Abstract
Background
Maternal death reviews and obstetric audits identify causes and circumstances related to occurrence of a maternal death or serious complication and inform improvements in quality of care. Given Nigeria’s high maternal mortality, the lessons learned from past experiences can provide a good evidence base for informed decision making. We aimed to synthesise findings from maternal death reviews and other obstetric audits conducted in Nigeria through a systematic review, seeking to identify common barriers and enabling factors related to the provision of emergency obstetric care.
Methods
We searched for maternal death reviews and obstetric care audits reported in the published literature from 2000–2014. A ‘best-fit’ framework approach was used to extract data using a structured data extraction form. The articles that met the inclusion criteria were assessed using a nine point quality score.
Results
Of the 1,841 abstracts and titles at initial screening, 329 full text articles were reviewed and 43 papers fulfilled the inclusion criteria. Four types of barriers were reported related to: transport and referral; health workers; availability of services; and organisational factors. Three elements stand out in Nigeria as contributing to maternal mortality: delays in Caesarean section, unavailability of magnesium sulphate and lack of safe blood transfusion services.
Conclusions
Obstetric care reviews and audits are useful activities to undertake and should be promoted by improving the processes used to conduct them, as well as extending their implementation to rural and basic level health facilities and to the community. Urgent areas for quality improvement in obstetric care, even in tertiary and teaching hospitals should focus on organisational factors to reduce delays in conducting Caesarean section and making blood and magnesium sulphate available for all who need these interventions.
Keywords: Maternal mortality, Maternal death reviews, Audit, Surveillance and response, Quality improvement, Emergency obstetric care
Background
Maternal death reviews and obstetric audits are quality improvement investigations which support the identification and analysis of causes and circumstances related to occurrence of maternal deaths or serious complications. They have been conducted for many years in various settings, although there have been recent efforts to promote their implementation, especially in low and middle income countries [1, 2]. Recently, the World Health Organization produced a guideline for conducting maternal death surveillance and response (MDSR), which builds on maternal death reviews and emphasises the continuous action cycle and ongoing monitoring necessary to link the health information system with quality improvement processes [3]. From a public services perspective, audit can be seen as a social process, which allows checking and verification, providing evidence to reduce problem areas [4, 5].
As a consequence of the size of its population, Nigeria is the African country with the highest contribution to maternal deaths, making up 14 % of the 289,000 annual global maternal deaths [6]. Although maternal mortality has fallen from 800 deaths per 100,000 live births in 2003 to 545 deaths per 100,000 live births in 2008 [7], the most recent estimates show that progress is slow. The maternal mortality in 2013 was 576, compared to a previous estimate in 2008 of 545 deaths per 100,000 live births [8]. At policy level, there is clear commitment in Nigeria to improve maternal health and reduce maternal mortality, with various national initiatives being implemented at national and state levels such as health insurance programmes, community health worker development and improvements in midwifery services [6, 9–12].
Rational and effective use of reliable, routinely collected data will result in better information for planning and action as well as generate an accountable and responsive health service. Conducting maternal death reviews and other types of obstetric audit are a way to achieve this pathway to change. The audits and reviews assess clinical practices to report health outcomes, highlight deficiencies in service provision, provide recommendations for improvements in care and are an established means to improve the quality of maternity care [1, 13–15] In recognition of these attributes, in 2013 the Ministry of Health in Nigeria, Society of Gynaecology and Obstetrics of Nigeria (SOGON) and International Federation of Gynaecology and Obstetrics (FIGO) embarked on a process to commence a national maternal death review programme [16]. Yet Nigeria already has a long history of conducting maternal death reviews and obstetric audit. Most have been conducted independently in individual hospitals, rather than as part of a structured programme. There have been no attempts to collectively summarise past experiences [17] which may strengthen the evidence base for decision-making beyond that of individualised efforts. In contribution to the efforts of SOGON and the Ministry of Health in Nigeria, we set out to synthesise the findings of previous maternal death reviews and other obstetric audits through a systematic review. Specifically, we sought to capture commonly encountered barriers and to identify enabling factors related to the provision of emergency obstetric care.
Methods
Eligibility criteria
A systematic search of the published literature was conducted using a pre-defined protocol. We used a broad definition of ‘audit’ and ‘reviews’ [13] to include studies and surveys which used clinical case records, organisation of clinical meetings or interviews to report on obstetric health care in Nigeria. For the sake or brevity, we will use the term ‘audit’ in the remainder of this paper. Studies using either numerical or qualitative data, or both, to record parameters associated with care provision were included. The population of interest were women who experienced any emergency obstetric complication which was life-threatening for the women themselves (including death), required emergency surgery as a consequence of the complications, or was life threatening for their babies. Studies could be undertaken at community, healthcare facility, or at district, regional or national level. The primary outcomes of interest were circumstances surrounding maternal deaths and complications after women sought care, including referral and transport; descriptions of clinical practice, treatment or management of women experiencing maternal mortality or complications; and descriptions of health professional performance or practice in a healthcare setting in relation to women during pregnancy and childbirth.
Studies with the following characteristics were excluded: documentation of causes or proportions of maternal deaths without descriptions of care practices or management; reports focusing exclusively on routine care (e.g., antenatal care, partogram use) with no obstetric complications; sole focus on socio-demographic risk factors (e.g., age, parity) and those that evaluated only knowledge, attitudes or satisfaction of pregnant women, their families or healthcare providers. Management of non-emergency conditions such as chronic obstetric fistula, congenital malformations or those requiring elective surgery and other procedures are excluded. Studies not located in Nigeria, even if they involved women from Nigeria, were excluded.
Search methods
Medline; Embase; CINAHL; Web of Knowledge and African Journal Online were searched in December 2013 and January 2014 using terms related to maternal and perinatal mortality and complications; setting (Nigeria) and study design (audit/confidential enquiry/review/survey). We restricted our search to studies published during or after the year 2000 because we were interested in contemporary practices and because Nigeria has seen considerable effort put into national strategies and interventions since 2000 [11]. Studies published after the year 2000, but which included data prior to the year 2000 were not included unless there was a means of separating the post-2000 data from previous years. There were no language restrictions imposed on the searches. Bibliographic references from the included studies were reviewed to identify additional studies.
Data collection and analysis
All titles, abstracts and full-text articles were reviewed by at least one reviewer and a sample checked by another reviewer. Disagreements were resolved by discussion. Data was extracted from included studies by one reviewer and checked by a second reviewer.
Data was synthesised based on a ‘best-fit’ framework approach [18, 19] as follows. A structured data extraction form, which reflected a pre-set thematic framework was used to extract data. The framework originated from the South African Confidential Enquiry format. Its structure was made up of categories related to patient factors, the clinical management of emergency complications health system factors such as transport, referral, health personnel and their training, the availability of services and organisational/administrative factors such as record keeping and policy or planning factors [20, 21]. Patient factors were analysed separately and reported elsewhere.
The focus of the review was to identify barriers and enabling factors reported in maternal death audits of obstetric emergencies.
Quality assessment
The articles that met the inclusion criteria were assessed using a nine point score adapted from others [1, 22]. A score of 0 or 1 was given for each study characteristic as follows: description of study population, explanation of sampling strategy, consideration of missing cases, pretesting or piloting of study instruments, use of a standard data collection form, description of data collectors, training, quality checks for data entry and assessment of inter-observer/inter-site variability. Two reviewers conducted the quality assessment independently, their assessments were compared and disagreements resolved by discussion.
Results
From the 1,841 relevant abstracts and titles found, 329 full text articles were retrieved (Fig. 1). All were in English. Of these, 43 papers fulfilled the inclusion criteria [23–65]. Two papers used the same data but analysed the findings from different viewpoints, so we merged these two papers as one [27, 28].
Fig 1.
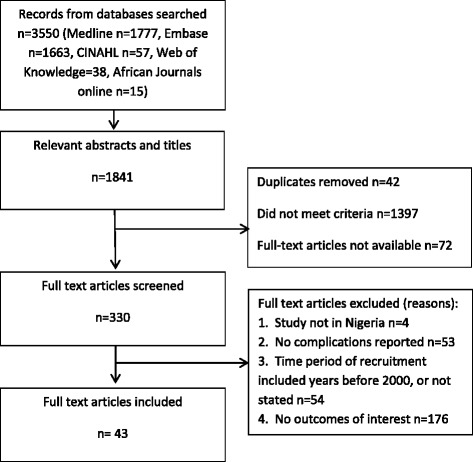
Search Results. Flow chart of search, screening, included papers and reasons for exclusion
The included papers and their characteristics are summarised in Table 1, categorised according to the complication or obstetric outcome of interest. The largest number of studies included were of eclampsia/pre-eclampsia and Caesarean sections. All studies were hospital based and the six geopolitical zones of Nigeria were represented in the included papers. The purpose of most of the studies were to ascertain or compare obstetric outcomes or practices and to provide recommendations for improved care. Studies made comparisons between cases and controls [30], hospitals [53], procedures [58], across time periods [27] or against rates of complications reported in other studies [35, 38, 47, 61]. A few conducted audits against pre-specified criteria or standard treatment protocols [27–30]. All but two studies [30, 53] were conducted in a single hospital. Two-thirds of the studies collected data retrospectively over a period of between one to ten years. Prospective studies were fewer in number and covered shorter periods of time from one to three years. Apart from using clinical case notes and other types of hospital case records (such as labour ward registers or admission books) as data sources, some studies used interviews and observation as an alternative [26, 32, 53]. A few papers did not fully describe the means of data collection [49, 54, 60], although the type of data reported suggested that case records were used. Quality scores ranged from 2–7 from a maximum of 9 points (Table 1).
Table 1.
Study characteristics
| Author, year | State/zone | Recruitment years | Setting | Study methods | Numbers of cases included | Numbers of maternal deaths reported | Quality score |
|---|---|---|---|---|---|---|---|
| Maternal deaths | |||||||
| Ande 2012 [23] | Benin, SS | 2005–2009 | 1 teaching hospital | Retrospective case record review | 184 | 184 | 2 |
| Ezugwu 2009 [24] | Enugu, SE | 2004–2008 | 1 teaching hospital | Retrospective case record review | 54 | 54 | 2 |
| Ozumba 2008 [25] | Enugu, SE | 2003–2005 | 1 teaching hospital | Case record review | 47 | 47 | 4 |
| Omo-Aghoja 2010 [26] | Benin, SS | 2005–2007 | 1 teaching hospital | Retrospective case record review, inspection of maternity unit and interview of healthcare providers | 84 | 84 | 4 |
| Near miss | |||||||
| Oladapo 2005 [27], Oladapo 2007 [28](same data for both papers) | Sagamu, SW | 2002–2004 | 1 teaching hospital | Retrospective case record review, clinical review panel | 255 | 44 | 3 |
| Hunyinbo 2008 [29] | Abeokuta, SW | 2002–2003 | 1 teaching hospital | Case record review | 130 | 4 | 4 |
| Adeoye 2013 [30] | Ile Ife, SW | 2006–2007 | 2 teaching hospitals | Prospective case record review | 75 | nr | 7 |
| Olagbuji 2012 [31] | Benin, SS | 2007–2010 | 1 teaching hospital | Retrospective case record review | 263 | 34 | 2 |
| Stillbirths | |||||||
| Ezugwu 2011 [32] | Enugu, SE | 2009 | 1 teaching hospital | Prospective case record review and interview of mothers | 153 | nr | 3 |
| Olusanya 2009 [33] | Lagos, SW | 2005–2007 | 1 teaching hospital | Case record review | 602 | nr | 2 |
| Abortion complications | |||||||
| Ibrahim 2012 [34] | Niger Delta, SS | 2007–2010 | 1 teaching hospital | Retrospective case record review | 63 | 3 | 2 |
| Raibu 2009 [35] | Lagos, SW | 2005–2007 | 1 tertiary hospital | Prospective case record review | 175 | nr | 3 |
| Nwogu-Ikijo 2007 [36] | Enugu, SE | 2000–2005 | 1 teaching hospital | Retrospective case record review | 11 | 11 | 2 |
| Ekanem 2009 [37] | Calabar, SS | 2003–2004 | 1 teaching hospital | Prospective case record review | 126 | 5 | 3 |
| Eclampsia/pre-eclampsia | |||||||
| Adinma 2013 [38] | Nnewi, SE | 2000–2009 | 1 teaching hospital | Retrospective case record review | 46 | 8 | 2 |
| Eke 2011 [39] | Anambra, SE | 2004–2009 | 1 tertiary hospital | Case record review | 212 | nr | 2 |
| Agida 2010 [40] | Abuja, NC | 2005–2008 | 1 teaching hospital | Retrospective case record review | 46 | 5 | 2 |
| Kulima 2009 [41] | Nguru, NE | 2003–2007 | 1 tertiary hospital | Retrospective case record review | 224 | 52 | 2 |
| Okafor 2008 [42] | Abuja, NC | 2001–2005 | 1 tertiary hospital | Retrospective case record review | 38 | 11 | 3 |
| Makinde 2009 [43] | Ile Ife, SW | 2006 | 1 teaching hospital | Prospective case record review | 34 | 4 | 2 |
| Uterine rupture | |||||||
| Nyengidiki 2011 [44] | Niger delta, SS | 2004–2007 | 1 teaching hospital | Retrospective case record review | 40 | 7 | 2 |
| Esiki 2011 [45] | Ebonyi, SE | 2000–2009 | 1 teaching hospital | Retrospective case record review | 101 | 12 | 3 |
| Osaikhuwuomwan 2011 [46] | Niger delta, SS | 2003–2007 | 1 teaching hospital | Retrospective case record review | 33 | 2 | 2 |
| Okafor 2006 [47] | Enugu, SE | 2000–2004 | 1 teaching hospital | Retrospective case record review | 23 | 1 | 2 |
| Mbamara 2012 [48] | Nnewi, SE | 2004–2009 | 1 teaching hospital | Retrospective case record review | 25 | 3 | 3 |
| Caesarean section | |||||||
| Onankpa 2009 [49] | Sokoto, NW | 2006–2007 | 1 teaching hospital | Prospective, unclear data source | 216 | nr | 3 |
| Ekanem 2008 [50] | Calabar, SS | 2000–2001 | 1 teaching hospital | Retrospective case record review | 349 | 12 | 2 |
| Ozumba 2006 [51] | Enugu, SE | 2000–2002 | 1 teaching hospital | Retrospective case record review | 463 | nr | 2 |
| Ojiyi 2012 [52] | Orlu, SE | 2004–2008 | 1 teaching hospital | Retrospective case record review | 358 | 3 | 2 |
| Onah 2005 [53] | Enugu, SE; Abuja, NC | 2003 | 2 hospitals | Prospective observation of events | 224 | nr | 5 |
| Faponie 2007 [54] | Ile Ife, SW | 2005 | 1 teaching hospital | Prospective, unclear data source | 641 | 2 | 2 |
| Peripartum hysterectomy | |||||||
| Abasiattai 2013 [55] | Uyo, SE | 2004–2011 | 1 teaching hospital | Retrospective case record review | 28 | 4 | 2 |
| Nwobodo 2012 [56] | Sokoto, NW | 2005–2010 | 1 teaching hospital | Retrospective case record review | 74 | 9 | 2 |
| Rabiu 2010 [57] | Lagos, SW | 2003–2007 | 1 teaching hospital | Retrospective case record review | 57 | 11 | 2 |
| Badjoko 2013 [58] | Ile Ife, SW | 2001–2010 | 1 teaching hospital | Retrospective case record review | 55 | 10 | 3 |
| Omole Ohinsi 2012 [59] | Kano, NW | 2003–2008 | 1 teaching hospital | Retrospective case record review | 30 | 4 | 4 |
| Other post partum complications | |||||||
| Mutihir 2011 [60] | Jos, NC | 2005–2008 | 1 teaching hospital | Prospective, unclear data source | 246 | nr | 3 |
| Ajenifuja 2010 [61] | Ile Ife, SW | 2002–2006 | 1 teaching hospital | Retrospective case record review | 112 | 6 | 2 |
| Agwu 2008 [62] | Ebonyi, SE | 2003–2006 | 1 teaching hospital | Retrospective case record review | 30 | nr | 2 |
| Miscellaneous complications | |||||||
| Adelaja 2011 [63] | Sagamu, SW | 2005–2007 | 1 teaching hospital | Retrospective case record review (obstetric emergencies) | 262 | 17 | 2 |
| Kalu 2011 [64] | Ebonyi, SE | 2001–2007 | 1 teaching hospital | Retrospective case record review (umbilical cord prolapse) | 46 | nr | 2 |
| Lawani 2013 [65] | Ebonyi, SE | 2002–2012 | 1 teaching hospital | Retrospective case record review (ectopic pregnancy) | 205 | 3 | 4 |
Barriers encountered
Four types of barriers were reported, summarised in Table 2. They related to: transport and referral; health workers; availability of services; and organisational factors.
Table 2.
Summary of reported barriers and enabling factors
| Barriers | Article reference | Enabling factors | Article reference |
|---|---|---|---|
| Transport and referral | |||
| Mismanagement by referring provider | [23, 25, 26, 32–38, 44–46, 48, 57, 61] | ||
| Inefficient ambulance services | [26, 62] | ||
| Lack of transport at night | [30, 55] | ||
| Health workers | |||
| Lack of manpower | [26, 28, 32, 49, 53] | Frequent training for clinical procedures | [27, 47] |
| Unskilled health professionals | [23, 26, 27, 29, 31, 35, 37, 47, 49, 50, 52, 53, 56, 58, 60] | ||
| Low staff morale | [25, 29] | ||
| Availability of supporting services and facilities | |||
| Lack of operation theatres and intensive care units | [26, 53] | Round the clock services | [26, 53] |
| Lack of specialist medical equipment and services | [25, 26, 42, 65] | Blood banking | [26, 35, 47, 51, 53, 59] |
| Unavailability of essential drugs and supplies including blood and magnesium sulphate | [25–29, 39–43, 53, 54, 63] | ||
| Unreliable telephone communications and power supply | [26, 28, 53] | ||
| Organisation of care | |||
| Poor record keeping | [24, 38, 45, 64, 65] | Conducting maternal death reviews | [27–29] |
| Teamwork | [26, 53] | Emergency treatment before requiring payment | [47] |
| Lack of planning for organisational change | [32, 53] | ||
Transport and referral
Ineffective and inappropriate referral were identified in the studies as important contributory factors to adverse outcomes. Referred obstetric emergencies were reportedly poorly managed prior to arrival. Practitioners responsible for mismanagement of referral and causing delays included traditional birth attendants [23, 44], general practitioners, private providers and unregulated medical providers [25, 33]. These practitioners were based in traditional maternity homes, churches and faith clinics [35, 46, 61] as well as within the routine health system in health facilities [38]. Reported mismanagement prior to arrival in the study hospital included unhygienic birth practices [35], manipulative procedures performed by unqualified people [34–36] and self-induced manipulation [37]. The injudicious use of oxytocin in labor was also described [32, 44, 45, 48]. Some studies described inefficient ambulance services, poor transport between health facilities [26, 62] and lack of transport especially at night [30, 55].
Health workers
The availability, skills and morale of health personnel were reported as key barriers to providing adequate care. Lack of manpower was identified [32], including insufficient numbers of nurses and midwives for the existing care loads [26] and absence of middle grade medical officers (registrars) [49]. Junior doctors were reportedly inexperienced and untrained [49, 53] and a number of studies reported delays in provision of appropriate care after the pregnant woman had arrived in the hospital [23, 26, 53]. One study reported that 32.9 % of critically ill women received treatment over an hour after diagnosis had been made [28]. Nursing staff did not perform well in routine monitoring of vital signs [29]. Poor diagnostic skills were a problem, for example with junior doctors and midwives on night duty missing cases of retained placenta [60], poor asepsis practised during procedures [35] and incorrect diagnosis before major surgery [58]. Deviations from standard treatment norms were reported in over 40 % of adverse maternal outcome [28]. Some studies reported a higher occurrence of morbidity during surgery by less experienced obstetricians and anaesthesiologists [37, 49, 56] although others acknowledged that the senior doctors performed more elective procedures which had lower rates of morbidity compared to emergency procedures done by junior and mid-level clinicians [52]. Poor staff morale and motivation were cited, with delays in receiving salaries and unwillingness to follow clinical protocols [29]. Industrial strike action by health workers was reported as contributing to maternal death [25].
Availability of supporting services and facilities
Insufficient availability of operation theatres and suboptimal intensive care units were described [26]. Mean decision to delivery intervals for Caesarean sections were 3.3 h in one hospital and 8.5 h in another [53]. Anaesthesia-related factors and poor blood availability were reported in several studies. For instance, delays in proceeding with surgery occurred due to lack of skilled anaesthetists, anaesthetic drugs, gases and equipment; as well as poor availability of blood and cross matching facilities and linen [25, 26, 28, 29, 53, 54, 63]. Other services and facilities reported as lacking included intensive clinical monitoring procedures like arterial blood and central venous pressure [42] and equipment like laparoscopy and ultrasound scanning for diagnosis and treatment [65]. The unavailability of magnesium sulphate was reported in several studies [27, 29, 39–43]. Apart from the clinical services, erratic and unreliable telephone services [53] and power supplies [28] were reported.
Organisation of care
Limitations were found in relation to record keeping, procedural norms and planning for change. Examples of poor record keeping included no recording of time from diagnosis to treatment [64] and missing records [24, 38, 45, 65]. The lack of interdepartmental teamwork [26] and poor organisation of rotas (despite availability of personnel) [53] were attributed to causing substandard care. In one review of maternal deaths, a sudden increase in maternal mortality had been observed after the hospital was upgraded from general to specialist level. The authors explained the phenomena as a result of manpower shortages and inadequate facilities to cope with the upgrade, cautioning that careful planning was required to mitigate against problems [32].
Enabling factors
Specialised and frequent training in abortion care was linked to good management of abortion related complications [27]. Highly experienced anaesthetists reportedly contributed to lowered maternal mortality in emergencies [47]. The availability of 24 h, round the clock medical and laboratory services, with organised staff rotas were cited as contributing factors when care was judged to be adequate in the included studies [26, 53]. The availability of blood bank facilities were cited as an enabling factors in several studies [26, 35, 47, 51, 53]. Conducting audit was found to be a positive experience that led to practical action and improvement in care practices [27–29]. The practice of treating emergencies before demanding payment was also highlighted [47].
Discussion
Improving care and reducing maternal mortality
Barriers related to referral, transport, the availability and skills of health professionals, physical infrastructure, lack of essential drugs and supplies, poor record keeping systems and disorganised planning were common factors found across the studies. There were few enabling factors reported. Intensive training for clinical procedures, 24 h services, conducting maternal death reviews and flexible payment modalities reportedly contributed to facilitating care.
The barriers identified concur with the findings of other studies in Africa as well as in other low income settings [66–68]. In a review of audit-identifiable avoidable factors in low resource settings, substandard practices by health workers and delays in blood transfusion were found to be the commonest reported problems [1]. Of the priority emergency obstetric services defined by the World Health Organization [69], three elements stand out in Nigeria: delays in Caesarean section, unavailability of magnesium sulphate and lack of safe blood transfusion services. We found that these three situations occur in tertiary and teaching hospitals in Nigeria, yet the facilities reporting their occurrence represent the pinnacle of service provision and it is likely the deficiencies are even more pronounced in rural and basic-level hospitals.
With a quarter of a century of safe, low cost magnesium sulphate use behind us, it is inexcusable that any country still experiences unavailability. Problems of production and distribution, inadequate and poorly implemented clinical guidelines, and the lack of political support for policy change need to be addressed [70]. In 2004, Nigeria was one of the recipients of the the US President’s Emergency Plan for AIDS Relief (PEPFAR) programme which aimed to strengthen national blood transfusion services in the setting of high HIV prevalence, yet calls to take action continue [71] . Our study gives weight to an urgent need for national and local efforts to resolve these fundamental shortcomings in the availability of blood and magnesium sulphate. Delays experienced in conducting emergency caesarean sections are analysed in depth by several authors of the included papers [28, 37, 53]. The challenges faced are complex and relate to a range of health system factors including availability, skills and skill mix of the obstetric team and organisation of services. Similarly, addressing the problems of transport, referral and record keeping require a health systems approach, further probing into root causes and combinations of solutions and actions both at local and central level.
Good practices for conducting obstetric audit
Apart from our aim of identifying barriers and enabling factors, this systematic review has drawn out important considerations related to improving how maternal death reviews and obstetric audits are conducted. In the case of Nigeria, this will have particular relevance given the mandate to roll-out a national programme. Given the years of experience found in Nigeria, the aim should be not only to promote the conduct of audit in settings outside the tertiary and teaching hospitals, but also to improve the way audits are conducted so as to implement a process that captures insights and problems more effectively. In this systematic review we found a few studies which explicitly made comparisons against pre-specified criteria [27–30], which allows for a structured and objective assessment of care against explicit criteria, making for improved utility as a quality improvement tool [1, 13]. Other studies found also provided useful insights into aspects of quality improvement, although the process through which their findings were reported could be haphazard and sometimes anecdotal. In addition, the quality assessment we used highlighted a number of good practices we think useful to consider in improving the conduct and reporting of audits and reviews. Of the nine criteria we used in our quality assessment, all papers described the study population and sampling process but other good practices such as training for data collectors and standardised data entry (Fig. 2) were not described by authors, and we surmise that they were not done. The presentation of maternal death reviews could be improved by paying greater attention to describing these criteria fully. Underlying these design and reporting issues are the need to improve case notes and reduce the proportion of missing information in the routine health information system.
Fig 2.
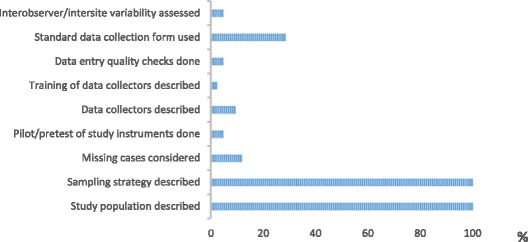
Percentage of included papers fulfilling quality assessment criteria. Graph showing percentage of papers included in the systematic review which fulfilled each of nine quality assessment criteria
Limitations
We faced some limitations in conducting the systematic review. Our search was confined to databases of published literature. Maternal death reviews done may not be published or may be reported in journals with incomplete archives, as evidenced by the relatively large number (n = 72) of full-text articles not available on-line or on inter-library loan from the British Library (Fig. 1). To capture a wider range of studies, we used broader inclusion criteria to define maternal death reviews and audits. Nevertheless our sample may not have been exhaustive. However, the purpose of synthesis in this review was to seek coherence of findings and to provide interpretive explanation. As similar barriers were found across the different and independent studies across Nigeria we suggest that commonly experienced factors are likely to have been captured [72]. Our study was confined in terms of its representativeness of different types of health facilities. All studies found were conducted in tertiary or teaching hospitals, so the findings cannot be extrapolated to the circumstances and care provided in primary and secondary level health facilities in Nigeria. With 36 % of deliveries occurring in health facilities in Nigeria and 38 % with health professionals [8] the services provided at tertiary level represent only the ‘tip of the iceberg’. It may be argued that critically ill women will present at tertiary facilities however, the reality is that many women in low and middle income countries are unable to reach this level of the health system [68]. It is likely that the barriers faced are greater in other types of health facilities, as the teaching and tertiary hospitals represent the best care available to the majority of women. In addition, the hospital based studies do not permit full elicitation of community factors that impact on emergency care. Despite these caveats, we believe useful lessons can be drawn from this systematic review.
Conclusion
This systematic review synthesises experiences of maternal death review and other obstetric audits in Nigeria. The barriers identified are avoidable and most can be overcome by strong and concerted action.
The recommendations emerging from this review are of three types: improving care, enhancing the existing audit process, and extending audit beyond the tertiary and teaching hospital setting. For the improvement of emergency obstetric care, it is clear that concerted effort is needed to make magnesium sulphate for eclampsia consistently available throughout the country and to improve blood transfusion services. Organisational change should especially address delays in conducting emergency Caesarean sections, referral barriers and manpower problems in the health system. The new national maternal death review system in Nigeria can take cognisance of the experience already built up and place emphasis on improving how audits are conducted. To enhance existing audit processes, we suggest that, by setting pre-specified criteria and making comparisons against these criteria, assessments of care may be improved by becoming more structured and objective I n nature. Training for those involved in audit especially individuals responsible for reporting and collecting data will be necessary, along with the need to improve on how events are recorded in clinical case notes. The storage and retrieval of case notes is also important to reduce the proportion of missing information. Finally, our knowledge of care practices is confined to the highest referral level. We recommend the extension of reviews and audits to other health facilities and in the community. This could be done initially by setting up well conducted small scale studies to learn from implementation of audit outside hospital environments: the problems are likely to be similar but more pronounced to those seen in hospitals, such as poor record keeping, lack of experience in conducting audits and low staff motivation. Identifying a suitable site to conduct pilot audit studies will also contribute to the learning experience before attempting to scale up efforts. Experiences will be gained by targeting various settings such as district hospitals, health centres and community-based locations, with each having a set of different barriers to overcome.
This synthesis has shown that the key challenges to reducing maternal mortality in Nigeria are already well known and that we also have the know-how to implement the required actions. ‘Business as usual’ is not enough. The challenge for the future is to build on the experiences of the past, deepen our understanding, generate creative solutions for complex problems and persist in implementing what we know should be done.
Acknowledgements
We would like to thank Yutaka Osakabe for co-ordinating the retrieval of full text articles. The John D. and Catherine T. MacArthur Foundation supported this study, grant number 12-100074-000-INP
Footnotes
Competing interests
The authors have no competing interests to declare.
Authors’ contributions
JH conceived the study idea and developed the protocol with MI. AH led the data extraction and was supported by OO and LK. OO and LK completed the quality assessment. The first draft was written by JH. All authors read, revised and commented on subsequent drafts of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Julia Hussein, Email: j.hussein@abdn.ac.uk.
Atsumi Hirose, Email: atsumi.hirose@gmail.com.
Oluwatoyin Owolabi, Email: toyindupcee@yahoo.com.
Mari Imamura, Email: m.imamura@abdn.ac.uk.
Lovney Kanguru, Email: l.n.kanguru@abdn.ac.uk.
Friday Okonofua, Email: feokonofua@yahoo.co.uk.
References
- 1.Merali HS, Lipsitz S, Hevelone N, Gawande AA, Lashoher A, Agrawal P, Spector J. Audit-identified avoidable factors in maternal and perinatal deaths in low resource settings: a systematic review. BMC Pregnancy Childb. 2014;14:280. doi: 10.1186/1471-2393-14-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hounton S, De Bernis L, Hussein J, Graham W, Danel I, Byass P. Mason EM Towards elimination of maternal deaths: maternal deaths surveillance and response. Reprod Health. 2013;10:1. doi: 10.1186/1742-4755-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Maternal death surveillance and response: technical guidance information for action to prevent maternal death. Geneva: WHO; 2013. [Google Scholar]
- 4.Power M. The Audit Society: Rituals of verification. New York: Oxford University Press Inc; 1997. [Google Scholar]
- 5.Mayne J. Audit and evaluation in public management: challenges, reforms and different roles. Can J Program Eval. 2006;21(1):11–45. [Google Scholar]
- 6.National Population Commission (NPC) [Nigeria] and ICF Internationa . Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF Internationa; 2014. [Google Scholar]
- 7.World Health Organization . Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. 2014. [Google Scholar]
- 8.Federal Republic of Nigeria . Countdown strategy 2010 to 2015, Millennium Development Goals (MDGs) Abuja: Government of the Federal Republic of Nigeria; 2010. [Google Scholar]
- 9.Gomez GB, Foster N, Brals D, Nelissen HE, Bolarinwa OA, Hendriks ME, Boers AC, van Eck D, Rosendaal N, Adenusi P, Agbede K, Akande TM, Boele van Hensbroek M, Wit FW, Hankins CA, Schultsz C. Improving Maternal Care through a State-Wide Health Insurance Program: A Cost and Cost-Effectiveness Study in Rural Nigeria. PLoS One. 2015;10(9):e0139048. doi: 10.1371/journal.pone.0139048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haver J, Brieger W, Zoungrana J, Ansari N, Kagoma J. Experiences engaging community health workers to provide maternal and newborn health services: implementation of four programs. Int J Gynaecol Obstet. 2015;Suppl 2:S32–S39. doi: 10.1016/j.ijgo.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Kana MA, Doctor HV, Peleteiro B, Lunet N, Barros H. Maternal and child health interventions in Nigeria: a systematic review of published studies from 1990 to 2014. BMC Public Health. 2015;15:334. doi: 10.1186/s12889-015-1688-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abimbola S, Okoli U, Olubajo O, Abdullahi MJ, Pate MA. The Midwives Service Scheme in Nigeria. PLoS Med. 2012;9(5):e1001211. doi: 10.1371/journal.pmed.1001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Beyond the numbers. Geneva: WHO; 2004. [Google Scholar]
- 14.Pattinson R, Kerber K, Waiswa P, Day LT, Mussell F, Asiruddin SK, Blencowe H, Lawn JE. Perinatal mortality audit: counting, accountability, and overcoming challenges in scaling up in low- and middle-income countries. Int J Gynaecol Obstet. 2009;107(Suppl 1):S113–S121. doi: 10.1016/j.ijgo.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Dumont A, Fournier P, Abrahamowicz M, Traore M, Haddad S, Fraser WD. Quality of care, risk management, and technology in obstetrics to reduce hospital-based maternal mortality in Senegal and Mali (QUARITE): a cluster-randomised trial. Lancet. 2013;382(9887):146–157. doi: 10.1016/S0140-6736(13)60593-0. [DOI] [PubMed] [Google Scholar]
- 16.Achem FF, Agboghoroma CO. Setting up facility-based maternal deaths reviews in Nigeria. BJOG. 2014;121(Suppl. 4):75–80. doi: 10.1111/1471-0528.12817. [DOI] [PubMed] [Google Scholar]
- 17.Hussein J, Okonofua F. Time for Action: Audit, accountability and confidential enquiries into maternal deaths in Nigeria. Afr J Reprod Health. 2012;16(1):9–14. [PubMed] [Google Scholar]
- 18.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, editors. Analyzing qualitative data. London: Sage; 1993. pp. 173–194. [Google Scholar]
- 19.Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ. 2000;320:116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Committee for Confidential Enquiry into Maternal Deaths (NCCEMD). Fifth report on the Confidential Enquiries into Maternal Deaths in South Africa: Comprehensive Report. Appendix 2: Process and method of assessment. Department of Health, Republic of South Africa; 2012.
- 21.D’Ambruoso L, Achadi E, Adisasmita A, Izati Y, Makowiecka K, Hussein J. Assessing quality of care provided by Indonesian village midwives with a confidential enquiry. Midwifery. 2009;25(5):528–539. doi: 10.1016/j.midw.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Pirkle CM, Dumont A, Zunzunegui MV. Criterion-based clinical audit to assess quality of obstetrical care in low- and middle-income countries: a systematic review. Int J Qual Health Care. 2011;23(4):456–463. doi: 10.1093/intqhc/mzr033. [DOI] [PubMed] [Google Scholar]
- 23.Ande A, Olagbuji B, Ezeanochie M. An Audit of Maternal deaths from a referral University Teaching Hospital in Nigeria: The Emergence of HIV/AIDS as a leading cause. Niger Postgrad Med J. 2012;19(2):83–87. [PubMed] [Google Scholar]
- 24.Ezugwu EC, Onah HE, Ezugwu FO, Okafor II. Maternal Mortality in a Transitional Hospital in Enugu, South East Nigeria. Afr J Reprod Health. 2009;13(4):67–72. [PubMed] [Google Scholar]
- 25.Ozumba BC, Nwogu-Ikojo EE. Avoidable maternal mortality in Enugu, Nigeria. J Royal Inst Public Health. 2008;122:354–360. doi: 10.1016/j.puhe.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 26.Omo-Aghoja LO, Aisien OA, Akuse JT, Bergstrom S, Okonofua FE. Maternal mortality and emergency obstetric care in Benin City, South-south Nigeria. J Clin Med Res. 2010;2(4):55–60. [Google Scholar]
- 27.Oladapo OT, Sule-Odu AO, Olatunji AO, Daniel OJ. “Near-miss” obstetric events and maternal deaths in Sagamu, Nigeria: a retrospective study. Reproductive Health. 2005;2:9. doi: 10.1186/1742-4755-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oladapo OT, Ariba AJ, Odusoga OL. Changing patterns of emergency obstetric care at a Nigerian University hospital. Int J Gynec Obstet. 2007;98:278–284. doi: 10.1016/j.ijgo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 29.Hunyinbo KI, Fawole AO, Sotiloye OS, Otolorin EO. Evaluation of criteria-based clinical audit in improving quality of obstetric care in developing country hospital. Afr J Reprod Health. 2008;12(3):59–70. [PubMed] [Google Scholar]
- 30.Adeoye IA, Onayade AA, Futusi AO. Incidence, determinants and perinatal outcomes of near miss maternal morbidity in Ile-Ife Nigeria: a prospective case control study. BMC Pregnancy Childb. 2013;13:93. doi: 10.1186/1471-2393-13-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olagbuji BN, Ezeanochie MC, Igbaruma S, Okoigi SO, Ande AB. Stillbirth in cases of severe acute maternal morbidity. Int J Gynec Obstet. 2012;119:53–56. doi: 10.1016/j.ijgo.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 32.Ezugwu EC, Ona HE, Ezugwui HC. Nnanji. Stillbirth rate at an emerging tertiary health institution in Enugu, Southeast Nigeria. Int J Gynec Obstet. 2011;115:164–166. doi: 10.1016/j.ijgo.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 33.Olusanya BO, Solanke OA. Predictors of term stillbirths in an inner-city maternity hospital in Lagos, Nigeria. Acta Obstet Gynecol. 2009;88:1243–1251. doi: 10.3109/00016340903287474. [DOI] [PubMed] [Google Scholar]
- 34.Ibrahim IA, Onwudiegwu U. Sociodemographic determinants of complicated unsafe abortions in a semi-urban Nigerian town: a four-year review. West Indian Med J. 2012;61(2):163–167. [PubMed] [Google Scholar]
- 35.Raibu KA, Omolulu OM, Ojo TO, Adewunmi AA, Alugo BG. Unsafe abortion in Lagos Nigeria: a continuing tragedy. Niger Postgrad Med J. 2009;16(4):251–255. [PubMed] [Google Scholar]
- 36.Nwogu-Ikojo EE, Ezegwui HU. Abortion-related mortality in a tertiary medical centre in Enugu, Nigeria. J Obstet Gynaecol. 2007;27(8):835–837. doi: 10.1080/01443610701718883. [DOI] [PubMed] [Google Scholar]
- 37.Ekanem EI, Etuk SJ, Ekabua JE, Iklaki C. Clinical presentation and complications in patients with unsafe abortions in University of Calabar Teaching Hospital, Calabar, Nigeria. Niger J Med. 2009;18(4):370–374. doi: 10.4314/njm.v18i4.51245. [DOI] [PubMed] [Google Scholar]
- 38.Adinma ED. Maternal and perinatal outcome of eclampsia in tertiary health institution in Southeast Nigeria. J Mater-fetal Neonatal Med. 2013;26(2):211–214. doi: 10.3109/14767058.2012.722708. [DOI] [PubMed] [Google Scholar]
- 39.Eke AC, Ezebialu IU, Okafor C. Presentation and outcome of eclampsia at a tertiary center in Southeast Nigeria - a 6-year review. Hypertens Pregnancy. 2011;30:125–132. doi: 10.3109/10641955.2010.525283. [DOI] [PubMed] [Google Scholar]
- 40.Agida ET, Adeka BI, Jibril KA. Pregnancy outcome in eclamptics at the University of Abuja Teaching Hospital, Gwagwalada, Abuja: a 3 year review. Niger J Clin Pract. 2010;13(4):394–398. [PubMed] [Google Scholar]
- 41.Kullima AA, Kawuwa MB, Audu BM, Usman H, Geidam AD. A 5-year review of maternal mortality associated with eclampsia in a tertiary institution in northern Nigeria. Ann Afr M. 2009;8(2):81–84. doi: 10.4103/1596-3519.56233. [DOI] [PubMed] [Google Scholar]
- 42.Okafor UV, Efetie RE. Critical care management of eclamptics: challenges in an African setting. Trop Dr. 2008;38:11–13. doi: 10.1258/td.2007.053260. [DOI] [PubMed] [Google Scholar]
- 43.Makinde ON, Adegoke OA, Adediran IA, Ndububa DA, Adeyemi AB, Owolabi AT, Kuti O, Orji EO, Salawu L. HELLP syndrome: the experience at Ile-Ife. Nigeria. J Obstet Gynaec. 2009;29(3):195–199. doi: 10.1080/01443610902753945. [DOI] [PubMed] [Google Scholar]
- 44.Nyengidiki TK, Allagoa DO. Rupture of the gravid uterus in a tertiary health facility in the Niger deltaregion of Nigeria: A 5-year review. Niger Med J. 2011;52(4):230–234. doi: 10.4103/0300-1652.93794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Esike COU, Umeora OUJ, Eze JN, Igberase GO. Ruptured uterus: the unabating obstetric catastrophe in South eastern Nigeria. Arch Gynecol Obstet. 2011;283:993–997. doi: 10.1007/s00404-010-1488-z. [DOI] [PubMed] [Google Scholar]
- 46.Osaikhuwuomwan JA, Ande AB. Reappraisal of ruptured uterus in an urban tertiary center in the Niger-delta region of Nigeria. J Mater-Fetal Neonatal Med. 2011;24(4):559–563. doi: 10.3109/14767058.2010.497880. [DOI] [PubMed] [Google Scholar]
- 47.Okafor UV, Aniebue U. Anaesthesia for uterine rupture in a Nigerian teaching hospital: maternal and fetaloutcome. Int J Obstet Anaesth. 2006;15:124–128. doi: 10.1016/j.ijoa.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 48.Mbamara SU, Obiechina NJA, Elije GU. An analysis of uterine rupture at the Nnamdi Asikiwi University Teaching Hospital Nnewi. Southeast Nigeria. Niger J Clin Pract. 2012;15(4):448–452. doi: 10.4103/1119-3077.104524. [DOI] [PubMed] [Google Scholar]
- 49.Onankpa B, Ekele B. Fetal outcome following cesarean section in a university teaching hospital. J Natl Med Assoc. 2009;101(6):578–581. doi: 10.1016/S0027-9684(15)30943-3. [DOI] [PubMed] [Google Scholar]
- 50.Ekanem AD, Udoma EJ, Etuk SJ, Eshiet AI. Outcome of emergency caesarean sections in Calabara, Nigeria: Impact of the seniority of the medical team. J Obstet Gynaecol. 2008;28(2):198–201. doi: 10.1080/01443610801912329. [DOI] [PubMed] [Google Scholar]
- 51.Ozumba BC, Ezegwui HU. Blood transfusion and caesarean section in a developing country. J Obstet Gynaecol. 2006;26(8):746–748. doi: 10.1080/01443610600955792. [DOI] [PubMed] [Google Scholar]
- 52.Ojiyi E, Dike E, Anolue F, Chukwulebe A. Appraisal Of Caesarean Section At The Imo State University Teaching Hospital, Orlu, Southeastern Nigeria. Internet J Gynecol Obstet. 2012;16(2):1–6. [Google Scholar]
- 53.Onah HE, Ibeziako N, Umezulike AC, Effetie ER, Ogbuokiri CM. Decision-delivery interval and perinatal outcome in emergency caesarean sections. J Obstet Gynaecol. 2005;25(4):342–346. doi: 10.1080/01443610500119671. [DOI] [PubMed] [Google Scholar]
- 54.Faponle AF, Makinde ON. Caesarean section: intra-operative blood loss and its restitution. East Afr Med J. 2007;84(1):31–34. doi: 10.4314/eamj.v84i1.9488. [DOI] [PubMed] [Google Scholar]
- 55.Abasiattai AM, Umoiyoho AJ, Utuk NM, Inyang-Etoh EC, Asuquo OP. Emergency peripartum hysterectomy in a tertiary hospital in southern Nigeria. Pan Afr Med J. 2013;15:60–66. doi: 10.11604/pamj.2013.15.60.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nwobodo EI, Nnadi DC. Emergency Obstetric Hysterectomy in a Tertiary Hospital in Sokoto, Nigeria. Ann Med Health Sci Res. 2012;2(1):37–40. doi: 10.4103/2141-9248.96935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rabiu KA, Akinlusi FM, Adewunmi AA, Akinola OI. Emergency peripartum hysterectomy in a tertiary hospital in Lagos, Nigeria: a five-year review. Trop Dr. 2010;40(1):1–4. doi: 10.1258/td.2009.090084. [DOI] [PubMed] [Google Scholar]
- 58.Badejoko OO, Awowole IO, Ijarotimi AO, Badejoko BO, Loto OM, Ogunniyi SO. Obstetric hysterectomy: Trend and outcome in Ile-Ife, Nigeria. J Obstet Gynaecol. 2013;33:581–584. doi: 10.3109/01443615.2013.786032. [DOI] [PubMed] [Google Scholar]
- 59.Omole-Ohonsi A, Olayinka HT. Emergency Peripartum Hysterectomy in a Developing Country. J Obstet Gynaecol. 2012;34(10):954–960. doi: 10.1016/S1701-2163(16)35409-3. [DOI] [PubMed] [Google Scholar]
- 60.Mutihir JT, Utoo BT. Postpartum maternal morbidity in Jos, north-central Nigeria. Niger J Clin Pract. 2011;14(1):38–42. doi: 10.4103/1119-3077.79238. [DOI] [PubMed] [Google Scholar]
- 61.Ajenifuja KO, Adepiti CA, Ogunniyi SO. Post partum haemorrhage in a teaching hospital in Nigeria: a 5-year experience. Afr Health Sci. 2010;10(1):71–74. [PMC free article] [PubMed] [Google Scholar]
- 62.Agwu UM, Umeora OUJ, Ejikeme BN, Egwuatu VE. Retained placenta aspect of clinical management in a tertiary health institution in Nigeria. Niger J Med. 2008;17(2):146–149. doi: 10.4314/njm.v17i2.37304. [DOI] [PubMed] [Google Scholar]
- 63.Adelaja LM, Taiwo OO. Maternal and Fetal Outcome of Obstetric Emergencies in a Tertiary Health Institution in South-Western Nigeria. ISRN Obstet Gynecol. 2011. doi:10.5402/2011/160932. [DOI] [PMC free article] [PubMed]
- 64.Kalu CA, Umeora OUJ. Risk factors and perinatal outcome of umbilical cord prolapse in Ebonyi State University Teaching Hospital, Abakaliki, Nigeria. Niger J Clin Pract. 2011;14(4):413–417. doi: 10.4103/1119-3077.91746. [DOI] [PubMed] [Google Scholar]
- 65.Lawani O, Anozie OB, Ezeonu PO. Ectopic pregnancy: a life-threatening gynaecological emergency. Int J Women's Health. 2013;5:515–521. doi: 10.2147/IJWH.S49672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Owens L, Semrau K, Mbewe R, Musokotwane K, Grogan C, Maine D, Hamer DH. The state of routine and emergency obstetric and neonatal care in Southern Province, Zambia. Int J Gynaecol Obstet. 2015;128(1):53–57. doi: 10.1016/j.ijgo.2014.07.028. [DOI] [PubMed] [Google Scholar]
- 67.Mirkuzie AH, Sisay MM, Reta AT, Bedane MM. Current evidence on basic emergency obstetric and newborn care services in Addis Ababa, Ethiopia; a cross sectional study. BMC Pregnancy Childb. 2014;14:354. doi: 10.1186/1471-2393-14-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ameh C, Msuya S, Hofman J, Raven J, Mathai M, van den Broek N. Status of emergency obstetric care in six developing countries five years before the MDG targets for maternal and newborn health. PLoS One. 2012;7(12):e49938. doi: 10.1371/journal.pone.0049938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lumbiganon P, Gülmezoglu AM, Piaggio G, Langer A, Grimshaw J. Magnesium sulfate is not used for pre-eclampsia and eclampsia in Mexico and Thailand as much as it should be. Bull World Health Organiz. 2007;85(10):733–820. doi: 10.2471/BLT.06.037911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.World Health Organization . Monitoring emergency obstetric care: a handbook. Geneva: WHO; 2009. [Google Scholar]
- 71.Osaro E, Charles AT. The challenges of meeting the blood transfusion requirements in Sub-Saharan Africa: the need for the development of alternatives to allogenic blood. Blood Med. 2011;2:7–21. doi: 10.2147/JBM.S17194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, Rashidian A. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev. 2013; Issue 10 Art. No.: CD010414. doi: 10.1002/14651858.CD010414.pub2. [DOI] [PMC free article] [PubMed]


