Abstract
Objective
This review investigates the relationship between leg muscle power and the chronic conditions of osteoarthritis, diabetes mellitus, and cardiovascular disease among older adults. Current literature assessing the impact of chronic disease on leg power has not yet been comprehensively characterized. Importantly, individuals with these conditions have shown improved leg power with training.
Methods
A search was performed using PubMed to identify original studies published in English from January 1998 to August 2013. Leg power studies, among older adults ≥ 50 years of age, which assessed associations with osteoarthritis, diabetes mellitus, and/or cardiovascular disease were selected. Studies concerning post-surgery rehabilitation, case studies, and articles that did not measure primary results were excluded.
Results
Sixteen studies met inclusion criteria, addressing osteoarthritis (n=5), diabetes mellitus (n=5), and cardiovascular disease (n=6). Studies generally supported associations of lower leg power among older adults with chronic disease, although small sample sizes, cross-sectional data, homogenous populations, varied disease definitions, and inconsistent leg power methods limited conclusions.
Conclusions
Studies suggest that osteoarthritis, diabetes mellitus, and cardiovascular disease are associated with lower leg power compared to older adults without these conditions. These studies are limited, however, by the heterogeneity in study populations and a lack of standardized measurements of leg power. Future larger studies of more diverse older adults with well-defined chronic disease using standard measures of leg power and interventions to improve leg power in these older adults with chronic disease are needed.
Keywords: Leg power, older adults, chronic disease, aging, muscle power
Introduction
Leg muscle power, the ability to exert force with the lower extremities quickly (Power= Force x Velocity) (1), is a predictor of disability among older adults (2, 3). Lower leg power is an early indicator of poor function and higher leg power may indicate preserved physical function (4, 5). High muscle power output involves the ability to produce high muscle force and develop high contraction velocity (6, 7). An inverse J-shaped power-load relationship exists, where higher external resistances generate lower muscle power due to the low velocity of the movement (8). In a similar manner, low muscle power is typically generated at very low external resistance due to a lower force component. In contrast to the assessment of muscle strength (most often measured during isometric conditions), muscle power can be assessed at a variable external resistance (i.e. individual’s own body weight during sit-to-stand) that ultimately determines the velocity of the movement. Aging adults experience muscle power decline earlier than muscle strength decline (9, 10). Therefore, leg power measurements may be more discriminant predictors of functional loss in older adults as well as identify individuals with preserved physical function (3, 11, 12).
The purpose of this review is to investigate the impact of osteoarthritis (OA), diabetes mellitus (DM), and cardiovascular disease (CVD) on leg power among older adults. These conditions have a high prevalence among older adults (13) and are associated with impairments of lower-extremity functioning and mobility (14–16). Individuals with OA experience muscle atrophy, joint stiffness and a reduced range of motion (16). As a result of decreased bone cartilage and abnormal bone formation surrounding joints affected by OA, surrounding muscle becomes weak and stiff (17). In addition, a wide range of comorbidities, including peripheral neuropathy and obesity, often present in DM are considered to play a key role in decreased muscle quality (18–20). Decreased exercise capacity in older adults with CVD may result in poorer muscle function (21, 22), as well as insufficient blood flow to active skeletal muscle, muscle fiber loss, and demyelination of peripheral nerves (23–25). OA, DM, and CVD are particularly important to evaluate in relationship to leg power since they are relatively modifiable conditions and are associated with physical function loss (26–28). Despite different pathological origins, OA, DM, and CVD share common pathways of reduced maximum working capacity and direct and/or indirect effects on neuromuscular function (with particular reference to muscle power), which potentially may be a pathway to a higher risk of disability.
Varied equipment, measurement techniques, exclusion criteria, and study populations make the direct comparison of findings across leg power studies difficult (29). When assessing age-related declines in leg power, optimal velocities and loads are essential for obtaining accurate measurements (30, 31). Leg power is often measured in seated positions and requires unilateral or bilateral leg press movements (Nottingham power rig, Concept II dynamometer, Keiser pneumatic leg press, isotonic mode of Biodex system III dynamometer). The Nottingham power rig is a measurement device where a fixed load (flywheel) is pushed unilaterally through a footplate during a leg press action (32). As a result of the fixed load, it is not possible to determine which portion of the power-load curve an individual falls. A direct consequence is that weaker individuals may work in a disadvantaged portion of the J-shaped power-load relationship (i.e. high “relative load” according to individual maximum power), resulting in poorer performance (8, 31). The Concept II dynamometer and isotonic mode of the Biodex system III dynamometer measure seated leg extensor power at a fixed load, similar to the Nottingham power rig. Although isokinetic assessments are common measures of muscle performance, these devices measure force at a given (constant) velocity and are not the optimal leg power measures for older adults. Other devices include force plate ergometry, where the body acts as an external resistance during weight-bearing conditions, to assess power. These methods include jumping mechanography (countermovement, squatting jumps), sit-to-stand movements, box stepping tests, and bike ergometry during a two-revolution maximum (33–35). These measures which are body-weight bearing may more closely approximate the power necessary to maintain activities of daily living in older adults.
The relationship between leg power and chronic disease in older adults has not yet been comprehensively examined. A limited amount of studies have assessed direct relationships between leg power and chronic conditions in older adults, however, previous findings have indicated a need for further investigation. Kuo et al. (36) found that each standard deviation increase in knee extensor power was associated with a 27–42% reduction of disability likelihood in a cohort aged ≥ 60 years with hypertension (67%) and DM (15.7%) (p< 0.004). Foldvari et al. (11) noted that leg power had the strongest univariate correlation to self-reported functional status among older women with a mean of 3.2 ± 1.9 chronic diseases (r= −0.47, p< 0.0001) compared to other independent variables such as leg press strength and chest press power. At baseline, results of Orr et al. (37) indicated a higher number of comorbidities (most common: 76% hypertension and 84% OA), poorer muscle power, and additional functional indicators such as gait speed, muscle contraction velocity, and percent body fat in older obese adults with type 2 DM were related to impaired balance (p< 0.05 for all). The mentioned studies emphasize the importance of more in-depth and mechanistic studies to better characterize the relationships of chronic disease in older adults and leg power.
Methods
The National Library of Medicine (PubMed) was used to identify articles published in English from January 1998 to August 2013 on the relationship between leg power and chronic disease. The keywords “chronic disease”, “osteoarthritis”, “diabetes”, “cardiovascular disease”, “myocardial infarction”, “coronary artery disease”, “heart failure”, “peripheral vascular disease”, “peripheral arterial disease”, and “hypertension” were combined with “muscle power”, “leg power”, “quadriceps power”, and “leg extensor power”. This search resulted in 99 articles [Figure 1]. Abstracts and full articles were reviewed to select relevant, original studies addressing associations between leg power and the specified chronic diseases among older adults. Due to the scarcity of existing literature, studies with participants ≥ 50 years of age were chosen to comprehensively include older adults with chronic disease impacting leg power as they approached late life.
Figure 1.
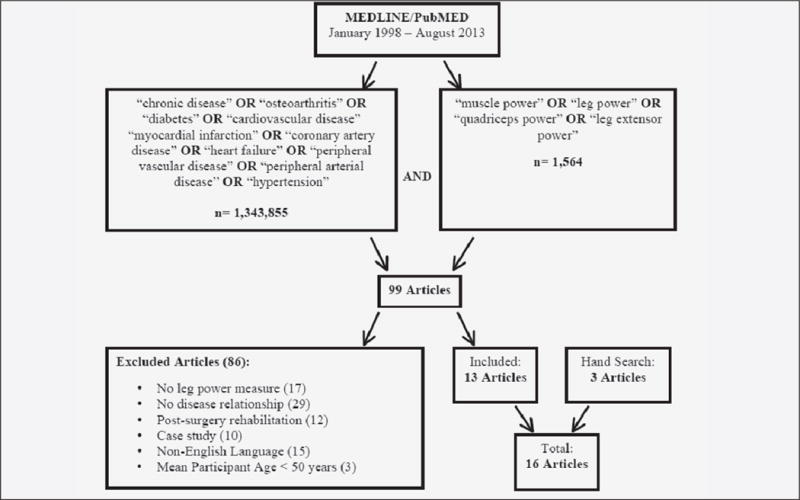
Literature review search strategy and selection criteria of MEDLINE/PubMED articles (January 1998 – August 2013) on the relationship between leg power and selected chronic disease (OA, DM, and CVD) in older adults
Eighty-six studies met exclusion criteria. Articles that did not measure primary results or leg power (n=17) and did not address the relationship between OA, DM, or CVD (n=29) were excluded, including studies that only reported chronic disease prevalence, measured leg power among populations with chronic disease without investigating associations, and/or only assessed the risk of disease development. Studies concerning post-surgery leg power rehabilitation (n=12), case studies (n=10), non-English language articles (n=15), and studies with a mean age ≤ 50 years (n=3) were excluded.
Three additional studies were found from a search of personal archives and cross-references. Overall, 16 articles met the selection criteria focusing on OA (n=5), DM (n=5), and CVD (n=6). Three of the studies used data from exercise, resistance or power training programs. Leg power measures were assessed by the Nottingham power rig (n=7), Keiser pneumatic leg press (n=1), half-squat test (n=1), Concept II dynamometer (n=1), Biodex System III isotonic dynamometer (n=1), and various isokinetic dynamometers (n=5).
Osteoarthritis (OA)
Knee OA has rarely been studied with respect to leg power in older adults (38). Arthritis and arthritic illnesses are the leading causes of lower-extremity disability in the United States (39). OA affects over half of all individuals aged ≥ 65 years (21, 40) and the incidence increases with age (41, 42). Symptomatic OA can result in chronic pain, muscle weakness, limited range of motion, and impaired daily activities (40). Pain and joint stiffness may impair comprehensive muscle function testing or result in deviations in protocols (11, 43).
Knee OA has been associated with lower leg power within older adults with the disease and in comparison to older adults without disease. Robertson et al. (29) assessed leg power and function of patients waiting for a primary unilateral knee replacement for OA. Unilateral leg press power (Nottingham power rig) was measured on affected and unaffected legs within seven days to assess reliability. Without pain adjustments, affected legs had lower power than unaffected legs with 9% CV for both legs (p< 0.05). Barker et al. (44) measured leg power among 123 patients with clinical knee OA diagnoses. Unilateral leg extension power (Nottingham power rig) was measured in the more symptomatic leg. The difference between leg power of patients with and without knee OA was not statistically analyzed. However, patients with knee OA had 75% lower leg power compared to a general population aged > 65 years (49) and 55% lower leg power compared to frail, older nursing home residents (0.46 W/kg vs. 1.81 W/kg vs. 1.02 W/kg) (50). These results indicate the dramatic effect that OA has on lower leg power in older adults.
More severe OA also is related to lower leg power. Juhakoski et al. (45) assessed the association between leg power, self-reported pain, and physical function in 118 older adults with hip OA. The Western Ontario and McMaster Osteoarthritis Index (WOMAC), a standardized questionnaire assessment of health status, was used to measure pain, stiffness, and physical function disability (51). Unilateral leg extensor power (Concept II dynamometer), normalized by body weight, negatively correlated with the WOMAC pain scale (r= −0.191, p< 0.05), WOMAC function scale (r= −0.277, p< 0.01), and positively with the RAND 36-Item Short-Form Health Survey of self-reported physical function (r= 0.256, p< 0.01). Berger et al. (46) investigated load-velocity and load-power relationships among participants with varying severity of knee OA and the association with self-reported function. Leg power was assessed, across a series of submaximal loads at maximum velocity, during unilateral concentric knee extensions (isotonic mode of Biodex System III dynamometer). Functional ability was measured with the WOMAC function subscale. Leg power among older adults with knee OA predicted a greater variance in function at lower loads and maximum velocity. Power measured without loading (minimum resistance) and 20% maximal voluntary isometric contraction explained the greatest variances in function (28%, p< 0.001 and 22%, p< 0.002). The study found that leg power was reduced across a functional spectrum of knee OA and individuals with higher WOMAC scores (more severe pain, stiffness, functional limitations) have even lower power comparatively.
Encouragingly, exercise intervention trials among older adults with and without OA have shown positive power improvements in both groups (47, 48). Sayers et al. compared muscle performance measures (strength, power, and speed) of community-dwelling older adults with (48) and without OA (47) across two studies. Participants were randomized to high-speed power training, slow-speed strength training, or a control group. Unilateral, concentric leg extensor power (Keiser pneumatic leg press) was measured at baseline and post-training. Significant improvements were found in leg power, after high-speed power training and slow-speed strength training, among older adults with and without OA (p< 0.05 and p< 0.001, respectively). Therefore, older adults with OA were found to be responsive to exercise programs and capable of improving leg power similarly to those without OA.
In conclusion, OA is strongly associated with reduced leg power among older adults and exercise intervention programs improve leg power similarly among older adults with and without OA. However, most studies of the relationship between OA and leg power are cross-sectional and many of these do not include older adults without OA. Future studies may better evaluate leg power among older adults with and without OA by using weight-bearing condition tests such as force plate ergometry and considering multiple joints and muscle groups.
Diabetes Mellitus (DM)
According to the Centers for Disease Control and Prevention, 10.9 million (26.9%) individuals in the United States aged ≥ 65 years or older have DM (52). A large increase in prevalence among those ≥ 75 years is expected in the future due to the diabetes epidemic and the rising number of older adults (53). Disability is approximately two to three times greater in diabetic older adults than those without DM (19). Type 2 DM may result in lower muscle mass and quality, defined by muscle strength per unit of muscle mass (18, 54). This ultimately may be related to an increased incidence of functional disability, especially in lower-extremity mobility tasks (15, 55). Approximately 60–70% of diabetic men and women have mild to severe forms of nervous system diseases such as peripheral neuropathy (PN) (56), which may additionally have a detrimental effect on muscle function, independent of muscle mass and quality (57). Poor peripheral nerve function among diabetic individuals is associated with worse physical performance, including gait speed, chair rise speed, muscle strength, and subclinical functional limitations, an indicator of early functional decline (58, 59).
Muscle power may better represent the neural component of muscle function since it incorporates velocity of movement, which is dependent on neural inputs (12, 60), and this is likely critical for impairments in older diabetic adults. Hilton et al. (61) studied leg power in individuals with obesity, DM, and PN, and corresponding healthy age- and sex- matched controls. Concentric isokinetic and isometric ankle plantar-flexor and ankle dorsiflexor power (Biodex Multi-joint System III Pro isokinetic dynamometer) was assessed. Obese participants with chronic DM and PN had lower ankle dorsiflexor power (83–86%) and ankle plantar-flexor power (73–77%, p< 0.05). However, the study was limited by the inability to separate the potential effects of obesity, DM, and PN.
Significant findings related DM to lower leg power in two cross-sectional analyses of large aging cohort studies (62, 63). Volpato et al. (62) noted significantly lower unilateral leg extension power (Nottingham power rig) among older adults with DM on pharmacological therapy compared to those without DM after adjusting for age and sex (−12.7 ± 5.2 W vs. 65.8 ± 1.8 W, p< 0.05). Kalyani et al. (63) assessed maximum voluntary concentric muscle force of the right knee extensor muscle (Kin-Com isokinetic dynamometer) with leg power calculated at peak quadriceps force in a cohort of 2573 adults aged > 50 years. Diabetic adults had lower leg power than non-diabetic older adults after adjustment for demographics and anthropometry (−4.9 ± 2.0 W, p= 0.02).
Importantly, training has shown to improve leg power in older diabetic adults. Sacchetti et al. (64) assessed knee extensor torque (Kin-Com isokinetic dynamometer) during maximal contractions at different angular velocities in non-diabetic sedentary control subjects, sedentary diabetic patients in the first (lower) quartile and fourth (higher) quartile of peroneal motor nerve conduction velocity, and trained diabetic adults (n=12 each). Older sedentary adults with DM had lower leg power than non-diabetic sedentary controls and older adults with DM that had been trained. Values of strength and power were similar between trained diabetic older adults and healthy sedentary controls, indicating that the lower leg power in older adults with DM may be improved with training interventions.
As further evidence of improvements with training, Ibanez et al. (65) compared leg power improvements of older sedentary men with type 2 DM to an age-matched, healthy control group after a progressive resistance training program. Weight-bearing leg power was assessed by lifting a bar in contact with the shoulders from a 90° knee angle to a full extension of 180° (half-squat). External load was set to 30% of a participant’s one repetition maximum and power was assessed at 4 weeks before training, baseline, and post-training. Post-training gains were found in leg power among control participants (323.5 ± 122.1 W vs. 394.4 ± 147.2 W, p< 0.001) and diabetic participants (239.5 ± 53.9 W vs. 312.3 ± 52.8 W, p< 0.01), yet no significant post-training difference was observed between the non-diabetic and diabetic men (34.2% ± 32.0% vs 33.0% ± 21.2%). This indicates that older adults with DM can improve leg power similarly to those without DM and that training may be a feasible intervention to address lower leg power in older diabetic adults.
These collective results consistently found lower leg power among older adults with DM in comparison to those without DM. Leg power was improved with training and may be a feasible intervention for older adults with DM. However, temporal or causal relationships were difficult to determine in the cross-sectional study designs and the training studies were very small with a lack of extensive longitudinal follow-up to determine the long term effect of the training.
Cardiovascular Disease (CVD)
CVD (myocardial infarction, coronary artery disease, heart failure, peripheral vascular disease (PVD), and hypertension) is responsible for one in three reported deaths in the United States each year (66, 67). CVD is a prominent cause of disability (67) and is frequently associated with reduced aerobic endurance, changes in body composition, bone loss, skeletal muscle atrophy, and weakness in older adults (21).
Suzuki et al. (23) assessed the relationship between muscle strength, muscle endurance, and cardiopulmonary parameters in 33 outpatients with stable chronic heart failure (CHF). CHF is associated with restrictions in peak blood flow to exercising muscle (73–75). The cardiopulmonary measures of peak oxygen uptake and anaerobic threshold are representative of skeletal muscle blood flow in patients with CHF. A pedal-type device (StrengthErgo240) measured isokinetic peak muscle power. Peak muscle power had significant correlations with peak oxygen uptake (r= 0.66, p< 0.001), anaerobic threshold (r= 0.42, p= 0.0124), and increase in oxygen uptake relative to change in work rate (r= 0.43, p= 0.0128). However, further investigation including a comparison to older adults without CHF is needed to better elucidate the relationship between muscle power and CHF.
McDermott et al. (68) measured unilateral leg extensor power (Nottingham power rig) in a cohort of men and women aged > 60 years with and without PVD. Older adults with lower extremity PVD had 19% lower leg power compared to those without PVD (83.69 W vs. 103.51 W, p< 0.001). Another study performed by McDermott et al. (69) that similarly measured leg power among older men and women with and without PVD found those with PVD had 20% lower leg power than those without PVD (93.49 ± 52.73 W vs. 117.17 ± 68.6 W, p< 0.001) even after adjusting for many variables including age, sex, race, comorbidities, body mass index, smoking history, leg symptoms, and recruitment cohort. These findings indicate that PVD is independently associated with lower leg power in older adults.
Higher mortality has also been associated with lower leg power among older adults. McDermott et al. (70) noted lower unilateral, leg extension power (Nottingham power rig) predicted higher all-cause mortality (p= 0.004) over a 4 year follow-up, after adjusting for age, sex, and race, in 434 participants with PVD. Deceased men had 24% lower baseline leg power than surviving men (94.49 ± 51.0 vs. 123.9 ± 52.1; p< 0.001) and deceased women had 20% lower leg power than surviving women (53.84 ± 30.7 vs. 67.65 ± 33.7, p= 0.04). Takata et al. (71) found isokinetic leg extension power (Aneropress 3500) to be significantly lower in the deceased participants after a 4 year follow-up for mortality outcomes. In men, but not women, baseline leg power was 13% lower in the non-surviving men (440.3 ± 144.9 W vs. 505.3 ± 184.6 W, p= 0.0434). No significant difference existed in isokinetic baseline leg power for those with CVD death compared to surviving men or women, however only 27/107 deaths were due to CVD. Therefore, lower leg power may predict mortality in older adults, with possibly a stronger effect among those with PVD.
Little research exists on training programs to improve leg power among older adults with CVD. Saunders et al. (72) assessed baseline, cross-sectional data from an exercise, randomized controlled trial of participants after a stroke. Unilateral leg power (Nottingham power rig) measured during hip and knee extension was not related to cardiovascular comorbidities (ischemic heart disease, left ventricular failure, hypertension). However, the homogeneity of the sample (high functioning, independently ambulatory subjects with stroke) may have limited the ability to find associations and further CVD populations should be studied.
Overall, muscle power was found to be lower among individuals with PVD. However, restrictive eligibility criteria and lack of diversity among the CVD populations studied limited findings. Additional well-designed longitudinal studies are needed to determine if and to what extent leg muscle power is related to cardiovascular disease. Importantly, training interventions should be evaluated to determine if the lower leg power among older adults with CVD may be improved and also if this higher leg power is associated with a corresponding decrease in CVD outcomes.
Conclusion
This review found OA, DM, and CVD to be associated with low muscle power to a variable degree among older adults. However, a limited amount of literature exists to determine a clear, causal relationship. Strong initial evidence exists for OA and DM associations with lower leg power and also that training may improve leg power in these groups. Inconsistent definitions of CVD across studies made it difficult to evaluate relationships and subsequently produced the least conclusive results, though PVD was consistently associated with lower leg power. Overall, cross-sectional analyses, small sample sizes, self-reported and varied disease definitions for OA, DM and CVD, lack of consideration for other disease-related comorbidities in analyses, and unrepresentative study populations of older adults were weaknesses of the 16 leg power studies in this review.
In addition, the number of the leg power methods used challenged the direct comparison of results across studies. The 16 studies in this review used 6 different measures of leg power. Five of the 16 studies used isokinetic dynamometer power measurements, which are not an ideal technique. Isokinetic devices measure force under constant velocity from very slow (i.e. 30 degrees/s) to very fast (i.e. 240 degrees/s) velocities and the selected velocities varied across studies. Seven of the studies in this review measured leg power with the Nottingham power rig and the Keiser pneumatic leg press was used once (76, 77). These measures involve unilateral or bilateral leg extension movements performed at maximum velocity in a seated position (32). The Nottingham power rig is a common and reproducible measure for power assessment (32, 78). Similarly, the Keiser leg press has been validated with high reproducibility in older adults (11, 43, 79, 80), although, one-repetition maximum measurements are required prior to power measurements. Obtaining a one repetition maximum in older adults with comorbidities associated with chronic pain and disability may be problematic methodologically (11, 43, 79, 81). Two additional dynamometers (Concept II and Biodex system III) measured leg extensor power in seated positions with a fixed load. Although the isotonic mode of the Biodex system III is reliable among younger populations (82) and the Concept II is considered comparable to the Nottingham power rig (45), these are less common measure among older adults. Only one study utilized a weight-bearing measure (half-squat test) (65). Nevertheless, performance-based techniques (i.e. jumping mechanography, sit-to-stand test methods, box-stepping tests, two-revolution maximum test) may also be important (33–35, 65). Force plate ergometry provides accurate measurements of force and velocity through the assessment of ground reaction force and individuals may be more capable of moving their own body weight in lieu of an external resistance. Much greater methodologic focus needs to be applied to studies of chronic disease and leg power in older adults, in order to determine which test is the most feasible and appropriate for certain conditions.
Not only is the identification of a simple, standard measurement of leg muscle power essential for future research in older adults with chronic disease, but importantly may vary depending on the condition being considered. Furthermore, differences in tests for specific joints and muscles (i.e. hip and knee) must be evaluated. Other disease-related comorbidities should also be carefully adjusted for across the reviewed diseases, to ensure that primary relationships are not explained by these. Although it may be impossible to truly attenuate the effects of aging, the benefits of physical activity and training programs should be evaluated in preventing or controlling for leg power decline in older adults with chronic disease (64). Several studies suggested that exercise training may attenuate the effect of chronic disease on lower leg power in older adults and further work is necessary to determine the timing and mechanism of these associations for each disease. Since the leg power and chronic disease relationship may be critical to preventing disability in older adults, future research should focus on larger studies of diverse older adults with well-defined chronic disease, utilize standard measures of leg power determined to be the most appropriate for the study population, and evaluate interventions to improve leg power in older adults with these chronic diseases.
Table 1.
Summary of studies examining the relationship between leg power and osteoarthritis in older adults
| Authors | Participants | Mean Age ± SD (years) | Design | Leg Power Measure | Findings |
|---|---|---|---|---|---|
| Robertson et al. 1998 (29) | 26 patients waiting for a primary unilateral knee replacement | 72 ± 8 | Cross-sectional | Nottingham power rig | ↓ leg power in affected leg |
| Barker et al. 2004 (44) | 123 patients with clinical knee OA diagnosis | 69.5 ± 8.1 | Cross-sectional | Nottingham power rig | ↓ leg power in adults with knee OA diagnosis |
| Juhakoski et al. 2008 (45) | 118 men (n=35) and women (n=83) with hip OA | 66.7 ± 6.5 | Cross-sectional | Concept II dynamometer | Leg power predicts physical function better than pain with hip OA |
| Berger et al. 2012 (46) | 40 community-dwelling men (n=21) and women (n=19) with knee OA | 60.7 ± 6 | Cross-sectional | Biodex system III isotonic dynamometer | ↓ leg power is associated with ↑ functional deficit in older adults with knee OA |
| Sayers et al. 2010, 2012 (47, 48) | 33 community-dwelling older adults with an OA diagnosis and 38 healthy community dwelling older adults without an OA diagnosis33 | OA diagnosis (67.6 ± 6.8) Without OA diagnosis (HSPT: 74.1 ± 6.4 years, SSST: 70.1 ± 7.0, CON: 72.8 ± 4.1) |
Randomized controlled trial (power training intervention) | Keiser pneumatic leg press | ↑ in leg power was similar among older adults with and without a diagnosis of knee OA33 |
OA= Osteoarthritis; HSPT= High-Speed Power Training; SSST= Slow-Speed Strength Training; CON= Control
Table 2.
Summary of studies examining the relationship between leg power and diabetes mellitus in older adults
| Authors | Participants | Mean Age ± SD (years) | Design | Leg Power Measure | Findings |
|---|---|---|---|---|---|
| Hilton et al. 2008 (61) | 6 obese participants with DM and PN and their 6 age- and sex-matched controls | Obese participants (58 ± 10) Controls (58 ± 9.2) |
Cross-sectional | Biodex Multi-joint System III Pro isokinetic dynamometer | ↓ leg power among obese participants with DM and PN |
| Volpato et al. 2012 (62) | 835 community-dwelling adults (11.4% with DM diagnosis) | With DM (73.8 ± 6.5) Without DM (73.9 ± 6.2) |
Cross-sectional analysis of InCHIANTI cohort | Nottingham power rig | ↓ leg power among participants with DM |
| Kalyani et al. 2013 (63) | 2573 adults aged ≥ 50 years (321 with DM diagnosis) | 63.3 ± 0.3 | Cross-sectional | Kin-Com isokinetic dynamometer | ↓ leg power among participants with DM |
| Sacchetti et al. 2013 (64) | Four groups (n=12 each) consisting of sedentary DM adults (DM1 and DM4), trained DM adults, and non-DM sedentary controls | Sedentary DM1 (60.0 ± 10.7), Sedentary DM4 (58.2 ± 17.5), trained DM adults (61.8 ± 19.4), control (62.5 ± 4.0) | Cross-sectional | Kin-Com isokinetic dynamometer | ↓ leg power among sedentary, but not trained participants with DM |
| Ibanez et al. 2008 (65) | 9 Type 2 DM, older sedentary men and 11 age-matched controls | DM (66.6 ± 3.1) Non-DM adults (64.8 ± 2.6) |
Cross-sectional (resistance training program) | Half-squat test | Leg power gains were similar among participants with and without DM |
DM= Diabetes Mellitus; PN= Peripheral Neuropathy; InCHIANTI= Invecchiare in Chianti, Aging in the Chianti Area; DM1= Sedentary DM in 1st Quartile of MNCV; DM4= Sedentary DM in 4th Quartile of MNCV; MNCV= Motor Nerve Conduction Velocity
Table 3.
Summary of studies examining the relationship between leg power and cardiovascular disease in older adults
| Authors | Participants | Mean Age ± SD (years) | Design | Leg Power Measure | Findings |
|---|---|---|---|---|---|
| Suzuki et al. 2004 (23) | 33 male (n=27) and female (n=6) outpatients with stable CHF | 60.3 ± 12.7 | Cross-sectional | StrengthErgo240 pedal type isokinetic device | Leg power is significantly and positively correlated with peak VO2, anaerobic threshold and an increase in oxygen uptake relative to change in work rate |
| McDermott et al. 2004 (68) | 979 community-dwelling men and women aged 60 years and older with (n=109) and without PVD | With PVD (78.27) Without PVD (73.78) |
Cross-sectional analysis of InCHIANTI cohort | Nottingham power rig | ↓ leg power in the lower extremities among participants with PVD |
| McDermott et al. 2008 (69) | 424 participants with PVD and 271 participants without PVD |
With PVD (71.39 ± 7.56) Without PVD (74.97 ± 8.24) |
Cross-sectional | Nottingham power rig | ↓ leg power among participants with PVD |
| McDermott et al. 2012 (70) | 434 participants with PVD | 75 ± 8.2 | Longitudinal mortality outcome | Nottingham power rig | ↓ leg power was associated with higher all-cause mortality among participants with PVD |
| Takata et al. 2007 (71) | 697 Japanese men (n=277) and women (n=420) | 80 | Longitudinal mortality outcome (4 year) | Isokinetic dynamometer | No significant difference was found between leg power and mortality due to CVD in men or women |
| Saunders et al. 2008 (72) | 66 community-dwelling and independently ambulatory men and women with after a stroke | 72.10 ± 9.91 | Cross-sectional baseline data from an exercise randomized controlled trial | Nottingham power rig | CVD comorbidities were not found to be predictive of leg power |
CHF= Chronic Heart Failure; CVD= Cardiovascular Disease; PVD= Peripheral Vascular Disease; VO2= Oxygen Uptake; InCHIANTI= Invecchiare in Chianti, Aging in the Chianti Area
Acknowledgments
Funding: This work was supported by the Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant – NIH P30 AG024826 and NIH P30 AG024827; National Institute on Aging Professional Services Contract HHSN271201100605P; NIA Aging Training Grant T32 AG000181; and by the Intramural Research Program of the National Institute on Aging.
Conflicts of Interest: Ms. Strollo reports grants from National Institutes of Health (NIH); Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant, grants from National Institute on Aging Professional Services Contract, grants from National Institute on Aging Training Grant, other from National Institute on Aging Intramural Research Program, during the conduct of the study. Dr. Caserotti has nothing to disclose. Dr. Ward reports grants from National Institutes of Health (NIH); Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant, grants from National Institute on Aging Professional Services Contract, grants from National Institute on Aging Training Grant, other from National Institute on Aging Intramural Research Program, grants from The National Institute on Disability and Rehabilitation Research, during the conduct of the study. Dr. Glynn reports grants from National Institutes of Health (NIH); Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant, grants from National Institute on Aging Professional Services Contract, grants from National Institute on Aging Training Grant, other from National Institute on Aging Intramural Research Program, during the conduct of the study. Dr. Goodpaster has nothing to disclose. Dr. Strotmeyer reports grants from National Institutes of Health (NIH); Pittsburgh Claude D. Pepper Older Americans Independence Center, Research Registry, and Developmental Pilot Grant, grants from National Institute on Aging Professional Services Contract, grants from National Institute on Aging Training Grant, other from National Institute on Aging Intramural Research Program, during the conduct of the study.
Contributor Information
S.E. STROLLO, Email: sara.strollo@nih.gov.
P. CASEROTTI, Email: pcaserotti@health.sdu.dk.
R.E. WARD, Email: rew27@bu.edu.
N.W. GLYNN, Email: glynnn@edc.pitt.edu.
B.H. GOODPASTER, Email: bgoodpaster@sanfordburnham.org.
E.S. STROTMEYER, Email: strotmeyere@edc.pitt.edu.
References
- 1.Bean JF, Kiely DK, Herman S, Leveille SG, Mizer K, Frontera WR, et al. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50:461–467. doi: 10.1046/j.1532-5415.2002.50111.x. [DOI] [PubMed] [Google Scholar]
- 2.Evans WJ. Exercise strategies should be designed to increase muscle power. J Gerontol A Biol Sci Med Sci. 2000;55:M309–310. doi: 10.1093/gerona/55.6.m309. [DOI] [PubMed] [Google Scholar]
- 3.Skelton DA, Kennedy J, Rutherford OM. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing. 2002;31:119–125. doi: 10.1093/ageing/31.2.119. [DOI] [PubMed] [Google Scholar]
- 4.Caserotti P, Aagaard P, Larsen JB, Puggaard L. Explosive heavy-resistance training in old and very old adults: changes in rapid muscle force, strength and power. Scand J Med Sci Sports. 2008;18:773–782. doi: 10.1111/j.1600-0838.2007.00732.x. [DOI] [PubMed] [Google Scholar]
- 5.Warburton DE, Gledhill N, Quinney A. Musculoskeletal fitness and health. Can J Appl Physiol. 2001;26:217–237. doi: 10.1139/h01-013. [DOI] [PubMed] [Google Scholar]
- 6.Edgerton VR, Roy RR, Gregor RJ, Rugg S. Morphological basis of skeletal muscle power output. In: Jones NL, McCartney N, McComas AJ, editors. Human muscle power. Champaign, IL: Human Kinetics; 1986. [Google Scholar]
- 7.Kraemer WJ, Newton RU. Training for muscular power. Phys Med Rehabil Clin N Am. 2000;11:341–368. vii. [PubMed] [Google Scholar]
- 8.Caserotti P, Harris TB, Vannozzi G, Aagaard P. Assessment of muscle power in older adults and association with functional performance. Gerontologist. 2009;49:210. [Google Scholar]
- 9.Jakobi JM, Rice CL. Voluntary muscle activation varies with age and muscle group. J Appl Physiol. 2002;93:457–462. doi: 10.1152/japplphysiol.00012.2002. [DOI] [PubMed] [Google Scholar]
- 10.Klass M, Baudry S, Duchateau J. Age-related decline in rate of torque development is accompanied by lower maximal motor unit discharge frequency during fast contractions. J Appl Physiol. 2008;104:739–746. doi: 10.1152/japplphysiol.00550.2007. [DOI] [PubMed] [Google Scholar]
- 11.Foldvari M, Clark M, Laviolette LC, Bernstein MA, Kaliton D, Castaneda C, et al. Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55:M192–199. doi: 10.1093/gerona/55.4.m192. [DOI] [PubMed] [Google Scholar]
- 12.Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40:4–12. doi: 10.1097/JES.0b013e31823b5f13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention and The Merck Company Foundation. The State of Aging and Health in America 2007. Whitehouse Station, NJ: The Merck Company Foundation; 2007. [Google Scholar]
- 14.Brochu M, Savage P, Lee M, Dee J, Cress ME, Poehlman ET, et al. Effects of resistance training on physical function in older disabled women with coronary heart disease. J Appl Physiol. 2002;92:672–678. doi: 10.1152/japplphysiol.00804.2001. [DOI] [PubMed] [Google Scholar]
- 15.Gregg EW, Mangione CM, Cauley JA, Thompson TJ, Schwartz AV, Ensrud KE, et al. Diabetes and incidence of functional disability in older women. Diabetes Care. 2002;25:61–67. doi: 10.2337/diacare.25.1.61. [DOI] [PubMed] [Google Scholar]
- 16.Hunter DJ, Felson DT. Osteoarthritis. BMJ. 2006;332:639–642. doi: 10.1136/bmj.332.7542.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haq I, Murphy E, Dacre J. Osteoarthritis. Postgrad Med J. 2003;79:377–383. doi: 10.1136/pmj.79.933.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park SW, Goodpaster BH, Strotmeyer ES, de Rekeneire N, Harris TB, Schwartz AV, et al. Decreased muscle strength and quality in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes. 2006;55:1813–1818. doi: 10.2337/db05-1183. [DOI] [PubMed] [Google Scholar]
- 19.Gregg EW, Beckles GL, Williamson DF, Leveille SG, Langlois JA, Engelgau MM, et al. Diabetes and physical disability among older U.S. adults. Diabetes Care. 2000;23:1272–1277. doi: 10.2337/diacare.23.9.1272. [DOI] [PubMed] [Google Scholar]
- 20.Andersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes. 2004;53:1543–1548. doi: 10.2337/diabetes.53.6.1543. [DOI] [PubMed] [Google Scholar]
- 21.Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85:S31–44. doi: 10.1016/j.apmr.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Brum PC, Bacurau AV, Medeiros A, Ferreira JC, Vanzelli AS, Negrao CE. Aerobic exercise training in heart failure: impact on sympathetic hyperactivity and cardiac and skeletal muscle function. Braz J Med Biol Res. 2011;44:827–835. doi: 10.1590/s0100-879x2011007500075. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki K, Omiya K, Yamada S, Kobayashi T, Suzuki N, Osada N, et al. Relations between strength and endurance of leg skeletal muscle and cardiopulmonary exercise testing parameters in patients with chronic heart failure. J Cardiol. 2004;43:59–68. [PubMed] [Google Scholar]
- 24.Farinon AM, Marbini A, Gemignani F, Govoni E, Bragaglia MM, Sianesi M, et al. Skeletal muscle and peripheral nerve changes caused by chronic arterial insufficiency–significance and clinical correlations–histological, histochemical and ultrastructural study. Clin Neuropathol. 1984;3:240–252. [PubMed] [Google Scholar]
- 25.Hedberg B, Angquist KA, Henriksson-Larsen K, Sjostrom M. Fibre loss and distribution in skeletal muscle from patients with severe peripheral arterial insufficiency. Eur J Vasc Surg. 1989;3:315–322. doi: 10.1016/s0950-821x(89)80067-2. [DOI] [PubMed] [Google Scholar]
- 26.Dieppe P. Strategies for the prevention of osteoarthritis. Int J Tissue React. 1993;15:93–97. [PubMed] [Google Scholar]
- 27.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 28.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% BMJ. 2003;326:1419. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robertson S, Frost H, Doll H, O’Connor JJ. Leg extensor power and quadriceps strength: an assessment of repeatability in patients with osteoarthritic knees. Clin Rehabil. 1998;12:120–126. doi: 10.1191/026921598673072472. [DOI] [PubMed] [Google Scholar]
- 30.De Vito G, Bernardi M, Forte R, Pulejo C, Macaluso A, Figura F. Determinants of maximal instantaneous muscle power in women aged 50–75 years. Eur J Appl Physiol Occup Physiol. 1998;78:59–64. doi: 10.1007/s004210050387. [DOI] [PubMed] [Google Scholar]
- 31.Macaluso A, De Vito G. Comparison between young and older women in explosive power output and its determinants during a single leg-press action after optimisation of load. Eur J Appl Physiol. 2003;90:458–463. doi: 10.1007/s00421-003-0866-7. [DOI] [PubMed] [Google Scholar]
- 32.Bassey EJ, Short AH. A new method for measuring power output in a single leg extension: feasibility, reliability and validity. Eur J Appl Physiol Occup Physiol. 1990;60:385–390. doi: 10.1007/BF00713504. [DOI] [PubMed] [Google Scholar]
- 33.Forte R, Macaluso A. Relationship between performance-based and laboratory tests for lower-limb muscle strength and power assessment in healthy older women. J Sports Sci. 2008;26:1431–1436. doi: 10.1080/02640410802208994. [DOI] [PubMed] [Google Scholar]
- 34.Alexander NB, Galecki AT, Grenier ML, Nyquist LV, Hofmeyer MR, Grunawalt JC, et al. Task-specific resistance training to improve the ability of activities of daily living-impaired older adults to rise from a bed and from a chair. J Am Geriatr Soc. 2001;49:1418–1427. doi: 10.1046/j.1532-5415.2001.4911232.x. [DOI] [PubMed] [Google Scholar]
- 35.Caserotti P, Aagaard P, Simonsen EB, Puggaard L. Contraction-specific differences in maximal muscle power during stretch-shortening cycle movements in elderly males and females. Eur J Appl Physiol. 2001;84:206–212. doi: 10.1007/s004210170006. [DOI] [PubMed] [Google Scholar]
- 36.Kuo HK, Leveille SG, Yen CJ, Chai HM, Chang CH, Yeh YC, et al. Exploring how peak leg power and usual gait speed are linked to late-life disability: data from the National Health and Nutrition Examination Survey (NHANES), 1999–2002. Am J Phys Med Rehabil. 2006;85:650–658. doi: 10.1097/01.phm.0000228527.34158.ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Orr R, Tsang T, Lam P, Comino E, Singh MF. Mobility impairment in type 2 diabetes: association with muscle power and effect of Tai Chi intervention. Diabetes Care. 2006;29:2120–2122. doi: 10.2337/dc06-1130. [DOI] [PubMed] [Google Scholar]
- 38.Sayers SP. High-speed power training: a novel approach to resistance training in older men and women. A brief review and pilot study. J Strength Cond Res. 2007;21:518–526. doi: 10.1519/R-20546.1. [DOI] [PubMed] [Google Scholar]
- 39.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54:226–229. doi: 10.1002/art.21562. [DOI] [PubMed] [Google Scholar]
- 40.American Geriatrics Society Panel on Exercise and Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc. 2001;49:808–823. doi: 10.1046/j.1532-5415.2001.00496.x. [DOI] [PubMed] [Google Scholar]
- 41.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 42.Andersen H, Gadeberg PC, Brock B, Jakobsen J. Muscular atrophy in diabetic neuropathy: a stereological magnetic resonance imaging study. Diabetologia. 1997;40:1062–1069. doi: 10.1007/s001250050788. [DOI] [PubMed] [Google Scholar]
- 43.Fielding RA, LeBrasseur NK, Cuoco A, Bean J, Mizer K, Fiatarone Singh MA. High-velocity resistance training increases skeletal muscle peak power in older women. J Am Geriatr Soc. 2002;50:655–662. doi: 10.1046/j.1532-5415.2002.50159.x. [DOI] [PubMed] [Google Scholar]
- 44.Barker K, Lamb SE, Toye F, Jackson S, Barrington S. Association between radiographic joint space narrowing, function, pain and muscle power in severe osteoarthritis of the knee. Clin Rehabil. 2004;18:793–800. doi: 10.1191/0269215504cr754oa. [DOI] [PubMed] [Google Scholar]
- 45.Juhakoski R, Tenhonen S, Anttonen T, Kauppinen T, Arokoski JP. Factors affecting self-reported pain and physical function in patients with hip osteoarthritis. Arch Phys Med Rehabil. 2008;89:1066–1073. doi: 10.1016/j.apmr.2007.10.036. [DOI] [PubMed] [Google Scholar]
- 46.Berger MJ, McKenzie CA, Chess DG, Goela A, Doherty TJ. Quadriceps neuromuscular function and self-reported functional ability in knee osteoarthritis. J Appl Physiol. 2012;113:255–262. doi: 10.1152/japplphysiol.00947.2011. [DOI] [PubMed] [Google Scholar]
- 47.Sayers SP, Gibson K. A comparison of high-speed power training and traditional slow-speed resistance training in older men and women. J Strength Cond Res. 2010;24:3369–3380. doi: 10.1519/JSC.0b013e3181f00c7c. [DOI] [PubMed] [Google Scholar]
- 48.Sayers SP, Gibson K, Cook CR. Effect of high-speed power training on muscle performance, function, and pain in older adults with knee osteoarthritis: a pilot investigation. Arthritis Care Res (Hoboken) 2012;64:46–53. doi: 10.1002/acr.20675. [DOI] [PubMed] [Google Scholar]
- 49.Health Education Authority and Sports Council. Allied Dunbar National Fitness Survey: main findings. Northampton: Belmont Press; 1992. [Google Scholar]
- 50.Bassey EJ, Fiatarone MA, O’Neill EF, Kelly M, Evans WJ, Lipsitz LA. Leg extensor power and functional performance in very old men and women. Clin Sci (Lond) 1992;82:321–327. doi: 10.1042/cs0820321. [DOI] [PubMed] [Google Scholar]
- 51.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 53.Centers for Disease Control and Prevention. Public health and aging: trends in aging–United States and worldwide. JAMA. 2003;289:1371–1373. [PubMed] [Google Scholar]
- 54.Park SW, Goodpaster BH, Strotmeyer ES, Kuller LH, Broudeau R, Kammerer C, et al. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes Care. 2007;30:1507–1512. doi: 10.2337/dc06-2537. [DOI] [PubMed] [Google Scholar]
- 55.Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Diabetes Care. 2010;33:1055–1060. doi: 10.2337/dc09-1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States. Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 2005. [Google Scholar]
- 57.Strotmeyer ES, de Rekeneire N, Schwartz AV, Resnick HE, Goodpaster BH, Faulkner KA, et al. Sensory and motor peripheral nerve function and lower-extremity quadriceps strength: the health, aging and body composition study. J Am Geriatr Soc. 2009;57:2004–2010. doi: 10.1111/j.1532-5415.2009.02487.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Strotmeyer ES, de Rekeneire N, Schwartz AV, Faulkner KA, Resnick HE, Goodpaster BH, et al. The relationship of reduced peripheral nerve function and diabetes with physical performance in older white and black adults: the Health, Aging, and Body Composition (Health ABC) study. Diabetes Care. 2008;31:1767–1772. doi: 10.2337/dc08-0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.De Rekeneire N, Resnick HE, Schwartz AV, Shorr RI, Kuller LH, Simonsick EM, et al. Diabetes is associated with subclinical functional limitation in nondisabled older individuals: the Health, Aging, and Body Composition study. Diabetes Care. 2003;26:3257–3263. doi: 10.2337/diacare.26.12.3257. [DOI] [PubMed] [Google Scholar]
- 60.Hakkinen K, Kallinen M, Izquierdo M, Jokelainen K, Lassila H, Malkia E, et al. Changes in agonist-antagonist EMG, muscle CSA, and force during strength training in middle-aged and older people. J Appl Physiol (1985) 1998;84:1341–1349. doi: 10.1152/jappl.1998.84.4.1341. [DOI] [PubMed] [Google Scholar]
- 61.Hilton TN, Tuttle LJ, Bohnert KL, Mueller MJ, Sinacore DR. Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Phys Ther. 2008;88:1336–1344. doi: 10.2522/ptj.20080079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Volpato S, Bianchi L, Lauretani F, Lauretani F, Bandinelli S, Guralnik JM, et al. Role of muscle mass and muscle quality in the association between diabetes and gait speed. Diabetes Care. 2012;35:1672–1679. doi: 10.2337/dc11-2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kalyani RR, Tra Y, Yeh HC, Egan JM, Ferrucci L, Brancati FL. Quadriceps strength, quadriceps power, and gait speed in older U.S. adults with diabetes mellitus: results from the National Health and Nutrition Examination Survey, 1999–2002. J Am Geriatr Soc. 2013;61:769–775. doi: 10.1111/jgs.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sacchetti M, Balducci S, Bazzucchi I, Carlucci F, Scotto di Palumbo A, Haxhi J, et al. Neuromuscular dysfunction in diabetes: role of nerve impairment and training status. Med Sci Sports Exerc. 2013;45:52–59. doi: 10.1249/MSS.0b013e318269f9bb. [DOI] [PubMed] [Google Scholar]
- 65.Ibanez J, Gorostiaga EM, Alonso AM, Forga L, Arguelles I, Larrion JL, et al. Lower muscle strength gains in older men with type 2 diabetes after resistance training. J Diabetes Complications. 2008;22:112–118. doi: 10.1016/j.jdiacomp.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 66.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McDermott MM. The international pandemic of chronic cardiovascular disease. JAMA. 2007;297:1253–1255. doi: 10.1001/jama.297.11.1253. [DOI] [PubMed] [Google Scholar]
- 68.McDermott MM, Guralnik JM, Albay M, Bandinelli S, Miniati B, Ferrucci L. Impairments of muscles and nerves associated with peripheral arterial disease and their relationship with lower extremity functioning: the InCHIANTI Study. J Am Geriatr Soc. 2004;52:405–410. doi: 10.1111/j.1532-5415.2004.52113.x. [DOI] [PubMed] [Google Scholar]
- 69.McDermott MM, Tian L, Ferrucci L, Liu K, Guralnik JM, Liao Y, et al. Associations between lower extremity ischemia, upper and lower extremity strength, and functional impairment with peripheral arterial disease. J Am Geriatr Soc. 2008;56:724–729. doi: 10.1111/j.1532-5415.2008.01633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McDermott MM, Liu K, Tian L, Guralnik JM, Criqui MH, Liao Y, et al. Calf muscle characteristics, strength measures, and mortality in peripheral arterial disease: a longitudinal study. J Am Coll Cardiol. 2012;59:1159–1167. doi: 10.1016/j.jacc.2011.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Takata Y, Ansai T, Akifusa S, Soh I, Yoshitake Y, Kimura Y, et al. Physical fitness and 4-year mortality in an 80-year-old population. J Gerontol A Biol Sci Med Sci. 2007;62:851–858. doi: 10.1093/gerona/62.8.851. [DOI] [PubMed] [Google Scholar]
- 72.Saunders DH, Greig CA, Young A, Mead GE. Association of activity limitations and lower-limb explosive extensor power in ambulatory people with stroke. Arch Phys Med Rehabil. 2008;89:677–683. doi: 10.1016/j.apmr.2007.09.034. [DOI] [PubMed] [Google Scholar]
- 73.Wilson JR, Wiener DH, Fink LI, Ferraro N. Vasodilatory behavior of skeletal muscle arterioles in patients with nonedematous chronic heart failure. Circulation. 1986;74:775–779. doi: 10.1161/01.cir.74.4.775. [DOI] [PubMed] [Google Scholar]
- 74.Zelis R, Nellis SH, Longhurst J, Lee G, Mason DT. Abnormalities in the regional circulations accompanying congestive heart failure. Prog Cardiovasc Dis. 1975;18:181–199. doi: 10.1016/0033-0620(75)90010-9. [DOI] [PubMed] [Google Scholar]
- 75.Coats AJ, Clark AL, Piepoli M, Volterrani M, Poole-Wilson PA. Symptoms and quality of life in heart failure: the muscle hypothesis. Br Heart J. 1994;72:S36–39. doi: 10.1136/hrt.72.2_suppl.s36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bean J, Herman S, Kiely DK, Callahan D, Mizer K, Frontera WR, et al. Weighted stair climbing in mobility-limited older people: a pilot study. J Am Geriatr Soc. 2002;50:663–670. doi: 10.1046/j.1532-5415.2002.50160.x. [DOI] [PubMed] [Google Scholar]
- 77.Bean JF, Herman S, Kiely DK, Frey IC, Leveille SG, Fielding RA, et al. Increased Velocity Exercise Specific to Task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community-dwelling older women. J Am Geriatr Soc. 2004;52:799–804. doi: 10.1111/j.1532-5415.2004.52222.x. [DOI] [PubMed] [Google Scholar]
- 78.Blackwell T, Cawthon PM, Marshall LM, Brand R. Consistency of leg extension power assessments in older men: the Osteoporotic Fractures in Men (MrOS) Study. Am J Phys Med Rehabil. 2009;88:934–940. doi: 10.1097/PHM.0b013e3181bbddfb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cuoco A, Callahan DM, Sayers S, Frontera WR, Bean J, Fielding RA. Impact of muscle power and force on gait speed in disabled older men and women. J Gerontol A Biol Sci Med Sci. 2004;59:1200–1206. doi: 10.1093/gerona/59.11.1200. [DOI] [PubMed] [Google Scholar]
- 80.Bean JF, Kiely DK, LaRose S, Alian J, Frontera WR. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88:604–609. doi: 10.1016/j.apmr.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 81.Thomas M, Fiatarone MA, Fielding RA. Leg power in young women: relationship to body composition, strength, and function. Med Sci Sports Exerc. 1996;28:1321–1326. doi: 10.1097/00005768-199610000-00017. [DOI] [PubMed] [Google Scholar]
- 82.Power GA, Dalton BH, Rice CL, Vandervoort AA. Reproducibility of velocity-dependent power: before and after lengthening contractions. Appl Physiol Nutr Metab. 2011;36:626–633. doi: 10.1139/h11-068. [DOI] [PubMed] [Google Scholar]


