Abstract
Background
Geriatric syndromes are common in older adults and associated with adverse outcomes. The prevalence, recognition, co-occurrence and recent onset of geriatric syndromes in patients transferred from hospital to skilled nursing facilities (SNFs) are largely unknown.
Design
Quality improvement project.
Setting
Acute care academic medical center and 23 regional partner SNFs.
Participants
686 Medicare beneficiaries hospitalized between January 2013 and April 2014 and referred to SNFs.
Measurements
Nine geriatric syndromes were measured by project staff -- weight loss, decreased appetite, incontinence and pain (standardized interview), depression (Geriatric Depression Scale), delirium (Brief-Confusion Assessment Method), cognitive impairment (Brief Interview for Mental Status), falls and pressure ulcers (hospital medical record utilizing hospital-implemented screening tools). Estimated prevalence, new-onset prevalence and common coexisting clusters were determined. The extent that syndromes were commonly recognized by treating physicians and communicated to SNFs in hospital discharge documentation was evaluated.
Results
Geriatric syndromes were prevalent in more than 90% of hospitalized adults referred to SNFs; 55% met criteria for 3 or more co-existing syndromes. Overall the most prevalent syndromes were falls (39%), incontinence (39%), decreased appetite (37%) and weight loss (33%). Of individuals that met criteria for 3 or more syndromes, the most common triad clusters included nutritional syndromes (weight loss, loss of appetite), incontinence and depression. Treating hospital physicians commonly did not recognize and document geriatric syndromes in discharge summaries, missing 33–95% of syndromes present as assessed by research personnel.
Conclusion
Geriatric syndromes in hospitalized older adults transferred to SNF are prevalent and commonly co-exist with the most frequent clusters including nutritional syndromes, depression and incontinence. Despite the high prevalence, this clinical information is rarely communicated to the SNF on discharge.
Keywords: Geriatric syndromes, skilled nursing facility, care transitions, older adults
INTRODUCTION
Geriatric syndromes represent clinical conditions common in older adults that share underlying causative factors and involve multiple organ systems.1,2 They include a number of clinical conditions, which unlike traditional syndromes, do not fit a discrete disease category. Examples of geriatric syndromes include incontinence, cognitive impairment, delirium, falls, pressure ulcers, pain, weight loss, anorexia, functional decline, depression, and multi-morbidity.3–5
Geriatric syndromes are prevalent among older adults6 and independently associated with a risk for adverse outcomes such as functional decline,7 the acquisition of additional syndromes, hospital admissions8 and mortality,5 even when controlling for illness severity and age. Additionally, studies have demonstrated a relationship between the increasing number of geriatric syndromes experienced by a patient and functional decline.5,9
Despite the contributing role of geriatric syndromes in the presentation, management and outcome of acute illness, they are often under-recognized and seldom the focus of the hospital treatment.10 Currently, it is unclear how well hospital providers convey information about geriatric syndromes to the skilled nursing facility (SNF) during the transition of care for older hospitalized adults.11,12 Thus, these syndromes may remain unaddressed during the convalescent period, which may lead to a chronic presence. Moreover, failure to document geriatric syndromes at hospital discharge could delay or prevent the development of care plans to manage these syndromes both during the SNF stay and at SNF discharge. Recent data document that SNF discharge planning is often inadequate and a high percentage of patients are readmitted to the hospital after SNF discharge.7–10,13
Although it is important to assess geriatric syndromes for all older hospitalized patients, these syndromes may have greater clinical significance among patients discharged to SNFs for several reasons. First, a greater proportion of Medicare beneficiaries are discharged to a SNF than to any other post-acute care setting.14 In addition, in comparison to patients who return home, patients discharged to a SNF are older, more disabled and have a higher prevalence of multi-morbidity which may in part account for the loss of independence and poor outcomes reported for many SNF patients.15–17 Despite this, the unique opportunity that the SNF environment provides to implement interventions to address geriatric syndromes, as compared to patients who return home, suggests that targeting this population may have the greatest impact.
To date, the majority of studies evaluating the prevalence of geriatric syndromes in the hospital setting have focused on individuals discharged home and who have specific conditions,15,18 such as heart disease. As a result, there are limited data describing the prevalence of geriatric syndromes in individuals discharged to SNFs, including the extent to which multiple syndromes co-occur and the prevalence of newly acquired syndromes associated with the hospital admission.7,19
In the current study, we aimed to address this knowledge gap as part of a larger Centers for Medicare and Medicaid Services (CMS) Health Care Innovations Award to improve the transition process from acute care to SNF for Medicare patients. In this study we had three objectives: 1) quantify the prevalence of nine geriatric syndromes, and among those, identify what proportion were newly diagnosed in relation to the recent hospitalization, 2) determine the most common clusters of geriatric syndromes; and, 3) measure the adequacy of discharge documentation provided by acute care providers to the accepting SNFs with respect to these geriatric syndromes.
METHODS
Participants & Setting
All Medicare patients discharged from a single large university hospital to 23 regional SNFs (partner facilities) from January, 2013 through April, 2014 were eligible for study inclusion. The university-affiliated Institutional Review Board provided approval for this project and waived the requirement for written, informed consent. Instead, eligible patients were provided a standardized description of the project by trained clinical personnel (at the time of their referral to one of the participating SNFs) and had the right to refuse the interview.
Medical Record Review
Trained research personnel used a standardized form to review the medical record of each participant for demographic information (e.g., age, sex, and ethnicity), length of hospital stay (in days), discharge service, admission diagnosis and number of medications at the time of discharge.
Geriatric Syndrome Assessments
Clinically trained research personnel independently assessed patients during the hospital admission for the presence or absence of nine geriatric syndromes (Table 1). Seven syndromes (delirium, cognitive impairment, depressive symptoms, pain, incontinence, unintentional weight loss, loss of appetite) were assessed by direct patient interview (see Table 1 for specific standardized interviews and criteria). For the remaining two syndromes falls and pressure ulcers, a combination of medical record review and interview were performed. The source of information for falls and pressure ulcers was used because there is a concurrent hospital wide effort to perform a standardized fall assessment and pressure ulcer risk assessment (including a Braden score) as part of the nursing admission history and physical. There is no consistent documentation or screening questions for the other syndromes. All information was collected for the purposes of improving the assessment of geriatric syndromes and was subsequently communicated to SNF providers at the point of hospital discharge as part of the larger quality improvement initiative.
Table 1.
Geriatric Syndrome Assessment
| Syndrome | Assessment Method | Details | Completion Rate |
|---|---|---|---|
| Weight Loss | 1-Item Interview | “Have you lost weight without trying to within the last month prior to being admitted to the hospital?” “Have you lost weight during this hospital stay?” |
66% |
| Decreased Appetite | 2-Item Interview | “Have you noticed a change in your appetite since being admitted to the hospital?” | 85% |
| Bladder & Bowel Incontinence | 2-Item Interview | “Do you have any urine or bowel accidents?, If ‘yes’ which?- bladder, bowel or both” If ‘yes’ did that start in hospital or shortly before you came to hospital or is this chronic/long-term?” |
86% |
| Depressive Symptoms | Geriatric Depression Scale (GDS) - 5 Item | Presence = GDS-5 Score ≥ 2, Absence = GDS-5 Score < 2 If GDS-5 Score ≥ 2 – “Do you think your answers show a change from what you were like a month ago?” |
76% |
| Delirium | Brief-Confusion Assessment Method (B-CAM) | Positive/Negative according to B-CAM | 84% |
| Cognitive Impairment | Brief Interview for Mental Status (BIMS) | Cognitively Impaired = Score ≤ 12, Cognitively Intact = Score 13–15 “Do you think you would have done better, worse, or the same on this test a month ago?” |
80% |
| Pain at Discharge | 3-Item Interview | “Please rate your current pain on a scale from 0 to 10 with 0 being no pain and 10 being the worst pain you can imagine” OR ““Please rate the intensity of your current pain – None, mild, moderate, severe, very severe” Presence of Moderate/Severe on verbal or = ≥5 on numeric scale “What is your usual pain level, prior to being admitted to the hospital?” (Numerical or Verbal) |
72% |
| Falls | Medical record review | Presence of falls in the last 3 months (from time of hospital admission) | 99% |
| Pressure Ulcers | Medical record review | Pressure Ulcers (Stage 1–4) at or during hospital admission | 91% |
The following standardized geriatric screening assessments were administered in person by research personnel during each participant’s hospital stay: Brief Confusion Assessment Method (BCAM),20–22 Brief Interview for Mental Status (BIMS)23,24 and the Geriatric Depression Scale (GDS) 5-item version.25,26 The BCAM is a short screening tool that assesses the presence of delirium. The BIMS is a short, objective screening tool for cognitive impairment and is highly correlated with other validated cognitive assessments. The BIMS total score ranges from 0 to 15 (0–7: severe impairment; 8–12: moderate impairment; 13–15: cognitively intact). A patient with a score of 12 or less was categorized as being cognitively impaired. Prior studies have demonstrated that older adults with mild to moderate cognitive impairment remain capable of reliably responding to structured interview questions about pain, so patients with lower BIMS scores were not excluded from analyses if they provided complete data.27–29 BIMS assessments were not included for patients who scored positively for delirium on the BCAM as the presence of delirium can result, itself, in the presence of cognitive dysfunction due to a variety of causes not attributed to dementia.30
The GDS 5-item is a screening tool for depression and has been shown to be reliable and valid in community-dwelling, acute care and long-term care patients.25 The GDS 5-item provides a total score between 0 (no symptoms) and 5 (all 5 symptoms endorsed), with a score of two or higher indicative of probable depression. In addition, patients were asked about their pain at the time of hospital discharge using the following structured questions: “Please rate your current pain on a scale from 0 to 10 with 0 being no pain and 10 being the worst pain you can imagine”. Individuals with a numeric response ≥ 5 were classified as having moderate to severe pain. Additionally, patients were asked about the presence of bladder or bowel incontinence, unintentional weight loss prior to and during their hospital stay and any recent loss of appetite (exact wording of questions provided in Table 1). Individuals were also asked whether self-reported problems with memory, depressive symptoms, pain and incontinence were new-onset (started within a month or less before hospital admission or during their hospital stay) or a chronic condition (present for more than a month prior to hospital admission).
Discharge Packets Sent to SNF Providers
Trained research personnel independently reviewed 54 discharge packets prepared by hospital staff and sent to partner SNFs during July of 2014, which reflects 100% of the Medicare patients transferred to these facilities in July. The discharge packets contain all hospital discharge documents on paper forms (contained in a marked discharge envelope) sent to SNFs at the time of transfer by social workers. These packets were independent of the materials sent by the research team. The results of the discharge packet review were then compared to the results of the standardized geriatric syndrome assessments conducted by research staff to determine the extent to which routine hospital discharge information reflected the geriatric syndromes, as measured by research staff.
Data Analysis
Interview responses of each participant were recorded by trained research personnel using the REDCap data management program.31 Baseline characteristics were reported as means and standard deviations (SD) for continuous variables and percent prevalence for categorical variables. A Pearson’s Chi-square test was used to differences in the prevalence of syndromes by sex. In order to provide a conservative estimate of each geriatric syndrome, we presumed an absence of the syndrome in all cases of missing or incomplete assessment (i.e., participants who were unable or unwilling to complete an assessment were assumed to not have the syndrome). Valid responses as a proportion of the overall study population are also reported as well as reasons for missing data (e.g., participant refusal, unresponsive, insufficient time to complete assessment prior to hospital discharge).
The numbers of syndromes present in each individual and the most frequent combinations of geriatric syndromes are reported only for participants who completed all interviews relevant to each syndrome. We chose to report the most common triads of geriatric syndromes in participants with at least three syndromes similar to previously reported analyses of chronic medical conditions in Medicaid32 and Medicare beneficiaries conducted by the Centers for Disease Control and Prevention (CDC).33 All possible combinations of three geriatric syndromes were assessed for the highest proportion of individuals and the most prevalent triads overall and by sex.
All analyses were performed using SPSS Statistical Package (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY).
RESULTS
Study Population
A total of 686 Medicare beneficiaries who completed one or more of the geriatric syndrome assessments by research staff were discharged to one of 23 participating SNFs between January, 2013 and April, 2014. Completion rates of the 9 geriatric syndromes assessments ranged from 66% for the weight loss assessment to 99% for the assessment of falls (Table 1). A total of 277 participants (36% of overall sample) completed all nine of the geriatric syndrome assessments included in this study (see Table 1 Completion Rates). Reasons for incomplete assessments included: unable to participate due to illness severity (15–20%), responses that were not known (presence of recent weight loss, 8%), patient refusal (2–5%), and insufficient time for research staff to complete the assessment prior to hospital discharge (2–4%).
Table 2 shows the baseline characteristics of participants (N = 686). Overall, 59% of the participants were women, 84% were white and the mean age was 75 years (± 11.8). The study population represented patients from a range of hospital specialties and a broad variety of admission diagnoses. The mean length of hospital stay for all participants prior to SNF transfer was 8.4 days (± 6.2), and the average number of medications per participant at hospital discharge was 14 (± 4.8).
Table 2.
Baseline Characteristics of Hospitalized Patients Transferred to Skilled Nursing Facility
| Characteristic | N = 686 |
|---|---|
| Age, in years, mean (± SD) | 75 (± 11.8) |
| Sex, n (%) | |
| Female | 405 (59%) |
| Race, n (%) | |
| White | 574 (83.7%) |
| African American | 97 (14.1%) |
| Other | 15 (2.2%) |
| Discharge Service, n (%) | |
| Orthopedics | 156 (22.74%) |
| Geriatrics | 114 (16.62%) |
| General Medicine | 97 (14.14%) |
| Cardiology/Cardiac Surgery | 92 (13.41%) |
| Neurology/Neurosurgery | 67 (9.77%) |
| Other | 160 (23.3%) |
| Admission Diagnosis, n (%) | |
| Falls/fracture | 127 (18.5%) |
| Pneumonia | 33 (4.8%) |
| Osteoarthritis | 30 (4.4%) |
| Ischemic Heart Disease | 27 (3.9%) |
| Urinary Tract Infection | 26 (3.8%) |
| Malignancy | 22 (3.2%) |
| Altered Mental Status | 22 (3.2%) |
| Cerebrovascular Event | 22 (3.2%) |
| Congestive Heart Failure | 14 (2.0%) |
| Chronic Obstructive Pulmonary Disease | 7 (1.0%) |
| Hospital Length of Stay, in days, mean(± SD) | 8.4 (± 6.2) |
| Number of Medications at Discharge (n=680)*, mean(±SD) | 13.9 (± 4.8) |
Data available for number of discharge medications
Prevalence of Geriatric Syndromes including New-Onset Syndromes
The estimated prevalence (as a percentage of the entire cohort) of each geriatric syndrome is displayed in Table 3 as is whether this prevalence reflected new-onset or a chronic condition. Of the geriatric syndromes we assessed, the most prevalent were falls (39%), incontinence (39%), decreased appetite (37%), and unintentional weight loss (33%). We found a sex difference in the prevalence of geriatric syndromes, with women more likely to endorse depressive symptoms (34.3% vs. 23.5%; chi-square= 10.50, P=0.001), moderate to severe pain (25.7% vs. 17.4%, P=0.003) and a history of falls (42.2% vs. 34.9%, P=0.042), and men more likely to endorse unintentional weight loss (37% vs. 29.9%, P=0.024) and have pressure ulcers (18.5% vs. 12.3%, P=0.042).
Table 3.
Prevalence of Geriatric Syndromes
| Geriatric Syndromes | Overall N = 686 | Male N = 281 | Female N = 405 | Pearson Chi-Sq | P- value* |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Weight Loss one month prior to or during hospital stay | 225 (32.8) | 104 (37) | 121 (29.9) | 5.090 | 0.024* |
| Decreased Appetite | 254 (37.0) | 98 (34.9) | 156 (38.5) | 1.383 | 0.240 |
| Incontinence | 265 (38.6) | 101 (35.9) | 164 (40.5) | 1.596 | 0.206 |
| Bladder | 133 (19.4) | 49 (17.4) | 84 (20.7) | ||
| Bowel | 40 (5.8) | 16 (5.7) | 24 (5.9) | ||
| Both | 92 (13.4) | 36 (12.8) | 56 (13.8) | ||
| New Onset of Incontinence (N: Overall=260; Male=99; Female=161)** | 98 (37.7) | 48 (48.5) | 50 (31.1) | ||
| Depressive Symptoms (GDS = 2 or higher) | 205 (29.9) | 66 (23.5) | 139 (34.3) | 10.499 | 0.001* |
| New Onset of Depressive Symptoms (N: Overall=104; Male=30; Female=74) | 29 (27.9) | 9 (30.0) | 20 (27.0) | ||
| Delirium at Initial Assessment (Positive BCAM) | 56 (8.2) | 27 (9.6) | 29 (7.2) | 1.484 | 0.224 |
| Cognitive Impairment (12 or lower on BIMS) | 175 (25.5) | 79 (28.1) | 96 (23.7) | 2.179 | 0.140 |
| New Onset of Cognitive Impairment (N: Overall=61; Male=30; Female=31) | 7 (11.6) | 2 (6.7) | 5 (16.1) | ||
| Moderate to severe pain at discharge | 153 (22.3) | 153 (17.4) | 105 (25.7) | 8.998 | 0.003* |
| New Onset of Moderate to Severe pain (N: Overall=68; Male n=24; Female=44) | 28 (41.2) | 11 (45.8) | 17 (38.6) | ||
| Pressure Ulcers | 102 (14.9) | 52 (18.5) | 50 (12.3) | 4.137 | 0.042* |
| Falls (Presence of fall history in the last 3 months) | 269 (39.2) | 98 (34.9) | 171 (42.2) | 3.962 | 0.047* |
Pearson’s Chi-square, GDS= Geriatric Depression Scale, BCAM= Brief Cognitive Assessment Method, BIMS= Brief Interview of Mental Status, New Onset= Within the few weeks before hospital admission or during their hospital stay.
Number of participants (N) for new onset of geriatric syndromes refers to the number of individuals asked this specific question related to the timing of onset and the prevalence of new onset in those individual participants. These questions were added to the quality improvement protocol as the study evolved and therefore the data is not available for all individuals.
In addition, we found that a proportion of these syndromes reflected new onset in close association with the onset of the acute medical cause for hospital admission (as a percent of individuals with that syndrome) including incontinence (37.7%), moderate or severe pain (41.2%), cognitive impairment (11.6%), and depressive symptoms (27.9%) (Table 3).
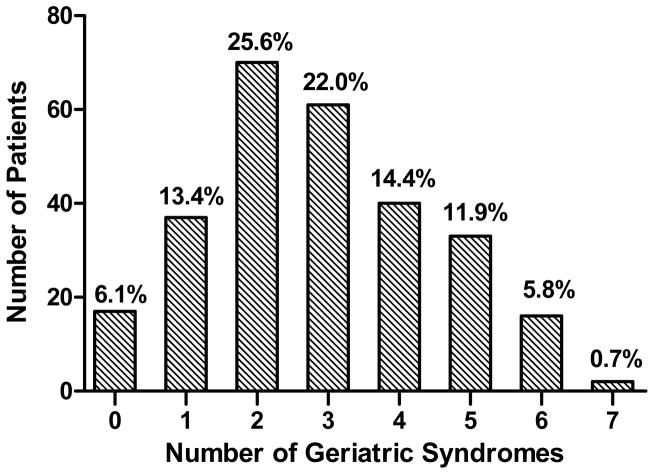
Clusters of Geriatric Syndromes
Figure 1 displays the number of geriatric syndromes present for participants who had complete data for all seven of the geriatric syndromes assessed via patient interview and the two syndromes assessed via medical record documentation (n=277). Of these 277 participants, 152 (55%) met criteria for three or more geriatric syndromes. Table 3 displays the most frequent (top 10) clusters of geriatric syndromes among participants with three or more. Weight loss and decreased appetite were the most common syndromes, occurring in 9 of the top 10 clusters. Depressive symptoms occurred in 6 of the top 10 clusters, incontinence in 5 and falls in 4 clusters.
Figure 1.
Prevalence of number of geriatric syndromes (from maximum of 9 possible) amongst hospitalized older adults transferred to partner skilled nursing facilities
Communication with SNF Providers during the Transition from Acute Care
The hospital discharge documents sent to SNF providers were reviewed for 54 patients during July 2014, and information about one or more geriatric syndromes was absent from each of the 54 discharge packets. The number of discharge packets that were missing documentation of geriatric syndromes, as assessed by research personnel assessments, was high overall and varied by syndrome ranging from 33% (falls) to 80–95% (weight loss, decreased appetite, incontinence, delirium and moderate to severe pain). For example, 24 patients reported bowel incontinence and 36 patients reported bladder incontinence according to research personnel assessments, but only 3 and 4 discharge packets, respectively, had any documentation about bowel and bladder incontinence, respectively. The syndromes that were most frequently documented in discharge documentation were falls and pressure ulcers.
DISCUSSION
The majority of Medicare beneficiaries discharged to SNF had three or more geriatric syndromes, and for many patients, these syndromes were of recent onset. For participants with three or more syndromes, the most common clusters included nutritional syndromes, (e.g., recent unintentional weight loss and/or reduced appetite), depression and incontinence. Despite the high prevalence of multiple syndromes per patient, this information was seldom communicated to SNF providers, with the exception of the two conditions that were the focus of hospital quality improvement efforts (i.e., falls and pressure ulcers).
This study identifies the prevalence, recent onset, recognition, and clusters of geriatric syndromes in hospital patients being discharged to SNF. This data represent a conservative assessment of prevalence in this population because we assumed the syndrome to be absent in cases of incomplete assessment. The true prevalence is likely to be higher, especially with regard to syndromes that may fluctuate in their presence (e.g. delirium). These results have at least three important clinical implications.
First, the identification of geriatric syndrome prevalence and clusters may lead to an understanding of common phenotypes, which could provide a novel strategy for screening older hospitalized patients during the hospital admission. For example, if a patient screens positive for nutritional problems (i.e., recent weight loss or decrease in appetite), care providers also should screen for incontinence and depressive symptoms because these conditions are often associated with nutritional issues.
Second, the fact that many of the syndromes were exacerbated or newly developed around the point of hospitalization underscores the need to detect syndrome clusters and begin the process of planning interventions before hospital discharge. Such interventions have the potential to reduce the phenomenon of “post-hospital syndrome”, an acquired condition of vulnerability as a result of the significant stressors imposed by the hospitalization itself rather than the admitting acute illness.10 The possible result suggests that “post-hospital syndrome” may place SNF patients at increased risk of readmission back to the hospital in the following 30 days for a cause frequently unrelated to the primary hospital diagnosis.34 Although intervening early in the hospital stay may be important, a successful intervention may additionally require that care processes extend into the SNF stay. For example, research by others has linked the administration of 10 or greater different medications with a decline in nutritional status, functional ability and an increased risk of cognitive impairment over time.35,36 In our study population, the average number of medications recorded on hospital discharge was 14 suggesting our population may be at risk for these reports adverse outcomes. Interventions to address polypharmacy, such as de-prescribing, would require significant time for tapering protocols and monitoring that is not feasible in the hospital setting but could, ideally, be carried out in both hospital and SNF care settings.
Third, the finding that even the presence of geriatric syndromes is infrequently communicated to the SNF under current practice highlights an area for improvement.12,17,37 For example, an older adult that reports depressive symptoms, unintentional weight loss and reduced appetite may benefit from the communication of this information so that the SNF can initiate active social engagement and supervision in conjunction with mealtimes. This type of mealtime intervention, as well as an aggressive between-meal snack program, has been demonstrated to improve intake.38,39 This intervention could be implemented immediately after SNF admission with timely transition information as opposed to later into the relatively short SNF care period. In addition, the early transmission of this important clinical information should influence SNF discharge planning, which recent reports suggest are problematic.40 Minimally, patients with a recent history of significant weight loss and poor appetite should be provided with home care services, and their primary care provider should be made aware of these problems at SNF discharge.
Finally, it should be noted that few interventions have been demonstrated to improve the most common syndromes documented in this study, even if each syndrome occurs in isolation. In general, the dearth of efficacious interventions for improving individual geriatric syndromes may be due, in part, to a failure to consider other associated syndromes that are frequently present concurrently and which may share a common contributing factor.1,2,41 An intervention that targets multiple geriatric syndromes (i.e., the most common cluster) and/or a factor common to multiple syndromes (e.g., polypharmacy) may be a more feasible, effective approach.1,2,41
There are several strengths and limitations of this study. First, these data were collected as part of a larger quality improvement project that included all hospitalized Medicare patients who transferred to partner SNFs. The strengths of this approach are that it allowed inclusion of all patients who may not traditionally be enrolled in a study involving more stringent enrollment criteria and written consent. We believe that this provides greater generalizability of our findings and allows us to document the challenges in measuring geriatric syndromes via patient interviews when there are minimal subject exclusion criteria. The fact that we did not exclude cognitively-impaired patients represents a strength of this study but also increased the number of patients who could not complete assessments (e.g., did not know how much weight they had lost or could not understand all of the questions). A future direction would be to gather at least some of this information more efficiently from family surrogates. Another strategy might be to focus the patient interview-based assessments on the most common cluster of three syndromes to reduce both staff time and patient response burden. In addition, the source of falls and pressure ulcer assessment is performed by clinical personnel, and although complete, may not be performed in exactly the same manner across all patients. However, since under-reporting appears to provide a more significant problem (in regard to the other reported syndromes) it is possible that the overall burden of falls and pressure ulcers represented in our population is also higher than our estimates.
A limitation of the study relates to the cross-sectional nature of the data reported; hence, we do not report the persistence of geriatric syndromes following hospital or SNF discharge or the effect of these conditions on other adverse outcomes (e.g., functional decline, hospital readmissions). It is possible that many of the geriatric syndromes documented as new onset or worsening in the hospital may be transient, but there are sparse data about the trajectory of geriatric syndromes over time for this patient population. One study showed that depressive symptoms among hospitalized patients discharged home changed over time but that depression levels remained higher than pre-hospital admission.42 If the stability and clinical importance of geriatric syndromes are to be investigated further, it will be necessary to start the assessment process in the hospital and continue monitoring at SNF discharge. This type of monitoring will require improvements in the quality of the information provided during these care transitions (hospital to SNF to home/Primary Care Provider) relative to current practices.
In summary, this study describes the prevalence of nine geriatric syndromes in hospitalized older adults discharged to SNF and, despite high prevalence as well as clustering of the syndromes; this information was rarely communicated to SNF providers or the focus of interventions in the hospital. This study also documents one reason that SNF patients are at high risk for decline (multiple geriatric syndromes) and provides specific directions for improvement in hospital care transitions and how a new generation of interventions will need to be developed to address these issues.
Table 4.
Top 10 Clusters of Geriatric Syndromes in Hospitalized Patients Transferred to Skilled Nursing Facility
| All | Number of Patients | Prevalence in patients with ≥3 syndromes (N=152) | Overall* Prevalence (N=277) |
|---|---|---|---|
| Weight Loss, Loss of Appetite, Incontinence | 35 | 23% | 13% |
| Weight Loss, Loss of Appetite, Depressive Symptoms | 32 | 21% | 12% |
| Weight Loss, Depressive Symptoms, Incontinence | 30 | 20% | 11% |
| Loss of Appetite, Depressive Symptoms, Incontinence | 27 | 18% | 10% |
| Weight Loss, Depressive Symptoms, Falls | 25 | 16% | 9% |
| Weight Loss, Incontinence, Fall | 25 | 16% | 9% |
| Weight Loss, Loss of Appetite, Fall | 25 | 16% | 9% |
| Depressive Symptoms, Incontinence, Falls | 24 | 16% | 9% |
| Weight Loss, Loss of Appetite, Pain | 23 | 15% | 8% |
| Loss of Appetite, Depressive Symptoms, Pain | 22 | 14% | 8% |
|
| |||
| Men | (N=63) | (N=117) | |
|
| |||
| Weight Loss, Loss of Appetite, Depressive Symptoms | 13 | 23% | 11% |
| Weight Loss, Depressive Symptoms, Incontinence | 12 | 21% | 10% |
| Weight Loss, Loss of Appetite, Incontinence | 12 | 21% | 10% |
| Weight Loss, Loss of Appetite, Pain | 11 | 20% | 9% |
| Weight Loss, Incontinence, Falls | 10 | 18% | 9% |
| Weight Loss, Loss of Appetite, Pressure Ulcers | 10 | 18% | 9% |
| Loss of Appetite, Depressive Symptoms, Incontinence | 9 | 16% | 8% |
| Weight Loss, Loss of Appetite, Falls | 9 | 16% | 8% |
| Depressive Symptoms, Incontinence, Cognitive Impairment | 8 | 14% | 7% |
| Weight Loss, Depressive Symptoms, Falls | 8 | 14% | 7% |
|
| |||
| Women | (N=89) | (N=160) | |
|
| |||
| Weight Loss, Loss of Appetite, Incontinence | 23 | 29% | 14% |
| Weight Loss, Loss of Appetite, Depressive Symptoms | 19 | 24% | 12% |
| Loss of Appetite, Depressive Symptoms, Incontinence | 18 | 23% | 11% |
| Weight Loss, Depressive Symptoms, Incontinence | 18 | 23% | 11% |
| Depressive Symptoms, Incontinence, Falls | 17 | 22% | 11% |
| Loss of Appetite, Depressive Symptoms, Falls | 17 | 22% | 11% |
| Weight Loss, Depressive Symptoms, Falls | 17 | 22% | 11% |
| Loss of Appetite, Incontinence, Falls | 16 | 20% | 10% |
| Weight Loss, Loss of Appetite, Falls | 16 | 20% | 10% |
| Depressive Symptoms, Incontinence, Pain | 15 | 19% | 9% |
Prevalence reported only for patients with complete data for all assessments
Acknowledgments
Funding Sources
This publication was made possible by Grant Number 1C1CMS331006-01-00 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services. Dr. Bell is funded by National Institutes of Health NICHD- K award 2K12HD043483-11 and the Eisenstein’s Women’s Heart Fund. Dr. Mixon is a VA HSR&D Career Development awardee at the Nashville VA. Dr. Vasilevskis is supported by NIH/NIA under Award Number K23AG040157 and the Veterans Affairs Geriatric Research, Education and Clinical Center (GRECC).
The authors would like to thank Emily A. Long, Amy Boegel, Kathy Kaelin Valdez, Carole Bartoo, Christopher Simon Coelho, Linda Beuscher, Lisa Brooks and Jane Gilliam for their contributions to the project.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author contributions:
Study Design and Concept: All authors
Acquisition of Subjects and/or data: Bell, Vasilevskis, Saraf, Jacobsen, Schnelle and Simmons
Analysis and Interpretation of data: Bell, Vasilevskis, Saraf, Jacobsen, Schnelle and Simmons
Preparation of Manuscript: All authors
Sponsor’s Role: The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Veterans Affairs, the National Institutes of Health, and the U.S. Department of Health and Human Services or any of its agencies.
References
- 1.Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: Clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55:780–791. doi: 10.1111/j.1532-5415.2007.01156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 3.Anpalahan M, Gibson SJ. Geriatric syndromes as predictors of adverse outcomes of hospitalization. Intern Med J. 2008;38:16–23. doi: 10.1111/j.1445-5994.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee PG, Cigolle C, Blaum C. The co-occurrence of chronic diseases and geriatric syndromes: The health and retirement study. J Am Geriatr Soc. 2009;57:511–516. doi: 10.1111/j.1532-5415.2008.02150.x. [DOI] [PubMed] [Google Scholar]
- 5.Buurman BM, Hoogerduijn JG, de Haan RJ, et al. Geriatric conditions in acutely hospitalized older patients: Prevalence and one-year survival and functional decline. PLoS One. 2011;6:e26951. doi: 10.1371/journal.pone.0026951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McRae PJ, Peel NM, Walker PJ, et al. Geriatric syndromes in individuals admitted to vascular and urology surgical units. J Am Geriatr Soc. 2014;62:1105–1109. doi: 10.1111/jgs.12827. [DOI] [PubMed] [Google Scholar]
- 7.Lakhan P, Jones M, Wilson A, et al. A prospective cohort study of geriatric syndromes among older medical patients admitted to acute care hospitals. J Am Geriatr Soc. 2011;59:2001–2008. doi: 10.1111/j.1532-5415.2011.03663.x. [DOI] [PubMed] [Google Scholar]
- 8.Wang HH, Sheu JT, Shyu YI, et al. Geriatric conditions as predictors of increased number of hospital admissions and hospital bed days over one year: Findings of a nationwide cohort of older adults from Taiwan. Arch Gerontol Geriatr. 2014;59:169–174. doi: 10.1016/j.archger.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Cigolle CT, Langa KM, Kabeto MU, et al. Geriatric conditions and disability: The Health and Retirement Study. Ann Intern Med. 2007;147:156–164. doi: 10.7326/0003-4819-147-3-200708070-00004. [DOI] [PubMed] [Google Scholar]
- 10.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kind AJH, Smith MA. Documentation of Mandated Discharge Summary Components in Transitions from Acute to Subacute Care. In: Henriksen K, Battles JB, Keyes MA, et al., editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 2: Culture and Redesign) Rockville, MD: 2008. [PubMed] [Google Scholar]
- 12.Kind AJ, Thorpe CT, Sattin JA, et al. Provider characteristics, clinical-work processes and their relationship to discharge summary quality for sub-acute care patients. J Gen Intern Med. 2012;27:78–84. doi: 10.1007/s11606-011-1860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wierenga PC, Buurman BM, Parlevliet JL, et al. Association between acute geriatric syndromes and medication-related hospital admissions. Drugs Aging. 2012;29:691–699. doi: 10.2165/11632510-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mor V, Intrator O, Feng Z, et al. The revolving door of rehospitalization from skilled nursing facilities. Health Aff. 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Toles M, Anderson RA, Massing M, et al. Restarting the cycle: Incidence and predictors of first acute care use after nursing home discharge. J Am Geriatr Soc. 2014;62:79–85. doi: 10.1111/jgs.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King BJ, Gilmore-Bykovskyi AL, Roiland RA, et al. The consequences of poor communication during transitions from hospital to skilled nursing facility: A qualitative study. J Am Geriatr Soc. 2013;61:1095–1102. doi: 10.1111/jgs.12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flood KL, Rohlfing A, Le CV, et al. Geriatric syndromes in elderly patients admitted to an inpatient cardiology ward. J Hosp Med. 2007;2:394–400. doi: 10.1002/jhm.234. [DOI] [PubMed] [Google Scholar]
- 19.Mecocci P, von Strauss E, Cherubini A, et al. Cognitive impairment is the major risk factor for development of geriatric syndromes during hospitalization: Results from the GIFA study. Dement Geriatr Cogn Disord. 2005;20:262–269. doi: 10.1159/000087440. [DOI] [PubMed] [Google Scholar]
- 20.Han JH, Wilson A, Shintani A, et al. 76 Validation of the Brief Confusion Assessment Method in Older Emergency Department Patients. Ann Emerg Med. 2012;60:S28–S29. doi: 10.1016/j.annemergmed.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: Validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62:457–465. doi: 10.1016/j.annemergmed.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han JH, Wilson A, Graves AJ, et al. Validation of the Confusion Assessment Method for the Intensive Care Unit in older emergency department patients. Acad Emerg Med. 2014;21:180–187. doi: 10.1111/acem.12309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chodosh J, Edelen MO, Buchanan JL, et al. Nursing home assessment of cognitive impairment: development and testing of a brief instrument of mental status. J Am Geriatr Soc. 2008;56:2069–2075. doi: 10.1111/j.1532-5415.2008.01944.x. [DOI] [PubMed] [Google Scholar]
- 24.Saliba D, Buchanan J, Edelen MO, et al. MDS 3.0: Brief interview for mental status. J Am Med Dir Assoc. 2012;13:611–617. doi: 10.1016/j.jamda.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Hoyl MT, Alessi CA, Harker JO, et al. Development and testing of a five-item version of the Geriatric Depression Scale. J Am Geriatr Soc. 1999;47:873–878. doi: 10.1111/j.1532-5415.1999.tb03848.x. [DOI] [PubMed] [Google Scholar]
- 26.Rinaldi P, Mecocci P, Benedetti C, et al. Validation of the five-item Geriatric Depression Scale in elderly subjects in three different settings. J Am Geriatr Soc. 2003;51:694–698. doi: 10.1034/j.1600-0579.2003.00216.x. [DOI] [PubMed] [Google Scholar]
- 27.Chibnall JT, Tait RC. Pain assessment in cognitively impaired and unimpaired older adults: A comparison of four scales. Pain. 2001;92:173–186. doi: 10.1016/s0304-3959(00)00485-1. [DOI] [PubMed] [Google Scholar]
- 28.Chu L, Schnelle JF, Cadogan MP, et al. Using the Minimum Data Set to select nursing home residents for interview about pain. J Am Geriatr Soc. 2004;52:2057–2061. doi: 10.1111/j.1532-5415.2004.52565.x. [DOI] [PubMed] [Google Scholar]
- 29.Cadogan MP, Schnelle JF, Al-Sammarrai NR, et al. A standardized quality assessment system to evaluate pain detection and management in the nursing home. J Am Med Direct Assoc. 2006;7:S11–19. S0. doi: 10.1016/j.jamda.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 30.Carlsson CM, Gleason CE, Puglielli L, et al. Chapter 65. Dementia Including Alzheimer’s disease. In: Halter JB, Ouslander JG, Tinetti ME, et al., editors. Hazzard’s Geriatric Medicine and Gerontology. 6. New York, NY: McGraw-Hill; 2009. [Accessed February 26, 2015]. http://accessmedicine.mhmedical.com/content.aspx?bookid=371&Sectionid=41587679. [Google Scholar]
- 31.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kronick RG, Bella M, Gilmer T, et al. The faces of Medicaid II: Recognizing the care needs of people with multiple chronic conditions. Center for Health Care Strategies; 2007. Incorporated. [Google Scholar]
- 33.Lochner KA, Cox CS. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Prev Chronic Dis. 2013;10:E61. doi: 10.5888/pcd10.120137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 35.Jyrkka J, Enlund H, Lavikainen P, et al. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol Drug Saf. 2011;20:514–522. doi: 10.1002/pds.2116. [DOI] [PubMed] [Google Scholar]
- 36.Oyarzun-Gonzalez XA, Taylor KC, Myers SR, et al. Cognitive decline and polypharmacy in an elderly population. J Am Geriatr Soc. 2015;63:397–399. doi: 10.1111/jgs.13283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gandara E, Ungar J, Lee J, et al. Discharge documentation of patients discharged to subacute facilities: A three-year quality improvement process across an integrated health care system. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2010;36:243–251. doi: 10.1016/s1553-7250(10)36039-9. [DOI] [PubMed] [Google Scholar]
- 38.Simmons SF, Keeler E, Zhuo X, et al. Prevention of unintentional weight loss in nursing home residents: A controlled trial of feeding assistance. J Am Geriatr Soc. 2008;56:1466–1473. doi: 10.1111/j.1532-5415.2008.01801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simmons SF, Zhuo X, Keeler E. Cost-effectiveness of nutrition interventions in nursing home residents: A pilot intervention. J Nutr Health Aging. 2010;14:367–372. doi: 10.1007/s12603-010-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sollins HL. Inspector general report finds skilled nursing facilities “often” fail to meet care planning and discharge planning requirements. Geriatr Nurs. 2013;34:233–243. doi: 10.1016/j.gerinurse.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 41.Tinetti ME, Gordon C, Sogolow E, et al. Fall-risk evaluation and management: challenges in adopting geriatric care practices. Gerontologist. 2006;46:717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]
- 42.Chen CM, Huang GH, Chen CC. Older patients’ depressive symptoms 6 months after prolonged hospitalization: Course and interrelationships with major associated factors. Arch Gerontol Geriatr. 2014;58:339–343. doi: 10.1016/j.archger.2013.12.007. [DOI] [PubMed] [Google Scholar]