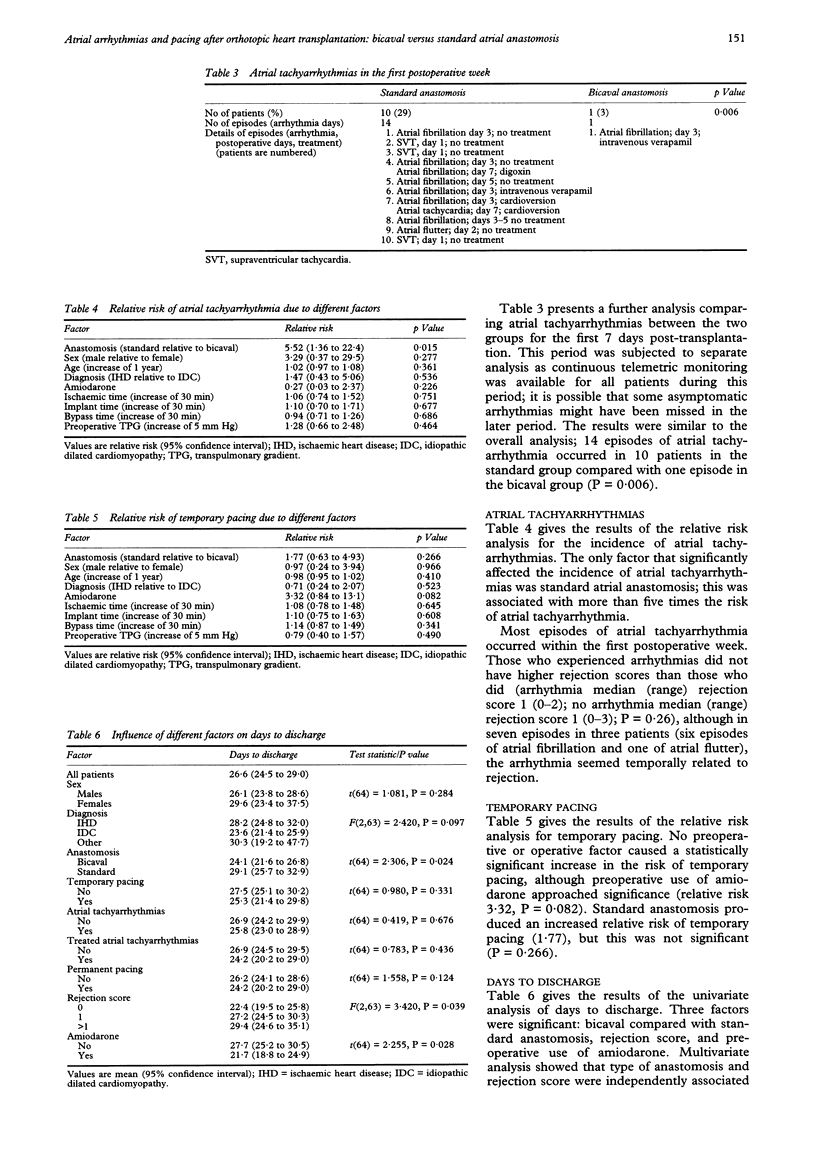
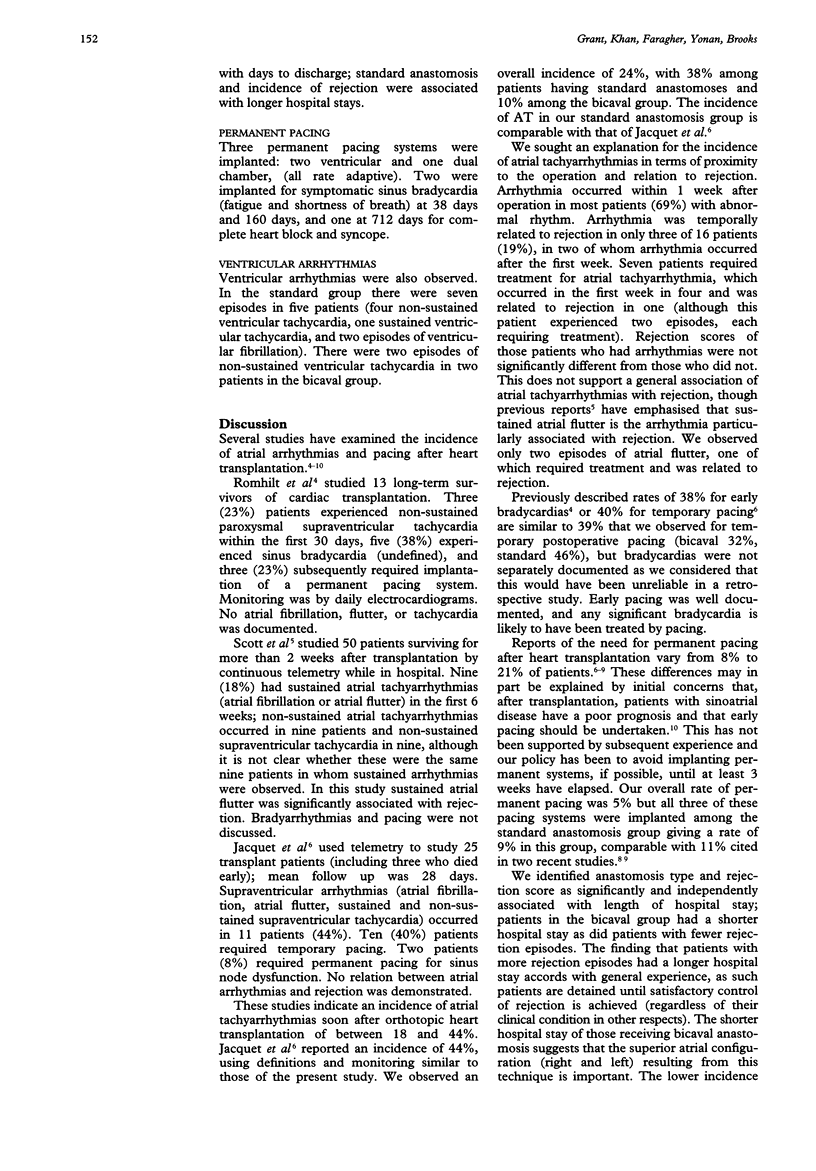
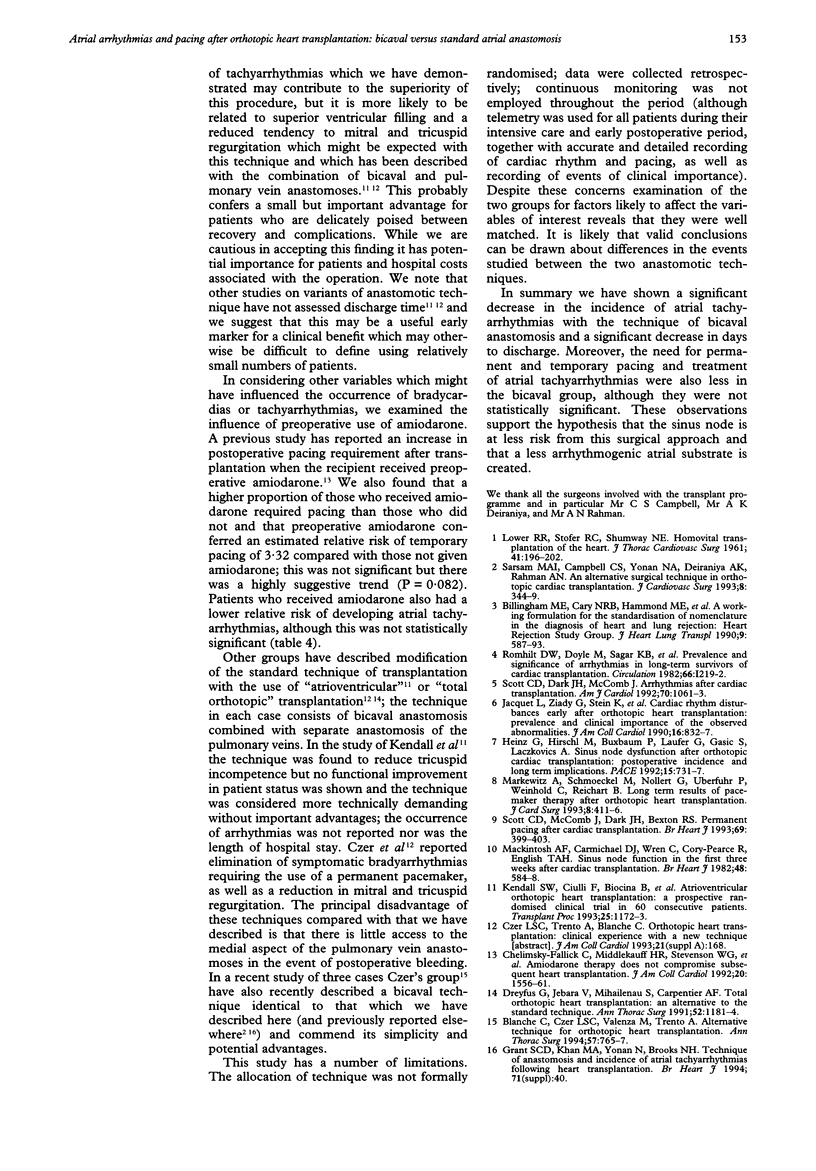
BACKGROUND--Right and left atrial configuration is more normal when the donor left atrium is anastomosed to a recipient left atrial cuff with direct anastomoses of the donor and recipient vena cavas on the right side. The right atrium and sinus node may be less disturbed by the technique of bicaval anastomosis than by the standard procedure. OBJECTIVE--To compare the incidence of atrial arrhythmias and pacing after bicaval and standard anastomoses. METHODS--75 patients had heart transplants between January 1991 and December 1993. The notes were reviewed. Nine patients who died within the first 30 days were excluded from further analysis (seven patients with standard anastomoses, one with bicaval anastomosis, and one with a hybrid technique). RESULTS--66 patients survived for more than 30 days. Thirty five patients had standard anastomoses and 31 bicaval anastomoses. Atrial tachyarrhythmias (atrial fibrillation, atrial flutter, atrial tachycardia, or supraventricular tachycardia) occurred on four days in three patients in the bicaval group compared with 27 days in 13 patients in the standard group (P = 0.009). The relative risk of atrial tachyarrhythmias with standard anastomosis was 5.52 (P = 0.015) compared with that of bicaval anastomosis. Atrial tachyarrhythmias requiring treatment occurred less often in the bicaval group (four episodes in three patients in the bicaval group and eight episodes in four patients in the standard group), and fewer patients with a bicaval anastomosis required temporary pacing (pacing on 20 days in 10 patients in the bicaval group, but pacing on 49 days in 16 patients in the standard group) and late permanent pacing (no patients in the bicaval group and three patients in the standard group), although these differences were not statistically significant. Patients in the bicaval group were discharged from hospital sooner than those in the standard group (mean 24.1 v 29.1 days, P = 0.024). CONCLUSIONS--The technique of bicaval anastomosis, in addition to theoretical advantages from maintaining a more normal atrial configuration, has a lower incidence of postoperative atrial tachyarrhythmias, may reduce the need for pacing, and allows earlier discharge from hospital.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Billingham M. E., Cary N. R., Hammond M. E., Kemnitz J., Marboe C., McCallister H. A., Snovar D. C., Winters G. L., Zerbe A. A working formulation for the standardization of nomenclature in the diagnosis of heart and lung rejection: Heart Rejection Study Group. The International Society for Heart Transplantation. J Heart Transplant. 1990 Nov-Dec;9(6):587–593. [PubMed] [Google Scholar]
- Blanche C., Czer L. S., Valenza M., Trento A. Alternative technique for orthotopic heart transplantation. Ann Thorac Surg. 1994 Mar;57(3):765–767. doi: 10.1016/0003-4975(94)90592-4. [DOI] [PubMed] [Google Scholar]
- Chelimsky-Fallick C., Middlekauff H. R., Stevenson W. G., Kobashigawa J., Saxon L. A., Moriguchi J., Brownfield E. D., Hamilton M. A., Drinkwater D., Laks H. Amiodarone therapy does not compromise subsequent heart transplantation. J Am Coll Cardiol. 1992 Dec;20(7):1556–1561. doi: 10.1016/0735-1097(92)90450-2. [DOI] [PubMed] [Google Scholar]
- Dreyfus G., Jebara V., Mihaileanu S., Carpentier A. F. Total orthotopic heart transplantation: an alternative to the standard technique. Ann Thorac Surg. 1991 Nov;52(5):1181–1184. doi: 10.1016/0003-4975(91)91311-i. [DOI] [PubMed] [Google Scholar]
- Heinz G., Hirschl M., Buxbaum P., Laufer G., Gasic S., Laczkovics A. Sinus node dysfunction after orthotopic cardiac transplantation: postoperative incidence and long-term implications. Pacing Clin Electrophysiol. 1992 May;15(5):731–737. doi: 10.1111/j.1540-8159.1992.tb06838.x. [DOI] [PubMed] [Google Scholar]
- Jacquet L., Ziady G., Stein K., Griffith B., Armitage J., Hardesty R., Kormos R. Cardiac rhythm disturbances early after orthotopic heart transplantation: prevalence and clinical importance of the observed abnormalities. J Am Coll Cardiol. 1990 Oct;16(4):832–837. doi: 10.1016/s0735-1097(10)80330-4. [DOI] [PubMed] [Google Scholar]
- Kendall S. W., Ciulli F., Biocina B., Mullins P. A., Schofield P., Wells F. C., Wallwork J., Large S. R. Atrioventricular orthotopic heart transplantation: a prospective randomised clinical trial in 60 consecutive patients. Transplant Proc. 1993 Feb;25(1 Pt 2):1172–1173. [PubMed] [Google Scholar]
- LOWER R. R., STOFER R. C., SHUMWAY N. E. Homovital transplantation of the heart. J Thorac Cardiovasc Surg. 1961 Feb;41:196–204. [PubMed] [Google Scholar]
- Mackintosh A. F., Carmichael D. J., Wren C., Cory-Pearce R., English T. A. Sinus node function in first three weeks after cardiac transplantation. Br Heart J. 1982 Dec;48(6):584–588. doi: 10.1136/hrt.48.6.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markewitz A., Schmoeckel M., Nollert G., Uberfuhr P., Weinhold C., Reichart B. Long-term results of pacemaker therapy after orthotopic heart transplantation. J Card Surg. 1993 May;8(3):411–416. doi: 10.1111/j.1540-8191.1993.tb00385.x. [DOI] [PubMed] [Google Scholar]
- Sarsam M. A., Campbell C. S., Yonan N. A., Deiraniya A. K., Rahman A. N. An alternative surgical technique in orthotopic cardiac transplantation. J Card Surg. 1993 May;8(3):344–349. doi: 10.1111/j.1540-8191.1993.tb00375.x. [DOI] [PubMed] [Google Scholar]
- Scott C. D., Dark J. H., McComb J. M. Arrhythmias after cardiac transplantation. Am J Cardiol. 1992 Oct 15;70(11):1061–1063. doi: 10.1016/0002-9149(92)90361-2. [DOI] [PubMed] [Google Scholar]
- Scott C. D., McComb J. M., Dark J. H., Bexton R. S. Permanent pacing after cardiac transplantation. Br Heart J. 1993 May;69(5):399–403. doi: 10.1136/hrt.69.5.399. [DOI] [PMC free article] [PubMed] [Google Scholar]


