Abstract
Actinomyces spp are found in the flora of the oral cavity and vagina and may cause infection with abscess formation and draining sinuses. Cervicofacial manifestations of actinomycosis involve head and neck soft tissue, however, spread to the cervical spine is rare. We report a case of an 8-year-old boy, presenting with neck pain for 1 month and denying a history of trauma or procedures. Radiography revealed an ulceration of the posterior oropharyngeal mucosa with a defect extending to the C1-C2 vertebra, mimicking a neoplastic process. The patient underwent laryngoscopy and multiple biopsies were taken from the ulcer and bone, showing severe osteomyelitis and intraosseous filamentous organisms, morphologically consistent with Actinomyces spp. The boy received long-term antibiotics with response to treatment. Actinomycosis has rarely been reported in the cervical vertebrae of paediatric patients. This should be considered as a differential diagnosis for such a presentation as prompt antibiotic treatment may be lifesaving.
Background
Actinomyces spp are Gram-positive, filamentous and non-motile anaerobic bacteria, often found in the normal flora of the oral cavity and vaginal tract. These bacteria are occasionally responsible for indolent infections causing chronic disease with abscess formation and draining sinuses that may express sulfur granules. Actinomycosis of the cervicofacial region is a relatively rare condition, however, this region is the most common anatomical location for Actinomyces spp infection, accounting for approximately 50–65% of cases.1 2 Adults with dental caries, gingivitis or gingival trauma are at the greatest risk for infection, as well as the immunocompromised and patients who have undergone recent dental procedures. Clinical presentation includes ‘woody’ fibrosis, indurated, cutaneous and soft tissue swelling with or without abscess formation and, rarely, direct bony invasion. The indolent course and soft tissue indurated lesions allow this entity to be frequently confused with neoplasms, especially in the absence of suppuration. We present a case of a paediatric patient with actinomycosis spread to the cervical vertebrae, which is a rare life-threatening condition that can mimic a neoplastic process.
Case presentation
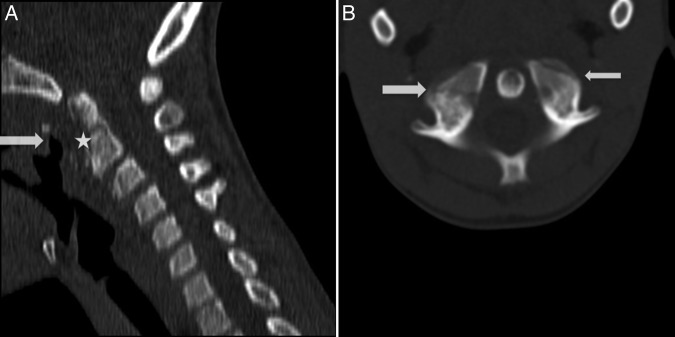
We report a case of an immunocompetent, afebrile 8-year-old boy, with no significant medical history, who presented to an outpatient clinic with slowly progressive neck pain for 1 month, with no neurological deficits and denying a recent history of trauma or dental procedures. CT images of the cervical spine were acquired without contrast from the skull base to the upper thoracic region (figure 1). The CT images demonstrated an ulceration extending from the dorsal oropharynx, with adjacent soft tissue thickening. Extensive erosive change of the anterior C1 arch and the odontoid process was demonstrated. In addition, there were irregular lucencies that extended to the C1 lateral masses, concerning for pathological fractures. MRI of the cervical spine was performed with and without contrast (figure 2). The MRIs showed erosive changes to the posterior oropharyngeal mucosa, with abnormal bone marrow oedema involving the C1 lateral masses and pedicles and odontoid process and the body of C2. The remaining vertebral bodies were free of marrow oedema. There was diffuse prevertebral soft tissue swelling; however, there was no evidence of epidural disease. The postcontrast images were limited due to patient motion artefacts.
Figure 1.
(A) Sagittal CT image of the cervical spine demonstrating extensive erosive changes of the anterior C1 arch and the anterior odontoid process (white star). There is adjacent ulceration of the dorsal oropharynx with adjacent soft tissue swelling (white arrow). (B) Axial CT image demonstrating irregular lucencies through the lateral masses of the C1, concerning for pathological fractures (white arrows).
Figure 2.
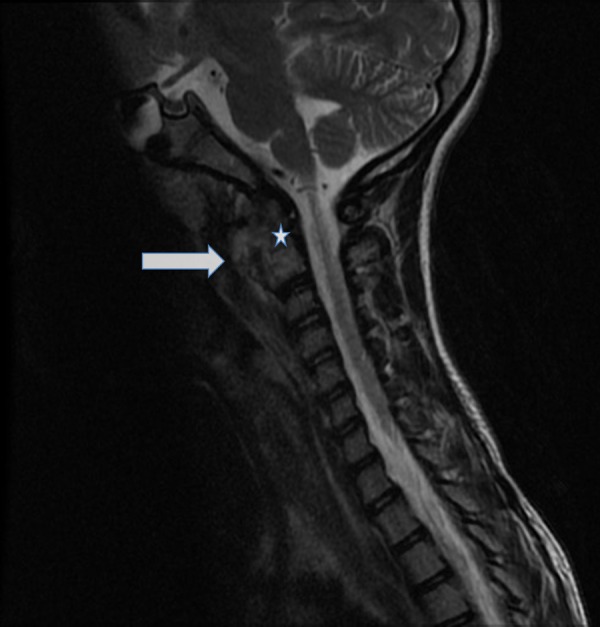
Sagittal T2-weighted MRIs demonstrating prevertebral soft tissue oedema (white arrow) and bone marrow oedema involving the C1 and the odontoid process (white arrow). No evidence of epidural disease is seen.
Investigations
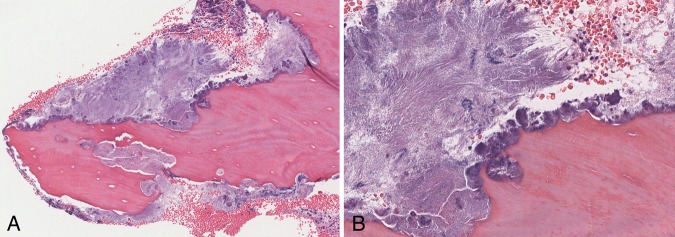
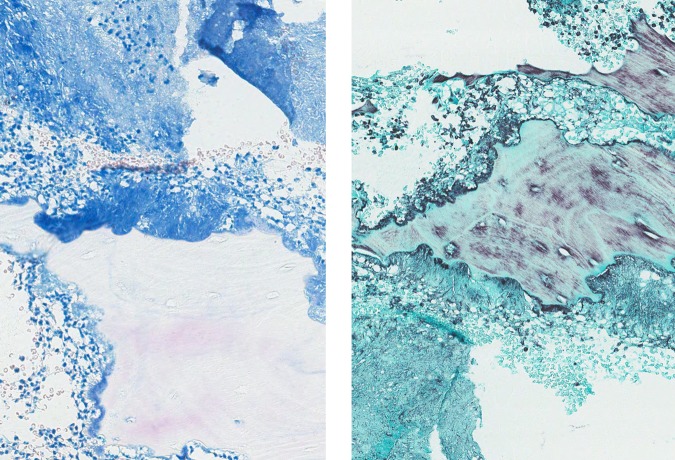
The patient underwent laryngoscopy, which found a deep ulcer surrounded by granulation tissue involving the posterior oropharyngeal wall, extending into the lower part of the nasopharynx. Subsequent debridement and biopsies of the ulcer and the odontoid process of the cervical spine showed severe acute osteomyelitis with osteonecrosis, remodelling, fragments of granulation tissue and fibrosis (figure 3). In addition to acute inflammation, intraosseous filamentous organisms, morphologically consistent with Actinomyces spp, were identified and supported by a positive Gomori methenamine silver stain and a negative acid-fast bacilli (AFB) stain (figure 4). Gram stain and tissue cultures were unremarkable.
Figure 3.
(A) Bone fragment showing severe acute osteomyelitis, osteonecrosis and organisms (H&E stain20). (B) Aggregate of filamentous organisms morphologically consistent with Actinomyces species (H&E stain ×200).
Figure 4.
Actinomyces colonies highlighted by Gomori methenamine silver stain (left) with negative acid-fast bacilli stain (right).
Differential diagnosis
On the basis of clinical presentation and radiographical findings, several differential diagnoses may be considered. When the bone marrow abnormality and erosive changes are confined to one or two adjacent vertebral body levels, infectious aetiology is high on the differential. Especially in the presence of adjacent soft tissue erosion, as in this case, the soft tissue defect is a likely source of direct inoculation. However, malignant intraosseous neoplasms can also present with similar radiological appearance. In this patient's age group, Ewing's sarcoma, osteogenic sarcoma and metastases are the most common malignant neoplasms involving the spine.
Outcome and follow-up
The patient was started on intravenous antibiotics, ampicillin/sulbactam and then switched over to oral penicillin for 4 weeks at discharge. At a 2-month follow-up, the boy showed great response to long-term antibiotics treatment and was pain free with improved range of motion.
Discussion
Cervicofacial actinomycosis infections are caused by Gram-positive bacteria belonging to the genus Actinomyces and A. israelii is the most common species responsible for actinomycosis in humans, however, A. odontolyticus may also be involved. Disruption of the mucosal barrier is an essential role in the pathogenesis of cervicofacial infections, as seen in cases with patients with poor dental hygiene, prior dental procedures and oral trauma. The subsequent invasion of the soft tissue can lead to slow contiguous spread ignoring tissue planes and, with time, sinus tracts may extend the infection into adjacent skin, organs or bone.
Infection with cervicofacial involvement is very uncommon in the USA, with a large domestic study showing incidence to be about 1 per 300 000 persons.3 The most commonly involved site is the angle of the jaw or the submandibular region, followed by the cheek, submental space, masticator space and the temporomandibular joint.4 Actinomycosis has rarely been reported in the cervical vertebra of paediatric patients. Several case reports have reported cervical spinal cord compression secondary to epidural oedema or abscess formation from Actinomyces spp. Clinically, these patients present with neurological deficits, however, these symptoms were progressive and most commonly preceded by neck pain.5 6 Proper and prompt diagnosis must be made because involvement of the cervical vertebra can potentially lead to central nervous system involvement, irreversible neurological damage or death. Abscess drainage and surgical debridement of bone and necrotic tissue along with antibiotic treatment may be lifesaving.
When reviewing radiographic findings in the cervical vertebra, a helpful rule of thumb in distinguishing neoplastic from infectious aetiologies is preservation of the disk space. The infectious process tends to involve the adjacent disk space causing a loss of disk height, while the neoplasms tend to preserve disk space.7 Unfortunately, for our patient, who had C1 and C2 joints that did not contain disk space, this criterion could not be used to help narrow down the differential.
The definitive diagnosis is made by tissue biopsy and culture, although cultures of the organisms may not produce fruitful results. Cultures are often contaminated by other commensal flora and require strict anaerobic conditions for up to 14 days. Studies have shown a low sensitivity of cultures for the identification of cervicofacial actinomycosis, ranging between 20% and 50%.8 9 Histological evaluation of the lesions reveals non-specific suppurative inflammation, central necrosis and bacterial aggregates arranged in tangles, often with acute angle branching. The draining sinus tracts can be multiple and express yellow exudate with characteristic sulfur granules. These sulfur granules are not specific to Actinomyces spp and they can be seen in other infections including nocardiosis. AFB stains are useful in distinguishing AFB-negative Actinomyces from AFB-positive nocardia.
In our case, the patient did not present with a history completely consistent with classical cervicofacial actinomycosis. The patient denied a recent history of trauma and was not immunosuppressed, however, he did present with a slowly progressive neck pain. The ulcer at the posterior oropharynx may suggest a site of mucosal disruption and point of invasion for the bacteria. Although the infection extended to the cervical vertebrae, the patient was fortunate there was no cord involvement. Finally, cultures of the lesion did not provide evidence for the diagnosis, but histological examination of the tissue proved to be most useful. Histological evaluation is encouraged in cases suspicious for cervicofacial actinomycosis; since the radiological differentials may include neoplasia; microbiology may be non-diagnostic and prompt antibiotic treatment is lifesaving.
Learning points.
Actinomyces spp are Gram-positive, rod-shaped, anaerobic to microaerophilic, non-spore forming bacteria that are natural members of the oral cavity flora.
Cervicofacial actinomycosis is associated with poor oral hygiene, dental procedures and oral trauma, most commonly caused by A. israelii and the most commonly involved site is the angle of the jaw.
Radiographic evidence concerning for an infectious process of the spine includes involvement of the adjacent disk space causing a loss of disk height, while neoplasms tend to preserve disk space.
Histopathological findings of Actinomyces spp include filamentous organisms, highlighted by Gomori methenamine silver stain and are acid-fast bacilli negative, with suppurative inflammation and necrosis; while sulfur granules may be present, they are non-specific.
Footnotes
Twitter: Follow Shyam Prajapati at @shyam_DO
Contributors: SP wrote the initial draft of the case report under the guidance of his attending AB. While DJY contributed to the radiology related text and figures under the guidance of his attending CLB. The authors contributed to drafting and finalising the content and approved the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck 1999;21:264–8. [DOI] [PubMed] [Google Scholar]
- 2.Tortorici S, Burruano F, Buzzanca ML et al. . Cervico-facial actinomycosis: epidemiological and clinical comments. Am J Infect Dis 2008;4:204–8. 10.3844/ajidsp.2008.204.208 [DOI] [Google Scholar]
- 3.Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period: a diagnostic ‘failure’ with good prognosis after treatment. Arch Intern Med 1975;135:1562–8. 10.1001/archinte.1975.00330120040006 [DOI] [PubMed] [Google Scholar]
- 4.Bennett JE, Dolin R, Blaser MJ. Principles and practice of infectious diseases. Elsevier Health Sciences, 2014. [Google Scholar]
- 5.Benzel EC. Cervical actinomycosis causing spinal cord compression and multisegmental root failure: case report and review of the literature. Neurosurgery 1998;43:940 10.1097/00006123-199810000-00120 [DOI] [PubMed] [Google Scholar]
- 6.Hung PC, Wang HS, Chiu CH et al. . Cervical spinal cord compression in a child with cervicofacial actinomycosis. Brain Dev 2014;36:634–6. 10.1016/j.braindev.2013.08.002 [DOI] [PubMed] [Google Scholar]
- 7.Hong SH, Choi JY, Lee JW et al. . MR imaging assessment of the spine: infection or an imitation? Radiographics 2009;29:599–612. 10.1148/rg.292085137 [DOI] [PubMed] [Google Scholar]
- 8.Heo SH, Shin SS, Kim JW et al. . Imaging of actinomycosis in various organs: a comprehensive review. Radiographics 2014;34:19–33. 10.1148/rg.341135077 [DOI] [PubMed] [Google Scholar]
- 9.Muzio LL, Favia G, Lacaita M et al. . The contribution of histopathological examination to the diagnosis of cervico-facial actinomycosis: a retrospective analysis of 68 cases. Eur J Clin Microbiol Infect Dis 2014;33:1915–18. 10.1007/s10096-014-2165-0 [DOI] [PubMed] [Google Scholar]