Abstract
We investigated the relationship between physical activity and physical function on the risk of falls over time in a cohort of Mexican American adults aged 75 and older from the Hispanic Established Population for the Epidemiologic Study of the Elderly (H-EPESE). Participants were divided into four groups according to the level of physical activity and physical function: low physical activity and low physical function (n=453); low physical activity and high physical function (n=54); high physical activity and low physical function (n=307); and high physical activity and high physical function (n=197). Using generalized linear equation estimation, we showed that participants with high physical activity and low physical function had a greater fall risk, overtime, followed by the high physical activity and high physical function group. Participants seldom took part in activities that improve physical function. To prevent falls, modifications to physical activity should be made for older Mexican Americans.
INTRODUCTION
Reducing the number of falls among older adults is a public health priority in the United States (Lundebjerg et al., 2001). In 2013, approximately 2.5 million adults over the age of 65 had a nonfatal fall (CDC, 2014). Nonfatal falls are associated with injuries, fractures, and hospitalization (Lundebjerg et al., 2001; Mertz, Lee, Sui, Powell, & Blair, 2010; Nowalk, Prendergast, Bayles, D’Amico, & Colvin, 2001). Falls may also lead to death, with an estimated 12,700 older adults dying from an unintentional fall each year (Stevens, Thomas, & Sogolow, 2007). To improve the health and well-being of older adults, effective fall prevention strategies are needed (Chang et al., 2004; Day et al., 2002; Lundebjerg et al., 2001; Michael et al., 2010; Nelson et al., 2007).
One strategy that is currently recommended by the American Geriatrics Society in a report from the Panel on Falls Prevention, is sustained physical activity, defined as “any bodily movement produced by skeletal muscles that results in energy expenditure” (Lundebjerg et al., 2001). Several studies have shown that physical activity is an effective therapeutic approach to prevent falls (Chang et al., 2004; Day et al., 2002; Kendrick et al., 2014; Michael et al., 2010; Nelson et al., 2007). Although physical activity is strongly recommended to prevent falls in older adults, the evidence for this is contradictory (B. Jefferis et al., 2015; Mertz et al., 2010; Peeters et al., 2010). For example, in an analysis of 1,680 older men, recurrent fallers took fewer steps, participated in fewer minutes of activity, and had more minutes of sedentary time than non-fallers (Jefferis et al., 2014). The authors suggested that “inactivity may lead to falls” (Jefferis et al., 2014). Conversely, secondary data analysis of the Aerobics Center Longitudinal study found that adults over 65 years of age were significantly more likely to fall while walking, compared to adults under the age of 45 (Mertz et al., 2010), suggesting that walking activities might increase fall risk in older adults. Findings from the Longitudinal Aging Study Amsterdam showed that playing sports, high intensity activities, and high mechanical strain activities were significantly associated with fall re-occurrence in older adults (Peeters et al., 2010), while non-recurrent fallers were less likely to do strength-building activities and were more likely to do heavy housework, and walk regularly (Peeters et al., 2010).
The exercise prescription (the frequency of activity and the types of activities) to maximize the benefit of physical activity is not yet well established in older adults (Lundebjerg et al., 2001; Nowalk et al., 2001; Vu, Weintraub, & Rubenstein, 2005). It is theorized that physical activity prevents falls by increasing an individual’s physical function level through balance and strengthening exercises (Lobo, 2012; Mangani et al., 2008; Tuunainen, Rasku, Jäntti, & Pyykkö, 2014). Increasing the level of physical function has been associated with reduction of an individual’s limitations in activities of daily living and with increasing the level of lower extremity performance (Guralnik et al., 1994). Unlike results based on the overall level of physical activity, there is consistent evidence that improvements in strength and balance result in a decreased risk of falls (L. Clemson et al., 2012; Day et al., 2002; Kendrick et al., 2014; Lobo, 2012; Lundebjerg et al., 2001; Mangani et al., 2008; Nelson et al., 2007). In a randomized controlled trial, where the participants were randomized to two exercise programs (Nowalk et al., 2001), the authors did not find significant associations between physical activity type or frequency and falls over a 2-year program, but they found that participants that fell had significant physical function limitations (Nowalk et al., 2001). A study using a strength and balance training program that was integrated into everyday activities yielded 1.66 falls per person years compared to 2.28 falls per person years in individuals that received light flexibility exercises (L. Clemson et al., 2012). This intervention found a 31% reduction in the rate of falls for participants, despite them being relatively physically active at baseline.
There is data in the literature that suggests that assessing an individual’s physical activity level and physical function level is important for evaluating the risk of falls in older adults. However, only a few studies have examined the combined effect of physical activity and physical function on the risk of falls (Hu, Xia, Jiang, Zhou, & Li, 2015; Ward et al., 2015). In a study of 3,043 community-dwelling women, Hu et. al. (2015) found that high physical activity and good balance ability were both beneficial in decreasing falls. However, the authors did not compare the influence of low and high physical activity and functional levels on the rate of falls.
The purpose of our study was to investigate the association between physical activity levels, measured with the Physical Activity Scale for Elderly (PASE), and physical function levels, measured with the Short Physical Performance Battery (SPPB), on the risk of falls over a six-year period among older Mexican Americans aged 75 years and older who participated in a study of frailty. We hypothesized that older Mexican Americans with high levels of physical activity and high levels of physical function are at less risk of having a fall over time.
METHODS
Data were from the Hispanic Established Populations for Epidemiologic Study of the Elderly (H-EPESE), an ongoing longitudinal study of Mexican Americans aged 65 and older, at baseline, residing in Texas, New Mexico, Colorado, Arizona, and California. Participants in the original sample were selected using area probability sampling procedures that involved selecting counties, census tracts, and households within selected census tracts. Further details on sampling procedures, assessment strategies, and participant characteristics are available and archived at the National Archive of Computerized Data on Aging (Markides, Ray, Angel, & Espino, 2009).
The original H-EPESE sample consisted of 3,050 participants interviewed in 1993/94 at baseline and continues to be followed. In 2004/05, 1,167 participants aged 75 and older from the original cohort were re-interviewed. A new cohort of 902 respondents aged 75 and older was added in 2004/05 using sampling procedures similar to those used in 1993/94. Both cohorts received identical evaluations at baseline and follow-up (sociodemographic characteristics, health conditions, psychosocial characteristics, blood pressure, anthropometric measures, and physical function measures). In 2005/06 a subsample aged 75 and older (n = 1,013) from the 2004/05 H-EPESE cohort was randomly selected to study frailty (K. J. Ottenbacher et al., 2009). The inclusion criteria were the ability to respond to questions and to complete performance tasks essential to the frailty index (e.g., a short walk). Proxy respondents (N=2) were excluded from this study.
The final sample included 1,011 participants with complete information on physical activity and physical function measures at baseline (2004/05). Two follow-up assessments were conducted in 2007/08 and 2010/11. Participants were examined in their homes by raters who were trained on interviewing methods and performance-based assessments. Interviews were conducted in English and Spanish, based on the respondent’s preference. At the end of follow-up, 624 participants were re-interviewed (538 in person and 86 via proxy), 101 (10%) were lost to follow-up, and 288 (28.4%) were confirmed dead through the National Death Index and reports from relatives. Participants with missing data on some of the covariates at baseline (N=196) were significantly more likely to have a lower Mini-Mental State Examination score (mean=19.7, standard deviation =7.9, p<0.01), and to report stroke (p=0.01), cancer (p=0.01), Parkinson’s disease (p=0.02), diabetes (p<0.01), hip fracture (p=0.03), emphysema (p<0.01), high depressive symptoms (p<0.01), distance vision impairment (p=0.02), and history of falls (p<0.01) compared with those without missing information.
The study protocol was approved by the university’s Institutional Review Board. Informed consent was obtained at the time the subjects were interviewed.
Measures
Independent Variable
Physical activity was measured with the PASE scale. PASE is a well-established and a validated instrument used to measure physical activity in older adults (Washburn, McAuley, Katula, Mihalko, & Boileau, 1999; Washburn, Smith, Jette, & Janney, 1993). Physical activity was measured from the frequency of activities completed in the previous week across three subscales: household, occupational, and leisure activity. Household activities included lawn work, gardening, housework, and caring for others. Occupational activity was determined from the hours of sedentary or active work. Finally, leisure physical activity included walking, sporting activity, muscle strength, and endurance. A score for each subscale (household, occupational, and leisure) and a total physical activity score was derived from an empirical weighting system (Washburn et al., 1999). For data analysis, we followed an established method to separate PASE scores into categories (A. J. Ottenbacher et al., 2012). Participants below the median PASE score (63), were categorized as low physical activity, and those above the median were considered to have high physical activity. For example, a person that participated in walking outside for less than an hour on most days of the week, and who completed light housework and gardening, would have a PASE score of 53.6 and be categorized as low physical activity. Whereas, a person who was physically active doing volunteer work 15 hours a week, was participating in moderate sporting activities for less than an hour on most days of the week, and completed light housework would have a PASE score of 79.9 and be categorized as high physical activity.
Physical function was determined using the SPPB. The SPPB includes three lower body extremity tests (Freiberger et al., 2012; Guralnik, Ferrucci, Simonsick, Salive, & Wallace; Guralnik et al.). These were: standing balance, walking speed, and repeated chair-stands. Standing balance was assessed through the performance of a progression of balance stances that increased in difficulty. Walking speed was assessed by measuring the time (nearest second) for the subjects to walk 8 feet. The time for repeated chair-stands (5 in total) was estimated to the nearest tenth of a second. Each lower body test was scored from 0 to 4, with 0 reflecting the inability to complete the test and 1–4 reflecting quartiles relating to task completion (higher score indicating higher performance). The final SPPB score was calculated by combining the results of the three tests. The combined scores ranged from a low of 0 to a high of 12, with higher scores indicating better physical functioning. Participants were divided into two categories: high physical function (SPPB score ≥ 9) and low physical function (SPPB score<9) (Guralnik et al., 1994).
To capture whether high level of physical activity and high level of physical function is associated with less risk of having falls over time, participants were divided into four groups: low physical activity (PASE < 63) and low physical function (SPPB score<9) (n=453), low physical activity (PASE < 63) and high physical function (SPPB score ≥ 9) (n=54), high physical activity (PASE ≥ 63) and low physical function (SPPB score < 9) (n=307), and high physical activity (PASE ≥ 63) and high physical function (SPPB score ≥ 9) (n=197).
Dependent Variable
Falls were determined from in-person interviews at baseline in 2004/2005 and at two follow up time points (2007/2008 and 2010/2011). At the time of the interview, participants were asked “during the past 12 months, how many times did you fall and land on the floor or ground?” (no falls, one fall, two falls, or three or more falls). Falls status was categorized as having no falls versus one or more falls..
Covariates
Covariates included variables identified in previous research as associated with risk of falls in older adults (Friedman, Munoz, West, Rubin, & Fried, 2002; Lundebjerg et al., 2001; Mertz et al., 2010; Tuunainen et al., 2014). Sociodemographic variables included age (as continuous and categorized as 75 to < 80, 80 to <85, and ≥ 85 years), gender, years of formal education, and marital status (married versus unmarried). Body mass index (BMI) was calculated by dividing weight in kilograms by height in meters squared (kg/m2). The Center for Epidemiologic Studies Depression Scale (CES-D) was used to determine depressive symptoms (Andresen, Malmgren, Carter, & Patrick, 1994). The Mini Mental State Examination (MMSE) was used to determine cognitive function (Folstein, Folstein, & McHugh, 1975). Near and distance vision impairment was determined by self-reported difficulty seeing at an arm’s length away and across the street, respectively. Frailty was assessed using a modified version of the construct described by Fried et al. (Al Snih et al., 2009; Fried, 1999). A sum total of present medical conditions was used to assess comorbidities. The following diseases and conditions were considered present if a doctor ever told the participant that he or she had a stroke, heart attack, cancer, Parkinson’s disease, hypertension, diabetes, hip fracture, emphysema, or arthritis.
Statistical Analysis
Chi-square, analysis of variance (ANOVA), and post hoc Tukey tests were used to examine the distribution of covariates for participants by physical activity and physical function groups at baseline. The general estimate equation (GEE) was fitted using PROC GENMOD in SAS to determine the association between physical activity and physical function groups and falls (one or more) over 6 years. All variables were analyzed as time-dependent covariates except age, gender, education, physical activity, and physical function. Two models were constructed to test the relationship between baseline physical activity and physical function groups and falls over a six-year period. Model 1 included time, age, gender, marital status, years of formal education, falls at baseline, physical activity and physical function groups, and the interaction term between group assignment and time. Model 2 included all variables in Model 1 along with comorbidities, distant and near vision impairment, BMI, cognitive function, high depressive symptoms, and frailty status. With these analyses we did not find any interaction effects between variables. Additional analyses were conducted to examine the association between physical activity and physical function groups and having 2 or more falls over time. All analyses were performed using SAS for Windows, version 9.3 (SAS Institute, Inc., Cary, NC) and significance was determined with alpha=0.05.
RESULTS
The mean age of participants at baseline was 82.3±4.6; 63.2% were female; 41.7% were married; and 36.4% experienced a fall within the previous year at baseline assessment. There was no significant difference in age between those with a history of falls at baseline (82.7± 4.7 years) and those without (82.0±4.5 years). The mean years of education were 4.9±3.9 years, and the mean BMI was 27.4±5.0 kg/m2. On average, participants had 2.1±1.2 comorbidities. The most prevalent comorbidities were hypertension (67.3%), arthritis (63.1%), and diabetes (35.0%). Fourteen percent of the participants were classified as frail. The mean MMSE score was 21.20±7.03, indicating that participants were within the range of cognitive impaired or poor cognition but not dementia (Folstein et al., 1975; Leveille et al., 1998).
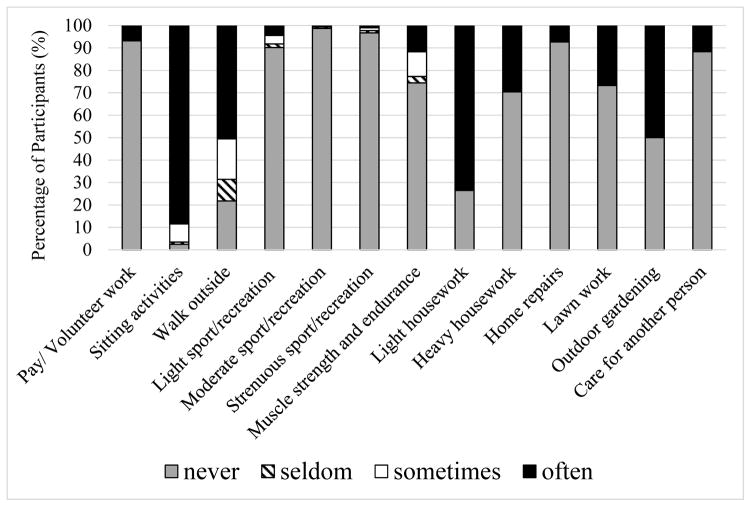
Most participants fell into the low physical activity-low physical function group (n=453). The physical activity-physical function groups were significantly different by age category. Individuals in the low physical activity-low physical function group were significantly older than those in the other groups. Complete characteristic information for participants at baseline by physical activity and physical function groups is outlined in Table 1. Participants were significantly different from one another across groups. Compared to all other groups, participants in the low physical activity-low physical function group were significantly more likely to have a lower score in the MMSE and to report more comorbidities (p<0.05). The low physical activity and function group was more likely to have fewer years of education compared to the high physical activity and function group (p<0.05). By the nature of the study design, participants differed by SPPB and PASE scores (p<0.01). The mean SPPB score was 5.6±3.6 with a range from 0–12. The mean PASE score was 77.2±61.4 with a range from 0 to 341.7. Participation in physical activities is displayed in Figure 1. The most prevalent physical activities were light housework (73.5%), walking outside of the home (50.5%), and outdoor gardening (50%).
Table 1.
Baseline Participant Characteristics by Physical Activity and Physical Function Level (N=1011)
| Baseline Characteristic | Low Physical Activity-Low Physical Function | Low Physical Activity-High Physical Function | High Physical Activity-Low Physical Function | High Physical Activity-High Physical Function | Total |
|---|---|---|---|---|---|
| Total (%) | 453 (44.8) | 54 (5.3) | 307 (30.4) | 197 (19.5) | 1 011 |
| Age, years, | 83.2 (4.72) | 81.2 (4.20) | 81.9 (4.55) | 80.9 (3.70) | 82.3 (4.57) ** |
| Mean (SD) | |||||
| < 80 years (%) | 115 (25.4) | 27 (50.0) | 111 (36.2) | 81 (41.1) | 334 (33.0)** |
| 80–84 years (%) | 178 (39.3) | 17 (31.5) | 123 (40.1) | 82 (41.6) | 400 (39.6)** |
| ≥85 years (%) | 160 (35.3) | 10 (18.5) | 73 (23.8) | 34 (17.3) | 277 (27.4)** |
| Female (%) | 329 (72.6) | 37 (68.5) | 180 (58.6) | 93 (47.2) | 639 (63.20)** |
| Married (%) | 140 (31.8) | 25 (50.0) | 140 (46.4) | 107 (54.6) | 412 (41.66)** |
| Years of education, mean (SD) | 4.7 (3.8) | 5.1 (3.7) | 5.1 (3.9) | 5.1 (3.9) | 4.94 (3.85) ** |
| Falls (%) | 203 (44.8) | 22 (40.7) | 94 (30.6) | 49 (24.9) | 368 (36.40)* |
| SPPB score, mean (SD) | 3.2 (2.7) | 9.8 (0.9) | 5.4 (2.2) | 10.3 (0.9) | 5.57 (3.60) ** |
| PASE score, mean (SD) | 27.7 (21.7) | 40.8 (17.3) | 114.7 (41.6) | 143.1 (54.2) | 77.17 (61.35) ** |
| Body Mass Index, kg/m2 | 27.6 (5.6) | 27.7 (4.8) | 27.6 (4.9) | 26.5 (4.0) | 27.36 (5.03) |
| Mean (SD) | |||||
| Depression (%) | 148 (32.7) | 7 (13.0) | 38 (12.4) | 7 (3.6) | 200 (19.78)** |
| Distance vision impairment (%) | 106 (23.4) | 7 (13.0) | 40 (13.0) | 17 (8.6) | 170 (16.82)* |
| Near vision impairment (%) | 27 (6) | 1 (1.9) | 5 (1.6) | 2 (1.0) | 35 (3.46)* |
| MMSE score, mean (SD) | 20.6 (6.5) | 22.9 (3.9) | 22.5 (5.4) | 24.8 (4.4) | 21.20 (7.03) |
| Frailty (%) | 128 (28.4) | 3(5.6) | 16 (5.2) | 1 (0.5) | 148 (14.7) *** |
| Number of Comorbidities, Mean (SD) | 2.5 (1.2) | 2.0 (1.2) | 2.0 (1.1) | 1.8 (1.2) | 2.1 (1.22) ** |
| Stroke (%) | 37 (8.2) | 1 (1.9) | 11 (3.6) | 9 (4.6) | 58 (5.74)* |
| Heart Attack (%) | 23 (5.1) | 1 (1.9) | 5 (1.6) | 3 (1.5) | 32 (3.17)* |
| Cancer (%) | 41 (9.1) | 3 (5.6) | 17 (5.5) | 15 (7.6) | 76 (7.53)* |
| Parkinson’s (%) | 20 (4.5) | 1 (1.9) | 4 (1.3) | 2 (1.0) | 27 (2.69)* |
| Hypertension (%) | 320 (72.0) | 29 (53.9) | 201 (63.9) | 128 (65.2) | 678 (67.31)** |
| Diabetes (%) | 195 (43.1) | 19 (35.2) | 91 (29.6) | 49 (24.9) | 354 (35.01)** |
| Fracture (%) | 14 (3.1) | 1 (1.9) | 1 (0.3) | 1 (0.5) | 17 (1.68)** |
| Emphysema (%) | 52 (11.6) | 5 (9.3) | 24 (7.8) | 12 (6.1) | 93 (9.25) |
| Arthritis (%) | 324 (71.8) | 32 (59.3) | 182 (59.9) | 97 (49.2) | 635 (63.12)** |
p<0.05,
p<0.01
p<0.0001
MMSE- Mini-Mental State Examination; PASE- Physical Activity Scale for the Elderly; SPPB- Short Physical Performance Battery
Figure 1.
Physical activities at baseline (N=1011).
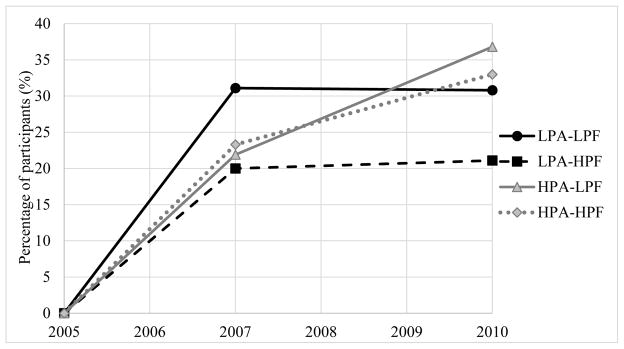
Figure 2 displays the rate of falls at each follow-up point by study group among the 643 participants who reported no falls at baseline. At the first follow- up (2007/2008) 31.1% of the low physical activity-low physical function, 20.0% of the low physical activity-high physical function, 21.9% of the high physical activity-low physical function, and 23.3% of the high physical activity-high physical function group reported a fall. At the second follow-up (2010/2011) 30.8% of the low physical activity-low physical function, 21.1% of the low physical activity-high physical function, 36.8% of the high physical activity-low physical function, and 33% of the high physical activity-high physical function group reported a fall.
Figure 2.
Rate of falls at each follow-up among participants with no falls at baseline (N=643). LPA-LPF: Low physical activity- Low physical function; LPA-HPF: Low physical activity- High physical function; HPA-LPF: High physical activity- Low physical function; HPA-HPF: High physical activity- High physical function.
Table 2 presents the odds ratio and 95 % Confidence Interval (CI) for developing a fall over time as a function of baseline physical activity – physical function groups. Model 1 included time, age, gender, marital status, education, falls at baseline (none, one or more), and group assignment. Low physical activity-low physical function was used as the reference group. At baseline, the association between physical activity – physical function groups and falls was statistically significant for the high physical activity – low physical function group [odds ratio (OR) = 0.34, 95% CI = 0.14 – 0.80] and for the high physical activity – high physical function group (OR = 0.35, 95 % CI = 0.14 – 0.91) compared to the reference group. The interaction term between physical activity – physical function groups and time of follow-up (falls over time) was statistically significant for the high physical activity – low physical function group (OR = 1.41, 95% CI = 1.08 – 1.89) and for the high physical activity – high physical function group (OR=1.41, 95 % CI = 1.05 – 1.89) compared to the low physical activity – low physical function reference group, suggesting that participants in these groups experienced more falls over time. No significant association at baseline or over time was found for the low physical activity – high physical function group and falls.
Table 2.
General Estimation Equations for Falls over 6-year of Follow-up as a Function of Baseline Physical Activity and Physical Function Group (N=1011)
| Variable | Model 1 | Model 2 |
|---|---|---|
|
| ||
| OR (95% Confidence Interval) | ||
| Main Effect | ||
| Low Physical Activity - Low Physical Function | Ref | Ref |
| Low Physical Activity - High Physical Function | 1.22 (0.24–6.92) | 1.19 (0.16–8.69) |
| High Physical Activity - Low Physical Function | 0.34 (0.14–0.80)* | 0.39 (0.14–0.99)* |
| High Physical Activity - High Physical Function | 0.35 (0.14–0.91)* | 0.60 (0.21–1.74) |
| Time | 1.06 (0.88–1.27) | 1.08 (0.87–1.35) |
| Time Interaction effect | ||
| Low Physical Activity - Low Physical Function | Ref | Ref |
| Low Physical Activity - High Physical Function | 0.79 (0.44–1.41) | 0.75 (0.37–1.52) |
| High Physical Activity - Low Physical Function | 1.41 (1.08–1.89) ** | 1.38 (1.01–1.90)* |
| High Physical Activity - High Physical Function | 1.41 (1.05–1.89)* | 1.20 (0.85–1.68) |
p<0.05,
p<0.01
Model 1 included time, age, gender, marital status, education, falls at baseline, and physical ability groups.
Model 2 included BMI, depressive symptoms, MMSE, and comorbidities along with variables in Model 1.
In the fully adjusted model (Table 2 - Model 2), the association between physical activity – physical function groups and falls at baseline remained statistically significant only for the high physical activity – low physical function group (OR = 0.39, 95% CI = 0.14 - 0.99) compared to the reference group. The interaction term between physical activity – physical function groups and time of follow-up (falls over time) remained statistically significant only for the high physical activity – low physical function group (OR=1.38, 95 % CI = 1.01 – 1.90) compared to the reference group, suggesting that participants in this group experienced more falls over time. Participants in the low physical activity – high physical function had greater decrease of falls over time compared to the reference group, however, this decrease was not statistically significant (OR=0.75, CI = 0.37 – 1.52).
Additional analyses were conducted to examine the association between physical activity – physical function groups and having 2 or more falls at baseline and over time. The associations were not statistically significant after adjusting for all covariates. Other significant variables associated with greater increase in the risk of falls over time included gender (p=0.04), history of previous fall (p<0.01), number of comorbidities (p=0.05), and high depressive symptoms (p=0.01).
DISCUSSION
The purpose of our study was to examine the association between physical activity and physical function on the risk of falls among older Mexican Americans aged 75 years and older who participated in a frailty study. We found that participants in the high physical activity and low physical function group had a greater increased risk of falls over time. Although it did not reach significance, participants in the high physical activity and high physical function group had an increased risk while participants in the low physical activity and high physical function group had a greater decrease in their risk of falls over time. Our results suggest, that in these older Mexican Americans maintaining high physical activity levels does not decrease an individual’s risk of falls over time.
These results support previous evidence that physical activity frequency results in an increased risk for falls (B. J. Jefferis et al., 2015; Lobo, 2012; Mertz et al., 2010; Peeters et al., 2010; Stahl & Albert, 2015; Wijlhuizen, Chorus, & Hopman-Rock, 2008). Physical activity incorporates a wide range of activities including lifestyle activities (walking, housework, gardening, etc.) (Washburn et al., 1993), aerobic exercise, muscle-strengthening, and balance activities (Nelson et al., 2007). Of these, muscle-strengthening and balance activities are most related to physical function (Guralnik et al., 1994). Physical activity interventions that have showed a reduction in falls are predominantly focused on increasing strength and balance (L. Clemson et al., 2012; Day et al., 2002; Hu et al., 2015; Kendrick et al., 2014; Lobo, 2012; Mangani et al., 2008). Only 11% of our participants took part in muscle-strengthening activities, and most participants had low physical function (n=760). Conversely, the majority of our participants were regularly physically active by completing light housework and walking. A study of 1,487 older adults, 50 years of age and older, found that individuals with the highest rates of walking and household activities were frequent fallers (Stahl & Albert, 2015). The high rates of walking and light housework may explain why 40% of our participants had a fall over the 6-year study period.
Based on our findings and information in the current literature, thoughtful considerations must be made in promoting physical activity to prevent falls. Physical activity should not be eliminated or decreased, because it provides several other health benefits for older adults (Nelson et al., 2007). Rather, how the physical activity is conducted must be modified for older adults at risk for falls. Data in the literature supports in-home exercises and environmental modifications, together with functional exercises to decrease risk of falls in this population (Campbell et al., 2005; L. Clemson et al., 2012).
Aerobic activity is essential for the health of older adults (Nelson et al., 2007). However, outdoor physical activity may increase a person’s risk for falls by increasing opportunities to have a fall (Wijlhuizen et al., 2008). Evidence from an energy expenditure study showed that walking in place for approximately 25 minutes is comparable to walking 1 mile at 3.0 mph (Steeves, Thompson, & Bassett, 2012). Stepping in place can potentially decrease the potential risks for falls while increasing an individual’s aerobic capacity and mobility. Physical function exercises can also be performed in the home. There is evidence that balance and strength exercises that are integrated into the daily lives of participants are effective in reducing falls (L. Clemson et al., 2012). The LiFE Study found a 31% reduction in the rate of falls at one year of follow up in the integrated exercise group compared to the control group who participated in a traditional in-home program (L. Clemson et al., 2012). The advantage of this type of exercise program is that it does not require additional exercise equipment or outdoor exercise, thus decreasing the external risk for falls (i.e. stairs, uneven sidewalks, improper equipment use).
The environment of physical activity should be modified, whether it is conducted indoors or outdoors. The addition of environmental modifications to a fall-risk prevention strategy can be effective (Lundebjerg et al., 2001). Tools such as the Westmead Home Safety Assessment (WeHSA) (L Clemson, Fitzgerald, & Heard, 1999a, 1999b), a very comprehensive tool that focuses on risks related to falls in traffic ways, indoors, living area, seating, bedroom, bathroom, kitchen and laundry, and on footwear, and medication management can be applied to older adults (L Clemson et al., 1999a, 1999b). A study that enrolled 391 visually impaired older adults for a year-long intervention found that WeHSA was successful in reducing falls. Participants were randomized to have a WeHSA program, in-home balance and strength training, WeHSA program and in-home balance and strength training, or social visits with no exercise or home safety programs. At the end of the study, there were 1.17 falls per person year in a group that received WeHSA modifications and exercise whereas the in-home exercise group alone experience 1.3 falls per person year (Campbell et al., 2005). Thus, providing a safe environment for physical activity may further decrease fall risk.
These recommendations are also suitable for frail older adults; however, more surveillance and motivational support is needed for a frail population (Geraedts, Zijlstra, Zhang, Bulstra, & Stevens, 2014). An in-home exercise program was developed by Geraedts and colleagues (2014) for frail older adults. The intervention incorporates in-home strength and balances exercises in addition to weekly phone calls and sensor monitoring for motivation and surveillance, respectively (Geraedts et al., 2014). A 6-month intervention is currently being conducted to test its effectiveness, but the authors believe that this program will increase physical activity and physical function in frail participants (Geraedts et al., 2014).
Strengths and Limitations
This study has some limitations. First, over the 6-year period, 10% of the study cohort was lost to follow-up and 28.4% died, which may have underestimated the incidence of falls. Second, our analysis does not account for the severity of the falls and, therefore, we cannot determine the ultimate effect on the health of our participants. Despite this limitation, falls are highly associated with adverse health events, such as injuries, fractures, and hospitalization (Lundebjerg et al., 2001; Mertz et al., 2010; Nowalk et al., 2001). Third, 33% of our participants had mild or moderate cognitive impairment which could have led to an underestimation of our findings. Fourth, our analysis does not account for the environment surrounding the physical activity, a factor that could add another risk for falls. However, the PASE scale is widely used and is a reliable instrument to measure physical activity in older adults (Washburn et al., 1999; Washburn et al., 1993). Fifth, the fully adjusted model was not adequately powered to detect significance in the low physical activity-high physical function group (N=54) or in the high physical activity-high physical function group (N=197). Lastly, the participants in this study were from a subsample of older Mexican-Americans that were enrolled in a study on frailty, and the results may not be generalizable to all older Mexican-Americans in the U.S.
The major strength of this study is that it evaluates the level of physical activity and the level of physical function on the risk of falls over time. Both measures, PASE and SPPB, are standard instruments to measure physical activity and physical function, respectively (Guralnik et al., 1994; Washburn et al., 1999; Washburn et al., 1993). To our knowledge, no study accounts for the levels of both physical activity and physical function on the rate of falls among older Mexican American adults. This gives insight on the types of physical activities that are most associated with falls within this population, information which is currently lacking in the literature (Lundebjerg et al., 2001).
Conclusion
The current guidelines encourage older adults to be physically active to prevent falls (Lundebjerg et al., 2001; Michael et al., 2010; Nelson et al., 2007). However, our findings suggest that high levels of physical activity with low levels of physical function are associated with an increased risk of falls among older Mexican American adults over time. Our participants predominately participated in lifestyle physical activities such as light housework, walking, and gardening, and rarely participated in muscle-strengthening and balance exercises that specifically improve physical function. Increasing the activities that improve physical function, instead of merely increasing the frequency of physical activity, should be the focus in order to prevent falls within this population. Based on the current literature, this population may benefit from in-home activities to decrease an individual’s risk of falls overtime.
Acknowledgments
The authors would like to thank Dr. Marinel Ammenheuser for her assistance in editing this manuscript.
Footnotes
Conflict of Interest: No financial disclosures were reported by the authors of this paper. This work was supported by the National Institutes of Health/National Institute of Aging (R01 AG10939, R01 AG17638, P30 AG024832, and R03 AG046409) and the National Institute for Child Health and Human Development (R24 HD065702). The funding institutions had no role in the study design; data collection, management, analysis, or interpretation; or preparation of the manuscript.
Author Contributions: ZH Lewis: Data analysis and interpretation and writing the manuscript. K Markides: Manuscript revisions and PI for original H-EPESE grant (R01-AG010939). KJ Ottenbacher: Manuscript revisions and funding (R01-AG017638). S Al Snih: Data analysis and interpretation, contributing to sections of the manuscript, and manuscript revisions.
References
- Al Snih S, Graham JE, Ray LA, Samper-Ternent R, Markides KS, Ottenbacher KJ. Frailty and incidence of activities of daily living disability among older Mexican Americans. J Rehabil Med. 2009;41(11):892–897. doi: 10.2340/16501977-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults- evaluation of short form of the CES-D. Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, Hale LA. Randomised controlled trial of prevention of falls in people aged > or =75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817. doi: 10.1136/bmj.38601.447731.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Older Adult Falls. Older Adult Falls: Get the Facts. 2014 Retrieved from http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html.
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Shekelle PG. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328(7441):680. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O’Loughlin P, Black D. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ. 2012;345:e4547. doi: 10.1136/bmj.e4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemson L, Fitzgerald M, Heard R. Content validity of an assessment tool to identify home fall hazards: The Westmead Home Safety Assessment. British Journal of Occupational Therapy. 1999a;62(4):171–179. [Google Scholar]
- Clemson L, Fitzgerald M, Heard R. Inter-rater reliability of a home fall hazards assessment tool. The Occupational Therapy Journal of Research. 1999b;19(2):83–100. [Google Scholar]
- Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325(7356):128. doi: 10.1136/bmj.325.7356.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state- practical method for grading cognitive state of patients for clinican. J Psychiat Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Freiberger E, de Vreede P, Schoene D, Rydwik E, Mueller V, Frändin K, Hopman-Rock M. Performance-based physical function in older community-dwelling persons: a systematic review of instruments. Age Ageing. 2012;41(6):712–721. doi: 10.1093/ageing/afs099. [DOI] [PubMed] [Google Scholar]
- Fried LJ. Principles of Geriatric Medicine and Gerontology. New York, NY: McGraw-Hill Professional; 1999. Frailty and failure to thrive; pp. 1387–1402. [Google Scholar]
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50(8):1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- Geraedts HA, Zijlstra W, Zhang W, Bulstra S, Stevens M. Adherence to and effectiveness of an individually tailored home-based exercise program for frail older adults, driven by mobility monitoring: design of a prospective cohort study. BMC Public Health. 2014;14:570. doi: 10.1186/1471-2458-14-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Hu J, Xia Q, Jiang Y, Zhou P, Li Y. Risk factors of indoor fall injuries in community-dwelling older women: A prospective cohort study. Arch Gerontol Geriatr. 2015;60(2):259–264. doi: 10.1016/j.archger.2014.12.006. [DOI] [PubMed] [Google Scholar]
- Jefferis B, Merom D, Sartini C, Wannamethee SG, Ash S, Lennon LT, Whincup PH. Physical Activity and Falls in Older Men: The Critical Role of Mobility Limitations. Med Sci Sports Exerc. 2015 doi: 10.1249/MSS.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferis BJ, Iliffe S, Kendrick D, Kerse N, Trost S, Lennon LT, Whincup PH. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014;14:114. doi: 10.1186/1471-2318-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferis BJ, Merom D, Sartini C, Wannamethee SG, Ash S, Lennon LT, Whincup PH. Physical Activity and Falls in Older Men: The Critical Role of Mobility Limitations. Med Sci Sports Exerc. 2015 doi: 10.1249/MSS.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick D, Kumar A, Carpenter H, Zijlstra GA, Skelton DA, Cook JR, Delbaere K. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;11:CD009848. doi: 10.1002/14651858.CD009848.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveille SG, Guralnik JM, Ferrucci L, Corti MC, Kasper J, Fried LP. Black/white differences in the relationship between MMSE scores and disability: the Women’s Health and Aging Study. J Gerontol B Psychol Sci Soc Sci. 1998;53(3):P201–208. doi: 10.1093/geronb/53b.3.p201. [DOI] [PubMed] [Google Scholar]
- Lobo A. Relationship between physical condition, functional fitness, and falls risk in elderly adults. J Am Geriatr Soc. 2012;60(9):1788–1789. doi: 10.1111/j.1532-5415.2012.04137.x. [DOI] [PubMed] [Google Scholar]
- Lundebjerg N, Rubenstein LZ, Kenny RA, Koval KJ, Martin FC, Tinetti ME Amer Acad Orthopaedic Surg P. Guideline for the prevention of falls in older persons. Journal of the American Geriatrics Society. 2001;49(5):664–672. [PubMed] [Google Scholar]
- Mangani I, Cesari M, Russo A, Onder G, Maraldi C, Zamboni V, Landi F. Physical function, physical activity and recent falls. Results from the “Invecchiamento e Longevità nel Sirente (ilSIRENTE)” Study. Aging Clin Exp Res. 2008;20(3):234–241. doi: 10.1007/bf03324778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Ray LA, Angel R, Espino DV. Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE) Wave 5, 2004–2005. Arizona, California, Colorado, New Mexico, and Texas: Inter-university Consortium for Political and Social Research (ICPSR); 2009. (ICPSR25041-v1 ed.) [Google Scholar]
- Mertz KJ, Lee DC, Sui X, Powell KE, Blair SN. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related falls. Am J Prev Med. 2010;39(1):15–24. doi: 10.1016/j.amepre.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y, Lin J, Whitlock E, Gold R, Fu R, O’Connor E, Lutz K. Evidence Synthesis No. 80. Rockville, MD: Agency for Healthcare Research and Quality; 2010. Interventions to Prevent Falls in Older Adults: An Updated Systematic Review. AHRQ Publication No. 11-05150-EF-1. [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- Nowalk MP, Prendergast JM, Bayles CM, D’Amico FJ, Colvin GC. A randomized trial of exercise programs among older individuals living in two long-term care facilities: the FallsFREE program. J Am Geriatr Soc. 2001;49(7):859–865. doi: 10.1046/j.1532-5415.2001.49174.x. [DOI] [PubMed] [Google Scholar]
- Ottenbacher AJ, Snih SA, Karmarkar A, Lee J, Samper-Ternent R, Kumar A, Ottenbacher KJ. Routine Physical Activity and Mortality in Mexican Americans Aged 75 and Older. J Am Geriatr Soc. 2012;60(6):1085–1091. doi: 10.1111/j.1532-5415.2012.03995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher KJ, Graham JE, Al Snih S, Raji M, Samper-Ternent R, Ostir GV, Markides KS. Mexican Americans and Frailty: Findings From the Hispanic Established Populations Epidemiologic Studies of the Elderly. Am J Public Health. 2009;99(4):673–679. doi: 10.2105/ajph.2008.143958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters GM, Verweij LM, van Schoor NM, Pijnappels M, Pluijm SM, Visser M, Lips P. Which types of activities are associated with risk of recurrent falling in older persons? J Gerontol A Biol Sci Med Sci. 2010;65(7):743–750. doi: 10.1093/gerona/glq013. [DOI] [PubMed] [Google Scholar]
- Stahl ST, Albert SM. Gender differences in physical activity patterns among older adults who fall. Prev Med. 2015;71:94–100. doi: 10.1016/j.ypmed.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steeves JA, Thompson DL, Bassett DR. Energy cost of stepping in place while watching television commercials. Med Sci Sports Exerc. 2012;44(2):330–335. doi: 10.1249/MSS.0b013e31822d797e. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Thomas KE, Sogolow ED. Seasonal patterns of fatal and nonfatal falls among older adults in the U.S. Accid Anal Prev. 2007;39(6):1239–1244. doi: 10.1016/j.aap.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Tuunainen E, Rasku J, Jäntti P, Pyykkö I. Risk factors of falls in community dwelling active elderly. Auris Nasus Larynx. 2014;41(1):10–16. doi: 10.1016/j.anl.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Vu MQ, Weintraub N, Rubenstein LZ. Falls in the nursing home: Are they preventable? J Am Med Dir Assoc. 2005;6(3 Suppl):S82–87. doi: 10.1016/j.jamda.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Ward RE, Leveille SG, Beauchamp MK, Travison T, Alexander N, Jette AM, Bean JF. Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc. 2015;63(2):315–320. doi: 10.1111/jgs.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- Wijlhuizen GJ, Chorus AM, Hopman-Rock M. Fragility, fear of falling, physical activity and falls among older persons: some theoretical considerations to interpret mediation. Prev Med. 2008;46(6):612–614. doi: 10.1016/j.ypmed.2008.01.016. [DOI] [PubMed] [Google Scholar]