Abstract
Background:
Challenges exist in the diagnosis, management and follow-up of patients with chronic obstructive pulmonary disease (COPD) in India. Lack of awareness of the disease, its symptoms and its implications may significantly contribute in preventing individuals with symptoms from seeking advice from their primary care physicians or eliminating risk factors. This cross-sectional survey aimed to explore the attitudes, beliefs, and knowledge of doctors (general practitioners [GPs], physicians and pulmonologists) related to COPD recognition, diagnosis, and treatment in India.
Methods:
Data was collated from 91 randomly selected GPs, physicians and pulmonologists through a questionnaire and face-to-face interviews, in 8 cities of India.
Results:
The response rate to the survey was 68% (61 out of 91). Majority of the doctors (90% of GPs-physicians and 82% of pulmonologists) reported that patients with COPD visit them at moderate to severe stages of the disease. 44% of the GPs and physicians reported that they had never performed spirometry to make a diagnosis of COPD. About 35% of doctors reported that COPD occurred only in smokers. The most common reported barriers to the treatment of COPD were difficulty in explaining COPD to the patients, poor patient compliance to the prescribed treatment and the inability of patients to give up smoking. Most doctors agreed that compliance with treatment is a major concern in patients with COPD due to an ageing population, existence of limited therapeutic options and presence of comorbidities.
Conclusion:
The results of this cross-sectional survey of doctors in India, highlighted the need for increasing the awareness about COPD at both doctor and patients level to overcome the prevalent under-diagnosis and under-treatment in COPD.
Keywords: Chronic obstructive pulmonary disease treatment, diagnosis, general practitioners, management, pulmonologists, spirometry
INTRODUCTION
Crude estimates suggest there are 30 million patients with chronic obstructive pulmonary disease (COPD) in India.[1] India contributes a significant and growing percentage to COPD mortality worldwide, and this is estimated to be among the highest in the world.[2] The prevalence of COPD is increasing but it remains under-diagnosed and under-treated. Diagnosis of COPD usually does not occur until significant lung function has already been lost.[2] By the time patients recognize that their symptoms are getting troublesome, they usually have reached a level where lung function is considerably reduced and there is a significant amount of systemic inflammation leading to co-morbidities.[2] Early detection of airflow limitation and early intervention can delay lung function decline, reduce the burden of COPD symptoms, and improve patients' quality of life.[3] Hence, it is important to identify the existing barriers to an early and correct diagnosis and treatment of COPD.
This face-to-face questionnaire-based survey of general practitioners (GPs), physicians and pulmonologists in various cities of India aimed at understanding issues associated with COPD management at various specialty levels. The survey aimed to explore the attitudes, beliefs, and knowledge of doctors related to COPD recognition, diagnosis, and treatment. We present the results of the doctors' understanding levels of COPD pathology, etiology, diagnosis and treatment options and ability to differentiate COPD from asthma.
METHODOLOGY
Study design and participants
The present cross-sectional study was conducted in February, 2014. Participant doctors were required to complete a structured questionnaire (practice assessment) related to COPD. They did not receive any financial compensation for their involvement in the present study. The questionnaires were developed by the study authors. The questionnaires consisted of 30 questions for GPs and physicians and 33 questions for pulmonologists. The study was conducted at individual doctor clinics across the country. The target recruitment population was GPs, physicians, and pulmonologists regionally distributed (North: Delhi, Amritsar, Jalandhar; East: Calcutta; West: Mumbai, Pune; South: Chennai, Coimbatore) across India.
Questionnaire details
Doctors who consented to participate completed a one-time paper questionnaire. The questionnaire was designed to collect data on the doctor's practice profile (e.g., type of practice, year of qualification and COPD patients percentage), characteristics of their COPD patients and physician perceptions of issues relevant to COPD (e.g., doctors attitudes towards COPD, the symptomatology and comorbidities in patients with COPD they treat, the diagnostic tests performed to diagnose COPD, doctors' attitude towards COPD treatment, inhaler device choice, patient compliance, communication with COPD patients, treatment failure reasons/barriers and patient inhaler device technique).
To understand the prescription patterns of doctors in COPD management, they were asked to fill a grid about the inhaled medications they were currently prescribing and; their intent to prescribe the medication in the future vis-à-vis the current status (increase, decrease, or same). This gave us the net percent prescribing intention of doctors in the future. Additional details of the questionnaires can be found in appendix A.
RESULTS
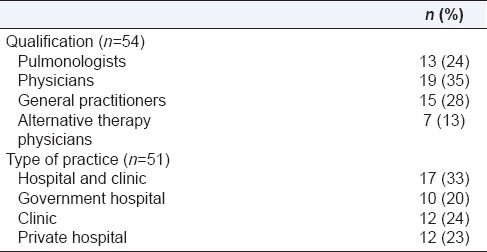
The overall response rate to the questionnaire survey was 68% (61 out of 91). The total number of useable surveys was 54 (59.34% overall). The doctors' demogrics are given in Table 1.
Table 1.
Physician demographics
Ratio of asthma: Chronic obstructive pulmonary disease patients
Sixty-seven percent of the total doctors reported that 60–70% of their respiratory patients were asthma patients.
Sixty-eight percent GPs and physicians reported that 60–70% of their respiratory patients were asthma patients. About 50% pulmonologists reported that asthma patients were only about 50% of their respiratory patients.
Ratio of smokers: Nonsmokers in chronic obstructive pulmonary disease patients
Sixty-nine percent of GPs and physicians reported that the majority of their COPD patients were smokers whereas 34% pulmonologists reported that only <10% of their COPD patients were smokers.
Ratio of males: Females in chronic obstructive pulmonary disease patients
Seventy percent of doctors reported that 70–100% of their COPD patients were males. This percentage is 78% for GPs and physicians and 55% for pulmonologists.
Doctor's attitude toward chronic obstructive pulmonary disease
This survey aimed to understand the knowledge of GPs and physicians (pulmonologists were excluded from this) about basic facts relating to COPD. 35% physicians believed that COPD was a disease only of smokers.
Symptomatology
The most commonly reported early symptoms of COPD were increased amount of sputum (by 19% GPs and physicians and 21% pulmonologists), shortness of breath during activity (by 31% GPs and physicians and 32% pulmonologists) and chronic coughing (by 36% GPs and physicians and 29% pulmonologists). Wheezing (by 6% GPs and physicians and 11% pulmonologists) and tightness in the chest (by 5% GPs and physicians and 7% pulmonologists), important symptoms in COPD patients, were noticed by GPs and physicians less frequently than by pulmonologists.
Comorbidities
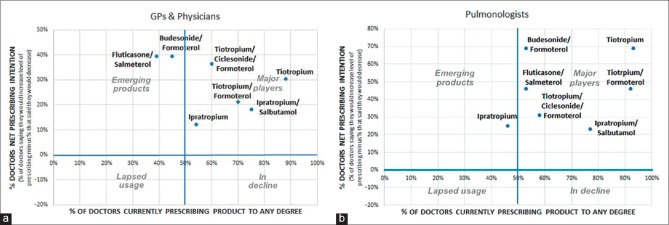
Most commonly reported cardiovascular comorbid conditions were congestive heart failure (26%) and hypertension (13%) per GPs and physicians and congestive heart failure (30%) and myocardial infarction (22%) per pulmonologists [Figure 1]. Most commonly reported noncardiovascular comorbid conditions were depression (26%), anxiety (20%) and gastro-esophageal reflux disease (19%) per GPs and physicians; and depression (27%), osteoporosis (23%) and anxiety (19%) per pulmonologists. Majority of GP's and physicians did not evaluate for comorbid conditions and pulmonologists refer patients with comorbidities to the concerned specialists.
Figure 1.
Physician reported cardiovascular concomitant conditions seen in chronic obstructive pulmonary disease patients
Stage at which chronic obstructive pulmonary disease patients first visit the doctor
The majority of the doctor's reported that the COPD patients visit them directly for COPD related symptoms, at later stages of the disease with moderate and severe severity. 38% of pulmonologists and 45% of GPs and physicians reported that COPD patients were in moderate stage of the disease whereas, 44% pulmonologists and 45% GPs and physicians reported that COPD patients were already in severe stages when they first approached them.
Chronic obstructive pulmonary disease diagnosis
Diagnostic tests performed
Forty-four percent of the GPs and physicians did not perform spirometry to make a diagnosis of COPD. All pulmonologists interviewed in the survey used spirometry to diagnose COPD. Chest X-ray was reported to be the most widely used tool to exclude other lung disorders.
Majority of pulmonologists reported that they had their own spirometry facilities (65%) or at government hospitals spirometry clinics (12%) (in case of government-hospital doctors) while GPs and physicians rely on private diagnostic laboratories (27%) and camps (20%) for getting spirometry done. Those doctors who had their own spirometers reported that it was a cost-efficient diagnostic tool.
Challenges faced in diagnosing chronic obstructive pulmonary disease
The most commonly listed challenge experienced by pulmonologists in diagnosing COPD was the resistance by patients for getting spirometry done (61%). About one in four GPs and physicians admitted to inadequate knowledge and training about the diagnosis of COPD. Other perceived barriers for the diagnosis of COPD that came up during the interview included lack of clear symptoms as well as the impact of multiple chronic conditions in patients with COPD.
Management of chronic obstructive pulmonary disease
Symptom relief and reduction in frequency of exacerbations were the most important drug-choice drivers for the doctors [Figure 2]. It was reported that pulmonologists emphasized on reducing exacerbations whereas GPs and physicians were more focused at immediate symptom relief. Pulmonologists tended to comply with the recommended treatment guidelines.
Figure 2.
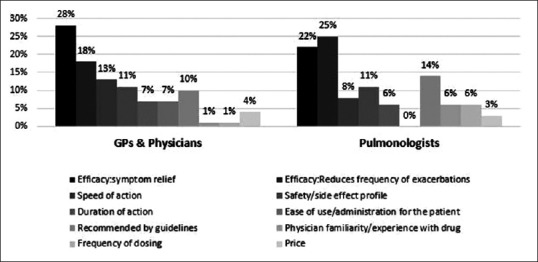
Most important drug-choice drivers for doctors
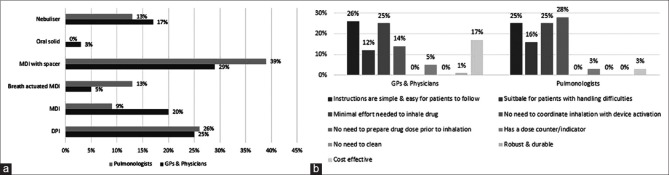
Current and future prescribing trends of inhaled medications
Figure 3a and b explain the current and future prescribing trends for GPs and physicians; and pulmonologists for inhaled medications currently available in India. For example, in Figure 3a and b, it can be seen that a triple combination of long-acting beta-2 agonists (LABA)/inhaled corticosteroids (ICS)/long acting muscarinic antagonists (LAMA) was currently prescribed by 60% GPs and physicians and by 58% pulmonologists; and a net increase of 38% and 32%, respectively, was reported by these doctors for the future prescribing intentions for LABA/ICS/LAMA combination. Similarly, 75% GPs and physicians and 78% pulmonologists were currently prescribing the fixed dose combination of ipratropium and salbutamol and a net increase of 28% and 22%, respectively is expected in its future prescription.
Figure 3.
(a) Current and future prescribing trends for general practitioners and physicians for inhaled medications currently available in India (b) Current and future prescribing trends for pulmonologists for inhaled medications currently available in India
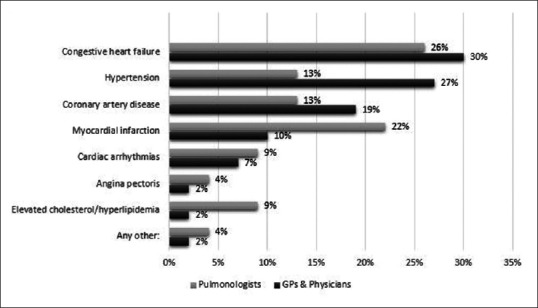
Device choice
Pressurized metered dose inhaler (pMDI) with a spacer was the most commonly used device for COPD patients, followed by dry powder inhalers (DPIs) [Figure 4a]. Most important device choice drivers were simple and easy instructions to use and requirement of minimal effort to inhale the drug [Figure 4b]. Pulmonologists give high importance to the difficulty faced by patients in coordination between inhalation and device actuation while the cost of the device is an important factor for GPs and physicians, especially since most of the patients in India pay out-of-pocket. More than 50% of the doctors agreed that COPD patients struggle with inhaler devices more so than asthma patients.
Figure 4.
(a) Device preferred by doctors for chronic obstructive pulmonary disease patients (b) Most important device-choice drivers for doctors
Doctors' attitude towards patient compliance in chronic obstructive pulmonary disease
Most doctors agreed that compliance with treatment is a major concern in case of COPD patients due to the ageing COPD population and existence of multiple comorbidities and, therefore, multiple therapies. Pulmonologists (54%) face less compliance issues with their patients than do GPs and physicians (78%).
Communication with chronic obstructive pulmonary disease patients
The terms-smokers' asthma (by 36% of GPs and physicians and 31% of pulmonologists) and chronic bronchitis (by 38% GPs and physicians and 8% pulmonologists), were used by doctors to explain COPD to their patients. Pulmonologists were of the opinion that the term COPD itself should be used and explained to the patients.
Barriers to chronic obstructive pulmonary disease treatment
Twenty-three percent GPs and physicians; and 30% pulmonologists reported that the difficulty in explaining COPD to patients was a common barrier to the treatment of COPD. Poor patient compliance to treatment was reported by 28% GPs and physicians; and 25% pulmonologists. The other barriers perceived by the treating doctors were the inability of patients to give up smoking and resistance to inhaler usage.
DISCUSSION
The prevalence and incidence of COPD is a growing concern globally. India contributes a significant percentage to COPD mortality worldwide.[4] In India, 30% of out-patients seen in chest clinics and up to 5% of hospital admissions are those of COPD. It is estimated that in India, a patient of COPD spends about 30% of his income on the treatment.[5] The Rural Household Survey and Death Certification (1998), estimated over 0.57 million deaths due to COPD. Despite these figures, the awareness about COPD as a disease in India is low.[6] There is also little-published evidence to assess the awareness, perception and attitude towards COPD at both the patient level and the doctor level.
This study reported that in spite of the growing health problem of COPD, there is inadequate awareness at the level of GPs and physicians toward COPD. Pulmonologists understand the disease better but are limited by the patients' attitude toward the disease and its management. The strongest issues that stand-out in this cross-sectional survey of doctors in India about COPD include diagnosis of the disease only in later stages of the disease with patients resistant to see their doctors early-on; limited availability and access to spirometry in India, the stigma associated with use of inhalers and the noncompliance of patients toward the treatment.
Majority of the respondent doctors reported seeing and treating more asthma cases than those of COPD-this implies that despite a high prevalence, COPD patients in India are either not approaching the doctors or not being diagnosed properly. Doctors were seen to have a bias, that females would have asthma and not COPD, and thus missing the proper diagnosis in many female patients with COPD.[7] COPD, surprisingly, is still seen primarily as a smoker's disease. In contrast to the pulmonologists, majority of the GPs and physicians reported that majority of their COPD patients were smokers and this indicates that GPs and physicians, who diagnose COPD based on history and clinical symptoms alone, fail to make a diagnosis of COPD in the absence of smoking history – thus missing out cases of COPD due to biomass exposure and other causes.[8] This will prevent from cases of COPD going undiagnosed. In a survey in Asian cities, it was concluded that the history of exposure to biomass fuels or dusty jobs related to the frequency of symptoms, severe airflow limitation, and poor quality of life.[9] Hence, more emphasis needs to be made on nonsmoking COPD[7,9] and COPD in females.[8]
Early detection of airflow limitation and early intervention can delay the decline in lung function, characteristic of COPD. Early management can additionally, reduce the burden of COPD symptoms and improve the quality of life in patients.[3] In this survey, it was seen that many patients approached the doctors at moderate to severe stages, indicating a deficit in awareness of COPD at the population level. As a consequence, the diagnosis of COPD usually does not occur until significant lung function has already been lost and patients have reached a level where there is a significant level of systemic involvement including presence of multiple comorbidities.[10] The cardiovascular (congestive heart failure, hypertension, myocardial infarction) and noncardiovascular comorbid conditions (depression, anxiety, gastro-esophageal reflux disease, osteoporosis) seen were consistent between the GPs and physicians and pulmonologists and comparable to that published in literature.[11,12]
According to the doctors, patient awareness about the disease and hence the need to seek a pulmonologist consultation is low. Early detection of COPD by spirometry is likely to reduce the overall burden of disease.[13] In India, many of the doctors diagnose COPD on the basis of clinical symptoms due to nonavailability of spirometry, unreliable spirometry reports, and high costs of spirometry. In most cases, COPD is being diagnosed by clinical symptoms and exclusion in India. There is a lack of consistently performed spirometry and spirometry training in primary care in India. These results highlight the need to create awareness about spirometry for COPD diagnosis at both the patient level and the doctor level in India.
Another hurdle faced by doctors in the management of COPD is that patients do not quit smoking rendering the treatment ineffective. To worsen the situation, there are time pressures on doctors that impact adversely on their ability to counsel and manage patients effectively for smoking cessation. Pulmonary rehabilitation is virtually nonexistent in India. The authors recommend the establishment of smoking cessation and pulmonary rehabilitation clinics managed by qualified paramedics with the supervision of pulmonologists. Guidelines for the management of COPD based on the global initiative for chronic obstructive lung disease are available for different levels of health care in India.[14,15] A guideline-directed strategy is adopted generally only by pulmonologists, and not by GPs and physicians.
Most pulmonologists and physicians preferred the pMDI device with a spacer or a DPI for their patients with COPD and most agreed that the availability of a low-cost breath-actuated pMDI would be their most preferred device option. Effective inhalation therapy depends on patient, device, drug and environment factors.[16] Therefore, it is important that the doctors treating patients with COPD are familiar with the characteristics of the available inhalation devices, the attitudes and preference of patients to eventually be able to improve clinical outcomes.[16] It is imperative that healthcare professionals select the best available device to meet each patient's needs, modify the selection of device based on the abilities, needs and preferences of the patient and additionally, spend adequate time in training and re-training of the inhalation device at every use.
The results of this cross-sectional survey of doctors in India, highlight the lack of awareness about COPD, its symptoms, and its implications contribute significantly in preventing people at risk from reaching out to their doctors. Inadequate use of access to spirometry and the belief that COPD is a smoker's disease are the most important barriers to diagnosis. This survey brings out the need for a large-scale study to understand the patient perceptions and to plan and implement educational and awareness programs for both doctors and patients with the aim to spread awareness about COPD, under-diagnosis and under-treatment associated with COPD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors are thankful to all the doctors for filling the questionnaire and the field staff of Cipla Ltd. for distributing and assembling the completed questionnaires. The authors are also appreciative of Dr Vaibhav Gaur, Global Medical Affairs, Cipla Ltd. for critically reviewing the manuscript. This study was supported by Cipla Ltd, India.
REFERENCES
- 1.Salvi SS, Manap R, Beasley R. Understanding the true burden of COPD: The epidemiological challenges. Prim Care Respir J. 2012;21:249–51. doi: 10.4104/pcrj.2012.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jindal SK. COPD: The unrecognized epidemic in India. J Assoc Physicians India. 2012;60(Suppl):14–6. [PubMed] [Google Scholar]
- 3.Price D, Freeman D, Cleland J, Kaplan A, Cerasoli F. Earlier diagnosis and earlier treatment of COPD in primary care. Prim Care Respir J. 2011;20:15–22. doi: 10.4104/pcrj.2010.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jindal SK, Aggarwal AN, Gupta D. A review of population studies from India to estimate national burden of chronic obstructive pulmonary disease and its association with smoking. Indian J Chest Dis Allied Sci. 2001;43:139–47. [PubMed] [Google Scholar]
- 5.Thiruvengadam KV, Sekar TS, Rajagopal KR. Study of chronic bronchitis in Tamilnadu. Indian J Chest Dis. 1974;16:1–10. [PubMed] [Google Scholar]
- 6.Nongkynrih B, Patro BK, Pandav CS. Current status of communicable and non-communicable diseases in India. J Assoc Physicians India. 2004;52:118–23. [PubMed] [Google Scholar]
- 7.Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374:733–43. doi: 10.1016/S0140-6736(09)61303-9. [DOI] [PubMed] [Google Scholar]
- 8.Ozbay B, Uzun K, Arslan H, Zehir I. Functional and radiological impairment in women highly exposed to indoor biomass fuels. Respirology. 2001;6:255–8. doi: 10.1046/j.1440-1843.2001.00339.x. [DOI] [PubMed] [Google Scholar]
- 9.Oh YM, Bhome AB, Boonsawat W, Gunasekera KD, Madegedara D, Idolor L, et al. Characteristics of stable chronic obstructive pulmonary disease patients in the pulmonology clinics of seven Asian cities. Int J Chron Obstruct Pulmon Dis. 2013;8:31–9. doi: 10.2147/copd.s36283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mapel DW, Dalal AA, Blanchette CM, Petersen H, Ferguson GT. Severity of COPD at initial spirometry-confirmed diagnosis: Data from medical charts and administrative claims. Int J Chron Obstruct Pulmon Dis. 2011;6:573–81. doi: 10.2147/COPD.S16975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sin DD, Man JP, Man SF. The risk of osteoporosis in Caucasian men and women with obstructive airways disease. Am J Med. 2003;114:10–4. doi: 10.1016/s0002-9343(02)01297-4. [DOI] [PubMed] [Google Scholar]
- 12.Feary JR, Rodrigues LC, Smith CJ, Hubbard RB, Gibson JE. Prevalence of major comorbidities in subjects with COPD and incidence of myocardial infarction and stroke: A comprehensive analysis using data from primary care. Thorax. 2010;65:956–62. doi: 10.1136/thx.2009.128082. [DOI] [PubMed] [Google Scholar]
- 13.Barthwal MS, Singh S. Early detection of chronic obstructive pulmonary disease in asymptomatic smokers using spirometry. J Assoc Physicians India. 2014;62:238–42. [PubMed] [Google Scholar]
- 14.Global Initiative for Chronic Obstructive Lung Disease. NHLMI/WHO Workshop Report. Bethesda: National Heart, Lung and Blood Institute, NIH Publication No. 2701; 2001. Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for Diagnosis, Management and Prevention of COLD; pp. 1–100. [Google Scholar]
- 15.Guidelines for Management of Chronic Obstructive Pulmonary Disease (COPD) in India. [Last accessed on 2015 Mar 01]. Available from: http://www.whoindia.org/noncommunicablediseases/respiratorydisease .
- 16.Lavorini F, Fontana GA, Usmani OS. New inhaler devices – The good, the bad and the ugly. Respiration. 2014;88:3–15. doi: 10.1159/000363390. [DOI] [PubMed] [Google Scholar]