Abstract
Introduction
Lumbar hernia account for less than 2% of al abdominal hernias, been the Grynfelt-Lesshaft's hernia (GLH) more frequent than the others. With approximately 300 cases published in the literature, the general surgeon may have the chance of treat it ones in their professional life.
Case report
A 42-years old male with human immunodeficiency virus and Diabetes Mellitus presented to the outpatient clinic with a GLH. Preoperative classified as a type “A” lumbar hernia an open approach was scheduled. We performed a Sandwich technique with a sublay and onlay ULTRAPRO® mesh fixed with PDS® II suture without complications and discharged the patient 24-h after. After six months, the patient denied any complication.
Discussion
Primary (spontaneous) lumbar hernias represent 50–60% of all GLH. The preoperative classification of a lumbar hernia is mandatory to propose the best surgical approach. According to the classification of Moreno-Egea A et al., the best technique for our patient was an open approach. The Sandwich technique has demonstrated good outcomes in the management of the GLH.
Conclusion
The surgical approach should be according to the classification proposed and to the experience of the surgeon. The Sandwich technique has good outcomes.
Keywords: Grynfelt hernia, Lumbar hernia, Grynfelt-Lesshaft hernia, Sandwich technique
Highlights
-
•
We present a Grynfelt-Lesshaft's hernia which account <2% of the abdominal hernias.
-
•
We document the new surgical approach for a Grynfelt-Lesshaft hernia.
-
•
We add a new case with a different technique with good outcomes.
1. Introduction
Grynfelt and Lesshaft described a hernia of the superior lumbar triangle in 1886 and 1870, respectively [1]. The lumbar region is an area bounded superiorly by the 12th rib, inferiorly by the iliac crest, medially by the erector spinae muscles, and laterally by the external oblique muscle. This area contains two well-defined areas of weakness: the inferior lumbar triangle (Petit's triangle), and the superior lumbar triangle (Grynfelt-Lesshaft's triangle) [2], [3], [4], [5]. The Grynfelt-Lesshaft triangle is an inverted triangle, which his boundaries are formed superiorly by the 12th thoracic rib, medially by the erector spinae muscle group, laterally by the internal oblique muscle. The floor of this triangle is formed by aponeurosis of the transversalis muscle, and the roof is formed by the latissimus dorsi muscle [2], [5], [6]. The Grynfelt's triangle has three well-described areas of weakness: immediately below the rib where the transversalis fascia is not covered by the external oblique muscle, in the area of fascial penetration of the 12th dorsal intercostal neurovascular pedicle, and between the inferior edge of the rib and the ligament of Henle [2], [3], [6].
With approximately 300 cases published in the literature [2], [3], the lumbar hernias represent 1.5%–2% of the abdominal hernias [7], [8], [9], been more frequent the Grynfelt's hernia [3], [5], [8], [10] Hafner et al. [9] stated that a general surgeon will have the opportunity to repair only one lumbar hernia case in his or her lifetime.
2. Case report
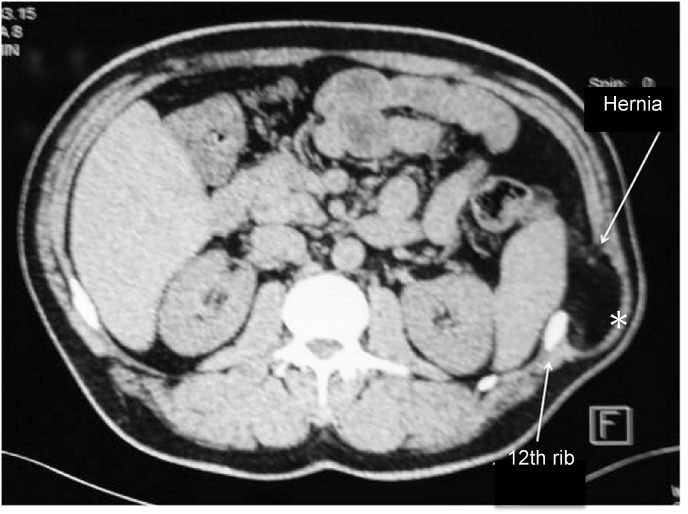
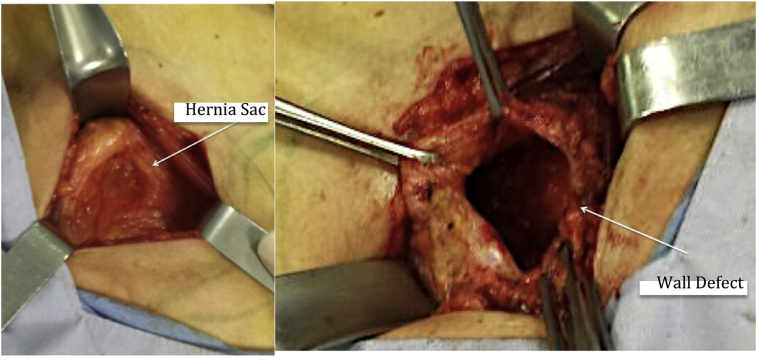
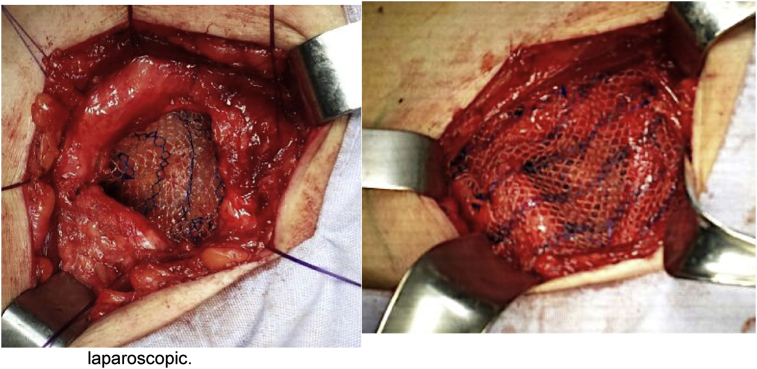
A 42-years male patient presented to the outpatient clinic referring a left lumbar mass that protrudes with efforts and reduced partially with ease. He is known to have human immunodeficiency virus (HIV), diabetes mellitus type 2, high blood pressure and an open cholecystectomy. On the physical examination we found, a left lumbar mass, soft and non-tender that reduced with manual compression and protruded when the patient coughed. The CT scan showed perisplenic fat protruding beneath the 12th rib (Fig. 1). The patient was scheduled for an elective repair of a Grynfelt-Lesshaft's hernia. The surgical approach was open with a lumbotomy incision, the sac was liberated of its adhesion and reduced, we encountered the hernia defect to measure approximately 10 cm with minor muscular atrophy (Fig. 2), the peritoneum was closed with a continuous absorbable suture; we repaired the wall defect by a Sandwich technique with a Sublay preperitoneal ULTRAPRO® mesh and an Onlay ULTRAPRO® mesh (Fig. 3). Both meshes were fixed with PDS® II suture. No immediate postoperative complications were seen, and we discharged the patient 24-h after the surgery.
Fig. 1.
CT scan shows protruding mass beneath the 12th rib. * shows the hernia content perisplenic fat.
Fig. 2.
Images are showing the hernia sac and wall defect after releasing the hernia sac.
Fig. 3.
The left image shows the sublay preperitoneal mesh and the right image shows the onlay mesh in the Sandwich technique.
3. Discussion
Lumbar hernias are a rare disease that can be congenital or acquired [2], [3], [5], [8]. The congenital hernias, which consist of 20% of all cases, are present in infants and children and are attributed to defects in the lumbar wall [2], [8], [10]. The acquired hernias that represent 80% of all, are subdivided in two [2], [3], [6], [10]: the spontaneous (primary) hernias which represent approximately 50–60% [2], [3]; the risk factors associated with its occurrence are elderly obese patients, extreme thinness, chronic debilitating disease, muscular atrophy, intense slimming, chronic bronchitis, wound infection, and postoperative sepsis [3].
As well as the secondary acquired hernias which have various mechanisms of pathogenesis: direct contusion, crushing, surgical lesions or infections of the pelvic bones and ribs, hepatic abscesses, infected retroperitoneal hematomas, and infectious processes that may alter the integrity of the lumbodorsal fascia [2], [3]. Our patient presented a primary acquired hernia probably due to the extreme thinness with muscular atrophy and the chronic debilitating disease (HIV). The most common clinical manifestation is a palpable non-tenderness lumbar mass that protrudes with coughing and physical activity [2], [3]. Although the most typical clinical presentation is as an elective outpatient, approximately in 9% of cases, the patient will show with symptoms of painful incarceration hernia or a strangulated hernia [3], [5].
Surgical treatment is the only therapeutic option and should be attempted early in the disease to avoid complications. The surgical approach will depend on the preoperative classification and the experience of the surgeon in the management of this disease. Loukas M et al. [6] described a postmortem classification of the Grynfelt's triangle accordingly to its measures into four types: type 0 (18%) when no triangle was formed, type I (50%) <5 cm2, type II (22%) 5–15 cm2 and, type III (10%) those larger than 15 cm2. As to our knowledge, the only preoperative classification of the Grynfelt's hernia with surgical implications was proposed by Moreno-Egea A et al. [3] (See Table 1), accordingly to their classification our patient presented a type “A” hernia and the surgical approach could be open or laparoscopic.
Table 1.
Classification of the Lumbar hernias [3] IP intraperitoneal. The presence of at least two criteria is necessary for defining a type.
| Characteristics | A | B | C | D (Pseudohernias) |
|---|---|---|---|---|
| Size cm | <5 | 5–15 | >15 | |
| Location | Superior | Inferior | Diffuse | |
| Contents | Extraperitoneal fat | Visceral | Visceral | |
| Etiology | Spontaneous | Incisional | Traumatic | |
| Muscular atrophy | No (minor) | Mild | Severe | Severe |
| Recurrence | No | Yes (open) | Yes (laparoscopic) | |
| Surgical approach | Open or laparoscopic approach | IP laparoscopy | Open approach | Open approach (double mesh) |
The advantages of the laparoscopic repair such as less postoperative pain, shorter in-hospital stay, and good cosmetic and functional results have been described [7], [11], [12]; nevertheless, advance laparoscopic skills and experience in the management of this disease are needed to perform the repair in this form. We decided to carry on an open approach because our previous experience as has been previously described by this type of hernia [12]. Different surgical techniques has been described (primary closure, fascial or gluteal flaps, and the use of mesh either underlay, inlay or onlay) [13], [14], but we decided to do a Sandwich hernia repair because it has been proven to have good outcomes in the ventral hernias management [15] . Also, Sahoo MR et al. [14] described four patients with a lumbar hernia treated with the Sandwich technique with no intraoperative or postoperative complications and a median follow-up ten months. Regarding open approaches to surgery no procedure has been shown to have definite advantages over the others, especially given the relative rarity of these cases. At 6-month follow-up, our patient has denied any complication such as pain, tenderness, numbness or recurrence.
4. Conclusion
Been the Grynfelt's hernia as infrequent as it is, the patients with this disease should be referred to a high volume Hospital with experience in the management of an abdominal hernia. The surgical approach should be individualized, although, the technique should be according to the Moreno-Egea A et al. [3] classification. We demonstrate that the Sandwich hernia repair is a safe procedure with good outcomes.
Conflict of interest
We declare no conflict of interest while writing the manuscript.
References
- 1.Liang T.J., Tsai C.Y. Grynfelt hernia. N. Engl. J. Med. 2013;369(11) doi: 10.1056/NEJMicm1213254. [DOI] [PubMed] [Google Scholar]
- 2.Cesar D., Valadão M., Murrahe R.J. Grynfelt hernia: case report and literature review. Hernia. 2012;16:107–111. doi: 10.1007/s10029-010-0722-8. [DOI] [PubMed] [Google Scholar]
- 3.Moreno-Egea A., Baena E.G., Calle M.C., Martínez J.A.T., Albasini J.L.A. Controversies in the current management of lumbar hernias. Arch. Surg. 2007;142:82–88. doi: 10.1001/archsurg.142.1.82. [DOI] [PubMed] [Google Scholar]
- 4.Tronco-Alves G.R., de-Andrade-Silva R.V., Missel-Corrêa J.R., Pereira-Haygert C.J. Grynfeltt-Lesshaft hernia. Ann. Gastroenterol. 2012;25(64) [PMC free article] [PubMed] [Google Scholar]
- 5.Walgamage T.B., Ramesh B.S., Alsawafi Y. Case report and review of lumbar hernia. Int. J. Surg. Case Rep. 2015;6:230–232. doi: 10.1016/j.ijscr.2014.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loukas M., El-Zammar D., Shoja M.M., Tubbs R.S., Zhan L., Protyniak B. The clinical anatomy of the triangle of Grynfeltt. hernia. 2008;12:227–231. doi: 10.1007/s10029-008-0354-4. [DOI] [PubMed] [Google Scholar]
- 7.Patnaik S., Nayak T.K., Patro S. Lumbar hernia: a case report and review of literature. Int. J. Sci. Study. 2015;3(8) [Google Scholar]
- 8.González-Rodríguez F.J., Gómez A.P., López M., Conde-Freire R.F., González-Vinagre S., Barreiro-Morandeira F. Hernia de Grinfelt. Discusión y manejo. Rev. Hispanoam. Hernia. 2014;2(2):63–66. [Google Scholar]
- 9.Hafner C.D., Wylie J.H., Brush B.E. Petit's lumbar hernia: repair with Marlex mesh. Arch. Surg. 1963;86:180–186. doi: 10.1001/archsurg.1963.01310080004002. [DOI] [PubMed] [Google Scholar]
- 10.Skrekas G., Stafyla V.G., Papalois V.E. A Grynfeltt hernia: report of a case. Hernia. 2005;9:188–191. doi: 10.1007/s10029-004-0278-6. [DOI] [PubMed] [Google Scholar]
- 11.Moreno-Egea A., Torralba-Martinez J.A., Morales G., Fernández T., Girela E., Aguayo-Albasini J.L. Open vs laparoscopic repair of secondary lumbar hernias. A prospective nonrandomized study. Surg. Endosc. 2005;19:184–187. doi: 10.1007/s00464-004-9067-7. [DOI] [PubMed] [Google Scholar]
- 12.Suarez S., Hernandez J.D. Laparoscopic repair of a lumbar hernia: report of a case and extensive review of the literature. Surg. Endosc. 2013;27:3421–3429. doi: 10.1007/s00464-013-2884-9. [DOI] [PubMed] [Google Scholar]
- 13.Mismar A., Al-Ardah M., Albsoul N., Younes N. Underlay mesh repair for spontaneous lumbar hernia. Int. J. Surg. Case Rep. 2013;4:534–536. doi: 10.1016/j.ijscr.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahoo M.R., Kumar T.A. Sandwich technique of closure of lumbar hernia: a novel technique. Int. J. Case Rep. Images. 2013;4(5) [Google Scholar]
- 15.Martín-Cartes J.A., Tamayo-López M.J., Bustos-Jimenez M. ‘Sandwich’ technique in the treatment of large and complex incisional hernias. ANZ J. Surg. 2015 doi: 10.1111/ans.13285. [DOI] [PubMed] [Google Scholar]