Abstract
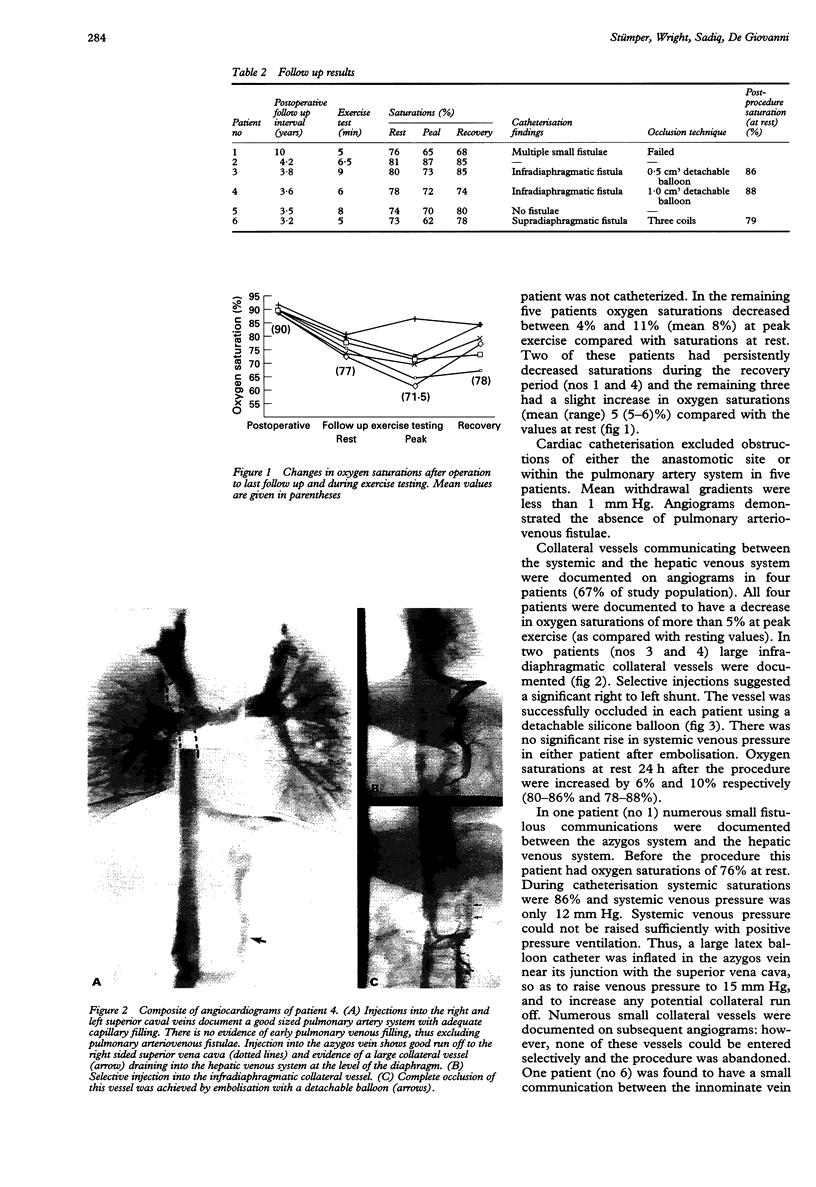
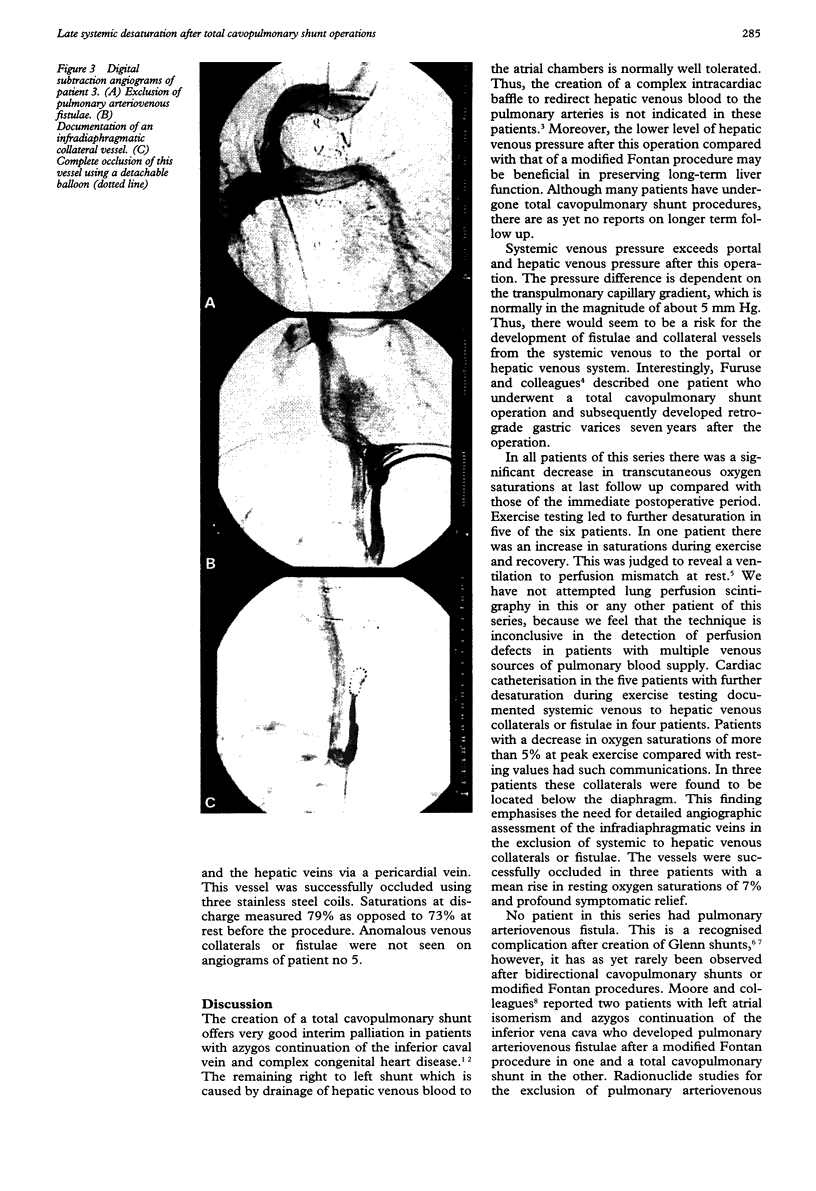
OBJECTIVES--To assess the medium-term results of total cavopulmonary shunt operations in children with left atrial isomerism, interrupted inferior vena cava, and complex congenital heart defects. BACKGROUND--Creation of a total cavopulmonary shunt provides very good interim palliation for children with interrupted inferior vena cava and complex congenital heart disease; however, longer term results after this operation have not been reported. METHODS--Detailed follow up of six children who underwent creation of a total cavopulmonary shunt at a tertiary referral centre. RESULTS--There were no early or late deaths. Oxygen saturations at discharge ranged from 89% to 92% (mean 90%). At last follow up (mean 4.7 years) saturations at rest ranged from 73% to 81% (mean 77%) (P < 0.05). All patients underwent exercise stress testing. At peak exercise oxygen saturations ranged from 62% to 87% (mean 71.5%) and during recovery from 68% to 85% (mean 78%). Cardiac catheterisation was performed in five patients with saturations of less than 80% at rest or peak exercise. No patient had pulmonary arteriovenous fistula. Systemic venous to hepatic venous collaterals were documented in four patients. These were localised below the diaphragm in three and above the diaphragm in one patient. The collateral vessel was successfully embolised in three of these patients, with a rise in resting oxygen saturations from 6 to 10% (mean 7%). CONCLUSIONS--The development of systemic venous to hepatic venous collaterals is a common complication in patients who undergo a total cavopulmonary shunt operation. This can lead to significant desaturation at rest and during exercise. Detailed angiographic studies of the infradiaphragmatic system veins is required for diagnosis. Transcatheter embolisation of such vessels gives good relief.
Full text
PDF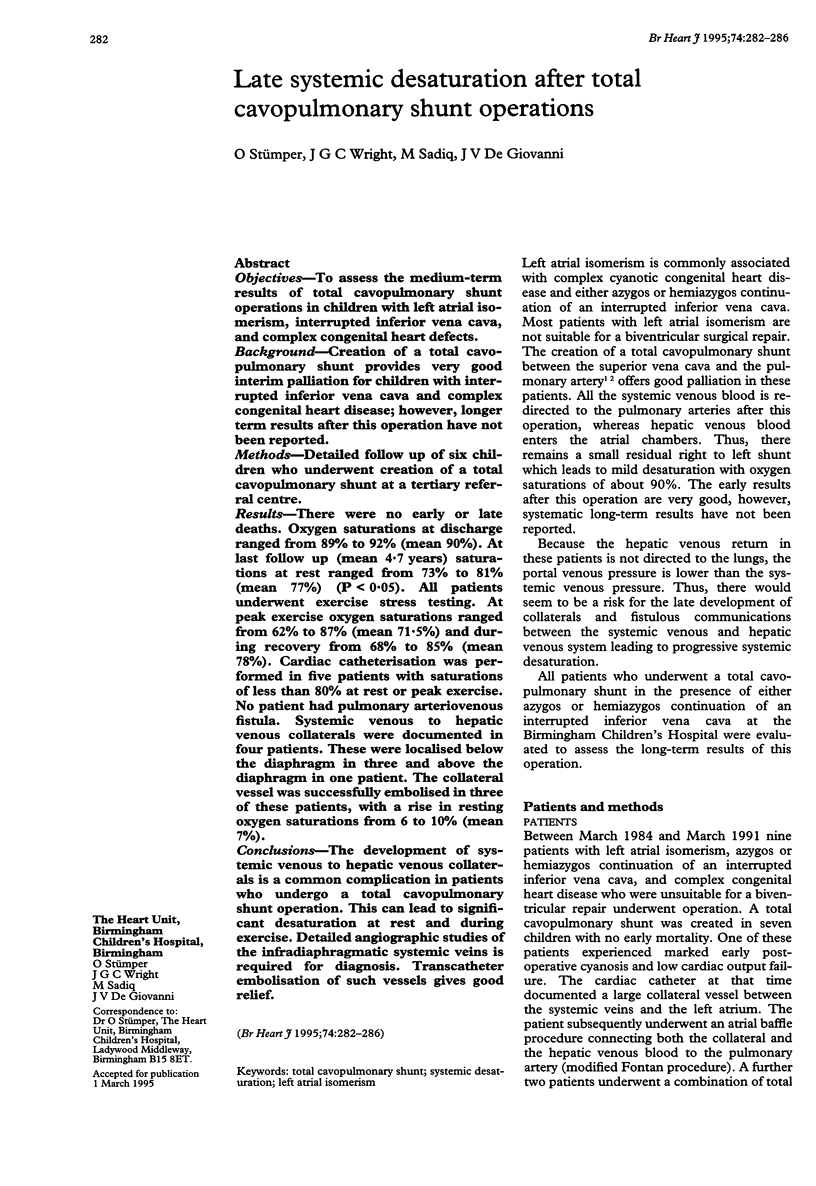

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bargeron L. M., Jr, Karp R. B., Barcia A., Kirklin J. W., Hunt D., Deverall P. B. Late deterioration of patients after superior vena cava to right pulmonary artery anastomosis. Am J Cardiol. 1972 Aug;30(3):211–216. doi: 10.1016/0002-9149(72)90060-4. [DOI] [PubMed] [Google Scholar]
- Cloutier A., Ash J. M., Smallhorn J. F., Williams W. G., Trusler G. A., Rowe R. D., Rabinovitch M. Abnormal distribution of pulmonary blood flow after the Glenn shunt or Fontan procedure: risk of development of arteriovenous fistulae. Circulation. 1985 Sep;72(3):471–479. doi: 10.1161/01.cir.72.3.471. [DOI] [PubMed] [Google Scholar]
- Furuse A., Koseni K., Takeshita M., Kotsuka Y., Yagyu K., Kawauchi M. Retrograde gastric varices in a patient with total cavopulmonary shunt. Ann Thorac Surg. 1993 Jun;55(6):1574–1575. doi: 10.1016/0003-4975(93)91117-6. [DOI] [PubMed] [Google Scholar]
- Kawashima Y., Kitamura S., Matsuda H., Shimazaki Y., Nakano S., Hirose H. Total cavopulmonary shunt operation in complex cardiac anomalies. A new operation. J Thorac Cardiovasc Surg. 1984 Jan;87(1):74–81. [PubMed] [Google Scholar]
- Kopf G. S., Laks H., Stansel H. C., Hellenbrand W. E., Kleinman C. S., Talner N. S. Thirty-year follow-up of superior vena cava-pulmonary artery (Glenn) shunts. J Thorac Cardiovasc Surg. 1990 Nov;100(5):662–671. [PubMed] [Google Scholar]
- Kreitmann P., Bourlon F., Jourdan J., Dor V. Surgical treatment of primitive ventricle and complex congenital heart malformation with total exclusion of the right heart: report of a case. J Thorac Cardiovasc Surg. 1982 Jul;84(1):150–150. [PubMed] [Google Scholar]
- Moore J. W., Kirby W. C., Madden W. A., Gaither N. S. Development of pulmonary arteriovenous malformations after modified Fontan operations. J Thorac Cardiovasc Surg. 1989 Dec;98(6):1045–1050. [PubMed] [Google Scholar]