Abstract
Objective
Cognitive impairment has been associated with late-life suicidal behavior. Without longitudinal data it is unclear whether these are transient features of a depressive state or stable impairments. We examined longitudinally the course of cognitive impairment in older adults with depression and a history of suicide attempt.
Methods
We investigated the persistence of cognitive impairment over time in 198 depressed older adults (age >60); 91 suicide attempters, 39 depressed individuals with suicidal ideation (ideators), and 68 non-suicidal depressed adults assessed over a 2-year period at four time points. We used linear mixed effects modeling to examine group differences in trajectories of cognitive decline over 2 years, using the Mini-Mental State Exam (MMSE), Mattis Dementia Rating Scale (DRS), and Executive Interview (EXIT).
Results
Over the 2-year period, suicide attempters performed significantly worse than both suicide ideators and nonsuicidal depressed older adults on the MMSE (mean difference: from ideators: −0.88, p = 0.02; from nonsuicidal depressed: −1.52, p < 0.01), while on the EXIT and DRS, suicide attempters performed significantly worse than non-suicidal depressed older adults (mean difference: in EXIT: −1.75, p=0.01; in DRS: 3.04, p < 0.01; in MMSE: 1.15, p < 0.01). Cognitive impairment in suicide attempters partly resolved, as indicated by a group*time interaction on the DRS (p= 0.039), but not the EXIT (p= 0.58) or the MMSE (p= 0.08).
Conclusions
Cognitive impairment in late-life suicidal behavior appears to involve both a stable and a state-related component.
Keywords: suicide, cognitive, executive function, depression, aged
INTRODUCTION
In most countries, the suicide rate increases with age (World Health Organization, 2005), as does the lethality of suicidal behavior (Goldsmith SK; Pellmar TC, 2002). There is robust evidence that cognitive impairment is part of the suicidal diathesis. Studies of attempted suicide find impairment on cognitive tasks demanding sustained attention, response inhibition, perseveration, set-shifting, and verbal fluency (Bartfai et al., 1990, Keilp et al., 2008, Keilp et al., 2013, Jollant et al., 2005, Cha et al., 2010, Westheide et al., 2008, Raust et al., 2007, Richard-Devantoy et al., 2012, Richard-Devantoy et al., 2014, Sachs-Ericsson et al., 2014, Ayalon et al., 2007). In a recent meta-analysis of 25 studies examining cognitive impairment associated with suicidal behavior, Richard-Devantoy and colleagues (Richard-Devantoy et al., 2014) found that individuals with a history of suicide attempt demonstrated impaired decision-making, assessed by the IOWA Gambling Task and impaired response inhibition, assessed by the Stroop Color-Word task, relative to non-suicidal individuals with mood disorders and individuals with no psychiatric diagnosis. These findings suggest that impairment in cognitive control and decision competence may predispose suicidal behavior.
While cognitive decline is common in old age, and depression in this age group could be the prodrome of a dementing process (Barnes et al., 2006), very few studies have examined its role in late-life suicidal ideation and behavior. King and colleagues (King et al., 2000) were the first to report on accelerated decline in executive function with age in suicide attempters relative to non-attempters, using the Trail Making Test Part B. Ayalon and colleagues found an association between cognitive impairment and suicidal ideation, using the Short Orientation Memory Concentration Test, in a large sample of older adults (N= 15,590) (Ayalon et al., 2007). More recently, Richard-Devantoy and colleagues (Richard-Devantoy et al., 2012) reported that depressed suicide attempters demonstrated greater impairment in cognitive inhibition compared to non-suicidal depressed and healthy older adult controls.
Our group’s previous studies used a case-control design to cross-sectionally examine whether suicide attempters in late life show greater executive impairment using the Executive Interview (EXIT) relative to older adults seriously contemplating suicide and to those with non-suicidal depression. We found in two partially overlapping samples that both suicide attempters and suicide ideators exhibited greater executive impairment than did non-suicidal individuals with depression (Dombrovski et al., 2008, Gujral et al., 2013). However, several other studies from our group have shown selective impairments in cognitive and decision processes among suicide attempters, relative to ideators and nonsuicidal depressed older adults (Clark et al., 2011, Dombrovski et al., 2010, Dombrovski et al., 2011,).
Cognitive impairments associated with suicidal behavior may be transient features of the suicidal crisis (Baumeister, 1990) or stable impairments (Andersson et al., 2008). To our knowledge, Sachs-Ericsson et al. (Sachs-Ericsson et al., 2014) is the only study that has longitudinally examined differences between older adult depressed suicide attempters and non-attempters over a 2-year follow-up, and they found that suicide attempt history was not associated with cognitive decline over the follow-up period. However, this study included only 23 attempters, and the MMSE was the only cognitive measure assessed over time. More longitudinal data are required to better understand the course of cognitive impairment in suicide attempters. Using repeated cognitive assessments three months after baseline (when substantial clinical improvement would reasonably be anticipated) and then one and two years after initial assessment, the primary aim of this study was to describe the course of cognitive function among three groups of older adults- depressed suicide attempters, depressed suicide ideators, and non-suicidal depressed patients. We tested whether (1) suicide attempters displayed poorer cognitive performance relative to comparison groups and (2) whether cognitive impairments in suicide attempters show any resolution over time.
METHODS
Study Groups
We studied three groups of participants aged 60 and older with current episodes of non-psychotic unipolar major depression. Depression diagnosis was made using the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID/DSMIV; (First et al., 2002)). Participants were 91 depressed suicide attempters, 39 depressed ideators without a history of suicide attempts, and 68 non-suicidal depressed. Participants could not have any neurological disorders (e.g., Parkinson’s disease, multiple sclerosis), delirium, or sensory impairments that may confound the outcomes of neuropsychological testing. None of the participants had an existing clinical diagnosis of dementia. Individuals who had received electroconvulsive therapy in the previous 6 months were excluded from the study because of the possible effects on cognitive functioning. All participants scored at least 18 on the Mini-Mental State Exam (MMSE) during initial recruitment; however, the minimum MMSE score required for participation was later increased to 24 to enable more detailed assessments. Only 15 subjects in the current sample are in the 18–23 MMSE range, and none was diagnosed with dementia at the time of baseline assessments. All participants provided written informed consent. The University of Pittsburgh Institutional Review Board approved the study.
Suicide Attempters (n = 91)
Suicide attempt was defined as a self-injurious act taken with the intent to die. Suicide attempters endorsed either 1) a suicide attempt within a 2-week period prior to study enrollment or 2) a previous suicide attempt with current suicidal ideation with a plan at the time of study enrollment. Suicide attempt history was verified by a psychiatrist (AYD or KSz), using all available information: participant report, medical records, information from the treatment team, and collateral information from family or friends. Significant discrepancies between these sources led to exclusion from the study. Suicidal intent associated with suicide attempts was assessed using the Beck Suicide Intent Scale (SIS), which is scored from 0–30 (Beck et al., 1974). Suicide intent on the SIS was high (mean[SD]): 17.6[4.8]). Current and worst lifetime suicidal ideation were assessed using the Beck Scale of Suicidal Ideation (SSI), which is scored from 0–38 (Beck et al., 1979). Suicide attempters’ mean current suicidal ideation score on the SSI at baseline was also high (21.0 [8.4]) and mean worst suicidal ideation in lifetime score on the SSI was 25.0 (5.6).
Suicide Ideators (n = 39)
Suicide ideators endorsed suicidal ideation with a specific plan but had no lifetime history of suicide attempt. These participants seriously contemplated suicide and communicated this to their family or medical professionals, typically triggering an inpatient admission or an increase in the level of outpatient care. Participants with passive death wish or fleeting suicidal thoughts without a clear plan were excluded from this group. The mean suicidal ideation score on the SSI for past month and worst lifetime for suicide ideators was high: (13.9 [5.0]) and (15.5 [7.5]), respectively.
Non-Suicidal Depressed Participants (n = 68)
A comparison group of non-suicidal depressed older adults was included to determine whether there is an association between suicidality (either ideation, attempt, or both) and impaired cognitive function above and beyond, or different from, the general effect of depression on cognitive function in older adults. These participants had a SCID/DSM-IV diagnosis of current major depressive episode and a score of 14 or higher on the 17-item Hamilton Rating Scale for Depression (HRSD-17) (Hamilton, 1960). Non-suicidal depressed participants had no lifetime history of self-injurious behavior, suicidal ideation, or suicide attempts verified by the clinical interview, review of medical records, SCID/DSM-IV, the SSI (lifetime), and the HRSD-17 suicide item.
Assessments
Clinical Assessments
We assessed depression severity with the 17-item Hamilton Rating Scale for Depression (Hamilton, 1960); comorbid physical illness with the Cumulative Illness Rating Scale adapted for Geriatrics (Miller et al., 1992); and level of hopelessness with the Beck Hopelessness Scale (Beck, 1974). We measured the intensity of pharmacotherapy for the current episode of depression with the Antidepressant Treatment History Form (ATHF) (Sackeim, 2001).
Cognitive Assessments
We administered both the Mini-Mental State Examination (MMSE) and the Dementia Rating Scale (DRS) (Mattis, 1988) to assess global cognitive function. The MMSE is a brief 30-item test that is commonly administered as a screening tool for cognitive impairment (0–30) (Folstein et al., 1983). Scores on the DRS range from 0–144, and it is comprised of subscales assessing Initiation/Perseveration, Attention, Construction, Conceptualization, and Memory. We assessed a spectrum of executive functions with the Executive Interview (EXIT) (Royall et al., 1992) (range 0–50). This is a brief “bedside” screening measure of cognitive control. The 25 items comprising this test are administered in rapid succession with minimal instructions to elicit automatic behaviors and disinhibition and also include modifications of well-known “frontal lobe” tests (number/letter sequencing, Stroop, fluency tests, go/no-go tests, and Luria’s hand sequences). Higher EXIT scores and lower MMSE and DRS scores indicate worse performance.
Procedures
Our study of late-life suicide was conducted on a psychogeriatric inpatient unit and an outpatient research clinic at the University of Pittsburgh. Participants were assessed within two weeks of inpatient admission or at the beginning of treatment as outpatients. Cognitive evaluations were administered by clinicians trained in neuropsychological testing, under the supervision of a Clinical Neuropsychologist (MAB). Patients continued to receive psychotropic medications as clinically indicated. Neuropsychological assessors were blind to clinical history and ratings.
Statistical Analyses
Baseline characteristics of the three groups are summarized using numbers and percentages for categorical variables, and differences across groups were tested using chi-square tests or its exact version as appropriate. Continuous variables are summarized using means and standard deviations (for normally distributed data) or medians and quartiles for skewed data, and differences across groups were tested using the F-test or Wilcoxon/Kruskal Wallis test. Finally, we used linear mixed effect models to examine EXIT, DRS and MMSE scores separately over time. Each model included age, sex, and education as covariates, time and group as predictors, and a group*time interaction term. Results were summarized using regression coefficients and corresponding p-values. The association between the groups and the changes in the scores over time was tested using the F-test of the interaction of time and group in this model. Candidate covariates were sex, age, and education at consent, and were chosen a priori.
An additional sensitivity analysis that accounts for the missing data was conducted using pattern mixture model. This analysis aimed to test the degree to which the suicide groups differ over time by missing patterns. For four time points, there are 24 missing data patterns. However, only 5 missing data pattern categories were included in the model. Some intermittent patterns are combined to form meaningful patterns as they are not easily discernible individually. For example, a missing pattern category was created based on the last available measurement. Combining patterns increases interpretability. Other pattern categories were created based on monotonous missing patterns. Data analysis was carried out using SAS version 9.3 (2000–2004).
RESULTS
As summarized in Table I, the suicide attempters, suicide ideators, and non-suicidal depressed older adults did not differ significantly by age (F(2, 195) = 0.35, p = 0.71), race (Exact Chi-sq , p = 0.73), or sex ( , p = 0.23), but differed by years of education (F(2, 195) = 4.75, p = 0.01; attempters<ideators=depressed). The three groups also differed on baseline HRSD-17 score (F(2, 156) = 15.78, p < 0.001; attempters= ideators < depressed). More years of schooling and younger age were associated with better cognitive function as measured by the EXIT, DRS, and MMSE, independent of group status.
Table 1.
Baseline Demographics and Clinical characteristics of Participants
| Attempters (N=91) | Ideators (N=39) | Depressed (N=68) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | % | Mean | SD | % | Mean | SD | % | Mean | SD | Test statistics | P-value | |
| Sex (Female) | 48.4 | 51.3 | 61.8 |
|
p=0.23 | |||||||
| Race (African-American) | 13.2 | 18.0 | 13.2 |
|
p=0.73 | |||||||
| Age (Years) | 69.9 | 8.5 | 69.5 | 7.9 | 70.8 | 8.4 | F(2,195)=0.35 | p=0.71 | ||||
| Education (Years) | 13.2 | 3.0 | 13.6 | 3.3 | 14.6 | 2.7 | F(2,195)=4.75 | p=0.01 | ||||
| HDRS-16 | 22.2 | 6.3 | 21.7 | 4.9 | 17.2 | 3.9 | F(2,156)=15.78 | p < 0.001 | ||||
We hypothesized that suicide attempters would show persistent cognitive impairment over a 2-year interval, as assessed by performance on the MMSE, EXIT, and DRS, relative to suicide ideators and nonsuicidal depressed older adults. Additionally, we tested whether this cognitive impairment would resolve over time.
MMSE scores differed across groups (p < 0.0001) on average over the 2-year follow-up period, with the suicide attempters having lower MMSE scores relative to both the non-suicidal depressed group (mean difference: −1.52, p < 0.0001) and the suicide ideators (mean difference: −0.88, p = 0.02; Fig. 1). There was a trend towards differential rate of decline across the groups (p= 0.08), such that suicide attempters showed improvement and the non-suicidal depressed older adults showed decline in MMSE scores over the 2-year follow-up. Predicted MMSE scores after covarying for age, sex, and education, are modeled in Figure 1, over the 2-year follow-up period at four time points.
Figure 1. Predicted MMSE scores over the 2-year follow-up period for Suicide Attempters, Suicide Ideators, and Non-suicidal Depressed Older Adults.
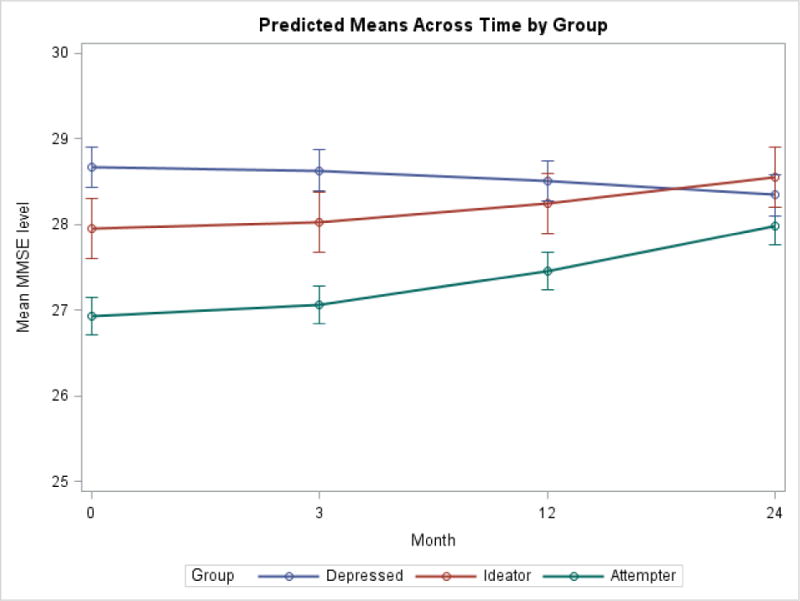
Figure 1 depicts the trajectories of MMSE scores over a 24-month follow-up period for suicide attempters, ideators, and nonsuicidal depressed older adults, and shows that suicide attempters performed significantly worse than both suicide ideators and the nonsuicidal depressed group across the four time points. There was a trend such that suicide attempters showed improvement and the nonsuicidal depressed group showed decline over time, but this failed to reach significance.
*All analyses included age, sex, and education as covariates. Age was coded in years, education was coded as years of education, and sex was coded as 1=male and 2=female.
**MMSE scores of 189 participants at baseline, N=132 with at least 2 data points, N=112 with least 3 data points, and N=81 of participants with 4 data points.
EXIT scores differed across groups (p = 0.035) on average over the 2-year follow-up period, with the suicide attempters having higher EXIT scores (worse executive performance) than the non-suicidal depressed (mean difference: 1.73, p = 0.01). However, there was no significant decline over time (p = 0.72). The rate of decline did not significantly differ across the three groups (p = 0.58). Predicted EXIT scores after covarying for age, sex, and education, are presented in Figure 2, over the 2-year follow-up period at four time points.
Figure 2. Predicted EXIT scores over the 2-year follow-up period for Suicide Attempters, Suicide Ideators, and Non-suicidal Depressed Older Adults.
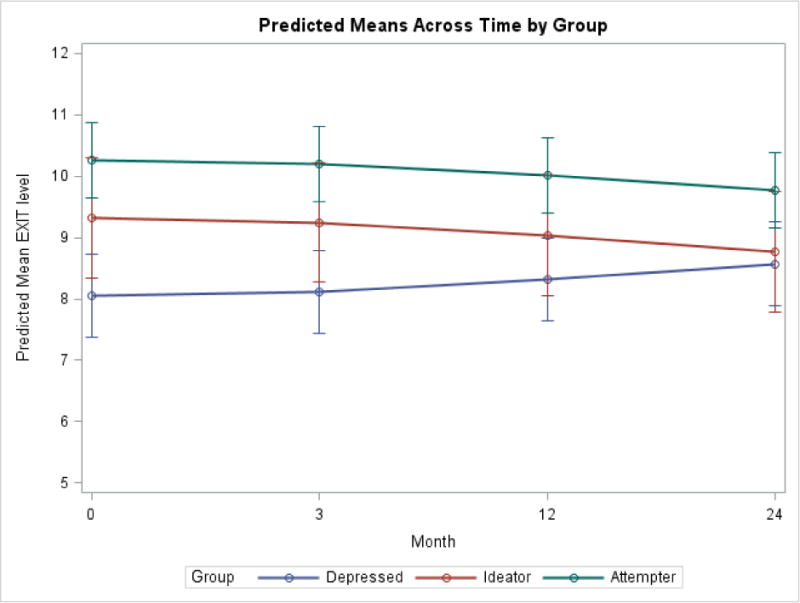
Figure 2 depicts the trajectories of EXIT scores over a 24-month follow-up period for suicide attempters, ideators, and nonsuicidal depressed older adults, with higher EXIT scores reflecting worse performance. Suicide attempters performed significantly worse on that EXIT than the nonsuicidal depressed group across the four time points. There was no evidence of decline in executive performance over the four time points across the groups.
*All analyses included age, sex, and education as covariates. Age was coded in years, education was coded as years of education, and sex was coded as 1=male and 2=female.
**EXIT scores of 199 participants at baseline, N=147 with at least 2 data points, N=103 with least 3 data points, and N=74 of participants with 4 data points.
DRS scores also differed across groups (p = 0.005) on average over the 2-year follow-up period, with the suicide attempters having lower DRS scores (worse performance) compared to the non-suicidal depressed older adults (mean difference: −3.03, p = 0.003). There was no significant decline in DRS scores over time (p = 0.19). However, the rate of change was different across the three groups (p = 0.039). Figure 3 and regression coefficients (Table 4) reveal that this difference was explained by a non-significant decline in the non-suicidal depressed group (p = 0.052) and the non-significant improvement in suicide ideators and attempters. Predicted DRS scores after covarying for age, sex, and education, are presented in Figure 3 over the 2-year follow-up period at four time points.
Figure 3. Predicted DRS scores over the 2-year follow-up period for Suicide Attempters, Suicide Ideators, and Non-suicidal Depressed Older Adults.
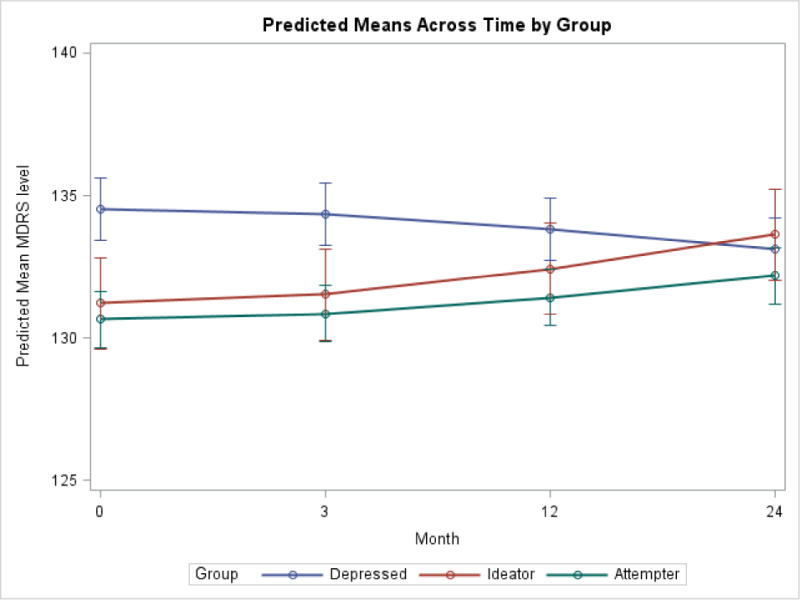
Figure 3 depicts the trajectories of DRS scores over a 24-month follow-up period for suicide attempters, ideators, and nonsuicidal depressed older adults, and shows that suicide attempters performed significantly worse on the DRS than the nonsuicidal depressed group across the four time points. The rate of change in performance on the DRS differed across three groups, such that the nonsuicidal group showed a trend toward decline in performance, and the suicide attempters and ideators showed a trend towards improvement in performance; however, the trajectory of change in DRS performance for each group failed to reach significance.
*All analyses included age, sex, and education as covariates. Age was coded in years, education was coded as years of education, and sex was coded as 1=male and 2=female.
**DRS scores of 210 participants at baseline, N=157 with at least 2 data points, N=105 with least 3 data points, and N=70 of participants with 4 data points.
Table 4.
Group Differences between Suicide Attempters, Ideators, and Nonsuicidal Depressed Older Adults in DRS performance over 2-year follow-up period, covarying for age, sex, and education.
| Parameters | Estimate | SE | DF | P |
|---|---|---|---|---|
| Intercept | 157.9 | 3.81 | 185 | <.0001 |
| Group | 0.0052 | |||
| Depressed vs. Attempter | 3.03 | 0.99 | 163 | 0.0028 |
| Ideator vs. Attempter | −0.057 | 1.13 | 163 | 0.96 |
| Time | 0.19 | |||
| Time × Group | 0.039 | |||
| Time × Attempter | 0.063 | 0.044 | 142 | 0.15 |
| Time × Depressed | −0.12 | 0.062 | 163 | 0.052 |
| Time × Ideator | 0.037 | 0.066 | 163 | 0.58 |
| Education | 0.73 | 0.14 | 163 | <.0001 |
| Sex | −1.44 | 0.81 | 163 | 0.076 |
| Age at consent | −0.52 | 0.048 | 163 | <.0001 |
In two sensitivity analyses, we ascertained that these group differences were not explained by change in depressive severity (including depression scores as a time-varying covariate) or potential differential dropout. First, we found that EXIT performance was not influenced by changes in severity of depression, as assessed by the HRSD-17 (p = 0.77), while DRS performance did covary with depressive severity over the 2-year follow-up period (p = 0.0001), independent of group status. However, the above-mentioned group differences in cognitive function, as measured by the EXIT and DRS, over the 2-year follow-up period, remained robust after covarying for severity of depression, as measured by the HRSD-17 (EXIT: p= 0.004, DRS: p = 0.001). In a second sensitivity analysis using a pattern mixture model, we tested whether there group differences over time in performance on the MMSE, EXIT, and DRS, differed as a function of differential dropout rates among the three groups, and found the interaction between group and patterns of dropout was not statistically significant (p < 0.05).
Given that we combined both remote and recent attempters into one group in our analyses, we conducted two more sensitivity analyses examining whether recent and remote attempters differed in cognitive performance at baseline, and whether inpatient status affected cognitive performance at baseline. We examined differences between recent and remote attempters using separate ANCOVAs for MMSE, EXIT, and DRS performance at baseline, covarying for age, gender, and education. We found that the recent attempters performed worse than the distal attempters on the MMSE at baseline (mean difference = −1.25, p=0.01). We found no differences between recent and remote attempters on EXIT and DRS performance at baseline (EXIT: mean difference = 1.61, p= 0.09; DRS: mean difference = −2.09, p=0.15). We then examined whether inpatient status at baseline was associated with worse cognitive performance in attempters and ideators. We found that inpatient status was not significantly associated with cognitive performance on the EXIT, DRS, or MMSE in suicide attempters and ideators (EXIT: F= 1.99, p=0.14; DRS: F= 1.70, p=0.19; MMSE: F= 0.26, p=0.77).
DISCUSSION
We examined the 2-year course of cognitive impairment in suicide attempters and ideators. First, we saw that, over this period, suicide attempters and ideators displayed lower levels of executive (EXIT) and global cognitive functioning (DRS and MMSE). Our findings with respect to resolution vs. stability of impairment in suicide attempters were not entirely conclusive. On the MMSE, the trend toward faster resolution of impairment in suicide attempters vs. non-suicidal depressed did not reach statistical significance. On the DRS, impairment partly resolved in suicide attempters relative to controls. We failed to find evidence of faster deficit resolution on the EXIT. Given that the DRS is the broadest and most sensitive of the three measures, a strong interpretation of our findings is that cognitive impairment in late-life suicide include both a stable and a state component.
There are few studies to date that examine the relationship between cognition and suicide. Our cross-sectional studies have suggested that older suicide attempters show impairment in executive functioning, as well as decision-making (Dombrovski et al., 2008, Dombrovski et al., 2010, McGirr et al., 2012, Gujral et al., 2013). Other studies that have examined cognitive markers of late-life suicide (King et al., 2000, Richard-Devantoy et al., 2014, Richard-Devantoy et al., 2012) have relied on small samples (N < 50) and specific tests of attentional control and response inhibition. To our knowledge, Sachs-Ericsson et al. (Sachs-Ericsson et al., 2014) is the only prior study that has longitudinally examined differences between older adult depressed suicide attempters and non-attempters over a 2-year follow-up. Although they failed to detect an association between suicide attempt history and cognitive decline, the small sample size (N=23) and insensitive measure of cognitive decline (MMSE) used in this study may help explain the null finding. Little is known about the etiology of cognitive impairment in suicidal behavior. Given that cognitive impairments have been found in both euthymic and depressed suicide attempters across the lifespan (King et al., 2000, Keilp et al., 2008, Keilp et al., 2013, Jollant et al., 2005, Richard-Devantoy et al., 2012, Gujral et al., 2013, Sachs-Ericsson et al., 2014), it is most likely a life-long vulnerability factor that accentuates with cognitive aging.
The inclusion of a suicide ideator control group in this study permitted an examination of correlates of suicidal behavior above and beyond suicidal ideation. However, suicide ideators’ executive (EXIT) and global cognitive (DRS) performance was intermediate between that of attempters and non-suicidal depressed, not differing significantly from that of attempters. One exception was the MMSE, were we found step-wise impairment. We have found no differences in stability of cognitive impairment between suicide attempters and ideators. We take a conservative view of these results, concluding that cognitive impairment appear to mostly operate at the stage of contemplation rather than the final decision to take one’s life. While a dose-response relationship between severity of cognitive impairment and seriousness of suicidal ideation – and hence probability of suicide attempt – is plausible, our study may have possessed only marginal power to detect it.
Limitations
A key limitation of our study is the case–control design, which precludes causal inferences. Second, the dropout rate was relatively large, reflecting the fact that many participants were very ill and had chaotic lives. Third, an observation period of 2 years was insufficient to detect cognitive decline caused by dementia. Further, our suicide ideator group was limited to those having suicidal ideation with a specific plan and may not be representative of depressed older adults with less serious suicidal ideation. However, the lack of a correlation between severity of suicidal ideation and performance on the EXIT in our study argues against the possibility that severity of suicidal ideation is associated with the level of executive impairment in suicidal older adults. Still, future studies need to examine whether executive function impairment in older adults are specifically related to the emergence of a suicidal plan. No inferences can be drawn here about suicidal older adults with dementia. Yet, the relatively low MMSE and DRS scores show that some of our participants were moderately cognitively impaired.
Finally, while the overall pattern of cognitive performance was similar across the measures, showing that attempters had significant impairment compared to non-suicidal depressed older adults, the degree of divergence between attempters and ideators as well as group*time effects varied among the three measures. The lack of deficit resolution on the EXIT vs. the DRS may indicate the relative stability of executive impairment. Poorer performance of suicide attempters vs. ideators on the MMSE but not the DRS is harder to interpret. We suspect that it may have reflected greater confusion in suicide attempters captured by the six orientation items of the MMSE, as recent suicide attempters had significantly worse performance on the MMSE than those with a remote (more than one month prior to assessment) attempt. The MMSE was included in the analyses because this widely used screening tool will allow for comparison with other studies.
In conclusion, we found that depressed older adults with a history of suicide attempt display stable cognitive impairment over a 2-year follow-up period relative to non-suicidal depressed older adults. We found no evidence of accelerated cognitive decline among elderly suicide attempters. While cognitive function did not co-vary with depression severity in our study, the existence of a state-related component that may resolve over time cannot be ruled out.
Table 2.
Group Differences between Suicide Attempters, Ideators, and Nonsuicidal Depressed Older Adults in MMSE performance over 2-year follow-up period, covarying for age, sex, and education.
| Parameters | Estimate | SE | DF | P |
|---|---|---|---|---|
| Intercept | 31.29 | 1.22 | 152 | <.0001 |
| Group | <.0001 | |||
| Depressed vs. Attempter | 1.52 | 0.33 | 172 | <.0001 |
| Ideator vs. Attempter | 0.88 | 0.38 | 172 | 0.021 |
| Time | 0.19 | |||
| Time × Group | 0.083 | |||
| Time × Attempter | 0.044 | 0.013 | 114 | 0.001 |
| Time × Depressed | −0.057 | 0.02 | 172 | 0.001 |
| Time × Ideator | −0.019 | 0.020 | 172 | 0.34 |
| Education | 0.20 | 0.043 | 172 | <.0001 |
| Sex | 0.002 | 0.26 | 172 | 0.99 |
| Age at consent | −0.10 | 0.015 | 172 | <.0001 |
Table 3.
Group Differences between Suicide Attempters, Ideators, and Nonsuicidal Depressed Older Adults in EXIT performance over 2-year follow-up period, covarying for age, sex, and education.
| Parameters | Estimate | SE | DF | P |
|---|---|---|---|---|
| Intercept | −6.25 | 2.52 | 182 | 0.014 |
| Group | 0.035 | |||
| Depressed vs. Attempter | −1.73 | 0.67 | 163 | 0.010 |
| Ideator vs. Attempter | −0.56 | 0.75 | 163 | 0.45 |
| Time | 0.72 | |||
| Time × Group | 0.58 | |||
| Time × Attempters | −0.020 | 0.037 | 135 | 0.58 |
| Time × Depressed | 0.042 | 0.05 | 163 | 0.40 |
| Time × Ideator | −0.003 | 0.053 | 163 | 0.96 |
| Education | −0.45 | 0.091 | 163 | <.0001 |
| Sex | −0.55 | 0.54 | 163 | 0.31 |
| Age at consent | 0.32 | 0.032 | 163 | <.0001 |
Acknowledgments
NIMH grants R01MH085651-03, R01MH085651-05, and American Foundation for Suicide Prevention Investigator grant to Katalin Szanto, as well as R01 MH05436, K23 MH086620, AG033575, National Science Foundation Graduate Research Fellowship Program under Grant No. 2014192810, and the UPMC Endowment in Geriatric Psychiatry.
Dr. Karp has received medication supplies from Pfizer and Reckitt Benckiser for investigator initiated studies.
References
- SAS 9.3 ed. Cary, NC: SAS Institute Inc; 2000–2004. [Google Scholar]
- Anderson L, Allebeck P, Gustaffson JE, Gunnell D. Association of IQ scores and school achievement with suicide in a 40-year follow-up of a Swedish cohort. Acta Psychiatr Scand. 2008;118:99–105. doi: 10.1111/j.1600-0447.2008.01171.x. [DOI] [PubMed] [Google Scholar]
- Ayalon L, Mackin S, Arean PA, Chen H, McDonel Herr EC. The role of cognitive functioning and distress in suicidal ideation in older adults. J Am Geriatr Soc. 2007;55:1090–4. doi: 10.1111/j.1532-5415.2007.01237.x. [DOI] [PubMed] [Google Scholar]
- Bartfai A, Winborg IM, Nordstrom P, Asberg M. Suicidal behavior and cognitive flexibility: design and verbal fluency after attempted suicide. Suicide Life Threat Behav. 1990;20:254–66. [PubMed] [Google Scholar]
- Baumeister RF. Suicide as escape from self. Psychol Rev. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. [DOI] [PubMed] [Google Scholar]
- Barnes DE, Alexopoulos GS, Lopez OL, Williamson JD, Yaffe K. Depressive symptoms, vascular disease, and mild cognitive impairment: findings from the Cardiovascular Health Study. Arch Gen Psychiatry. 2006;63:273–279. doi: 10.1001/archpsyc.63.3.273. [DOI] [PubMed] [Google Scholar]
- Beck A, Weissman A, Lester D, Trexler L. The measurement of pessimism: The Hopelessness Scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kvoacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–52. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck AT, Shuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HLP, Lettieri DJ, editors. The prediction of Suicide. Charles Press; Bowie: 1974. [Google Scholar]
- Cha CB, Najmi S, Park JM, Finn CT, Nock MK. Attentional bias toward suicide-related stimuli predicts suicidal behavior. J Abnorm Psychol. 2010;119:616–22. doi: 10.1037/a0019710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark L, Dombrovski AY, Siegle GJ, Butters MA, Shollenberger CL, Sahkian BJ, Szanto K. Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychology and Aging. 2011;26:321–330. doi: 10.1037/a0021646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Butters MA, Reynolds CF, III, et al. Cognitive Performance in Suicidal Depressed Elderly: Preliminary Report. Am J Geriatr Psychiatry. 2008;16:109–115. doi: 10.1097/JGP.0b013e3180f6338d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Clark L, Siegle GJ, et al. Reward/Punishment reversal learning in older suicide attempters. Am J Psychiatry. 2010;167:699–707. doi: 10.1176/appi.ajp.2009.09030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Siegle GJ, Wallace ML, Forman SD, Sahkian BJ, Reynolds CF, III, Clark L. Lethal Forethought: Delayed Reward Discounting Differentiates High- and Low-Lethality Suicide Attempts in Old Age. Biological Psychiatry. 2011;70:138–144. doi: 10.1016/j.biopsych.2010.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlagsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry. 2008;16:220–8. doi: 10.1097/JGP.0b013e3181602a12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition. Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Folstein MF, Robins LN, Helzer JE. The Mini-Mental State Examination. Arch Gen Psychiatry. 1983;40:812. doi: 10.1001/archpsyc.1983.01790060110016. [DOI] [PubMed] [Google Scholar]
- Goldsmith SK, Pellmar TC, K A, Bunney WE, editors. Reducing Suicide: A National Imperative. National Acadamies Press; Washington, D.C.: 2002. [PubMed] [Google Scholar]
- Gujral S, Dombrovski AY, Butters M, et al. Impaired Executive Function in Contemplated and Attempted Suicide in Late Life. Am J Geriatr Psychiatry. 2013;22:811–819. doi: 10.1016/j.jagp.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haw C, Harwood D, Hawton K. Dementia and suicidal behavior: a review of the literature. Int Psychogeriatr. 2009;21:440–53. doi: 10.1017/S1041610209009065. [DOI] [PubMed] [Google Scholar]
- Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. American Journal of Psychiatry. 2005;162:304–10. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Gorlyn M, Oquendo MA, Burke AK, Mann JJ. Attention deficit in depressed suicide attempters. Psychiatry Research. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keilp JG, Gorlyn M, Russell M, et al. Neuropsychological function and suicidal behavior: attention control, memory and executive dysfunction in suicide attempt. Psychol Med. 2013;43:539–51. doi: 10.1017/S0033291712001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DA, Conwell Y, Cox C, et al. A neuropsychological comparison of depressed suicide attempters and nonattempters. Journal of Neuropsychiatry & Clinical Neurosciences. 2000;12:64–70. doi: 10.1176/jnp.12.1.64. [DOI] [PubMed] [Google Scholar]
- Mattis S. Dementia Rating Scale (DRS) Psychological Assessment Resources; Odessa: 1988. [Google Scholar]
- McGirr A, Dombrovski AY, Butters MA, Clark L, Szanto K. Deterministic learning and attempted suicide among older depressed individuals: cognitive assessment using the Wisconsin Card Sorting Task. J Psychiatr Res. 2012;46:226–32. doi: 10.1016/j.jpsychires.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–48. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Raust A, Slama F, Mathieu F, et al. Prefrontal cortex dysfunction in patients with suicidal behavior. Psychol Med. 2007;37:411–9. doi: 10.1017/S0033291706009111. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim MT, Jollant F. A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychol Med. 2014;44:1663–73. doi: 10.1017/S0033291713002304. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Jollant F, Kefi Z, et al. Deficit of cognitive inhibition in depressed elderly: a neurocognitive marker of suicidal risk. J Affect Disord. 2012;140:193–9. doi: 10.1016/j.jad.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the executive interview. J Am Geriatr Soc. 1992;40:1221–6. doi: 10.1111/j.1532-5415.1992.tb03646.x. [DOI] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Hames JL, Joiner TE, et al. Differences between suicide attempters and nonattempters in depressed older patients: depression severity, white-matter lesions, and cognitive functioning. Am J Geriatr Psychiatry. 2014;22:75–85. doi: 10.1016/j.jagp.2013.01.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sackeim HA. The definition and meaning of treatment-resistant depression. J Clin Psychiatry. 2001;62:10–17. [PubMed] [Google Scholar]
- Seyfried LS, Kales HC, Ignacio RV, Conwell Y, Valenstein M. Predictors of suicide in patients with dementia. Alzheimers Dement. 2011;7:567–73. doi: 10.1016/j.jalz.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westheide J, Quednow BB, Kuhn KU, et al. Executive performance of depressed suicide attempters: the role of suicidal ideation. Eur Arch Psychiatry Clin Neurosci. 2008;258:414–421. doi: 10.1007/s00406-008-0811-1. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Suicide prevention [Online] 2005 Available: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/


