Abstract
Use of deceased diabetic donor kidneys has increased over recent decades. However, scarce patient and allograft survival data are available taking into account recipient diabetes status. Here we performed a retrospective cohort study using data from the United Network of Organ Sharing in patients transplanted from 1994 to 2014. Multivariable Cox regression assessed recipient outcomes of 9, 074 diabetic versus 152, 555 non-diabetic donor kidneys. Recipients of diabetic donor kidneys had elevated rates of all-cause allograft failure (hazard ratio 1.21, 95% confidence interval 1.16-1.26) and death (1.19, 1.13-1.24) compared to recipients of kidneys from non-diabetic donors. Younger recipients of diabetic donor kidneys had worse allograft survival than older recipients of non-diabetic donor kidneys. There was significant interaction between donor and recipient diabetes status. To minimize the effect of unmeasured confounders, we used paired analyses of recipients of mate-kidneys from the same donor, with one diabetic recipient and the other non-diabetic. Among discordant recipient pairs of diabetic donor kidneys, diabetic recipients had significantly higher risk of allograft failure (1.27, 1.05-1.53) and death (1.53, 1.22-1.93) than non-diabetic recipients. After stratifying by Kidney Donor Profile Index risk category, diabetic recipients of diabetic donor kidneys continued to have worse allograft survival compared to all other patients. Thus, risks are associated with the use of diabetic donor kidneys. Understanding these risks will enable clinicians to better educate potential recipients.
Keywords: diabetes, diabetic nephropathy, chronic kidney disease
INTRODUCTION
The demand for deceased donor kidneys exceeds the availability of high quality organs. As a result, there has been increased utilization of kidneys from donors with risk factors for allograft failure, such as diabetes.1 The use of these high risk, or marginal, donor kidneys is widely accepted in the United States, as some patients derive a survival benefit from transplantation with marginal donor organs compared to remaining on dialysis.2 However, the long-term consequences of using these kidneys, as opposed to non-marginal kidneys, on recipient outcomes remains unclear.1, 3
There have been various approaches to the allocation of marginal donor kidneys as their utilization has expanded. The Expanded Criteria Donor (ECD) classification was one such approach, and identified kidneys from donors aged 60 years or older, or age 50 to 59 years in the presence of at least two of three risk factors including 1) cerebrovascular cause of death, 2) history of hypertension, or 3) serum creatinine >1.5 mg/dL, as being associated with a 1.7-fold higher risk of allograft failure compared to “standard criteria” donor kidneys.4 While these clinical criteria frequently coincided with donor diabetes, the ECD classification did not account for donor diabetes status. The new Kidney Allocation System (KAS), implemented in December 2014, uses the Kidney Donor Profile Index (KDPI) which assigns a graft failure risk score to deceased donor kidneys based on a much broader range of donor characteristics than ECD criteria.5, 6 Diabetes is heavily weighted in the KDPI scoring.7 The newly implemented KAS also incorporates recipient diabetes in the allocation of kidneys through its inclusion in the Estimated Post Transplant Survival (EPTS) recipient risk score.8 Under the new KAS, diabetic recipients have higher EPTS scores than their non-diabetic counterparts,9 which will limit their access to low KDPI kidneys and increase the likelihood of allocating diabetic donor kidneys to diabetic recipients.
Few studies have evaluated patient and allograft survival among recipients of diabetic donor kidneys.1, 2, 10, 11 These studies demonstrated no significant effect of donor diabetes on allograft and patient survival compared to non-diabetic donor kidneys, and even suggested that diabetic donor kidneys were superior to ECD kidneys.1, 10 However, these investigations have significant limitations including small sample size,11 relatively short duration of follow up,1, 2, 10 and a potential for organ allocation bias based on unmeasured donor characteristics. Histologic reversal of diabetic nephropathy when diabetic donor kidneys are transplanted into non-diabetic recipients has been described in small, single-center case series.12, 13 Little is known about the impact of transplanting diabetic donor kidneys into diabetic recipients.
In light of the uncertainty about recipient outcomes and recent changes in the allocation system, we undertook this study to better understand the risks to recipients of broadening the utilization of diabetic donor kidneys. The goal of this study was to evaluate the impact of diabetic donor kidney transplantation on allograft and patient survival among both diabetic and non-diabetic recipients, including a mate-kidney analysis to control for unmeasured donor characteristics that may strongly influence organ allocation. We aim to guide clinicians on optimal allocation of these organs, and to educate patients about the risks associated with such organ offers.
RESULTS
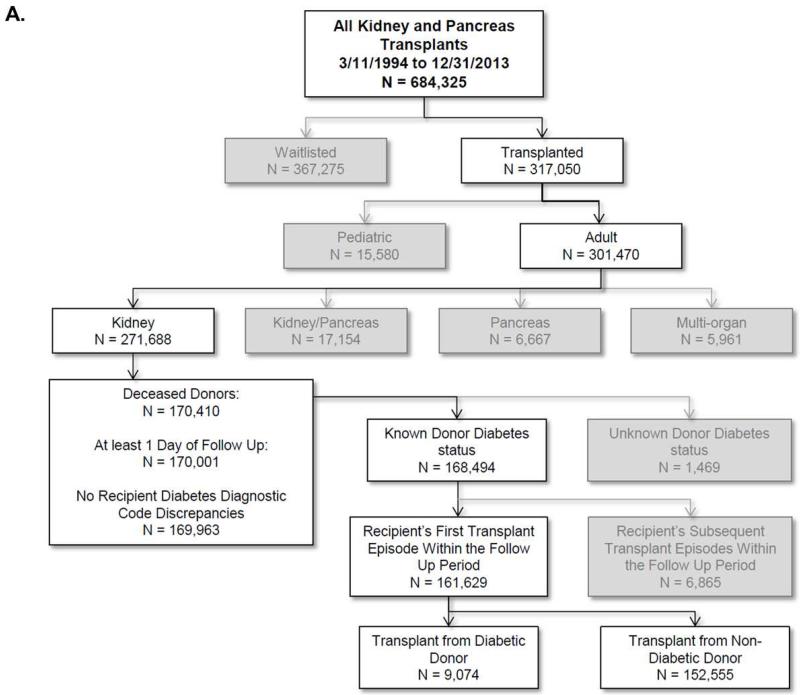
Primary Cohort Assembly (Figure 1a)
Figure 1a.
Cohort selection for evaluation of recipients of diabetic versus non-diabetic donor kidneys.
Overall, 684 325 kidney and pancreas transplant and waitlist registrations were recorded in the database from March 11, 1994 to December 31, 2013. We excluded patients who remained on the waitlist throughout the duration of the study period, pediatric patients, pancreas transplant recipients, simultaneous kidney-pancreas or multiple organ transplant recipients, and recipients of living donor kidneys. There were 161 629 eligible patients. Among these patients, there were 9 074 recipients of diabetic donor kidneys and 152 555 recipients of non-diabetic donor kidneys. From 1994 to 2004, there were 2 528 diabetic donor kidneys utilized, of which 685 (27.1%) were transplanted into diabetic recipients. From 2004 to 2014, there were 6 175 diabetic donor kidneys utilized, of which 2 423 (39.2%) were transplanted into diabetic recipients.
There was a statistically significant difference between recipients of diabetic donor kidneys and recipients of non-diabetic donor kidneys in most parameters evaluated (Table 1a), in part related to the large sample size. Recipients of diabetic donor kidneys were older (median age 56 versus 51), had longer waitlist times (median 688 days versus 616 days), were more frequently diabetic themselves (35.9% versus 29.7%), and were more likely to have delayed graft function (30.1% versus 24.6%). Diabetic donor kidneys had a higher KDPI (as expected given inclusion of diabetes in the calculation; median KDPI 77 versus 40), more frequently met ECD criteria (37.3% versus 15.1%), and came from donors with a higher body mass index (29.7 kg/m2 versus 25.2 kg/m2). Induction immunosuppression was used in the majority of patients in both groups and tacrolimus was the predominant calcineurin inhibitor. There was no regional variation between the groups.
Table 1a.
Baseline characteristics of recipients of non-diabetic vs. diabetic donor kidneys
| Diabetic Donors N = 9,074* |
Non-Diabetic Donors N = 152,555* |
P-value | |
|---|---|---|---|
| Recipient Characteristics | |||
|
| |||
| Median age in years (IQR) | 56 (47-64) | 51 (41-60) | P < 0.001 |
|
| |||
| Male (%) | 5,612 (61.9) | 92,258 (60.5) | p = 0.009 |
|
| |||
| Race (%) | p < 0.001 | ||
| Caucasian | 4,247 (46.8) | 75,502 (49.5) | |
| African American | 2,915 (32.1) | 45,949 (30.1) | |
| Latino | 1,204 (13.3) | 19,831 (13.0) | |
| Asian | 539 (5.9) | 8,063 (5.3) | |
| Other | 169 (1.9) | 3,210 (2.1) | |
|
| |||
| Cause of ESRD (%) | p < 0.001 | ||
| Diabetes | 2,516 (27.7) | 37,335 (24.5) | |
| Hypertension | 2,606 (28.7) | 37,335 (24.5) | |
| Glomerular Disease | 1,353 (14.9) | 27,169 (17.8) | |
| Cystic Disease | 764 (8.4) | 13,571 (8.9) | |
| Other | 1,350 (14.9) | 27,238 (17.9) | |
| Missing | 485 (5.3) | 9,701 (6.4) | |
|
| |||
| Pre-transplant Dialysis (%) | 8,208 (90.5) | 138,048 (90.5) | p = 0.035 |
|
| |||
| Median Years on Dialysis (IQR) | 3.3 (1.9-5.2) | 3.2 (1.8-5.1) | p < 0.001 |
|
| |||
| Median Total Days on Wait List (IQR) | 688 (293-1208) | 616 (249-1141) | p < 0.001 |
|
| |||
| Repeat Renal Transplant | 797 (8.8) | 16,974 (11.1) | p < 0.001 |
|
| |||
| HBV Surface Ag + (%) | 194 (2.1) | 2,866 (1.9) | p = 0.056 |
|
| |||
| HCV+ Recipient (%) | 457 (5.0) | 8,920 (5.9) | p < 0.001 |
|
| |||
| PRA ≥ 30% (%) | 1,689 (18.6) | 32,831 (21.5) | p < 0.001 |
|
| |||
| ≥ 1 HLA Zero Mismatch (%) | 663 (7.3) | 16,608 (10.9) | p < 0.001 |
|
| |||
| Pre-transplant Diabetes (%) | 3,260 (35.9) | 45,245 (29.7) | p < 0.001 |
|
| |||
| Median BMI (kg/m2) | 27.3 (23.8-31.2) | 26.7 (23.3-30.8) | p < 0.001 |
|
| |||
| Donor Characteristics | |||
|
| |||
| KDPI Percentile (IQR) | 77 (59-90) | 40 (18-64) | p < 0.001 |
|
| |||
| Expanded Criteria Donor (%) | 3,388 (37.3) | 23,026 (15.1) | p < 0.001 |
|
| |||
| HCV+ Donor (%) | 152 (1.7) | 3,776 (2.5) | p < 0.001 |
|
| |||
| Median Donor Age in Years (IQR) | 50 (42-57) | 38 (22-50) | p < 0.001 |
|
| |||
| Median BMI (kg/m2) | 29.7 (25.4-35.0) | 25.2 (22.0-29.2) | p < 0.001 |
|
| |||
| Transplant Characteristics | |||
|
| |||
| Median CIT in Hours (IQR) | 18 (13-25) | 18 (13-24) | p < 0.001 |
|
| |||
| Delayed Graft Function (%) | 2,727 (30.1) | 37,453 (24.6) | p < 0.001 |
|
| |||
| Acute Rejection at One Year (%) | 1,049 (14.9) | 20,516 (17.0) | p < 0.001 |
|
| |||
| Tacrolimus Maintenance (%) | 6,577 (72.5) | 96,268 (63.1) | p < 0.001 |
|
| |||
| Mycophenolate Maintenance (%) | 7,558 (83.3) | 119,925 (78.6) | p < 0.001 |
|
| |||
| No Induction (%) | 2,285 (25.2) | 44,828 (29.4) | p < 0.001 |
|
| |||
| Lymphodepleting Induction (%) | 5,079 (56.0) | 77,424 (50.8) | p < 0.001 |
|
| |||
| Non-Lymphodepleting Induction (%) | 2,073 (22.9) | 35,790 (23.5) | p = 0.179 |
|
| |||
| Both Types of Induction (%) | 363 (4.0) | 5,487 (3.6) | p = 0.045 |
N denotes the number of recipients in each donor category
Discordant Mate-Kidney Recipient Cohort Assembly (Figure 1b)
Figure 1b.
Cohort selection for discordant mate-kidney diabetic and non-diabetic recipient pairs
Among recipients of diabetic donor kidneys, there were 1 539 discordant pairs where one recipient was diabetic and the mate-kidney recipient was non-diabetic (3 078 individual recipients); there were 21 459 discordant recipient pairs (42 918 individual recipients) from non-diabetic donor kidneys. As in the primary cohort, there were significant differences between the groups in most parameters evaluated (Table 1b). Notably, within each donor stratum, diabetic recipients were significantly older (median age 59 versus 55 in recipients of diabetic donor kidneys, and 57 versus 50 in recipients of non-diabetic donors) and spent less time on the wait list (646 days versus 717 days in recipients of diabetic donor kidneys, 582 days versus 628 days in recipients of non-diabetic donors). They were less likely to have a repeat transplant (4.9% versus 9.2% in recipients of diabetic donors, 5.8% versus 11.7% in recipients of non-diabetic donors) and were less highly sensitized. Diabetic recipients had more frequent delayed graft function than non-diabetic recipients (33.6% versus 26.4% in recipients of diabetic donor kidneys, 28.5% versus 23.1% in recipients of non-diabetic donors). KDPI was again higher in diabetic donors (median KDPI 78 versus 44). As in the primary analysis, diabetic donor kidneys were more likely to meet ECD criteria (38.3% versus 17.7%) and come from older donors (median age 50 versus 42).
Table 1b.
Baseline characteristics among discordant diabetic and non-diabetic mate-kidney recipients
| Diabetic Donors | Non-Diabetic Donors | ||||
|---|---|---|---|---|---|
|
| |||||
| Diabetic Recipients N = 1,539 |
Non-Diabetic Recipients N = 1,539 |
Diabetic Recipients N = 21,459 |
Non-Diabetic Recipients N = 21,459 |
P-value | |
| Recipient Characteristics | |||||
|
| |||||
| Median age in years (IQR) | 59 (52-65) | 55 (45-64) | 57 (49-63) | 50 (40-60) | p < 0.001 |
|
| |||||
| Male (%) | 1,014 (65.9) | 941 (61.1) | 13.699 (63.8) | 12,916 (60.2) | p < 0.001 |
|
| |||||
| Race (%) | p < 0.001 | ||||
| Caucasian | 652 (42.4) | 747 (48.5) | 9,845 (45.9) | 11,009 (51.3) | |
| African American | 495 (32.2) | 495 (32.2) | 6,599 (30.8) | 6,366 (29.7) | |
| Latino | 268 (17.4) | 268 (17.4) | 3,382 (15.8) | 2,556 (11.9) | |
| Asian | 86 (5.6) | 102 (6.6) | 1,026 (4.8) | 1,151 (5.4) | |
| Other | 38 (2.5) | 15 (1.0) | 607 (2.8) | 377 (1.8) | |
|
| |||||
| Pre-transplant Dialysis (%) | 1,405 (91.3) | 1,368 (88.9) | 19,701 (91.8) | 19,119 (89.1) | p < 0.001 |
|
| |||||
| Median Years on Dialysis (IQR) | 3.2 (1.8-4.9) | 3.4 (1.8-5.4) | 3.0 (1.8-4.7) | 3.2 (1.8-5.2) | p < 0.001 |
|
| |||||
| Median Total Days on Wait List (IQR) | 646 (281-1147) | 717 (302-1228) | 582 (234-1086) | 628 (257-1142) | p < 0.001 |
|
| |||||
| Repeat Renal Transplant | 76 (4.9) | 142 (9.2) | 1,252 (5.8) | 2,516 (11.7) | p < 0.001 |
|
| |||||
| HBV Surface Ag + (%) | 23 (1.5) | 26 (1.7) | 382 (1.8) | 448 (2.09) | p = 0.027 |
|
| |||||
| HCV+ Recipient (%) | 65 (4.2) | 75 (4.9) | 1,194 (5.6) | 1,237 (5.8) | p = 0.054 |
|
| |||||
| PRA ≥ 30% (%) | 222 (14.4) | 302 (19.6) | 3,813 (17.8) | 4,743 (22.1) | p < 0.001 |
|
| |||||
| ≥ 1 HLA Zero Mismatch (%) | 133 (8.6) | 107 (7.0) | 2,322 (10.8) | 2,234 (10.4) | p < 0.001 |
|
| |||||
| Median BMI (kg/m2) | 28.8 (25.5-32.6) | 26.7 (23.3-30.7) | 28.6 (25.1-32.5) | 26.3 (23.1-30.2) | p < 0.001 |
|
| |||||
| Donor Characteristics | |||||
|
| |||||
| KDPI Percentile (IQR) | 78 (60-89) | 44 (21-67) | p < 0.001 | ||
|
| |||||
| Expanded Criteria Donor (%) | 590 (38.3) | 3,788 (17.7) | p < 0.001 | ||
|
| |||||
| HCV+ Donor (%) | 17 (1.1) | 557 (2.6) | p < 0.001 | ||
|
| |||||
| Median Donor Age in Years (IQR) | 50 (43-57) | 42 (26-52) | p < 0.001 | ||
|
| |||||
| Median BMI (kg/m2) | 29.9 (26.0-35.3) | 25.8 (22.5-29.9) | p < 0.001 | ||
|
| |||||
| Transplant Characteristics | |||||
|
| |||||
| Median CIT in Hours (IQR) | 17.8 (13-24) | 17.3 (13-24) | 17.6 (12-24) | 17.2 (12-23) | p = 0.025 |
|
| |||||
| Delayed Graft Function (%) | 517 (33.6) | 406 (26.4) | 6,124 (28.5) | 4,955 (23.1) | p < 0.001 |
|
| |||||
| Acute Rejection at One Year (%) | 175 (14.6) | 152 (12.6) | 2,322 (13.6) | 2,608 (15.1) | p = 0.001 |
|
| |||||
| Tacrolimus Maintenance (%) | 1,182 (76.8) | 1,174 (76.3) | 14,839 (69.2) | 15,008 (69.9) | p < 0.001 |
|
| |||||
| Mycophenolate Maintenance (%) | 1,334 (86.7) | 1,312 (85.3) | 18,099 (84.3) | 18,103 (84.4) | p = 0.075 |
|
| |||||
| No Induction (%) | 372 (24.2) | 330 (21.4) | 5,887 (27.4) | 5,884 (27.4) | p < 0.001 |
|
| |||||
| Lymphodepleting Induction (%) | 825 (53.6) | 866 (56.3) | 10,801 (50.3) | 11,009 (51.3) | p < 0.001 |
|
| |||||
| Non-Lymphodepleting Induction (%) | 413 (26.8) | 395 (25.7) | 5,680 (26.5) | 5,294 (24.7) | p < 0.001 |
|
| |||||
| Both Types of Induction (%) | 71 (4.6) | 52 (3.4) | 909 (4.2) | 728 (3.4) | p < 0.001 |
Patient and Allograft Survival
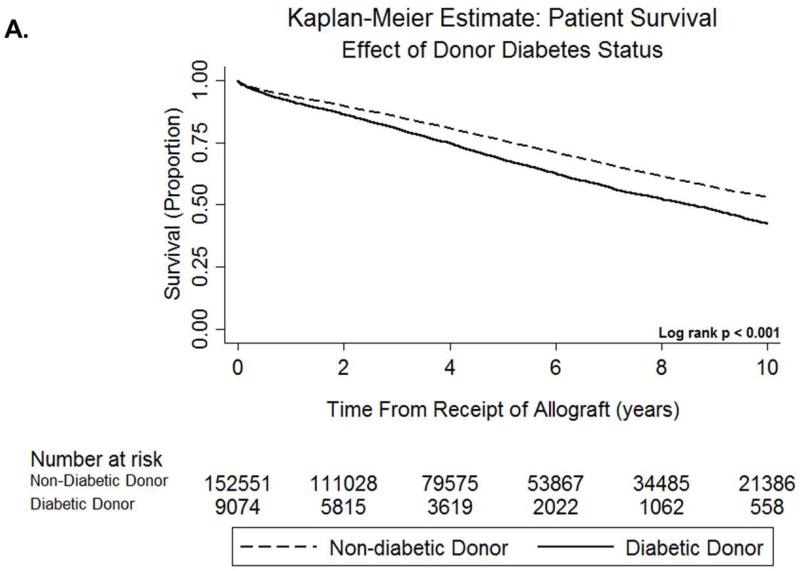
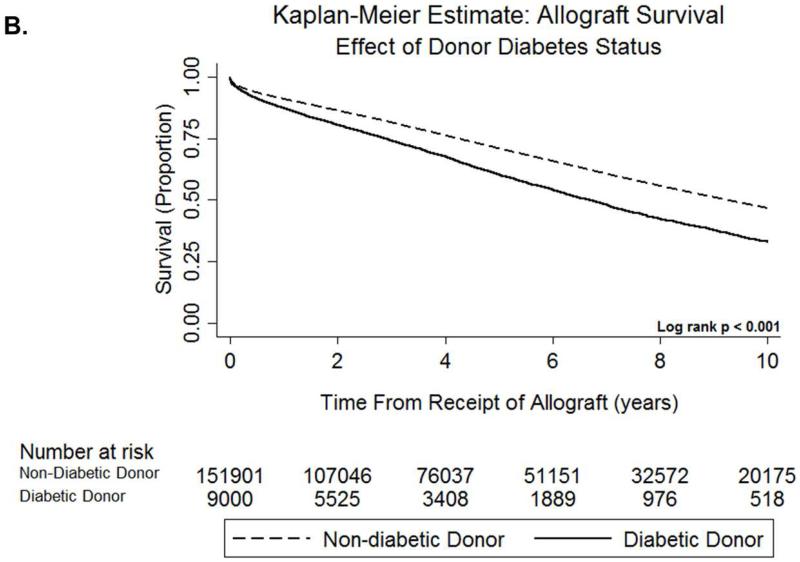
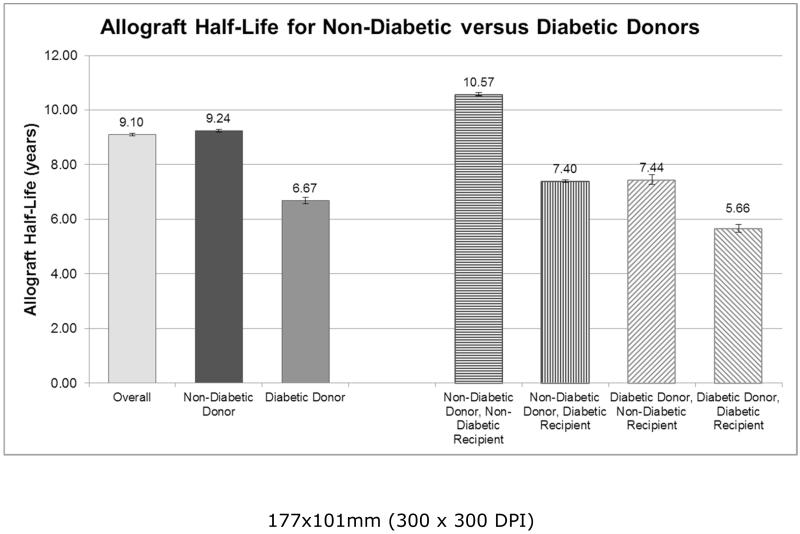
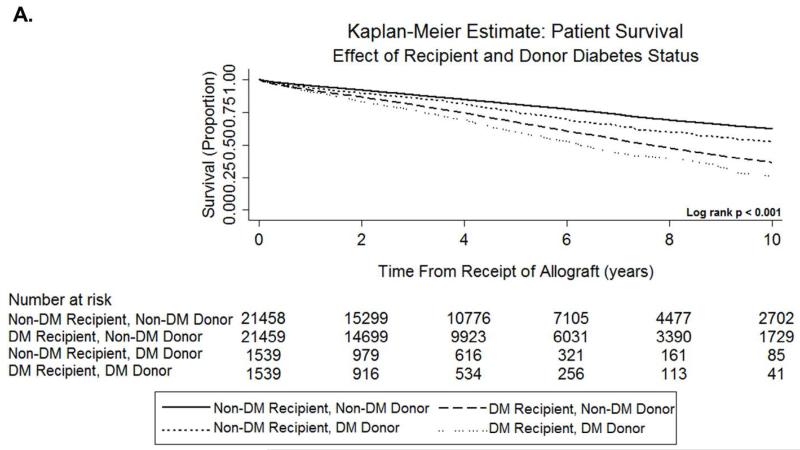
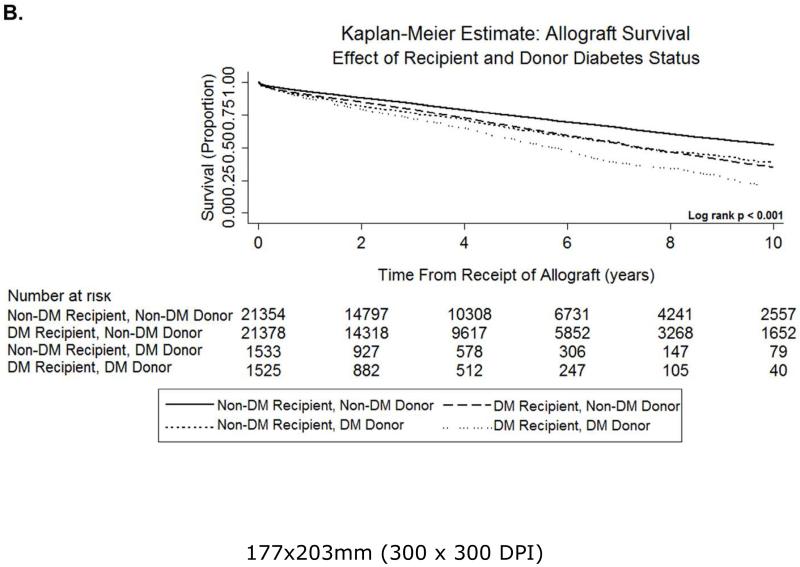
Median follow up of recipients in the primary analysis was 10.6 years. Patients who received diabetic donor kidneys had an increased mortality rate compared to those who received non-diabetic donor kidneys (Figure 2a, log rank p < 0.001). Recipients of diabetic donor kidneys had an increased rate of all-cause allograft failure compared to recipients of non-diabetic donor kidneys (Figure 2b, log rank p < 0.001). Non-diabetic recipients of non-diabetic donor kidneys had the longest allograft half-life (Figure 3, 10.57 years, 95% CI 10.44-10.68), followed by diabetic recipients of non-diabetic donor kidneys and non-diabetic recipients of diabetic donor kidneys, which had similar allograft half-lives (7.40 years, 95% CI 7.30-77.50 and 7.44 years, 95% CI 7.12-7.78, respectively). Diabetic recipients of diabetic donor kidneys had the shortest allograft half-life (5.66 years, 95% CI 5.33-5.99). Recipients ≤ 45 years old who received diabetic donor kidneys had an increased rate of all-cause allograft failure (log rank p < 0.001), but not mortality, compared to recipients > 45 years old who received non-diabetic donor kidneys (Figures S1a-S1b). After performing sensitivity analyses by age strata, age 65 was the youngest age at which receipt of diabetic donor kidneys in younger recipients yielded less relative disadvantage than receipt of non-diabetic donor kidneys in older recipients with regard to adverse allograft outcomes (Figures S1c-S1e). When comparing discordant recipient pairs, mortality risk was greatest in diabetic recipients of diabetic donor kidneys, followed by diabetic recipients of non-diabetic donor kidneys (Figure 4a, log rank p < 0.001). Mortality rate was lowest in non-diabetic recipients of non-diabetic donor kidneys. Among discordant recipient pairs, diabetic recipients of diabetic donors had the highest rate of all-cause allograft failure, and non-diabetic recipients of non-diabetic donors had the lowest rate of all-cause allograft failure (Figure 4b, log rank p < 0.001). Diabetic recipients of non-diabetic donor kidneys and non-diabetic recipients of diabetic donor kidneys had similar rates of all-cause allograft survival.
Figure 2a.
Kaplan-Meier curve evaluating mortality in recipients of diabetic versus non-diabetic donor kidneys.
Figure 2b.
Kaplan-Meier curve evaluating all-cause allograft failure in recipients of diabetic versus non-diabetic donor kidneys.
Figure 3.
Allograft half-life by donor and recipient diabetes status for the overall cohort.
Figure 4a.
Kaplan-Meier curve evaluating mortality in discordant mate-kidney recipients of diabetic and non-diabetic donor kidneys.
Figure 4b.
Kaplan-Meier curve evaluating all-cause allograft failure in discordant mate-kidney recipients of diabetic and non-diabetic donor kidneys.
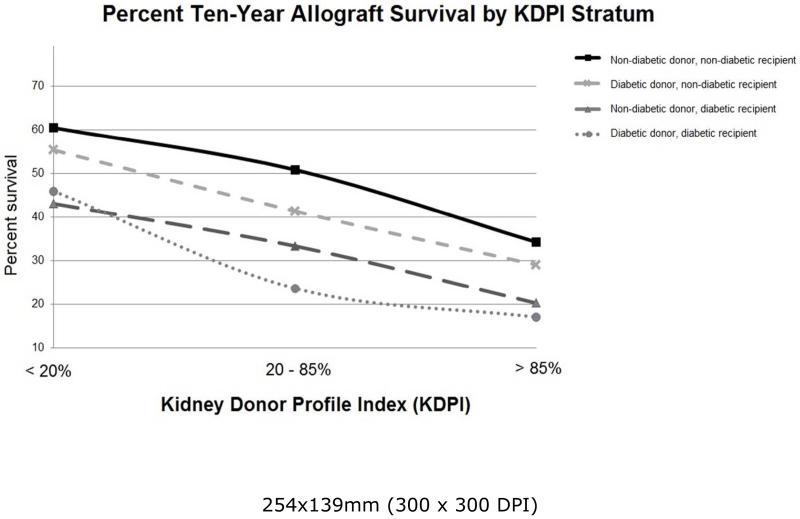
All-cause allograft failure for the overall cohort at one and two years by KDPI reflected the expected values calculated by the Organ Procurement and Transplantation Network for use in the new KAS (Figure 5; Tables S3a-S3d).5 Non-diabetic recipients of non-diabetic donor kidneys had the highest rate of allograft survival by KDPI (log rank p < 0.001 for the overall duration of follow up). Non-diabetic recipients of diabetic donor kidneys had the next highest rate of allograft survival by KDPI with similar one year allograft survival to the overall cohort, and worse two year, five year, and ten year allograft survival compared to the overall cohort. Diabetic recipients of diabetic donor kidneys had the lowest allograft survival stratified by KDPI.
Figure 5.
Kaplan-Meier estimates of ten-year allograft survival by KDPI stratum. Log rank and log rank test for trend p < 0.001
Results of Multivariable Regression Analysis
In adjusted analyses, diabetic donor kidneys were associated with increased risk of mortality compared to non-diabetic donor kidneys (Table 2; hazard ratio [HR] 1.19, 95% confidence interval [CI] 1.13-1.24). Recipient age > 40 years, male gender, African American race, dialysis vintage, repeat kidney transplant, positive HCV serostatus, and diabetes were associated with mortality. Diabetic donor kidneys were also associated with an increased risk of all-cause allograft loss compared to non-diabetic donor kidneys (Table 3; HR 1.21, 95% CI 1.16-1.26). ECD status and recipient characteristics including age > 40 years, male gender, African American race, panel reactive antibody (PRA) ≥ 30%, diabetes, and no induction immunosuppression therapy were all associated with allograft failure. There was significant interaction between donor and recipient diabetes status regarding mortality (likelihood ratio test p < 0.001) and all-cause allograft failure (likelihood ratio test p = 0.017).
Table 2.
Cox proportional hazards model for time to death in recipients of diabetic vs. non-diabetic donor kidneys
| Univariate Analysis | Multivariable Analysis* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | SE | z | p-value | 95% CI | HR | SE | z | p-value | 95% CI | |
| Donor Characteristics | ||||||||||
| Diabetes | 1.344 | 0.026 | 15.25 | < 0.001 | 1.294-1.396 | 1.186 | 0.027 | 7.48 | < 0.001 | 1.134-1.240 |
| ECD | 1.702 | 0.019 | 48.33 | < 0.001 | 1.667-1.739 | |||||
| Obese (BMI >=30) | 1.032 | 0.012 | 2.77 | 0.006 | 1.009-1.055 | |||||
| Recipient Characteristics | ||||||||||
| Age > 40 | 2.172 | 0.027 | 62.03 | < 0.001 | 2.120-2.226 | 1.995 | 0.031 | 44.44 | < 0.001 | 1.935-2.056 |
| Male | 1.182 | 0.011 | 18.16 | < 0.001 | 1.160-1.203 | 1.087 | 0.012 | 7.40 | < 0.001 | 1.063-1.111 |
| African American Race | 1.098 | 0.011 | 9.58 | < 0.001 | 1.077-1.119 | 1.069 | 0.013 | 5.47 | < 0.001 | 1.044-1.095 |
| Pre-Transplant Dialysis** | 1.024 | 0.001 | 18.91 | < 0.001 | 1.022-1.027 | 1.025 | 0.002 | 15.75 | < 0.001 | 1.022-1.028 |
| Time on Waitlist (days) | 1.000 | 0.000 | −4.59 | < 0.001 | 1.000-1.000 | |||||
| Prior Renal Transplant | 0.910 | 0.013 | −6.49 | < 0.001 | 0.885-0.936 | 1.154 | 0.022 | 7.36 | < 0.001 | 1.111-1.198 |
| HCV+ | 1.540 | 0.026 | 25.55 | < 0.001 | 1.489-1.591 | 1.426 | 0.028 | 18.01 | < 0.001 | 1.372-1.482 |
| Max PRA ≥30 | 0.964 | 0.011 | −3.18 | 0.001 | 0.943-0.986 | 0.954 | 0.015 | −3.03 | 0.002 | 0.926-0.983 |
| ≥ 1 HLA Mismatch | 1.155 | 0.017 | 9.94 | < 0.001 | 1.123-1.189 | |||||
| Pre-Transplant Diabetes** | 1.024 | 0.000 | 64.14 | < 0.001 | 1.024-1.025 | 1.020 | 0.000 | 49.16 | < 0.001 | 1.020-1.021 |
| Obese (BMI >=30) | 1.116 | 0.011 | 10.83 | < 0.001 | 1.094-1.138 | |||||
| Cold Ischemia Time | 1.008 | 0.001 | 16.41 | < 0.001 | 1.007-1.009 | |||||
| Delayed Graft Function | 1.662 | 0.016 | 52.54 | < 0.001 | 1.631-1.694 | |||||
| Acute Rejection at 1 Year | 1.416 | 0.017 | 28.98 | < 0.001 | 1.383-1.450 | |||||
| No Induction Immunosuppression |
1.134 | 0.010 | 13.70 | < 0.001 | 1.114-1.155 | |||||
Tacrolimus and the interaction term between tacrolimus and time were also included in the multivariable model
Included as an interaction term along with duration of dialysis or diabetes, as appropriate
Table 3.
Cox proportional hazards model for time to all-cause allograft failure in recipients of diabetic vs. non-diabetic donor kidneys
| Univariate Analysis | Multivariable Analysis* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | SE | z | p-value | 95% CI | HR | SE | z | p-value | 95% CI | |
| Donor Characteristics | ||||||||||
| Diabetes | 1.447 | 0.025 | 21.53 | < 0.001 | 1.399-1.497 | 1.210 | 0.024 | 9.67 | < 0.001 | 1.164-1.258 |
| ECD | 1.641 | 0.017 | 48.56 | < 0.001 | 1.608-1.674 | 1.573 | 0.019 | 37.92 | < 0.001 | 1.537-1.611 |
| Obese (BMI >=30) | 1.069 | 0.011 | 6.59 | < 0.001 | 1.048-1.091 | |||||
| Recipient Characteristics | ||||||||||
| Age > 40 | 1.181 | 0.011 | 17.33 | < 0.001 | 1.159-1.203 | 1.008 | 0.012 | 0.67 | 0.505 | 0.985-1.031 |
| Male | 1.115 | 0.009 | 13.09 | < 0.001 | 1.097-1.133 | 1.073 | 0.011 | 7.07 | < 0.001 | 1.052-1.094 |
| African American Race | 1.355 | 0.012 | 35.29 | < 0.001 | 1.333-1.379 | 1.333 | 0.014 | 28.21 | < 0.001 | 1.306-1.359 |
| Pre-Transplant Dialysis** | 1.029 | 0.001 | 25.72 | < 0.001 | 1.027-1.032 | |||||
| Time on Waitlist (days) | 1.000 | 0.000 | 4.89 | < 0.001 | 1.000-1.000 | |||||
| Repeat Renal Transplant | 1.048 | 0.013 | 3.69 | < 0.001 | 1.022-1.074 | |||||
| HCV+ | 1.543 | 0.024 | 27.86 | < 0.001 | 1.497-1.591 | 1.458 | 0.026 | 21.54 | < 0.001 | 1.409-1.509 |
| Max PRA ≥30 | 1.081 | 0.011 | 7.70 | < 0.001 | 1.060-1.103 | 1.119 | 0.014 | 8.97 | < 0.001 | 1.092-1.146 |
| ≥ 1 HLA Mismatch | 1.281 | 0.018 | 17.95 | < 0.001 | 1.246-1.316 | |||||
| Pre-Transplant Diabetes** | 1.015 | 0.000 | 39.03 | < 0.001 | 1.014-1.015 | 1.012 | 0.000 | 30.90 | < 0.001 | 1.012-1.013 |
| Obese (BMI >=30) | 1.150 | 0.011 | 15.31 | < 0.001 | 1.130-1.171 | |||||
| Cold Ischemia Time | 1.007 | 0.000 | 14.24 | < 0.001 | 1.006-1.008 | |||||
| Delayed Graft Function | 1.780 | 0.016 | 65.72 | < 0.001 | 1.750-1.811 | |||||
| Acute Rejection at 1 Year | 1.592 | 0.017 | 43.48 | < 0.001 | 1.559-1.626 | |||||
| No Induction Immunosuppression |
1.040 | 0.009 | 4.65 | < 0.001 | 1.023-1.058 | 1.116 | 0.012 | 10.57 | < 0.001 | 1.093-1.139 |
Tacrolimus and the interaction term between tacrolimus and time were also included in the multivariable model
Included as an interaction term along with duration of dialysis or diabetes, as appropriate
In the discordant mate-kidney recipient analysis, diabetic recipients of non-diabetic kidneys were associated with an increased risk of mortality (Table 4; HR 1.93, 95% CI 1.81-2.06) and all-cause allograft loss (Table 5; HR 1.45, 95% CI 1.37-1.53) compared to non-diabetic recipients of non-diabetic kidneys. Diabetic recipients of diabetic kidneys had an increased risk of mortality (Table 4; HR 1.53, 95% CI 1.22-1.93) and all-cause allograft loss (Table 5; HR 1.27, 95% CI 1.05-1.53) compared to non-diabetic recipients of diabetic kidneys. Recipient age > 40 years, dialysis vintage, and prior kidney transplant increased the risk for death; however recipient gender, race, and HCV serostatus did not influence mortality. African American race and PRA ≥ 30% increased the risk of all-cause allograft loss; however recipient age, gender, and use of induction immunosuppression did not influence allograft outcome.
Table 4.
Cox proportional hazards model for time to death in discordant diabetic vs. non-diabetic recipient pairs
| Univariate Analysis | Multivariable Analysis* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | SE | z | p-value | 95% CI | HR | SE | Z | p-value | 95% CI | |
| Non-Diabetic Donor | ||||||||||
| Diabetic Recipient | 1.990 | 0.045 | 30.72 | < 0.001 | 1.905-2.080 | 1.932 | 0.063 | 20.20 | < 0.001 | 1.812-2.060 |
| Non-Diabetic Recipient | REF | REF | ||||||||
| Diabetic Donor | ||||||||||
| Diabetic Recipient | 1.847 | 0.156 | 7.24 | < 0.001 | 1.564-2.180 | 1.532 | 0.179 | 3.64 | < 0.001 | 1.218-1.927 |
| Non-Diabetic Recipient | REF | REF | ||||||||
| Recipient Characteristics | ||||||||||
| Age > 40 | 1.837 | 0.085 | 13.21 | < 0.001 | 1.679-2.011 | 1.928 | 0.125 | 10.12 | < 0.001 | 1.698-2.189 |
| Male | 1.118 | 0.036 | 3.47 | 0.001 | 1.050-1.191 | 1.025 | 0.046 | 0.54 | 0.591 | 0.937-1.120 |
| African American Race | 0.996 | 0.038 | −0.12 | 0.907 | 0.924-1.072 | 0.954 | 0.052 | −0.87 | 0.386 | 0.858-1.061 |
| Pre-Transplant Dialysis** | 1.058 | 0.006 | 9.30 | < 0.001 | 1.046-1.071 | 1.052 | 0.009 | 5.96 | < 0.001 | 1.035-1.070 |
| Time on Waitlist (days) | 1.000 | 0.000 | 2.85 | 0.004 | 1.000-1.000 | |||||
| Prior Renal Transplant | 1.047 | 0.059 | 0.83 | 0.409 | 0.938-1.169 | 1.200 | 0.102 | 2.16 | 0.031 | 1.017-1.417 |
| HCV+ | 0.647 | 0.228 | −1.24 | 0.216 | 0.324-1.291 | 1.090 | 0.116 | 0.81 | 0.417 | 0.885-1.343 |
| Max PRA ≥30 | 1.162 | 0.051 | 3.41 | 0.001 | 1.066-1.267 | |||||
| ≥ 1 HLA Mismatch | 1.011 | 0.071 | 0.16 | 0.873 | 0.881-1.160 | |||||
| Obese (BMI >=30) | 1.036 | 0.036 | 1.03 | 0.304 | 0.968-1.109 | |||||
| Cold Ischemia Time | 1.007 | 0.003 | 2.83 | 0.005 | 1.002-1.012 | |||||
| Delayed Graft Function | 1.942 | 0.043 | 30.32 | < 0.001 | 1.486-1.734 | |||||
| Acute Rejection at 1 Year | 1.396 | 0.077 | 6.03 | < 0.001 | 1.252-1.555 | |||||
| No Induction Immunosuppression |
0.995 | 0.039 | −0.12 | 0.906 | 0.921-1.076 | |||||
Tacrolimus and the interaction term between tacrolimus and time were also included in the multivariable model
Included as an interaction term along with duration of dialysis or diabetes, as appropriate
Table 5.
Cox proportional hazards model for time to all-cause allograft failure in discordant diabetic vs. non-diabetic recipient pairs
| Univariate Analysis | Multivariable Analysis* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | SE | z | p-value | 95% CI | HR | SE | z | p-value | 95% CI | |
| Non-Diabetic Donor | ||||||||||
| Diabetic Recipient | 1.494 | 0.030 | 19.73 | < 0.001 | 1.436-1.555 | 1.445 | 0.041 | 13.07 | < 0.001 | 1.367-1.527 |
| Non-Diabetic Recipient | REF | REF | ||||||||
| Diabetic Donor | ||||||||||
| Diabetic Recipient | 1.349 | 0.099 | 4.06 | < 0.001 | 1.168-1.558 | 1.269 | 0.120 | 2.52 | 0.012 | 1.054-1.528 |
| Non-Diabetic Recipient | REF | REF | ||||||||
| Recipient Characteristics | ||||||||||
| Age > 40 | 1.033 | 0.039 | 0.86 | 0.390 | 0.959-1.113 | 1.019 | 0.051 | 0.37 | 0.712 | 0.923-1.125 |
| Male | 1.092 | 0.032 | 3.02 | 0.003 | 1.031-1.156 | 1.061 | 0.042 | 1.50 | 0.134 | 0.982-1.146 |
| African American Race | 1.197 | 0.041 | 5.29 | < 0.001 | 1.120-1.280 | 1.250 | 0.056 | 4.96 | < 0.001 | 1.145-1.366 |
| Pre-Transplant Dialysis** | 1.054 | 0.006 | 9.45 | < 0.001 | 1.042-1.065 | |||||
| Time on Waitlist (days) | 1.000 | 0.000 | 3.07 | 0.002 | 1.000-1.000 | |||||
| Repeat Renal Transplant | 1.180 | 0.059 | 3.30 | 0.001 | 1.069-1.301 | |||||
| HCV+ | 0.941 | 0.281 | −0.20 | 0.838 | 0.524-1.690 | 1.114 | 0.099 | 1.22 | 0.222 | 0.936-1.326 |
| Max PRA ≥30 | 1.165 | 0.046 | 3.90 | < 0.001 | 1.079-1.258 | 1.226 | 0.066 | 3.80 | < 0.001 | 1.104-1.361 |
| ≥ 1 HLA Mismatch | 1.139 | 0.073 | 2.02 | 0.043 | 1.004-1.292 | |||||
| Obese (BMI 7 gt;=30) | 1.127 | 0.035 | 3.83 | < 0.001 | 1.060-1.198 | |||||
| Cold Ischemia Time | 1.006 | 0.002 | 2.56 | 0.010 | 1.001-1.010 | |||||
| Delayed Graft Function | 1.770 | 0.063 | 16.00 | < 0.001 | 1.650-1.898 | |||||
| Acute Rejection at 1 Year | 1.782 | 0.089 | 11.59 | < 0.001 | 1.616-1.965 | |||||
| No Induction Immunosuppression |
0.987 | 0.036 | −0.37 | 0.715 | 0.919-1.060 | 1.083 | 0.054 | 1.61 | 0.108 | 0.983-1.193 |
Tacrolimus and the interaction term between tacrolimus and time were also included in the multivariable model
Included as an interaction term along with duration of dialysis or diabetes, as appropriate
The results of both multivariate analyses were unchanged when re-analyzed using death-censored allograft failure as the outcome (Tables S1a-S1b). The results of the overall cohort analyses were unchanged after stratifying by era (1994-2003 and 2004-2014; Table S2a-S2b); there was a similar degree of effect observed but insufficient power to detect differences in the mate-kidney analyses (Tables S2c-S2d).
DISCUSSION
This analysis of kidney transplant recipients spanning from 1994 to 2014 is the largest study to date evaluating the impact of donor diabetes on allograft and patient survival, as well as the first study to thoroughly investigate the interplay between donor and recipient diabetes status with regard to long-term outcomes. Our study demonstrates that the impact of donor diabetes status is dependent on recipient diabetes status; diabetic donor kidneys transplanted into diabetic recipients are associated with the highest risk of all-cause allograft loss and patient mortality compared to all other donor-recipient combinations of diabetes status. To control for unmeasured confounding and minimize donor allocation bias based on donor diabetes status, we performed a discordant mate-kidney recipient analysis in which one recipient was diabetic and the mate-kidney recipient was non-diabetic. We observed that diabetic recipients had greater mortality than non-diabetic recipients. Although diabetic donor kidneys fared worse in the primary analysis, allograft outcomes in the discordant mate-kidney analysis were similar in non-diabetic recipients of diabetic donor kidneys and diabetic recipients of non-diabetic donor kidneys. The use of a sub-cohort in the mate-kidney analysis does somewhat limit the generalizability of the results to the overall transplant population; that said, the allograft half-life in the overall cohort is also similar in non-diabetic recipients of diabetic donor kidneys and diabetic recipients of non-diabetic donor kidneys. This suggests that the exposure of kidneys to an environment of diabetes, either prior to (in the donor) or post-transplant (in the recipient), leads to comparably adverse allograft outcomes. Furthermore, this negative effect of diabetes on allograft survival is magnified in kidneys that are exposed to a diabetic milieu in both the donor and recipient settings.
The results of our study differ from previous studies evaluating outcomes of diabetic donor kidneys. Mohan et al. observed no difference in death-censored allograft survival between diabetic and non-diabetic recipients of diabetic donor kidneys.1 In a propensity score-matched study, Ahmad et al. observed no difference in mortality between diabetic donor and non-diabetic donor kidneys, and very small effect size regarding death-censored allograft failure.10 However, these studies both had a substantially smaller sample size and shorter duration of follow up than our study, with the latest transplant date in their analyses occurring in 2004. Since that time, the number of diabetic donor transplants has more than doubled (from 2 528 per decade to 6 175 per decade), and the number of diabetic recipients of diabetic donor kidneys almost quadrupled (from 685 per decade to 2 423 per decade). Thus, our study encompasses an extraordinarily different landscape of diabetic donor transplantation that has evolved over the past decade.
Another notable finding of our study is that younger recipients of diabetic donor kidneys have worse allograft outcomes compared to older recipients of non-diabetic kidneys. This is in contrast to the existing literature; younger recipient age is typically at least somewhat protective against adverse allograft outcomes.2 In accordance with findings in previous studies, our discordant mate-kidney recipient analyses demonstrated that African American race and allosensitization were associated with increased risk of allograft failure.14-17 Similarly, our findings that age > 40 years, dialysis vintage, and repeat kidney transplant were associated with mortality corroborate prior observations.18 Overall, our findings support that patients over age 65 have the least relative burden of adverse allograft outcomes from being transplanted with diabetic donor kidneys compared to younger recipients.
When contemporized to account for KDPI, our study demonstrates that diabetic recipients of diabetic donor kidneys continue to have the worst allograft outcomes, followed by diabetic recipients of non-diabetic donor kidneys. A recent study demonstrated greater long-term survival following transplant with high-KDPI kidneys (KDPI 71-80%) in both diabetic and non-diabetic recipients compared to remaining on the waitlist until receiving a lower KDPI kidney, particularly among recipients >age 50 and those with higher than average wait times.19 However, this and other previous studies investigating the impact of KDPI on recipient outcomes have not specifically evaluated differences based on donor and recipient diabetes status.7, 19-21 This information will allow us to better inform patients of underlying implications of accepting these organs based on the recipients’ risk factors, outside of that information provided by the KDPI alone.
Our study is strengthened by the fact that it is the largest study evaluating diabetic donor outcomes to date, comprising a total of 161 629 kidney recipients. As this is large-scale registry data, an extensive range of recipient and donor-related characteristics were available to be taken into consideration in the analyses, permitting evaluation of broad trends in patient and allograft survival. Our novel paired study design permitted thorough evaluation of recipient factors contributing to worse outcomes after effectively controlling for unmeasured donor characteristics and minimizing organ allocation bias.
The study is limited by our use of registry data. Registry data, while extensive, is also incomplete. We are limited by the scope of recipient comorbidities collected by United Network of Organ Sharing (UNOS), as well as by the completeness and accuracy to which that data is reported by the transplant centers. For example, the cause of allograft failure was missing in a significant number of patients. Procurement kidney biopsy data was also inconsistently reported (only 30% of donor kidneys had biopsies performed at the time of transplant) and did not provide any information regarding diabetic changes in donor kidneys. Furthermore, the UNOS dataset does not collect follow-up biopsy data to permit assessment of histological progression, or potential regression, following transplant with diabetic kidneys. Additionally, new onset diabetes after transplant is not reliably captured by the dataset, and may substantially influence allograft outcomes particularly among recipients of diabetic organs. Furthermore, although poor glycemic control and duration of diabetes are known contributors to the development of adverse outcomes (at least among type 1 diabetics in the general, non-transplant population22), information on donor diabetes severity, including renal manifestations, is not available in the UNOS dataset. By performing a mate-kidney analysis, this limitation is circumvented in a far more robust manner than would be expected from a propensity-matching strategy utilizing donor characteristics reported in the UNOS dataset.
In the past, the presence of diabetes in the donor was considered a relative contraindication to transplantation. The precipitous rise in the number of diabetic donor kidneys utilized over the past twenty years has been a rational and necessary response to the increasing demand for donor organs.23 Our findings carry important implications for patients considering accepting diabetic donor kidneys, as a supplement to the KDPI scoring system. Patients will benefit from increased counseling regarding specific risk factors for adverse outcomes, balanced with the risks associated with remaining on the waitlist. Further studies are needed to evaluate if enhanced monitoring or specific interventions such as strict glycemic control or renin-angiotensin system blockade can improve outcomes in diabetic recipients of diabetic donor kidneys.
METHODS
Data Source
We performed a retrospective analysis of national registry data collected by UNOS. The study was approved under exempt status by the Institutional Review Board at the University of Pennsylvania (protocol # 821021).
Subjects
The cohort was restricted to patients who were transplanted between March 11, 1994 (the first recorded date of a diabetic donor kidney transplant) and December 31, 2013. Patient follow up was through March 31, 2014. We only included patients who were adult recipients (≥ age 18), because parameters for pediatric transplant and recipient risk factors vary significantly from those in adults. Additionally, in order to perform comparable analyses across all donor and recipient groups, only kidney transplants from deceased donors were included in the study.
Variables and Covariates
The primary outcomes in the study were all-cause mortality and all-cause allograft failure. Death-censored allograft failure was also evaluated (results are included in the supplement). Mortality and allograft loss data provided in the UNOS dataset were used to determine outcomes. Patient survival was corroborated by linkage to the Social Security Master Death File. Recipient diabetes status was reported in the database as “DIAB,” and donor diabetes status was reported as “DIABETES_DON.” The “DGN-TCR” variable in the database, which defines diagnostic etiology of recipient end stage renal disease, does provide additional information regarding diabetes status in some patients. There were a small number of discrepancies between information provided from in “DGN_TCR” and “DIAB”; patients with discrepancies were excluded from the study (38 total patients). KDPI was calculated using the scaled Kidney Donor Risk Index for 2014.6, 24 Recipient sensitization was designated as PRA > 30%.25 Locally weighted scatterplot smoothing was performed on recipient age, and demonstrated a clear cut-point for recipient age regarding increased mortality and allograft failure at 40 years.26 The same age cut-point has been utilized in existing literature.27
Statistical Analysis
Statistical analyses were performed using STATA version 13.0 (Statacorp LP, College Station, TX) with 2-sided hypothesis testing and p-value of < 0.05 as the criteria for statistical significance. Descriptive statistics (mean, median, and proportion) were used to describe baseline donor and recipient clinical and demographic characteristics comparing all diabetic and non-diabetic donors, as well as discordant diabetic and non-diabetic recipient pairs of kidneys from the same donor. Continuous variables were compared using Student’s t test, or ranksum test for non-normally distributed variables. Categorical and binary variables were compared using chi-square test. For the mate-kidney analysis paired descriptive statistics were performed.
In our primary analysis, we compared outcomes of non-diabetic donor kidneys versus diabetic donor kidneys. In our secondary analysis, we compared outcomes of discordant recipient pairs of kidneys from the same donor, where one recipient was diabetic and the mate-kidney recipient was non-diabetic. Kaplan Meier curves were generated and log rank testing was performed to assess for equality of survival distributions.28 Cox proportional hazards regression was used to estimate HRs and 95% CIs. We assessed for confounding by evaluating for a change in the unadjusted HR of the outcome of interest in our exposure categories by more than 10%; none of the covariates met the definition for confounding. For the multivariable regression, we selected variables a priori that were known to be risk factors for mortality or allograft loss based on clinical judgment and previously published literature.14-18 Pre-transplant dialysis and duration of dialysis vintage, as well as recipient diabetes and diabetes duration, were included as interaction terms. For the secondary paired analyses, all of the models were stratified by donor identification number.
The proportional hazards assumption was assessed via weighted versions of Kaplan-Meier curves using log-log plots as well as statistical testing and graphical displays based on the Schoenfeld and scaled Schoenfeld residuals. If a variable violated the proportional hazards assumption on statistical testing (i.e. p < 0.05), but had a parallel appearance on visual inspection of the log-log plot, it was retained in the model without adjustment; this discrepancy was attributed to the large size of the dataset.29 One variable, discharge immunosuppression, did not meet the proportional hazards assumption, as patterns of tacrolimus use changed over the course of the study period. This variable was included in the multivariable analyses with an interaction term with time in order to address changes in the effect size over time.
We also created survival tables stratifying all-cause allograft survival for the overall cohort by KDPI allocation group (KDPI < 20%, KPDI 20-85%, and KDPI >85%).5 We created a scatterplot of the allograft survival rate by KDPI allocation group, comparing each stratum of donor and recipient diabetes exposure.
Handling of Covariate Missingness
Subjects were excluded from the study in whom donor diabetes status was missing (<1%). Most covariates included in the multivariate models were < 5% incomplete. We performed multiple imputation of all missing covariates by the chained equations method, and found no difference in the results (Tables S4a-S4d). Etiology of allograft failure and cause of death were missing in >50% of patients; thus, we omitted this information.
Supplementary Material
Footnotes
DISCLOSURE
All authors declared no competing interests.
REFERENCES
- 1.Mohan S, Tanriover B, Ali N, et al. Availability, utilization and outcomes of deceased diabetic donor kidneys; analysis based on the UNOS registry. Am J Transplant. 2012;12:2098–2105. doi: 10.1111/j.1600-6143.2012.04167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ojo AO, Hanson JA, Meier-Kriesche H, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J Am Soc Nephrol. 2001;12:589–597. doi: 10.1681/ASN.V123589. [DOI] [PubMed] [Google Scholar]
- 3.Schold JD, Meier-Kriesche HU. Which renal transplant candidates should accept marginal kidneys in exchange for a shorter waiting time on dialysis? Clin J Am Soc Nephrol. 2006;1:532–538. doi: 10.2215/CJN.01130905. [DOI] [PubMed] [Google Scholar]
- 4.Port FK, Bragg-Gresham JL, Metzger RA, et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation. 2002;74:1281–1286. doi: 10.1097/00007890-200211150-00014. [DOI] [PubMed] [Google Scholar]
- 5.Friedewald JJ, Samana CJ, Kasiske BL, et al. The kidney allocation system. Surg Clin North Am. 2013;93:1395–1406. doi: 10.1016/j.suc.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Rao PS, Schaubel DE, Guidinger MK, et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation. 2009;88:231–236. doi: 10.1097/TP.0b013e3181ac620b. [DOI] [PubMed] [Google Scholar]
- 7.Israni AK, Salkowski N, Gustafson S, et al. New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol. 2014;25:1842–1848. doi: 10.1681/ASN.2013070784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Network OPaT . Allocation Calculators. 2015. Estimated Post Transplant Survival Calculator. [Google Scholar]
- 9.Schold JD, Buccini LD, Reese PP, et al. Effect of dialysis initiation for preemptively listed candidates in the revised kidney allocation policy. Am J Transplant. 2014;14:2855–2860. doi: 10.1111/ajt.12957. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad M, Cole EH, Cardella CJ, et al. Impact of deceased donor diabetes mellitus on kidney transplant outcomes: a propensity score-matched study. Transplantation. 2009;88:251–260. doi: 10.1097/TP.0b013e3181ac68a9. [DOI] [PubMed] [Google Scholar]
- 11.Becker YT, Leverson GE, D’Alessandro AM, et al. Diabetic kidneys can safely expand the donor pool. Transplantation. 2002;74:141–145. doi: 10.1097/00007890-200207150-00027. [DOI] [PubMed] [Google Scholar]
- 12.Abouna GM, Adnani MS, Kumar MS, et al. Fate of transplanted kidneys with diabetic nephropathy. Lancet. 1986;1:622–623. doi: 10.1016/s0140-6736(86)92849-7. [DOI] [PubMed] [Google Scholar]
- 13.Abouna GM, Al-Adnani MS, Kremer GD, et al. Reversal of diabetic nephropathy in human cadaveric kidneys after transplantation into non-diabetic recipients. Lancet. 1983;2:1274–1276. doi: 10.1016/s0140-6736(83)91151-0. [DOI] [PubMed] [Google Scholar]
- 14.Fan PY, Ashby VB, Fuller DS, et al. Access and outcomes among minority transplant patients, 1999-2008, with a focus on determinants of kidney graft survival. Am J Transplant. 2010;10:1090–1107. doi: 10.1111/j.1600-6143.2009.03009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gondos A, Dohler B, Brenner H, et al. Kidney graft survival in Europe and the United States: strikingly different long-term outcomes. Transplantation. 2013;95:267–274. doi: 10.1097/TP.0b013e3182708ea8. [DOI] [PubMed] [Google Scholar]
- 16.Narayanan M, Pankewycz O, Shihab F, et al. Long-term outcomes in African American kidney transplant recipients under contemporary immunosuppression: a four-yr analysis of the Mycophenolic acid Observational REnal transplant (MORE) study. Clin Transplant. 2014;28:184–191. doi: 10.1111/ctr.12294. [DOI] [PubMed] [Google Scholar]
- 17.Faravardeh A, Eickhoff M, Jackson S, et al. Predictors of graft failure and death in elderly kidney transplant recipients. Transplantation. 2013;96:1089–1096. doi: 10.1097/TP.0b013e3182a688e5. [DOI] [PubMed] [Google Scholar]
- 18.Cardinal H, Hebert MJ, Rahme E, et al. Modifiable factors predicting patient survival in elderly kidney transplant recipients. Kidney Int. 2005;68:345–351. doi: 10.1111/j.1523-1755.2005.00410.x. [DOI] [PubMed] [Google Scholar]
- 19.Massie AB, Luo X, Chow EK, et al. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am J Transplant. 2014;14:2310–2316. doi: 10.1111/ajt.12830. [DOI] [PubMed] [Google Scholar]
- 20.Gandolfini I, Buzio C, Zanelli P, et al. The Kidney Donor Profile Index (KDPI) of marginal donors allocated by standardized pretransplant donor biopsy assessment: distribution and association with graft outcomes. Am J Transplant. 2014;14:2515–2525. doi: 10.1111/ajt.12928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernandez RA, Malek SK, Milford EL, et al. The combined risk of donor quality and recipient age: higher-quality kidneys may not always improve patient and graft survival. Transplantation. 2014;98:1069–1076. doi: 10.1097/TP.0000000000000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Boer IH, Sun W, Cleary PA, et al. Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. N Engl J Med. 2011;365:2366–2376. doi: 10.1056/NEJMoa1111732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schold J, Srinivas TR, Sehgal AR, et al. Half of Kidney Transplant Candidates Who Are Older than 60 Years Now Placed on the Waiting List Will Die before Receiving a Deceased-Donor Transplant. Clinical Journal of the American Society of Nephrology. 2009;4:1239–1245. doi: 10.2215/CJN.01280209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Organ Procurement and Transplantation Network . KDRI to KDPI Mapping Table. 2014. [Google Scholar]
- 25.Susal C, Opelz G. Kidney graft failure and presensitization against HLA class I and class II antigens. Transplantation. 2002;73:1269–1273. doi: 10.1097/00007890-200204270-00014. [DOI] [PubMed] [Google Scholar]
- 26.Goodall C. A survey of smoothing techniques. In: Long JFaJS., editor. Modern Methods of Data Analysis. Sage; Newbury Park, CA: 1990. pp. 126–176. [Google Scholar]
- 27.Merion RM, Ashby VB, Wolfe RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294:2726–2733. doi: 10.1001/jama.294.21.2726. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Statist Assoc. 1958;53:457–481. [Google Scholar]
- 29.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model (Statistics for Biology and Health) Springer; New York: 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.