Abstract
AIM: To determine the outcome of the management of iatrogenic gastrointestinal tract perforations treated by over-the-scope clip (OTSC) placement.
METHODS: We retrospectively enrolled 20 patients (13 female and 7 male; mean age: 70.6 ± 9.8 years) in eight high-volume tertiary referral centers with upper or lower iatrogenic gastrointestinal tract perforation treated by OTSC placement. Gastrointestinal tract perforation could be with oval-shape or with round-shape. Oval-shape perforations were closed by OTSC only by suction and the round-shape by the “twin-grasper” plus suction.
RESULTS: Main perforation diameter was 10.1 ± 4.3 mm (range 3-18 mm). The technical success rate was 100% (20/20 patients) and the clinical success rate was 90% (18/20 patients). Two patients (10%) who did not have complete sealing of the defect underwent surgery. Based upon our observations we propose two types of perforation: Round-shape “type-1 perforation” and oval-shape “type-2 perforation”. Eight (40%) out of the 20 patients had a type-1 perforation and 12 patients a type-2 (60%).
CONCLUSION: OTSC placement should be attempted after perforation occurring during diagnostic or therapeutic endoscopy. A failed closure attempt does not impair subsequent surgical treatment.
Keywords: Over-the-scope clip, OVESCO, Perforation, Gastrointestinal tract
Core tip: The aim of this study was to determine the outcome of over-the-scope clip management of patients with iatrogenic gastrointestinal tract perforations in eight high-volume tertiary referral centers. Technical success was of 100% and clinical success of 90%. Moreover, after evaluating our results we did a classification of the iatrogenic perforation: We defined the perforation with round-shape “type-1 perforation” and the oval-shape one as “type-2 perforation”.
INTRODUCTION
Iatrogenic perforations that occur during endoscopic procedures are generally managed surgically[1,2]. Some authors prefer a non-surgical approach in selected cases, despite the considerable risk of morbidity and mortality[3,4]. Most cases of iatrogenic perforation occur during therapeutic endoscopic procedures, including bilio-pancreatic procedures, particularly in the context of endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) for the treatment of superficial neoplasia, but there are also descriptions of cases occurring during diagnostic upper or lower gastrointestinal (GI) endoscopy[5-7]. The reported incidence of perforation during diagnostic endoscopy is between 0.01% and 0.6% while that during therapeutic endoscopy is between 0.6% and 5.5%. Using an over-the-scope clip (OTSC) it would be possible to close these perforations immediately during the endoscopy.
Through-the-scope (TTS) clip closure of endoscopic perforations has been described in the literature since 1997[8,9]. However, there are limitations to closing full-thickness defects with TTS clips. The closure is confined to the mucosal and submucosal layers, with relatively low closure force, and the opening span between the jaws is restricted. A new device, the OTSC system (Ovesco Endoscopy AG, Tübingen, Germany) is designed to create full-thickness closure by using teeth arranged in the shape of a bear trap and has a simple method of application. The OTSC is made of a super-elastic, shape-memory alloy (nitinol), which takes its former, unbent shape after the clip is released, and thus exerts constant compression on the tissue between the jaws of the clip. von Renteln et al[10] showed, in a porcine model, that the OTSC clips provide a full-thickness closure of perforations.
Although the use of an OTSC has been well established during natural orifice transluminal endoscopic surgery[11] and treatment of bleeding[12-14] in recent years some reports have been published describing the usefulness of OTSC in closing acute iatrogenic perforations, first in animal models and then in humans[15-17].
The aim of our study was to determine the outcome of the management of iatrogenic gastrointestinal tract perforations treated by OTSC.
MATERIALS AND METHODS
Data were retrospectively collected from eight high-volume tertiary referral endoscopy units. Data from all patients undergoing immediate or 24 h - delayed OTSC placement for acute iatrogenic perforation, during diagnostic or therapeutic endoscopy or other therapeutic maneuvers, in the period between December 2012 and January 2015 were reviewed and reported as mean ± SD. All endoscopic procedures were carried out in patients who were conscious or deeply sedated with anesthesiologist support. The length of follow-up was of 3-mo.
Two different techniques were used for placing the OTSC at the site of the perforation: Only aspirating the defect inside the cap in which OTSC is mounted, or using the “twin-grasper” (Figure 1). The twin-grasper is generally used when the defect assumed a round-shape and only aspiration was used when oval-shape.
Figure 1.

Over-the-scope clip pre-loaded on the scope with the “twin-grasper” (from ovesco.com).
The twin-grasper, deployed through the working channel of the scope, was used to approximate the two edges of tissue, withdrawing them inside the cap, before releasing the OTSC. The twin-grasper has two independently movable lateral arms, allowing the two edges of the perforation to be grasped at two different times. The twin-grasper ensures that all layers of the gastrointestinal wall are contained in the bite, creating a full-thickness closure of the perforation. The technical success or failure of the OTSC placement was documented by contrast X-ray.
Two different OTSC clip were used in the study: With traumatic and with atraumatic teeth. Traumatic OTSC differ from the atraumatic because of the presence of a spike over the tooth, allowing a best grasping of the tissue.
RESULTS
Of the 20 patients recruited, thirteen were female and seven male. Their mean age was 70.6 ± 9.8 years. The sites of perforation were esophagus (n = 1), stomach (n = 3), duodenum (n = 4), jejunum (n = 2), cecum (n = 1), ascending colon (n = 1), sigmoid colon (n = 7) and rectum (n = 1). Twelve of the perforations occurred during diagnostic endoscopy [3 during endoscopic ultrasound; 7 during colonoscopy in patients with diverticular disease and 2 in a Billroth II patient with a duodenoscope during identification of the papilla of Vater during endoscopic retrograde cholangiopancreatography (ERCP)] and eight during therapeutic endoscopy (4 during endoscopic EMR, 2 during ESD, one during therapeutic ERCP and one during tracheostomy). The diameters of the OTSC used were 9 mm (n = 2), 10 mm (n = 5) and 11 mm (n = 13). Mean perforation diameter was 10.1 ± 4.3 mm (range 3-18 mm). Seventeen of the 20 perforations were treated by application of OTSC immediately, and 3 the day after. Most of the used OTSC clips had traumatic teeth (19 traumatic and 1 atraumatic). Results are summarized in Table 1.
Table 1.
Site, type of procedure being during occurred gastrointestinal perforation and type of applied over-the-scope clip
| Number of patients | 20 (13 F and 7 M) |
| Site | Esophagus (n = 1) |
| Stomach (n = 3) | |
| Duodenum (n = 4) | |
| Jejunum (n = 2) | |
| Cecum (n = 1) | |
| Ascending colon (n = 1) | |
| Sigmoid colon (n = 7) | |
| Rectum (n = 1) | |
| Procedure | Diagnostic colonoscopy (n = 7) |
| EUS (n = 3) | |
| EMR (n = 4) | |
| ERCP (n = 3) | |
| ESD (n = 2) | |
| Tracheostomy (n = 1) | |
| OTSC-type | 9/t mm (n = 2) |
| 10/t mm (n = 5) | |
| 11/a mm (n = 1) | |
| 11/t mm (n = 12) |
OTSC: Over-the-scope clip; F: Female; M: Male; EUS: Endoscopic ultrasound; EMR: Endoscopic mucosal resection; ERCP: Endoscopic retrograde cholangio-pancreatography; ESD: Endoscopic submucosal dissection; a: Atraumatic teeth; t: Traumatic teeth.
In all of the 20 patients the OTSC was placed successfully (100% technical success) with the correct deployment of the OTSC clip in the site of the defect. The clinical success rate was 90% (18 of the 20 patients) (Figure 2). In two of the patients (10%) the defect was not completely sealed. The first case of unsuccessful closure was a duodenal perforation, as shown by an X-ray transit study of the upper gastrointestinal tract performed immediately after placement of the OTSC, and the patient underwent duodenocefalo-pancreatectomy on the same day because of pancreatic head neoplasia. In both failures the OTSC was applied immediately after the recognition of the perforation. The second case was a sigmoid perforation during colonoscopy; the patient underwent sigmoid laparoscopic resection the day after because developing of peritonitis and the surgical specimen showed an incompletely sealed defect. No technical difficulties were encountered by the different endoscopists in placing the clips in different sites of the gut. No adverse events or deaths were recorded after OTSC placement during 3-mo follow-up and OTSC clips were not retrieved. Eight (40%) out of the 20 patients had a round-shape perforation and 12 patients an oval-shape one (60%). In all of 8 patients with round-shape perforation the defect was closed by twin-grasper plus suction and in all of the 12 patients with oval-shape perforation the defect was closed only by suction.
Figure 2.
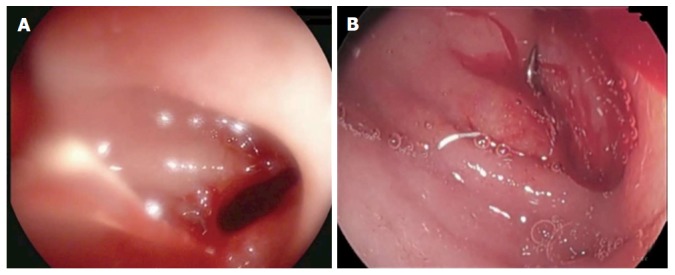
Duodenal type-2 perforations after endoscopic ultrasound (A) sealed by an over-the-scope clip (B).
DISCUSSION
Iatrogenic perforation has always been considered a potential pitfall of diagnostic and therapeutic endoscopic maneuvers and a challenge to treat, especially before the advent of OTSC. In our series the technical success rate was 100% (20/20 patients) and the clinical success rate was 90% (18/20 patients). In two cases (10%) we did not have complete sealing of the perforation and the patients underwent surgery. Similar data were reported by Voermans et al[18] in the Clipper study, with a clinical success of 89%. Importantly, in this prospective multicenter study the mean endoscopic closure time was 5 min and 44 s ± 4 min and 15 s.
The efficacy of OTSC is based on the capacity of the clip to provide full-thickness closure of the perforation, a property well proven in some studies in animal models. At post-mortem examination executed after the OTSC placement, laparotomies revealed the full-tickness closure of the defect and peritoneum or small bowel included in the closure in some cases[19-21].
On the analysis of our data we observed that most of the round-shape defects were closed with the aid of the “twin-grasper” and the oval-shape defect were closed by scope aspiration. On the basis of these results we can propose classification of perforations into two types: Round-shape “type-1 perforation” and oval-shape “type-2 perforation” (Figure 3). The “twin-grasper” plays an essential role in presence of large perforations for its capability to approximate the two edges of the defect allowing a more secure grasp of the defect by the OTSC clip.
Figure 3.
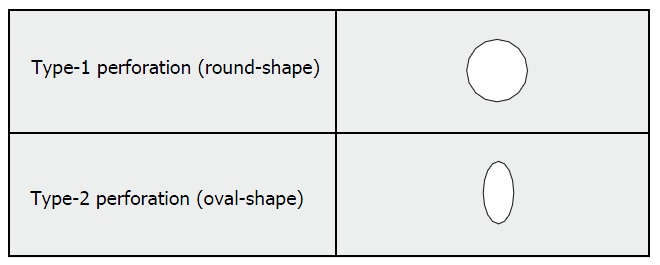
Mangiavillano’s classification of gastrointestinal tract perforations.
The use of suction has to be done in moderation, since excessive suction may grasp a good amount of the bowel wall and result in lumenal restrictions. Excessive suction applied in the perforation area can also theoretically lead to catch of anatomical structures from outside of the bowel wall and involve them into the clipping site. The reason is the relatively low control of the tissue invagination process into the cap and the frequent limitation in visualization during suction. The suction should be used with caution in the colon, which has a relatively thin wall.
The role of OTSC in the management of endoscopic iatrogenic perforation has been discussed also in some case reports and small series. A case of spontaneous iatrogenic perforations sealed by OTSC clip have been described[22]. Changela et al[23] recently described three cases of endoscopic perforation successfully treated by OTSC.
In 2010 Parodi et al[24] demonstrated the usefulness of the OTSC in a small series of patients with GI perforations up to 20 mm. One of the 10 treated cases was solved completely by placing two additional covered stent. More than one OTSC clip can be placed in presence of an iatrogenic perforation. A Japanese group published recently the possibility to apply as many as three OTSC clips in a series of 23 treated patients for bleeding, fistula and perforation of which 4 mucosal defect were observed during ESD[25]. Moreover, a recent systematic review performed by Weiland et al[26] based on a small case series because of the lack of randomized and clinical trials in this field, showed OTSC clip placemen to be a safe and effective method in the closure of GI tract defects, as perforations and acute anastomotic leak.
Gubler et al[27] in a series of 14 patients treated by OTSC clip placement for acute iatrogenic perforations of the GI tract demonstrated closure of the GI defects is possible in the presence of a perforation up to 30 mm diameter.
The largest study currently available in the literature about the use of OTSC in acute perforation by Haito-Chavez et al[28] including 188 patients with 48 perforations, with a median defect diameter of 7 mm. The rate of successful technical closure of the perforations was 97.5%, with an immediate clinical success of 94.9% and an overall long-term follow-up (207 d) rate of 90%; this rate was higher than that for closure of leaks (73.3%) and significantly higher than that for closure of fistulae (42.9%).
It is now established that the use of OTSC clips may reduce the rate of emergency surgery[29] when an accidental perforation occurs and maybe considered as a mini-invasive endoscopic alternative to surgical repair. Recently, the position statement of the European Society of Gastrointestinal Endoscopy, has introduced the use of OTSC clips in GI tract acute iatrogenic perforations[30]. However, despite the good results reported in the different published studies, OTSC clips are inappropriate in presence of delayed diagnosis by days or weeks, in individuals in whom there is significant peritoneal contamination, in long serosal tears of the colon, and perforations with endoscopic sphincterotomy where placement may result in sealing off the pancreatico-biliary orifices.
In our opinion, considering the high rates of technical and clinical success in sealing perforations of the gastrointestinal tract, OTSC placement should be performed to manage perforations occurring during diagnostic or therapeutic endoscopy or other therapeutic maneuvers, even in small endoscopic centers provided that the endoscopists’ training is adequate. It allows a short stay in hospital and results in less hospital costs. Moreover, a failed attempt at OTSC deployment does not preclude subsequent surgical treatment. We suggest using the “twin-grasper” plus aspiration when a perforation type-1 occurs and only aspiration, if the endoscopist is confident with the OTSC system, in perforation type-2.
COMMENTS
Background
Gastrointestinal iatrogenic perforations are generally surgically managed. The reported incidence of perforation during diagnostic endoscopy is 0.01%-0.6%, while during therapeutic endoscopy is 0.6%-5.5%. Using an over-the-scope clip (OTSC) it is possible to close these perforations immediately.
Research frontiers
Through-the-scope (TTS) clip closure of endoscopic perforations has been described in the literature since 1997. However, there are limitations to closing full-thickness defects with TTS clips. The closure is confined to the mucosal and submucosal layers, with relatively low closure force, and the opening span between the jaws is restricted.
Innovations and breakthroughs
Iatrogenic perforation has always been considered a potential pitfall of diagnostic and therapeutic endoscopic maneuvers and a challenge to treat, especially before the advent of OTSC. In the authors’ series the technical success rate was 100% (20/20 patients) and the clinical success rate was 90% (18/20 patients). Moreover, on the basis of the shape of the defect, the authors propose a classification of gastrointestinal (GI) tract perforations.
Applications
OTSC clip placement should be performed to manage perforations occurring during diagnostic or therapeutic endoscopy or other therapeutic maneuvers, even in small endoscopic centers provided that the endoscopists’ training is adequate. It allows a short stay in hospital and results in less hospital costs. Moreover, a failed attempt at OTSC deployment does not preclude subsequent surgical treatment.
Terminology
Iatrogenic perforations are defect of the entire GI wall (from mucosa to serosa) caused by diagnostic or therapeutic maneuvers.
Peer-review
The authors have performed an interesting study of 20 cases with iatrogenic gastrointestinal perforations treated by endoscopic over-the-scope-clipping with high success rate.
Footnotes
Institutional review board statement: This is a retrospective study, a case-collection. Data of the patients treated were analyzed from the clinical data of our hospitals and OTSC clip were used not for the aim of the study. The aim of the study was only to review retrospective data from the clinical records of the patients. Then, we have no need of IRB statement.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: No conflicts of interest to declare.
Data sharing statement: Technical appendix, statistical code, and dataset available from the corresponding author at b_mangiavillano@hotmail.com. Participants informed consent for data sharing was not obtained but the presented data are anonymized and risk of identification is low.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: October 22, 2015
First decision: December 11, 2015
Article in press: January 31, 2016
P- Reviewer: Jodlowski T, Kamberoglou D, Kozarek RA, Kate V, Lorenzo-Zuniga V, Meshikhes AWN S- Editor: Qi Y L- Editor: A E- Editor: Li D
References
- 1.Chaudhary A, Aranya RC. Surgery in perforation after endoscopic sphincterotomy: sooner, later or not at all? Ann R Coll Surg Engl. 1996;78:206–208. [PMC free article] [PubMed] [Google Scholar]
- 2.Bell RC, Van Stiegmann G, Goff J, Reveille M, Norton L, Pearlman NW. Decision for surgical management of perforation following endoscopic sphincterotomy. Am Surg. 1991;57:237–240. [PubMed] [Google Scholar]
- 3.Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191–198. doi: 10.1097/00000658-200008000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung RS, Sivak MV, Ferguson DR. Surgical decisions in the management of duodenal perforation complicating endoscopic sphincterotomy. Am J Surg. 1993;165:700–703. doi: 10.1016/s0002-9610(05)80791-3. [DOI] [PubMed] [Google Scholar]
- 5.Minami S, Gotoda T, Ono H, Oda I, Hamanaka H. Complete endoscopic closure of gastric perforation induced by endoscopic resection of early gastric cancer using endoclips can prevent surgery (with video) Gastrointest Endosc. 2006;63:596–601. doi: 10.1016/j.gie.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 6.Abe S, Oda I, Suzuki H, Nonaka S, Yoshinaga S, Odagaki T, Taniguchi H, Kushima R, Saito Y. Short- and long-term outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Endoscopy. 2013;45:703–707. doi: 10.1055/s-0033-1344396. [DOI] [PubMed] [Google Scholar]
- 7.Kojima T, Parra-Blanco A, Takahashi H, Fujita R. Outcome of endoscopic mucosal resection for early gastric cancer: review of the Japanese literature. Gastrointest Endosc. 1998;48:550–554; discussion 554-555. doi: 10.1016/s0016-5107(98)70108-7. [DOI] [PubMed] [Google Scholar]
- 8.Mangiavillano B, Viaggi P, Masci E. Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 2010;11:12–18. doi: 10.1111/j.1751-2980.2009.00414.x. [DOI] [PubMed] [Google Scholar]
- 9.Yoshikane H, Hidano H, Sakakibara A, Ayakawa T, Mori S, Kawashima H, Goto H, Niwa Y. Endoscopic repair by clipping of iatrogenic colonic perforation. Gastrointest Endosc. 1997;46:464–466. doi: 10.1016/s0016-5107(97)70045-2. [DOI] [PubMed] [Google Scholar]
- 10.von Renteln D, Schmidt A, Vassiliou MC, Rudolph HU, Gieselmann M, Caca K. Endoscopic closure of large colonic perforations using an over-the-scope clip: a randomized controlled porcine study. Endoscopy. 2009;41:481–486. doi: 10.1055/s-0029-1214759. [DOI] [PubMed] [Google Scholar]
- 11.Kratt T, Küper M, Traub F, Ho CN, Schurr MO, Königsrainer A, Granderath FA, Kirschniak A. Feasibility study for secure closure of natural orifice transluminal endoscopic surgery gastrotomies by using over-the-scope clips. Gastrointest Endosc. 2008;68:993–996. doi: 10.1016/j.gie.2008.06.057. [DOI] [PubMed] [Google Scholar]
- 12.Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 13.Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162–3164. doi: 10.1007/s00464-013-2871-1. [DOI] [PubMed] [Google Scholar]
- 14.Mangiavillano B, Arena M, Morandi E, Viaggi P, Masci E. Successful treatment with an over-the-scope clip of Dieulafoy’s gastric lesion resistant to conventional endoscopic treatment. Endoscopy. 2012;44 Suppl 2 UCTN:E387. doi: 10.1055/s-0032-1310141. [DOI] [PubMed] [Google Scholar]
- 15.Mangiavillano B, Morandi E, Arena M, Santoro T, Masci E. An ‘omental patch’ created during over-the-scope clipping completely sealed a duodenal perforation after endoultrasonography. Therap Adv Gastroenterol. 2014;7:280–281. doi: 10.1177/1756283X14540223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mangiavillano B, Arena M, Morandi E, Santoro T, Masci E. Successful closure of an endoscopic ultrasound-induced duodenal perforation using an over-the-scope-clip. Endoscopy. 2014;46 Suppl 1 UCTN:E206–E207. doi: 10.1055/s-0034-1365389. [DOI] [PubMed] [Google Scholar]
- 17.Mangiavillano B, Arena M, Masci E. Treatment of a sigmoid perforation with an over-the-scope clip during diagnostic colonoscopy. Clin Gastroenterol Hepatol. 2014;12:xxi–xxii. doi: 10.1016/j.cgh.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Voermans RP, Le Moine O, von Renteln D, Ponchon T, Giovannini M, Bruno M, Weusten B, Seewald S, Costamagna G, Deprez P, et al. Efficacy of endoscopic closure of acute perforations of the gastrointestinal tract. Clin Gastroenterol Hepatol. 2012;10:603–608. doi: 10.1016/j.cgh.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Matthes K, Jung Y, Kato M, Gromski MA, Chuttani R. Efficacy of full-thickness GI perforation closure with a novel over-the-scope clip application device: an animal study. Gastrointest Endosc. 2011;74:1369–1375. doi: 10.1016/j.gie.2011.07.057. [DOI] [PubMed] [Google Scholar]
- 20.Schurr MO, Hartmann C, Ho CN, Fleisch C, Kirschniak A. An over-the-scope clip (OTSC) system for closure of iatrogenic colon perforations: results of an experimental survival study in pigs. Endoscopy. 2008;40:584–588. doi: 10.1055/s-2008-1077354. [DOI] [PubMed] [Google Scholar]
- 21.von Renteln D, Rudolph HU, Schmidt A, Vassiliou MC, Caca K. Endoscopic closure of duodenal perforations by using an over-the-scope clip: a randomized, controlled porcine study. Gastrointest Endosc. 2010;71:131–138. doi: 10.1016/j.gie.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Bona D, Aiolfi A, Rausa E, Bonavina L. Management of Boerhaave’s syndrome with an over-the-scope clip. Eur J Cardiothorac Surg. 2014;45:752–754. doi: 10.1093/ejcts/ezt363. [DOI] [PubMed] [Google Scholar]
- 23.Changela K, Virk MA, Patel N, Duddempudi S, Krishnaiah M, Anand S. Role of over the scope clips in the management of iatrogenic gastrointestinal perforations. World J Gastroenterol. 2014;20:11460–11462. doi: 10.3748/wjg.v20.i32.11460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos) Gastrointest Endosc. 2010;72:881–886. doi: 10.1016/j.gie.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752–2760. doi: 10.3748/wjg.v19.i18.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27:2258–2274. doi: 10.1007/s00464-012-2754-x. [DOI] [PubMed] [Google Scholar]
- 27.Gubler C, Bauerfeind P. Endoscopic closure of iatrogenic gastrointestinal tract perforations with the over-the-scope clip. Digestion. 2012;85:302–307. doi: 10.1159/000336509. [DOI] [PubMed] [Google Scholar]
- 28.Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video) Gastrointest Endosc. 2014;80:610–622. doi: 10.1016/j.gie.2014.03.049. [DOI] [PubMed] [Google Scholar]
- 29.Hagel AF, Naegel A, Lindner AS, Kessler H, Matzel K, Dauth W, Neurath MF, Raithel M. Over-the-scope clip application yields a high rate of closure in gastrointestinal perforations and may reduce emergency surgery. J Gastrointest Surg. 2012;16:2132–2138. doi: 10.1007/s11605-012-1983-6. [DOI] [PubMed] [Google Scholar]
- 30.Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693–711. doi: 10.1055/s-0034-1377531. [DOI] [PubMed] [Google Scholar]


