Abstract
Background
Zuckerkandl tubercle (ZT) is a lateral projection from the lateral thyroid lobe which is a constant landmark for finding the recurrent laryngeal nerve during thyroid surgery. It is the condensed thyroid parenchyma located in the cricothyroid junction. Even today, ZT and its relationship with recurrent laryngeal nerve (RLN) is not well known by all surgeons. The objectives of the present study were to find out the incidence of ZT in our thyroidectomies and to investigate whether the ZT has a relationship with RLN. We also discussed how to prevent RLN injury during thyroidectomy.
Materials and methods
One hundred operations were performed by the same surgeon included in this study. All operations performed with intraoperative neuromonitorization (IONM) for proving the visualization of RLN. In each patient, particularly the ZT and its relationship with RLN searched and recorded. We also analyzed the patients in terms of sex, age, clinical diagnosis, and types of performed operations.
Results
In 100 operations, 173 thyroid lobectomies were considered. 87 of these lobectomies were in right side and 86 in left side. The ZT was determined in 127 of 173 (73.41%) lobectomies. ZT was detected in 68 (78.16%) of right thyroid lobes whereas in 59 (68.60%) of left thyroid lobes. We observed that the ZT was detected more frequently in the right side. In 115 (90.55%) of these occasions, the recurrent nerve was directed upwards covered by the ZT.
Conclusions
If it is present, ZT is a real constant landmark pointing to the RLN. In order to find and protect RLN during thyroid surgery, a careful, bloodless, and meticulous dissection should be carried out around the ZT. Although our results are encouraging, further researches are still needed on this topic.
Keywords: Zuckerkandl, Thyroid, Landmark, Laryngeal nerve
Highlights
-
•
Zuckerkandl tubercle (ZT) is a lateral projection from the lateral thyroid lobe.
-
•
Even today, ZT and its relationship with recurrent laryngeal nerve (RLN) is not well known by all surgeons.
-
•
If it is present, ZT is a real constant landmark pointing to the RLN.
-
•
In order to find and protect RLN during thyroid surgery, a careful dissection should be carried out around the ZT.
1. Introduction
The recurrent laryngeal nerve (RLN) is very important for airway and voice quality. Unilateral injury of the RLN during thyroid surgery can cause hoarseness of voice and dysphagia. The consequences are more severe and life-threatening in bilateral injuries, which may compromise the airway and necessitate immediate tracheostomy. Rates of RLN injury are reported to be as high as 10%. The RLN identification and protection during thyroid surgery is essential for avoiding intraoperative RLN injury [1], [2], [3], [4], [5], [6], [7], [8], [9].
In 1902, Emil Zuckerkandl (1849–1910), an Austrian anatomist described a protuberance which arises from the posterior border of thyroid lobes [1]. He named this protubarance as processus posterior glandulae thyroidea [2]. It is commonly seen as a thickening or a nodule in the posterior aspect of the gland. Today it is called Zuckerkandl tubercle (ZT) [3], [4]. Thirty-six years later, Gilmour described a possible relationship between ZT and the recurrent nerve, he also mentioned its proximity to the upper parathyroid glands. However, this anatomical relationship, did not attract the attention of surgeons during the subsequent half century. Today it is accepted by some authors that this structure is usually present as a lateral projection from the lateral thyroid lobe with a close relationship to the extralaryngeal termination of the recurrent laryngeal nerve [1], [2], [3], [4], [5], [6]. They suggested that, it may be a useful landmark to find and protect the RLN during thyroid surgery but others do not agree [7]. Additionally, some authors were reported that leaving ZT in the operation field may cause an insufficient surgery [3], [4], [5], [6].
The primary objective of the present study was to find out the incidence of ZT in our thyroidectomies and our secondary objective was to investigate whether the ZT has a relationship with RLN. We also discussed how to prevent RLN injury during thyroidectomy.
2. Materials and methods
2.1. Study design and the extent of surgery
This study was approved by the ethics committee of the Adana Numune Research and Training Hospital. The present study was designed as a descriptive study and carried out on patients who underwent thyroid surgery from 1st January 2013 to 31st December 2015. 113 operations performed under IONM of RLN in our hospital. 13 of these operations were complementary surgery which were referred from other hospitals did not included in this study. The inclusion criteria were all cases of primary total thyroidectomy or lobectomy, with or without central neck dissection. Revision surgical cases and operations performed without IONM were excluded. 100 operations included in this study. Operations were performed by the same medium volume surgeon (50–70 thyroidectomies/year) (Oİ). The IONM was strictly used in all cases in order to prove the dissection and visualization of RLN. The mean age of the patients was 47 years, ranging between 18 and 82 (M/F was 15/85). There were 73/100 total thyroidectomies (73%), and 27/100 hemithyroidectomies (27%). Of the hemithyroidectomies, 14/27 were right and 13/27 were left. So we were able to analyse 173 thyroid lobe (87 right and 86 left) (Table 1). We also analyzed the structure in terms of sex, age, clinical diagnosis, and types of operations. The datas were recorded according to observation sheets and operation datas.
Table 1.
Indications of patients for thyroid surgery.
| Operation indication | n |
|---|---|
| Multinodular goitre | 28 |
| Malignancy or suspicion of malignancy in FNAC | 22 |
| Graves-Basedow disease | 6 |
| Follicular neoplasia | 6 |
| Hurtle cell neoplasia | 2 |
| Toxic multinodular goitre | 8 |
| Toxic nodulary goitre | 6 |
| Nodulary goitre | 22 |
| Total | 100 |
2.2. Surgical technique
All operations were performed on patients under general anaesthesia by one experienced surgeon (Oİ). A similar thyroidectomy technique was choosed to perform which is also used with Pelizzo et al. [8] who were described ZT classification [8]. In this technique, an approach to the RLN from Zuckerkandl tubercle was preferred instead of classically using inferior thyroid artery as an anatomic landmark. The phases of operation is almost all the same as in the current standard procedure [8], [9]. Firstly, the middle thyroid vein sectioned in order to achive a good thyroid mobilization and making visible the cricothyroid space. Secondly, the superior pole vessels are ligated and divided carefully with protecting the external branch of the superior laryngeal nerve after that the inferior thyroid veins are subsequently divided also [8], [9], [10]. Thirdly, after the thyroid lobe is gently retracted to medial, it released from the surrounding thin areolar tissue by bloodless blunt dissection. The extra capsular plane was followed for dissection [10]. Fourthly, we begin the RLN dissection with delicate workmanship by looking specifically for Zuckerkandl tubercle. It is easy to identify, if it is well-developed. As it is described by Pezillo [8], when it is encountered, the tuberculum looks like an arrow pointing toward the nerve. Frequently the nerve runs in a tunnel deep behind the tubercule. Additionally, the nerve may lies in front when the tuberculum is a very small lateral projection or only a thickening of the lateral edge of thyroid lobes [8], [9], [10], [11], [12], [13], [14]. In each patient, the ZT searched. If present, its relationship with RLN investigated and then recorded. To avoid a RLN injury, the dissection should be done very carefully. The crucial aspect of RLN dissection in this region is to dissect beyond the lateral border of the tubercle and lift it up to ensure that the RLN is not damaged. We do not carry out subtotal thyroidectomies.
All operations performed with intraoperative neuromonitorization (IONM) for proving the visualization of RLN. We facilitated the visual identification of the RLN via the IONM system, with the nerve mapping technique. Once, we carefully identified the RLN, repeated stimulations with the monopolar probe of the IONM system served to trace the nerve path in the operative field. We always tested its functional integrity during dissection and before finishing the operation.
2.3. Characteristics of patients
The preoperative clinical indications for thyroid surgery as follows: Multinodular goitre in 28 patients, malignancy or suspicion of malignancy in FNAC in 22 patients, Graves-Basedow disease in 6 patients, follicular neoplasia in 6 patients, hurtle cell neoplasia 2 patients, toxic multinodular goitre in 8 patients, toxic nodular goitre in 6 patients, and nodular goitre in 22 patients. The characteristics of the patients are presented in (Table 1). In the excluded patients, operation indications were for recurrent multinodular goitre (4 patients) and malignancy (9 patients).
2.4. ZT classification
We studied the percentage of cases in which the ZT was certainly detected and when it appeared in the right lobe and when in the left lobe. Size of the tubercle was measured intraoperatively by using a sterilized needle with calibrations in millimeters. We modified the classification system described by Pelizzo et al. [8] because according to that grading system, grades 0 (unrecognizable) and 1 (only a thickening of the lateral lobe) tubercles may not help surgeon to indicate the location of the nerve and can not be applied from a surgical perspective. Therefore, we revised the grading system as grade 0/1: when the ZT was not recognised; grade 2: the ZT is less than 10 mm; grade 3: the ZT is more than 10 mm.
3. Results
There was no RLN injury in this study. Of the 173 thyroid lobectomies considered. 87 of 173 lobectomies were performed in the right side whereas 86 were in the left side. we located the ZT in 127 of 173 (73.41%) lobectomies. In the RL, ZT detected in 68 of 87 (78.16%) lobectomies whereas it is existed in 59 of 86 (68.60%) left lobectomies. We observed that the ZT was detected more frequently in the right side. The ZT was not detected in 46/173 thyroid lobectomies (26.58%).
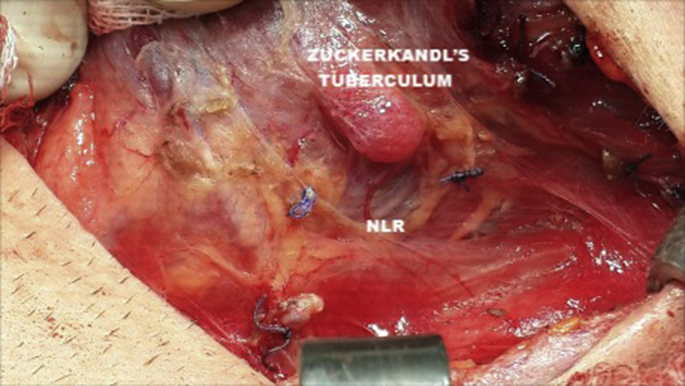
On 115/127 occasions (90.55%) the recurrent nerve was directed upwards covered by the ZT; the nerve followed a channel under the ZT and lateral to the surface of the trachea and the Berry ligament (Fig. 1). In 46 of 173 (26.58%) lobectomies, ZT was not recognised (Grade 0/1). In 92 (53.17%) lobectomies ZT were less than 10 mm. In the remaining 35 (20.23%) lobectomies ZT were more than 10 mm (Table 2).
Fig. 1.
The tuberculum looks like an arrow pointing toward the nerve. Frequently the nerve runs in a tunnel deep behind the tuberculum.
Table 2.
Grades of Zuckerkandl tubercle in lobectomies.
| Grade | n (number of lobectomies) | % |
|---|---|---|
| 0 and 1 (Absent or Unrecognisable) | 46 | 26.58 |
| 2 (ZT ≤ 10 mm) | 92 | 53.18 |
| 3 (ZT > 10 mm) | 35 | 20.24 |
| Total | 173 | 100 |
4. Discussion
It is generally accepted that iatriogenic injury of RLN and subsequent paralysis of vocal cords is one of the most serious complication in thyroid surgery. Unfortunately, when it is occur bilaterally, it may results with serious functional problems [15], [16]. These are respiratory, phonatory, and psychological problems which may have an negative affect on working capacities and social relationships of the patients [15]. Therefore, the most important key aim of thyroid surgery is to minimize as much as possible the incidence of RLN palsy [16]. Iatriogenic injury to the RLN may be prevented by its full and careful isolation based on good knowledge of the anatomy [1]. Some authors stated that the ZT and RLN have close relationship which increases their surgical importance. According to their experience, although, ZT is a constant landmark for RLN and for superior parathyroid, careful and meticulous dissection around the tubercle is mandatory for safety of thyroid operations [7], [8], [9], [10], [11], [12], [13], [14]. Embryologically, the thyroid gland mainly develops from 3 anlages: median anlage is the larger and lateral anlages are the smaller. ZT occurs from the embryologic fusion of the ultimobranchial body with the median anlage and the lateral thyroid anlages of the fourth pharyngeal pouch. The RLN usually passing medial to ZT in the tracheo esophageal groove [17] (Video 1). In this study we firstly aimed to investigate the incidence of ZT in our thyroidectomies and secondly to investigate whether the ZT has a relationship with RLN.
The following is the supplementary data related to this article:
The RLN usually passing medial to ZT in the tracheo esophageal groove.1
It is known that, various studies have been performed on the incidence of ZT and its relationship to the RLN in many countries. Surprisingly, these studies have showed different incidences among different populations. The highest incidences of ZT have been reported as 90% and 88.75% from Sri Lankan and Turkey, respectively [13], [18]. In Malaysia, the incidence has been concluded as 80.2% whereas 77% in Italy, 63% in Australia, and 45% in Rome [8], [11], [12], [13], [14]. This study is conducted in the Mediterranean region of Turkey. In the present study, 173 thyroid lobectomies considered and ZT determined in 127 of 173 (73.41%) lobectomies. These differences may be due to the geographic, national and genetic variations. Additionally, it may be also due to the accuracy and perseverance of searching ZT during thyroidectomy as reported by Pelizzo et al. [8]. An operating telescope might help in such recognition, but more important is that a search should be made [8], [9].
A Rajapaksha and et al. [18] reported that the ZT was present on the right side in 70 (88%) patients and on the left side in 57 (71%) patients. Additionally, Elisa Gil-Carcedo and et al. [3] concluded that ZT was present on the right side in 84 (84.84%) patients and on the left side in 71 (73.95%) patients. Most of the investigators observed that the ZT was detected more frequently in the right side [5]. In this study, we found that ZT existed on the right side in 68 of 87 (78.16%) patients and on the left lobe in 59 of 86 (68.60%) patients. We also observed that the ZT was detected more frequently in the right side. These result were consistent with the literature [3], [5]. More frequently detection of ZT in the right side may be due to the embryological difference of the two sides in relation to pharyngeal arches.
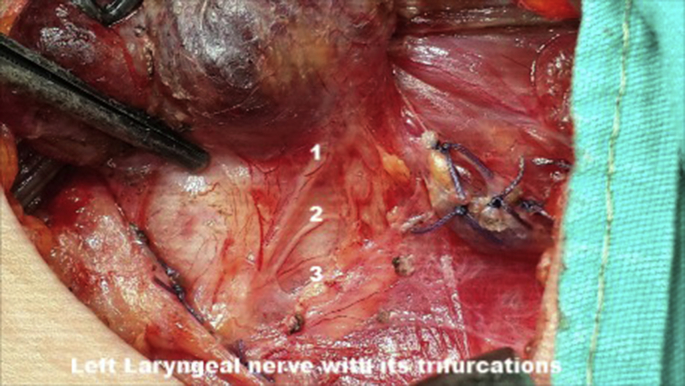
Elisa Gil-Carcedo and et al. [3] reported that on 147 occasions (94.83%), the recurrent nerve was directed towards the cricothyroid membrane beneath the Zuckerkandl tubercle, laterally to the tracheal surface in relation with the Berry ligament. In the present study, we determined that ZT detected in 127 occasions. In 115 (90.55%) of these occasions, the recurrent nerve was directed upwards covered by the ZT; the nerve followed a channel under the ZT (Fig. 1). The remainings are 1 cm around the ZT. These result were consistent with the current literature [3], [4], [5]. The author, like many other researchers, would like to underline that when it is present, ZT is a reliable and fixed anatomical landmark pointing to the RLN and is a “helper” of experienced thyroid surgeon [2], [3], [11], [13]. On the other hand, when large and if the surgeon is inexperienced, it may also increase the rate of insufficient surgery and complications. In other words, not surprisingly, the constant relationship between the RLN and ZT may cause a potential danger for nerve in the hands of inexperienced surgeons as reported by Koçak and Aydintug [7]. They stated that the recurrent nerve can have two or more branches in some cases. One of those branches may be localized just in the tunnel described previously, the others may pass more anterior or posteriorly. Identifying the first branch can mislead the surgeon not to search for the others (Fig. 2). Therefore, a thyroid surgeon should be aware of the all anatomic variations of the gland and of adjacent structures and must have a thorough knowledge of the normal anatomy to achive a high standard of care [19], [20], [21], [22]. Additionally, it has therefore been recommended that an understanding of the embryology is important, and the combined embryological and anatomical approach to thyroid surgery is more useful than a purely anatomical one [2], [12]. ZT is also the site for maximum density of C cells, making its resection mandatory in total thyroidectomy for medullary thyroid cancer.
Fig. 2.
Left laryngeal nerve with its trifurcation.
In this study, the author used a classification system which is a modification of described by Pelizzo et al. [8]. According to that grading system, grade 0 indicates an ZT unrecognizable and grade 1 indicates only a thickening of the lateral lobe. So that, In daily surgical practice grade 0 and 1 tuberculum, was an irrelevant parameter and these tubercles can not detectable during thyroid surgeries especially in patients with multiple nodules. Therefore, the author of this study believe that grade 0 and 1 tuberculum should be ignored. As also stated by Petros Milas [21], Pelizzo's system seems problematic. Further refinements for both diseased and normal thyroids may therefore be needed, not necessarily using the same grading for hyperplasia/neoplasia and normal variations of the thyroid [13], [21]. So that, similar to the recommendations of Miliras [21], a modified classification system was used in this study. In 46 of 173 (26.58%) lobectomies, ZT were not recognised (grade 0/1), In 92 (53.17%) lobectomies ZT were less than 10 mm (grade 2) and in the remaining 35 (20.23%) lobectomies ZT were more than 10 mm (grade 3). This study showed that most of the ZT in our patients were less than 10 mm and the surgeon should be careful for recognising it. These results were similar to the current literature. On the other hand, the author believes that the sizes of ZT may vary according to multiple factors such as the volume of thyroid gland, the severity of the thyroid disease, and the number of nodules. Therefore, such grading system is infact do not have an importance in surgical practice. A new and practical classification should be made which can be applied from a surgical perspective. Our study carried out in patients with primary surgery but future investigations should also be carried out in patients with secondary surgery.
Our study has some limitations. This study was conducted on a group of patients who are living in Mediterranean region of Turkey. Additionally, the patients were operated by a single surgeon in a single institute. The size of the tubercle was measured approximately by using a non-standard instrument. Therefore, these finding should not be fully generalized to the other parts of the world. Although our results are encouraging, further researches are still needed on this topic.
5. Conclusion
The main factors influencing a reduction of RLN injury rates are meticulous dissection technique and respect of the gold standard that includes routine visualization of the RLN. The most important landmarks for RLN dissection are: the Berry ligament and the inferior thyroid artery. Our results showed that ZT may also help to the identification of RLN during thyroid surgery. On the other hand, if the surgeon is inexperienced and unaware of ZT, it may heighten the rate of insufficient surgery and complications such as RLN injury. Therefore, a thyroid surgeon should have complete knowledge of embryological development of the gland, all anatomic variations with adjacent structures and must have a thorough knowledge of the landmarks to achieve a high standard of care.
Ethical approval
This study was approved by the ethics committee of the Adana Numune Research and Training Hospital.
Funding
No funding was used.
Author contribution
Oktay irkorucu: Designed the study, Collected the datas, Analysed the datas, and wrote the manuscript.
Declaration of interest
The author reports no conflicts of interest. The author alone are responsible for the content and writing of the paper.
Guarantor
There is no guarantor other than the author. The author alone are responsible for the content and writing of the paper.
Research registration unique identifying number (UIN)
Researchregistry863.
References
- 1.Zuckerkandl E. Nebst Bermerkungen uber die Epithelkorperchen des Menschen. Anat. Hefte. 1902;LXI:61. [Google Scholar]
- 2.Gurleyik E., Gurleyik G. Incidence and surgical importance of Zuckerkandl's tubercle of the thyroid and its relations with recurrent laryngeal nerve. ISRN Anat. 2012;1:1–5. doi: 10.5402/2012/450589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gil-Carcedo Elisa, Mene ´ndez Marı ´a E., Vallejo Luis A., Herrero David, Gil-Carcedo Luis M. The Zuckerkandl tubercle: problematic or helpful in thyroid surgery? Eur. Arch. Otorhinolaryngol. 2013;270:2327–2332. doi: 10.1007/s00405-012-2334-7. [DOI] [PubMed] [Google Scholar]
- 4.Shoja M.M., Tubbs R.S., Loukas M., Shokouhi G., Jerry Oakes W. Emil Zuckerkandl (1849-1910): anatomist and pathologist. Ann. Anat. 2008;190(1):33–36. doi: 10.1016/j.aanat.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Mehanna R., Murphy M.S., Sheahan P. Thyroid tubercle of Zuckerkandl is more consistently present and larger on the right: a prospective series. Eur. Thyroid. J. 2014;3:38–42. doi: 10.1159/000355823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurleyik E., Dogan S., Gunal O., Pehlivan M. The rare coincidence: nonrecurrent laryngeal nerve pointed by a Zuckerkandl's tubercle. Case Rep. Med. 2012;2012:143049. doi: 10.1155/2012/143049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koçak S., Aydintug S. Zuckerkandl's tuberculum. J. Am. Coll. Surg. 2000;190:98–99. doi: 10.1016/s1072-7515(99)00231-8. [DOI] [PubMed] [Google Scholar]
- 8.Pelizzo M.R., Toniato A., Gemo G. Zuckerkandl's tuberculum: an arrow pointing to the recurrent laryngeal nerve (Constant Anatomical Landmark) J. Am. Coll. Surg. 1998;187:333–336. doi: 10.1016/s1072-7515(98)00160-4. [DOI] [PubMed] [Google Scholar]
- 9.Akin J.T., Skandalakis J.E. Technique of total thyroid lobectomy. Am. Surg. 1976;42:648–652. [PubMed] [Google Scholar]
- 10.Wang C. The use of the inferior cornu of the thyroid cartilage in identifying the recurrent laryngeal nerve. Minerva Chir. 1993;48:189–191. [PubMed] [Google Scholar]
- 11.Hisham A.N., Aina E.N. Zuckerkandl's tubercle of the thyroid gland in association with pressure symptoms: a coincidence or consequence? ANZ J. Surg. 2000;70:251–253. doi: 10.1046/j.1440-1622.2000.01800.x. [DOI] [PubMed] [Google Scholar]
- 12.Gauger P.G., Delbridge L.W., Thompson N.W. Incidence and importance of the tubercle of Zuckerkandl in thyroid surgery. Eur. J. Surg. 2001;167:249–254. doi: 10.1080/110241501300091363. [DOI] [PubMed] [Google Scholar]
- 13.Yalcin B., Tatar I., Ozan H. The Zuckerkandl tubercle and the recurrent laryngeal nerve. Am. J. Surg. 2008;196:311–312. doi: 10.1016/j.amjsurg.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 14.Gravante G., Delogu D., Rizello A., Filingeri V. The Zuckerkandl tubercle. Am. J. Surg. 2007;193:484–485. doi: 10.1016/j.amjsurg.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 15.Sturniolo G., D'Alia C., Tonante A., Gagliano E., Taranto F., Lo Schiavo M.G. The recurrent laryngeal nerve related to thyroid surgery. Am. J. Surg. 1999;177:485–488. doi: 10.1016/s0002-9610(99)00101-4. [DOI] [PubMed] [Google Scholar]
- 16.Serpell Jonathan W. New operative surgical concept of two fascial layers enveloping the recurrent laryngeal nerve. Ann. Surg. Oncol. 2010;17:1628–1636. doi: 10.1245/s10434-010-0928-0. [DOI] [PubMed] [Google Scholar]
- 17.Lee T.C., Selvarajan S.K., Curtin H., Mukundan S. Zuckerkandl tubercle of the thyroid: a common imaging finding that may mimic pathology. Am. J. Neuroradiol. 2012;33:1134–1138. doi: 10.3174/ajnr.A2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajapaksha A., Fernando R., Ranasinghe N., Iddagoda S. Morphology of the tubercle of Zuckerkandl and its importance in thyroid surgery. Ceylon Med. J. 2015;60(1):23–24. doi: 10.4038/cmj.v60i1.7141. [DOI] [PubMed] [Google Scholar]
- 19.Page C., Monet P., Peltier J., Bonnaire B., Strunski V. Non-recurrent laryngeal nerve related to thyroid surgery: report of three cases. J. Laryngol. Otol. 2008;122(7):757–761. doi: 10.1017/S0022215107008389. [DOI] [PubMed] [Google Scholar]
- 20.Makay O., Icoz G., Yilmaz M., Akyildiz M., Yetkin E. The recurrent laryngeal nerve and the inferior thyroid artery—anatomical variations during surgery. Langenbeck's Arch. Surg. 2008;393(5):681–685. doi: 10.1007/s00423-008-0320-8. [DOI] [PubMed] [Google Scholar]
- 21.Mirilas Petros. Grades of Zuckerkandl's tubercle in normal thyroids. Surg. Today. 2007;237:918. doi: 10.1007/s00595-007-3510-z. [DOI] [PubMed] [Google Scholar]
- 22.Bhargav P.R.K. Salient anatomical landmarks of thyroid and their practical significance in thyroid surgery: a pictorial review of thyroid surgical anatomy (revisited) Indian J. Surg. 2014;76(3):207–211. doi: 10.1007/s12262-013-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The RLN usually passing medial to ZT in the tracheo esophageal groove.1