Abstract
This study evaluated how clinicians assess antiretroviral (ARV) adherence in clinical encounters, and which questions elicit accurate responses. We conducted conversation analysis of audio-recorded encounters between 34 providers and 58 patients reporting ARV non-adherence in post-encounter interviews. Among 42 visits where adherence status was unknown by providers, 4 providers did not discuss ARVs (10%), 6 discussed ARVs but did not elicit non-adherence disclosure (14%), and 32 discussed ARVs with disclosure (76%). Questions were classified as: 1) clarification of medication (“Are you still taking the Combivir?”); 2) broad (“How’s it going with your meds?”); 3) positively-framed (“Are you taking your medications regularly?”); 4) negatively-framed (“Have you missed any doses?”). Clinicians asked 75 ARV-related questions: 23 clarification, 12 broad, 17 positively-framed, and 23 negatively-framed. Negatively-framed questions were 3.8 times more likely to elicit accurate disclosure than all other question types (p<0.0001). Providers can improve disclosure probability by asking directly about missed doses.
Keywords: HIV/AIDS, antiretrovirals, adherence, physician-patient communication
INTRODUCTION
Medication adherence is critically important for the successful treatment of patients with HIV. However, previous studies have found that 19% to 53% of HIV patients are not adherent with their antiretroviral medications (ARVs) (1–3). At the same time, it is well-documented that physicians’ estimates of patient ARV adherence are highly inaccurate, with physicians routinely failing to detect poor adherence and missing counseling opportunities (4–6). Despite these phenomena, there is a dearth of research exploring how providers elicit information about medication adherence in the clinical interview.
In the context of hypertension, Steele et al identified the need for research regarding medication adherence dialogue in 1990 stating that “the issue is not simply whether the clinician asks about adherence but how” (7). Steele’s study found that providers only accurately identified 53% of adherence problems to antihypertensive medications, and that physicians were most successful when they used an “information-intensive approach,” which elicited disclosures 80% of the time (7). However, this study did not analyze the questions asked by providers in detail, but rather classified the dialogue into three broad categories: “indirect,” “simple direct” and “information intensive.” Bokhour et al developed a different schema and concluded that open-ended questioning, collaborative style, and use of lay language elicit more discussion about antihypertensive medications (8).
Two previous studies have examined medication adherence dialogue in HIV care, but neither assessed the correlation between the type of dialogue and the rates of accurate patient disclosure elicited (9, 10). One study interviewed 12 physicians who reported a wide range of strategies for asking about ARV adherence, with some asking broad questions, others asking direct questions about missed doses, and still others relying on patients to report unprompted (10). This study did not observe patient-provider encounters. A more recent study of 34 physicians did observe clinical encounters and found that very few physicians asked about ARV adherence in depth, with some failing to ask at all (9).
Our study looks critically at audio-recorded dialogue regarding ARV medications between providers and non-adherent patients, with the novel goal of analyzing the questions asked by providers and assessing the likelihood that different question types elicit patient disclosures of non-adherence. The overall objective of this study is to inform HIV providers regarding the most effective ways to ask about ARV adherence.
METHODS
Study Design, Subjects, and Setting
The data for this study were collected as part of the Enhancing Communication and HIV Outcomes (ECHO) Study, which included 45 providers and 434 HIV-positive patients in four sites: Baltimore, New York, Portland, and Detroit. The study received IRB approval at all sites. Eligible providers included physicians, nurses, and physician assistants who provide primary care for patients with HIV. Eligible patients were HIV-positive, at least 18 years old, English-speaking, and had at least one previous visit with their provider. Visits between patients and providers were audio-recorded and transcribed verbatim by a professional transcription company. Research assistants conducted post-encounter interviews with each participating patient, using questionnaires that included detailed information about patients’ ARV regimens and medication adherence. Data (e.g. viral loads) were also abstracted from the patients’ medical records. Additional details about the ECHO study have been previously published (11–14).
Sample Selection and Qualitative Analysis
From the ECHO study, we selected all transcripts of patients who had been prescribed antiretrovirals (ARVs) and who reported non-adherence to their ARV regimen (missing doses in the past 3 days) using a detailed, validated questionnaire in post-encounter interviews (15,16).
One author (WC) read through each of the eligible transcripts in its entirety and identified all dialogue relating to ARVs, and within that dialogue, identified and abstracted all ARV-related provider questions directed at the patient and indicated whether or not the patient disclosed non-adherence in response to the question. There was no predetermined limit to the number of questions that a provider could ask a patient in any particular visit, so we included all ARV-related questions asked during the visit. We did not include questions that were asked after disclosure was elicited.
Analysis of the providers’ questions was guided by the principles of conversation analysis. Conversation analysis examines interactions between individuals as sequential events that have patterns that can be identified by approaching data without preconceived hypotheses and instead allowing patterns to emerge as the data is analyzed in a case-by-case manner. This allows the investigator to determine how a given outcome of an interaction is achieved as well as the different ways that it is achieved in that setting (17,18). In this study, categories of question types were generated inductively by two authors (WC and MCB) and were modified continuously throughout the analytic process. As primary categories emerged, we also identified additional subcategories based on patterns evident in the data. Two investigators (WC and MCB) agreed upon the final categories through iterative consensus.
Quantitative analysis
After categorizing all ARV-related questions, we assessed the frequency of each question type and the rates of patient non-adherence disclosures following each question type. We used negative binomial regression modeling to calculate the unadjusted and adjusted relative risks of patient non-adherence disclosure by the question type, sequential order of the question (whether it was the first, second, or third question asked about ARVs during the visit), and whether the question was leading. Leading questions were defined as those that lead the patient to deny non-adherence (e.g. “you’re taking all your medications right?”) and were one of the subtypes identified within two of the primary question categories. All data analysis was conducted using Stata/SE version 10.0 (College Station, Texas).
RESULTS
Provider and Patient Characteristics
Of the 434 patients in the entire study, 334 (79%) were on ARV therapy and, of those, 59 (18%) reported missing doses in the past 3 days. One patient had an unusable audio-recording, leaving 58 patients for analysis. Characteristics of patients and providers are presented in Table I. The 58 patients were seen by 34 providers who were equally split by gender. The majority were physicians and most were non-Hispanic white (70.6%). All were experienced HIV health-care providers.
Table I.
Provider and Patient Samples
| Provider Characteristics (N = 34) | |
| Female, n (%) | 17 (50) |
| Race, n (%) | |
| White | 24 (71) |
| Black | 3 (9) |
| Asian | 6 (18) |
| Latino | 1 (3) |
| Health profession, n (%) | |
| Physician | 25 (74) |
| Nurse practitioner | 6 (18) |
| Physician assistant | 3 (9) |
|
| |
| Patient Characteristics (N = 58) | |
|
| |
| Age, mean (SD) | 43.3 (8.5) |
| Female, n (%) | 26 (45) |
| Race, n (%) | |
| White | 7 (12) |
| Black | 39 (67) |
| Other | 12 (21) |
| Education, n (%) | |
| Less than high school | 20 (34) |
| Years with this provider, n (%) | |
| < 1 year | 6 (10) |
| 1–5 years | 27 (47) |
| > 5 years | 25 (43) |
| Viral Load | |
| Not suppressed (>400) | 25 (43%) |
| Suppressed (≤400) | 33 (57%) |
There were no differences in patient age, gender, race/ethnicity, education, viral load, or length of patient provider relationship between patients whose non-adherence status was discovered by providers (n = 48) and those whose was not (n = 10) However, there was a trend (p=0.061) towards those who knew their provider for less than one year to be less likely to have their non-adherence discovered (50% discovered) compared to those who knew their provider for 1–5 years (89% discovered) or >5 years (84% discovered).
The 58 patients had a mean age of 43. Just fewer than half were female and two-thirds were black. One-third lacked a high-school degree, and 90% had known their provider for more than one year. Twenty-five patients (43%) had an unsuppressed viral load (> 400 copies/ml). The mean visit length for this sample was 24 minutes (range 5–65 minutes).
Dialogue Characteristics
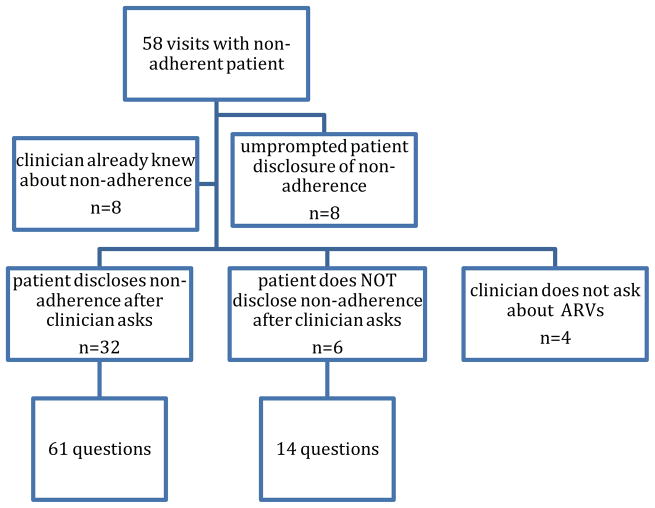
In 8 of the encounters it was apparent that providers already knew of patient non-adherence prior to the visit, and in another 8 encounters the patient disclosed non-adherence unprompted by providers (Figure I). These 16 encounters were thus removed from subsequent analysis. In the remaining 42 encounters, 4 providers did not discuss ARVs (10%), 6 discussed ARVs but did not elicit a disclosure of non-adherence (14%), and 32 discussed ARVs which prompted a disclosure of non-adherence (76%).
Figure I.
Characteristics of Dialogue and Number of Questions Asked
In these 42 encounters, the clinicians asked 75 questions about ARVs (mean 1.8 questions/visit). Thirty-two of the questions elicited disclosures of non-adherence (43%) and the remaining 43 did not (57%). Of these 43 questions that did not elicit disclosure, 29 were asked in visits where the provider later elicited an accurate patient response with a subsequent question, and 14 were questions asked in the 6 visits where disclosure was never elicited.
Question Types
Four primary categories of questions emerged from our content analysis: broad, clarifying, positively-framed, and negatively-framed. These questions are described in more detail below (and summarized in the Appendix).
I. Broad
Twelve questions were classified as ‘broad’ and asked generally about the patient’s experience with the medications. These questions were all open-ended. Two examples are shown below.
“How you been doin’ on taking your medications?”
“So, the medications, how is that going?”
II. Clarifying
Twenty-three questions were classified as ‘clarifying’, in which we deemed the main goal to be medication reconciliation or clarification of the patient’s medication regimen (e.g. drug name, prescribed dose). These questions were further subcategorized into ‘simple clarifying’, which asked about only the drug name or generally asked if the patient’s medicines were still the same (n=16), and ‘detailed clarifying’, which clarified additional details about the dose or regimen (n=7).
Simple clarifying
Among the 16 ‘simple clarifying’ questions, 13 asked about specific medications (example 1) and 3 were non-specific (example 2). All questions in this category were closed-ended.
“Are you still taking the Combivir, Viread and Sustiva?”
“So are you on the same medicines now, or did you change any of them since then?”
Detailed clarifying
Among the 7 ‘detailed clarifying’ questions, 5 were closed-ended (example 1 in which the provider gives the patient the regimen and asks for confirmation) and 2 were open-ended (example 2 in which the provider asks the patient to explain her medication regimen).
“So this is the um Epivir, which you take one twice a day? One in the morning, one at night?”
“Now tell me how you're taking the Epivir?”
III. Positively-framed
Seventeen questions were positively-framed, focusing specifically on the issue of medication adherence by asking about whether medications were being taken regularly or everyday. All of these questions were closed-ended and 4 were classified as ‘leading’ the patient to deny adherence (example 3).
-
1
“Do you take your HIV medicines every day?”
-
2
“Using all your medicines regularly?”
Leading
-
3
“Uh you have been taking HIV medications, right?”
IV. Negatively-framed
Twenty-three questions were negatively-framed, focusing specifically on the issue of medication adherence by using words such as “missed” or “skipped.” Five of these questions asked about a specific timeframe (examples 1–2) and the remaining 18 asked about a general timeframe (examples 3–4). Four explicitly normalized missing doses by asking about when or how many doses had been missed (rather than if any doses were missed; examples 5–6). Five were classified as leading the patient to deny non-adherence (example 7–8). Finally, 2 used laboratory evidence to suggest that the patient might be missing doses (example 9).
Specific timeframe
-
1
“In the past three days would you say that you missed any of the dosages of your medicines?”
-
2
“Have you missed any doses in the last four weeks?”
General timeframe
-
3
“Now, have you missed any?”
-
4
“Um, well have you missed any doses of your Fuzeon, Viramune, etcetera?”
Normalizing with ‘when or ‘how often’
-
5
“Okay, um when was the last time you completely missed a dose? Do you remember?”
-
6
“How many doses have you missed?”
Leading
-
7
“You haven’t been missing any of the medicine, right?”
-
8
“So you haven’t missed any HIV meds at all?”
Confronts with evidence
-
9
“So, do you miss these sometimes?... Cuz your viral load has gone up.”
Characteristics of Questions and Disclosure of Non-Adherence
Physicians asked up to 4 adherence questions per visit, and were most likely to start with a clarifying question (34%) and least likely to start with a negatively-framed question (16%). Subsequent questions were more likely to be negatively-framed, with 40% of second questions and 64% of third questions falling into this category.
Table II shows prevalence of question characteristics and disclosure rates. Overall, 32 of the 75 questions elicited disclosures of non-adherence (43%). By question type, rates of disclosure were 33% for broad questions, 13% for clarifying questions, 29% for positively-framed questions, and 87% for negatively-framed questions. Of the 3 negatively-framed questions that did not elicit disclosures, 1 was a leading question (“you haven’t been missing any of the medicines, right?,” one asked about a general timeframe, and one about a specific timeframe. In addition, disclosure was elicited following 6 of the 9 questions that were classified as “leading” the patient to deny non-adherence. Five of the leading questions were in the form of “you haven’t missed any meds, right?,” with 4 eliciting disclosure (80%) and the remaining 4 were in the were in the form of “you’re taking all your meds, right?,” with 2 eliciting disclosure (50%). The first question asked during the encounter was least likely to elicit an accurate response while subsequent questions were increasingly more likely to elicit accurate responses. However, after adjusting for question type, the association between question order and disclosure was non-significant.
Table II.
Association of Question Type and Question Number with Disclosure of Non-Adherence
| Question type | Prevalence | Disclosed | Not disclosed |
|---|---|---|---|
| Broad | 12 | 4 (33.3%) | 8 (66.7%) |
| Clarifying | 23 | 3 (13.0%) | 20 (87.0%) |
| Positively-framed | 17 | 5 (29.4%) | 12 (70.6%) |
| Negatively-framed | 23 | 20 (87%) | 3 (13%) |
| Leading | 9 | 6 (67%) | 3 (33%) |
| Question Number | Prevalence | Disclosed | Not disclosed |
|---|---|---|---|
| 1 | 38 | 13 (34.2%) | 25 (65.8%) |
| 2 | 25 | 10 (40.0%) | 15 (60.0%) |
| 3 | 11 | 8 (73%) | 3 (27%) |
| 4 | 1 | 1 (100%) | 0 (0%) |
Table III shows the unadjusted and adjusted risk of disclosure following questions with different characteristics. After adjusting for other question characteristics (including the question order and whether or not it was leading), the likelihood of non-adherence disclosure was 3.64 times higher for negatively-framed questions compared to all other question types.
Table III.
Unadjusted and Adjusted Risk of Disclosure based on Question Characteristics
| Unadjusted | Adjusteda | |||
|---|---|---|---|---|
| Relative Risk | 95% CI | Relative Risk | 95% CI | |
| Negatively- framed | ||||
| no | 1.00 | 1.00 | ||
| yes | 3.77*** | 2.23 – 6.37 | 3.64*** | 2.09– 6.34 |
| Order | ||||
| 1 | 1.00 | 1.00 | ||
| 2 | 1.17 | 0.61– 2.25 | 0.80 | 0.49– 1.32 |
| 3 | 2.19** | 1.26– 3.81 | 1.20 | 0.65– 2.23 |
| Leading | ||||
| no | 1.00 | 1.00 | ||
| yes | 1.69* | 0.97– 2.94 | 1.15 | 0.64– 2.06 |
p<0.10,
p<0.05,
p<0.001
adjusted for question order, whether it was leading, and whether it was negatively- framed
DISCUSSION
We found that, although most providers elicited accurate disclosures of ARV non-adherence, a substantial minority (24%) either did not ask or did not elicit accurate disclosure from patients who were asked. Of the four question types used routinely by providers, our study found that one type of question clearly outperformed all others: negatively-framed questions that explicitly ask about missed doses were by far the most likely to elicit accurate patient disclosures. This finding has never before been demonstrated in clinical encounters, and has the potential to impact HIV practice widely.
We propose two theories that may explain why negatively-framed questions elicit much higher rates of disclosure than other question types. First, the question “have you missed any doses?” does not allow for varying interpretations. In response to this question, a patient who knows she has missed doses must either tell the truth or knowingly hide the truth from the provider. Second, providers’ use of words such as “missed” or “skipped” may normalize non-adherence, lowering the barrier to disclosure. Notably, the four questions that even more explicitly normalized missing doses (by asking about the last time a patient missed or how many doses a patient has missed) all elicited disclosures. Previous studies have found that patients feel embarrassed about disclosing non-adherence to their providers (19). Thus, by using what Barford et al previously referred to as “suggestive phrasing,” providers may implicitly give permission to patients to disclose that they have missed doses (9).
It is not surprising that the other three question types elicited much lower rates of disclosure. For example, the intent of broad and clarifying questions does not appear to be adherence monitoring. Clarifying questions are often asked in the context of medication reconciliation, with the provider asking about each medication in the patient’s medical record in sequence. Patients likely interpret these questions as they seem to be intended: confirmations of whether they have been prescribed those medications, not as questions regarding their degree of adherence. Similarly, broad questions are vague and at times may seem perfunctory. In the same way that we answer “fine” to the question “how are you?,” the question “how’s it going with your medications?” tends to elicit a short, affirmative response from the patient (“pretty good”).
Finally, positively-framed questions, although more specific than broad questions, also allow room for interpretation. A patient’s answer to “are you taking your medications regularly?” is dependent on her interpretation of the word “regularly,” which may differ from person to person. In addition, positively-framed question do not lower the barrier to disclosure in the same way that negatively-framed questions do. While negatively-framed questions normalize “missing,” positively-framed questions have the opposite implication: they suggest that “taking” is the expected behavior. This then may lead patients to feel less comfortable admitting non-adherence. We recognize that our finding that 6 of 9 leading questions elicited disclosures may be surprising. As discussed above, 5 of the leading questions were negatively framed (“you haven’t missed any meds, right?”), with 4 eliciting disclosure (80%). The remaining 4 were positively framed (“you’re taking all your meds, right?”), with 2 eliciting disclosure (50%). We suspect that even when asked in a leading manner, asking about missed doses may still be more likely to prompt the patient to disclose non-adherence.
There are several differences between our study and previous studies with regard to how often providers discuss adherence, and how often it is accurately elicited when discussed. A previous study found that primary care physicians failed to ask about hypertension medication adherence in 33% of encounters with patients who had uncontrolled hypertension (8). In contrast, in our sample only 10% of HIV providers failed to ask about ARV adherence even though fewer than half of the patients (43%) had unsuppressed viral loads. Furthermore, another study about hypertension medications found that only 53% of instances of non-adherence were accurately identified (7), compared to 80% of instances of non-adherence in our study. These differences may be due to several factors. First, there is a marked emphasis on adherence in HIV care that may not be present in other disease conditions, resulting in HIV providers being more likely to ask about, and patients being more likely to report, problems with taking their medications because they are aware of the risk of viral resistance. This is supported by the instances in our sample in which patients disclosed non-adherence unprompted by providers or in response to broad or clarifying questions that did not explicitly ask about adherence. Finally, it should be noted that our study focused specifically on how providers might most effectively ask about adherence when speaking to patients, rather than focusing on what the most effective way to ask the question in a standardized questionnaire such as a survey or prompted by the medical record. While our findings may have some relevance for standardized questioning in surveys or medical records, a broad body of literature has addressed that question (2, 16, 20–22). Given that previous studies have found especially low rates of non-adherence disclosure in medical interviews (as compared to written surveys), our study instead focuses on how to optimize adherence disclosure in the medical interview (23).
Opportunities exist for future research regarding how providers respond to disclosures of non-adherence. It is possible that some of the patient disclosures, particularly unprompted ones, may be explained by the provider previously responding to similar disclosures in a way that made patients feel comfortable and supported. Understanding the impact of providers’ responses on future disclosures of non-adherence is important, as previous studies have found that patients sometimes choose not to disclose because they are afraid of their provider’s disapproval (19). Further research is also necessary to understand providers’ thoughts and motivations regarding adherence monitoring. A previous study observed that “physicians who did not ask specific questions about missed doses stated that they believed doing so was probably a good idea; they simply had not yet incorporated it into their routines” (10). This suggests that there may be barriers to providers implementing changes in the way that they ask about medication adherence. One possible reason is that providers find it awkward to ask questions they perceive as confrontational, or are afraid to offend patients (9).
This study has several limitations. First, it is possible that patients’ and providers’ behavior was influenced by the knowledge that the encounter was being recorded. However, we observed a wide range of behavior and communication styles that do not suggest that patient and provider communication was strongly inhibited. Previous studies addressing this question have found that recording medical interactions has no significant effect on patient or provider behavior (24–26). Moreover, we would expect the presence of the audio-recorder to lead providers to be more cognizant of their communication styles, so our observation that a substantial minority of providers did not elicit disclosures of non-adherence is a conservative finding. Second, although we had a large sample size and detailed data about patient adherence, we still only had a small number of questions in secondary categories. Therefore we were not able to statistically test the impact of leading questions (which are generally thought not to be effective) or of negatively-framed questions that explicitly normalize missing doses (“when was the last time you missed a dose?” vs. “have you missed any doses?”). Finally, self-reported measures of adherence rely on patient recall and truth-telling, and patients who were not adherent but did not report non-adherence during the post-encounter interview would not have been captured in our sample. Our determination of non-adherence was based on missing any doses within the last 3 days, as reported by patients during a post-encounter interview with a research assistant. We chose this measure based on prior research showing its relation to virologic and immunologic outcomes (16). We also explored the use of other measures of self-reported adherence, including global measures such as general or 30-day estimations, that have been widely used and tested previously (27–29). We found a high correlation between our three-day recall measure and a question asking patients to estimate the percentage of days they took their medications in the past 30 days, and another asking patients to rate their adherence to ARV medications in general.
In summary, it is critical that providers caring for HIV-positive patients be aware of patient non-adherence to ARVs in order to counsel patients and adjust treatment appropriately so as to avoid the risk of viral resistance. Our findings suggest that questions clarifying medication regimens, broad questions about how the patients is doing on the medications, and even questions asking if a patient is taking their medications regularly may not constitute a sufficient inquiry regarding medication adherence. Providers can improve the probability with which they elicit accurate disclosures of non-adherence by using negatively-framed questions that ask explicitly about missed doses.
Acknowledgments
This research was supported by a contract from the Health Resources Service Administration and the Agency for Healthcare Research and Quality (AHRQ 290-01-0012). In addition, Dr. Korthuis was supported by the National Institute of Drug Abuse (K23 DA019809). Dr. Saha was supported by the Department of Veterans Affairs, Dr. Beach was supported by the National Institute of Drug Abuse (K24 DA037804). None of the funders had a role in the design and conduct of this analysis, nor was it subject to their final approval.
APPENDIX
Table IV.
Types of Questions
| Primary category | Secondary categorya | Examples |
|---|---|---|
| Broad (n = 12) | Open (n = 12) |
|
|
| ||
| Clarifying (n = 23) | Simple, specific, closed (n = 13) |
|
| Simple, non-specific, closed (n = 3) |
|
|
| Detailed, closed (n = 5) |
|
|
| Detailed, open (n = 2) |
|
|
|
| ||
| Positively-framed (n = 17) | Closed (n = 17) |
|
| Leading (n = 4) |
|
|
|
| ||
| Negatively-framed (n = 23) | Specific timeframe, closed (n = 5) |
|
| General timeframe, closed (n = 18) |
|
|
| Normalizing (n = 4) |
|
|
| Leading (n = 5) |
|
|
| Presents evidence (n = 2) |
|
|
Secondary categories are not mutually exclusive or exhaustive, to the total number of questions in that primary category
Footnotes
None of the authors have any relevant financial conflicts of interest.
References
- 1.Hinkin CH, Hardy DJ, Mason KI, Castellon SA, Durvasula RS, Lam MN, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS Lond Engl. 2004;18:S19–25. doi: 10.1097/00002030-200418001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knobel H, Alonso J, Casado JL, Collazos J, González J, Ruiz I, et al. Validation of a simplified medication adherence questionnaire in a large cohort of HIV-infected patients: the GEEMA Study. AIDS Lond Engl. 2002;16:605–13. doi: 10.1097/00002030-200203080-00012. [DOI] [PubMed] [Google Scholar]
- 3.Nieuwkerk PT, Sprangers MA, Burger DM, Hoetelmans RM, Hugen PW, Danner SA, et al. Limited patient adherence to highly active antiretroviral therapy for HIV-1 infection in an observational cohort study. Arch Intern Med. 2001;161:1962–8. doi: 10.1001/archinte.161.16.1962. [DOI] [PubMed] [Google Scholar]
- 4.Miller LG, Liu H, Hays RD, Golin CE, Beck CK, Asch SM, et al. How Well Do Clinicians Estimate Patients’ Adherence to Combination Antiretroviral Therapy? J Gen Intern Med. 2002;17:1–11. doi: 10.1046/j.1525-1497.2002.09004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gross R, Bilker WB, Friedman HM, Coyne JC, Strom BL. Provider inaccuracy in assessing adherence and outcomes with newly initiated antiretroviral therapy. AIDS Lond Engl. 2002;16:1835–7. doi: 10.1097/00002030-200209060-00021. [DOI] [PubMed] [Google Scholar]
- 6.Bangsberg DR, Hecht FM, Clague H, Charlebois ED, Ciccarone D, Chesney M, et al. Provider assessment of adherence to HIV antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;26:435–42. doi: 10.1097/00126334-200104150-00005. [DOI] [PubMed] [Google Scholar]
- 7.Steele DJ, Jackson TC, Gutmann MC. Have you been taking your pills? The adherence-monitoring sequence in the medical interview. J Fam Pract. 1990;30:294–9. [PubMed] [Google Scholar]
- 8.Bokhour BG, Berlowitz DR, Long JA, Kressin NR. How Do Providers Assess Antihypertensive Medication Adherence in Medical Encounters? J Gen Intern Med. 2006;21:577–83. doi: 10.1111/j.1525-1497.2006.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barfod TS, Hecht FM, Rubow C, Gerstoft J. Physicians’ communication with patients about adherence to HIV medication in San Francisco and Copenhagen: a qualitative study using Grounded Theory. BMC Health Serv Res. 2006;6:154. doi: 10.1186/1472-6963-6-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts KJ, Volberding P. Adherence communication: a qualitative analysis of physician-patient dialogue. AIDS Lond Engl. 1999;13:1771–8. doi: 10.1097/00002030-199909100-00022. [DOI] [PubMed] [Google Scholar]
- 11.Beach MC, Saha S, Korthuis PT, Sharp V, Cohn J, Wilson IB, et al. Patient-provider communication differs for black compared to white HIV-infected patients. AIDS Behav. 2011;15:805–11. doi: 10.1007/s10461-009-9664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beach MC, Saha S, Korthuis PT, Sharp V, Cohn J, Wilson I, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25:682–7. doi: 10.1007/s11606-010-1310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beach MC, Roter D, Korthuis PT, Epstein RM, Sharp V, Ratanawongsa N, et al. A multicenter study of physician mindfulness and health care quality. Ann Fam Med. 2013;11:421–8. doi: 10.1370/afm.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saha S, Korthuis PT, Cohn JA, Sharp VL, Moore RD, Beach MC. Primary care provider cultural competence and racial disparities in HIV care and outcomes. J Gen Intern Med. 2013;28:622–9. doi: 10.1007/s11606-012-2298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 16.Mannheimer S, Thackeray L, Huppler Hullsiek K, Chesney M, Gardner EM, Wu AW, et al. A randomized comparison of two instruments for measuring self-reported antiretroviral adherence. AIDS Care. 2008;20:161–9. doi: 10.1080/09540120701534699. [DOI] [PubMed] [Google Scholar]
- 17.Drew P, Chatwin J, Collins S. Conversation analysis: a method for research into interactions between patients and health-care professionals. Health Expect. 2001;4:58–70. doi: 10.1046/j.1369-6513.2001.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peräkylä A. Conversation analysis: a new model of research in doctor-patient communication. J R Soc Med. 1997;90:205–8. doi: 10.1177/014107689709000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tugenberg T, Ware NC, Wyatt MA. Paradoxical Effects of Clinician Emphasis on Adherence to Combination Antiretroviral Therapy for HIV/AIDS. AIDS Patient Care STDs. 2006;20:269–74. doi: 10.1089/apc.2006.20.269. [DOI] [PubMed] [Google Scholar]
- 20.Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. AIDS Lond Engl. 2002;16:269–77. doi: 10.1097/00002030-200201250-00017. [DOI] [PubMed] [Google Scholar]
- 21.Lu M, Safren SA, Skolnik PR, Rogers WH, Coady W, Hardy H, et al. Optimal Recall Period and Response Task for Self-Reported HIV Medication Adherence. AIDS Behav. 2007;12:86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 22.Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-Report Measures of Antiretroviral Therapy Adherence: A Review with Recommendations for HIV Research and Clinical Management. AIDS Behav. 2006;10:227–45. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42:649–52. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- 24.Pringle M, Stewart-Evans C. Does awareness of being video recorded affect doctors’ consultation behaviour? Br. J Gen Pract. 1990;40:455–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Penner LA, Orom H, Albrecht TL, Franks MM, Foster TS, Ruckdeschel JC. Camera-Related Behaviors during Video Recorded Medical Interactions. J Nonverbal Behav. 2007;31:99–117. [Google Scholar]
- 26.Wolraich ML, Albanese M, Stone G, Nesbitt D, Thomson E, Shymansky J, et al. Medical Communication Behavior System. An interactional analysis system for medical interactions. Med Care. 1986;24:891–903. doi: 10.1097/00005650-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Wilson IB, Carter AE, Berg KM. Improving the self-report of HIV antiretroviral medication adherence: is the glass half full or half empty? Curr. HIV/AIDS Rep. 2009;6:177–86. doi: 10.1007/s11904-009-0024-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fowler FJ, Lloyd SJ, Cosenza CA, Wilson IB. Coding Cognitive Interviews An Approach to Enhancing the Value of Cognitive Testing for Survey Question Evaluation. Field Methods. 2014 [Google Scholar]
- 29.Wilson IB, Fowler FJ, Cosenza CA, Michaud J, Bentkover J, Rana A, et al. Cognitive and field testing of a new set of medication adherence self-report items for HIV care. AIDS Behav. 2014;18:2349–58. doi: 10.1007/s10461-013-0610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]