Abstract
Background: Surgery for infection represents a substantial, although undefined, disease burden in low- and middle-income countries (LMICs). Médecins Sans Frontières–Operations Centre Brussels (MSF-OCB) provides surgical care in LMICs and collects data useful for describing operative epidemiology of surgical need otherwise unmet by national health services. This study aimed to describe the experience of MSF-OCB operations for infections in LMICs. By doing so, the results might aid effective resource allocation and preparation of future humanitarian staff.
Methods: Procedures performed in operating rooms at facilities run by MSF-OCB from July 2008 through June 2014 were reviewed. Projects providing specialty care only were excluded. Procedures for infection were described and related to demographics and reason for humanitarian response.
Results: A total of 96,239 operations were performed at 27 MSF-OCB sites in 15 countries between 2008 and 2014. Of the 61,177 general operations, 7,762 (13%) were for infections. Operations for skin and soft tissue infections were the most common (64%), followed by intra-abdominal (26%), orthopedic (6%), and tropical infections (3%). The proportion of operations for skin and soft tissue infections was highest during natural disaster missions (p<0.001), intra-abdominal infections during hospital support missions (p<0.001) and orthopedic infections during conflict missions (p<0.001).
Conclusion: Surgical infections are common causes for operation in LMICs, particularly during crisis. This study found that infections require greater than expected surgical input given frequent need for serial operations to overcome contextual challenges and those associated with limited resources in other areas (e.g., ward care). Furthermore, these results demonstrate that the pattern of operations for infections is related to nature of the crisis. Incorporating training into humanitarian preparation (e.g., surgical sepsis care, ultrasound-guided drainage procedures) and ensuring adequate resources for the care of surgical infections are necessary components for providing essential surgical care during crisis.
Surgery is an essential component of health systems and is recognized increasingly as a public health priority, particularly in low- and middle-income countries (LMICs) [1–5]. Planning decisions for health systems strengthening through peri-operative capacity improvements must be made from accurate assessments of surgical need [6–8]. Despite this, there is limited appreciation of the burden and distribution of surgical disease in LMICs, particularly among populations disrupted by humanitarian crisis [9,10].
Whereas many humanitarian organizations provide surgical services in low-income settings, the scope and impact of this work is poorly understood [9]. Médecins Sans Frontières (MSF) is a humanitarian assistance organization that provides surgical care to communities in need. Médecins Sans Frontières is divided into five operational centers, each capable of providing surgical care; Operations Centre Brussels (OCB) is one. Médecins Sans Frontières-Operations Centre Brussels operates projects in LMICs affected by crisis. In addition, OCB provides humanitarian assistance to fragile health care systems that are unable to meet the local surgical needs (Table 1). Médecins Sans Frontières-Operations Centre Brussels collects simple operational data routinely from these projects to guide resource allocation. However, the data are also useful for describing operative epidemiology in LMICs and the volume and diversity of surgical need that is otherwise unmet by national health systems.
Table 1.
Countries in Which Médecins Sans Frontières Operations Centre Brussels Provided Surgical Assistance from 2008–2014
| Country |
|---|
| Afghanistan |
| Central African Republic |
| Chad |
| Côte d'Ivoire |
| Democratic Republic of the Congo |
| Haiti |
| India |
| Mali |
| Mauritania |
| Pakistan |
| Philippines |
| Somalia |
| South Sudan |
| Sudan |
| Syria |
Given unhygienic conditions and delayed presentation, a significant proportion of surgical needs in LMICs likely result from infection [5,11]. A number of pathologies and pathogens result in surgical infections; some of these are unique to tropical LMICs, while others are ubiquitous [5,12,13]. In LMICs, surgical infections often result from untreated conditions, such as cellulitis, peptic ulcer disease, typhoid, symptomatic cholelithiasis, and Buruli ulcer [5,14,15]. In addition, individuals in LMICs face substantial barriers to surgical care, making conditions that are usually readily treatable with antibiotics or a minor procedure progress to needing major surgery(s) [16]. Those able to access health care often find facilities without necessary medications, equipment, and staff for provision of safe surgery [17]. Because survival and quality of life after severe surgical infection depends on prompt resuscitation, antibiotics, and operative intervention, a large proportion of individuals with surgical infections may be left with disability or not survive. Subsequently, the surgical disease burden, condition for condition, is significantly greater in LMICs than the rest of the world [5,9,11].
This study aimed to describe the experience of MSF-OCB surgery for infections in LMICs. Understanding this operative epidemiology will aid effective resource allocation and preparation of humanitarian staff likely to care for patients with surgical infections, as well as further characterize unmet surgical needs in LMICs.
Patients and Methods
Ethics
The analysis of routinely collected, de-identified data satisfied criteria for MSF Ethical Review Board exemption. The Johns Hopkins Bloomberg School of Public Health Institutional Review Board provided ethical approval for analysis.
Study design and data collection
This study was a retrospective review of all procedures performed in an operating room in a facility managed by MSF-OCB worldwide. Operations are logged using a standardized Patient Surgical Record (PSR). The PSR was developed by MSF for operational research needs (i.e., guide human and physical resource allocation, financial planning). Therefore, patient-specific clinical data, such as detailed sociodemographic information or imaging, laboratory, or culture results are not recorded. Furthermore, unique patient identifiers are not used, making longitudinal assessment of their operations or outcomes impossible. The PSR variables are: age, gender, American Society of Anesthesia physical status score, condition requiring surgery, procedure(s) performed, operating room time, peri-operative death (death between induction of anesthesia and discharge from the recovery ward), and program site. In addition, brief descriptive notes on cases are occasionally recorded. The PSR is transcribed monthly into a database (Excel, Microsoft, Redmond, WA) and transmitted to MSF-OCB headquarters in Brussels, Belgium. At headquarters, the Surgical, Anesthesia, Gynecology and Emergency Medicine (SAGE) Unit review all data for completeness and accuracy. Discrepancies, missing data, and questions are corrected immediately after reconciliation with program personnel.
Projects focused solely on a single condition (i.e., maternity care, obstetric fistulas, sub-specialty missions) were not included because they do not represent usual operative epidemiology in LMICs. Surgical infections were divided into skin and soft tissue, intra-abdominal, tropical, and orthopedic. Table 2 provides examples of conditions common or endemic in areas in which MSF-OCB provided assistance. Major operations were defined as exploratory laparotomy, thoracotomy, major amputation, extensive debridement, removal of sequester, or hardware removal. Minor operations were defined as simple debridements, incision and drainage, drain placement, peri-anal procedures, curettage for osteomyelitis, and joint washout.
Table 2.
Infections Common or Endemic in Areas in Which Médecins Sans Frontières Operations Centre Brussels Provided Surgical Assistance from 2008–2014
| Skin and soft tissue | Intra-abdominal | Tropical | Orthopedic |
|---|---|---|---|
| Abscess | Appendicitis | Amoebiasis | Hardware infection |
| Benign anorectal conditions | Cholangitis | Buruli and tropical ulcer | Osteomyelitis |
| Diabetic foot infection | Cholecysitis | Cystic echinococcosis | Septic arthritis |
| Necrotizing soft tissue infection | Diverticulitis | Filariasis | |
| Pilonidal disease | Peptic ulcer (Helicobacter pylori) | Helminthiasis | |
| Pyomyositis | Hepatic & splenic abscess | Schistosomiasis | |
| Wound infection | Non-typhoid perforations | Tuberculosis | |
| Tubo-ovarian abscess | Typhoid perforation |
Tuberculosis—often of the breast and abdomen.
Data analysis
Patient Surgical Record data from July 2008 through June 2014 were extracted, combined, and analyzed with descriptive statistics using Stata v13 (StataCorp, College Station, TX). The reason for MSF-OCB assistance for each project was characterized as natural disaster, hospital support, or conflict. Programs dispatched to support fragile LMIC health care systems and not caring for those injured as a result of conflict or natural disasters were considered to be hospital support. There is some overlap between the reasons for assistance. For example, conflict in fragile states often degenerates to protracted complex humanitarian emergencies and fragile health care systems that require hospital support despite no ongoing conflict.
Chi square testing and forward stepwise logistic regression were performed. Regression models adjusted for covariates age, gender, and project to examine the relation between each covariate and having undergone an operation for infection compared with a non-infection procedure.
Results
A total of 96,239 operations were performed at 27 MSF-OCB sites in 15 countries between 2008 and 2014. After excluding sub-specialty missions for reasons described above, there were 61,177 operations of which 7,762 (13%) were for infections.
Operations for skin and soft tissue infections were the most common (64%), followed by intra-abdominal (26%), orthopedic (6%), and tropical infections (3%; Table 3). Infants requiring surgery had more than twice the odds of having a procedure for an infection than did the elderly (adjusted odds ratio [aOR] 2.27, 95% confidence interval [CI] 1.94–2.65). Skin and soft tissue operations were the most common procedure performed in all age groups, except those for injury in children ages 1 to 13 y. Of those requiring surgery, a higher proportion of adolescents and adults underwent an operation for intra-abdominal, orthopedic, and tropical infections compared with infants and children. Males requiring surgery were more likely to undergo a procedure for infection than women (aOR 1.68, 95% CI 1.60–1.76).
Table 3.
Demographic and Site Characteristics of Those Undergoing Operations for Infection at Médecins Sans Frontières Operations Centre Brussels Projects from 2008–2014
| Surgical infections | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All operations | All surgical infections | Skin and soft tissue | Intra-abdominal | Tropical | Orthopedic | |||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Age | ||||||||||||
| <1 y | 905 | (1) | 282 | (4) | 264 | (5) | 14 | (1) | 1 | (0) | 3 | (1) |
| 1–12 y | 9,776 | (16) | 1,769 | (23) | 1,265 | (25) | 287 | (14) | 69 | (27) | 148 | (30) |
| 13–17 y | 4,033 | (7) | 848 | (11) | 442 | (9) | 281 | (14) | 40 | (16) | 85 | (17) |
| 18–50 y | 40,011 | (65) | 3,769 | (49) | 2,224 | (45) | 1,273 | (63) | 116 | (45) | 156 | (32) |
| ≥50 y | 6,424 | (11) | 1,092 | (13) | 797 | (16) | 164 | (8) | 30 | (12) | 101 | (20) |
| Gender | ||||||||||||
| Male | 26,490 | (43) | 4,240 | (55) | 2,648 | (53) | 1,158 | (57) | 132 | (52) | 302 | (61) |
| Female | 34,666 | (57) | 3,520 | (45) | 2,344 | (47) | 861 | (43) | 124 | (48) | 191 | (39) |
| Mission type | ||||||||||||
| Natural disaster | 4,675 | (8) | 895 | (12) | 749 | (15) | 78 | (4) | 34 | (13) | 34 | (7) |
| Hospital support | 32,193 | (53) | 3,594 | (46) | 1,741 | (35) | 1,617 | (80) | 83 | (32) | 153 | (31) |
| Conflict | 23,923 | (39) | 3,273 | (42) | 2,504 | (50) | 324 | (16) | 139 | (54) | 306 | (62) |
| Total operations | 61,177 | (100) | 7,762 | (100) | 4,994 | (64) | 2,019 | (26) | 256 | (3) | 493 | (6) |
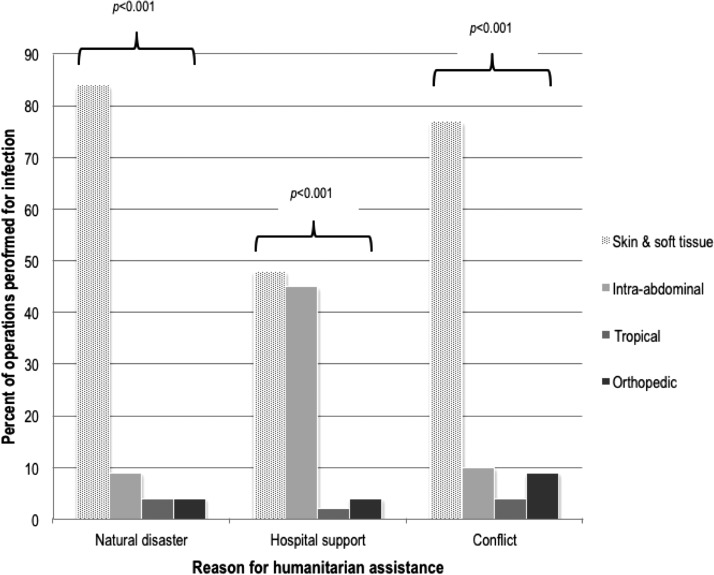
Skin and soft tissue infections accounted for 84% of operations performed for infection where humanitarian assistance was being provided for natural disaster and 48% when projects were supporting hospitals. Furthermore, there was evidence for a difference in the percentage of operations for each infection and reason for humanitarian assistance (Fig. 1). For example, operations for skin and soft tissue infections were more common during natural disaster and conflict projects than during hospital support missions (84 and 77% versus 48%, respectively; p<0.001). Operations for intra-abdominal infections were more common during hospital support missions (45% of operations for infection) compared with other reasons for assistance (p<0.001). Operations for orthopedic infections were performed more commonly during conflict projects (9%) than during the other reasons for humanitarian assistance (4% in both natural disaster and hospital support projects).
FIG. 1.
Percent of operations performed for each infection by reason for providing humanitarian assistance at Médecins Sans Frontières Operations Centre Brussels projects from 2008–2014. p values represent evidence for a difference between percent of operations performed for each infection and reason for humanitarian assistance using χ2 test.
Most procedures for skin and soft tissue and orthopedic infections were minor (76% and 58%, respectively), whereas most procedures for intra-abdominal infections were major operations (98%). Planned returns to the operating room, such as serial washouts or debridements and “second looks,” were more common after procedures for orthopedic (38%) and skin and soft tissue infections (33%) than for intra-abdominal infections. Planned serial operations after damage control laparotomy for surgical infections were performed frequently (7% of all laparotomies for infection). Unplanned returns to the operation room were not common after procedures for surgical infections. The majority of patients with surgical infections were otherwise healthy or with mild systemic disease. Spinal, regional, and general anesthetics without a definitive airway were used safely during most procedures (Table 4).
Table 4.
Clinical Characteristics of Operations for Infections Performed at Médecins Sans Frontières Operations Centre Brussels Projects from 2008–2014
| Skin and soft tissue | Intra-abdominal | Orthopedic | ||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Procedure | ||||||
| Major | 1,221 | (24) | 2,114 | (98) | 210 | (42) |
| Minor | 3,860 | (76) | 55 | (2) | 293 | (58) |
| Operation | ||||||
| Initial | 3,400 | (67) | 1,997 | (92) | 309 | (61) |
| Planned return | 1,654 | (33) | 142 | (7) | 191 | (38) |
| Unplanned return | 27 | (<1) | 28 | (1) | 58 | (1) |
| ASA class | ||||||
| I | 3,408 | (68) | 884 | (43) | 356 | (72) |
| II | 1,327 | (26) | 827 | (40) | 88 | (18) |
| III | 249 | (5) | 278 | (14) | 41 | (8) |
| IV | 31 | (1) | 65 | (3) | 12 | (2) |
| V | 1 | (<1) | 8 | (<1) | 0 | (0) |
| Anesthetic | ||||||
| GA without airway | 3,842 | (76) | 1,029 | (48) | 294 | (59) |
| GA with airway | 84 | (2) | 305 | (14) | 27 | (5) |
| Spinal or regional | 452 | (9) | 718 | (33) | 138 | (27) |
| Other | 703 | (14) | 115 | (5) | 44 | (9) |
| OR time; median (IQR) | 30 | (10–240) | 65 | (25–300) | 55 | (20–200) |
| Peri-operative deaths | 0 | (0) | 11 | (1) | 0 | (0) |
Tropical infections are included into the type of operation they require (i.e., skin and soft tissue for Buruli ulcer, intra-abdominal for typhoid perforation, etc.).
Peri-operative deaths are those that occurred in the operating theatre or in the post-anesthetic recovery area.
ASA=American Society for Anesthesia; GA=general anesthesia; OR=operating room; IQR=interquartile range.
Discussion
This study aimed to describe the experience of MSF-OCB surgery for infections in LMICs. By doing so, needs for training and resource allocation can be identified and addressed to improve humanitarian response. Operations for infections represented a significant proportion of the surgical volume in LMICs, particularly procedures for skin and soft tissue infections. In addition, serial operations were relatively common for all infection groups, highlighting the potential for greater than expected surgical resource requirements. Although tropical infections are not common, they are encountered in LMICs and require clinicians familiar with their presentation and management to ensure appropriate care. The number of procedures MSF-OCB provided during hospital support projects underscores the need for strengthening national health systems to care for these common conditions that may have otherwise been neglected (e.g., abscesses, appendicitis).
Return trips to the operating room were most common for skin and soft tissue and orthopedic infections. Appreciating the disproportionately high resource requirements for these common pathologies during crisis is important for planning an adequate response. During crisis, conditions are particularly unhygienic and local health care and transport infrastructure are often destroyed. Subsequently, many wounds are contaminated wounds, common pathologies go untreated, and pre-hospital times are extraordinarily long [18,19]. As a result, wounds invariably require cleansing and often serial debridement [20]. Other reports from surgical care during crisis corroborate this MSF experience [20,21], For example, during humanitarian assistance, much of the wound care is performed in the operating room (as opposed to on the ward) given lack of skilled nursing care and need for aggressive debridement with intensive pain management techniques [20]. Complicating this necessary practice in LMICs, operating room resources (e.g., surgeons, anesthetists, available time, equipment, and supplies) are scarce in LMICs [7,22]. Anticipating this operative burden and delivering the requisite input for surgical care, particularly during crisis, requires consideration of the operative epidemiology by type of mission (i.e., conflict, natural disaster, hospital support), inventory of available resources, and understanding of pre-mission unmet surgical needs. Together, these data might allow more accurate and cost-effective provision of necessary resources for surgical care during crisis.
One in every 13 operations for intra-abdominal infections was a return trip to the operating room, likely related to delayed presentation and complications thereof (e.g., peritonitis, severe sepsis), need for utilizing damage control techniques, and occasionally, drainage of a deep space wound infection. Despite appropriate use of damage control surgery, intra-abdominal abscesses are not unusual [23,24]. Austere health care settings, such as sites described in this study, rarely have access to minimally invasive or percutaneous drainage capacity for intra-abdominal abscess [25]. Therefore, signs and symptoms of ongoing sepsis after laparotomy required return to the operating room for exploration and drainage. Given the morbidity and mortality associated with such procedures, establishing basic training workshops and capacity for percutaneous drainage procedures (e.g., ultrasound-guided drain placement equipment and supplies), may reduce complications attributable to uncontrolled intra-abdominal infections or re-laparotomy [26–28].
Although not among the more common conditions requiring operation by MSF-OCB, tropical infections requiring surgery remain prevalent in LMICs [11,15,29–31]. Their presentations are often similar to non-tropical diseases and risk being treated inappropriately by inexperienced providers (e.g., appendicitis versus typhoid ileal perforation; congenital versus filarial hydrocele; liver abscess versus cystic echinococcosis) [30,32]. Therefore, clinicians embarking on humanitarian missions in tropical LMICs should familiarize themselves with the diagnosis and management of these conditions to avoid good-intentioned but ineffective care [10].
Prior to using these data for planning a more effective humanitarian response, several limitations should be mentioned. First, this study analyzed routinely collected operational data. Although clinical and outcome data would be informative for planning and monitoring capacity development and quality improvement interventions, sustainable collection of these data is difficult during crisis and has not yet been done for humanitarian surgical assistance programs. Nonetheless, these results are useful for general assessment of unmet surgical need and deploying resources for humanitarian surgical assistance programs more accurately. Second, quality care for surgical infections requires a comprehensive system, ideally including prevention, diagnostics, resuscitation, critical care, and recovery. This study was unable to describe the characteristics and proxies for resource requirements of MSF-OCB's other infection-related activities given the strictly procedural data. However, multi-disciplinary strategy is an integral part of programs caring for surgical conditions in any context. Next, hydroceles were not included among the tropical infections, making these figures a bare minimum estimate. An unknown proportion of hydroceles represents the effects of chronic lymphatic filariasis and requires post-operative anti-parastic therapy. The etiology of the hydroceles, or associated signs, was not recorded routinely for description. Despite these limitations, this is the largest examination of humanitarian surgical treatment of infections published and contributes substantially to the operationalization of surgical care in equivalent settings.
Conclusion
Surgical infections are common causes for operation in LMICs, particularly during crisis. This study found that infections require greater than expected surgical input given frequent need for serial operations to overcome contextual challenges and those associated with limited resources in other areas (e.g., ward care). Furthermore, these results demonstrate that the pattern of operations for infections is related to nature of the crisis. As a result, resources necessary for the treatment of skin and soft tissue infections are more needed during natural disasters (e.g., dressing supplies), those for intra-abdominal infections more needed in hospital support missions (e.g., closed suction drains, temporary abdominal closure systems), and those for orthopedic infections more common during conflict (e.g., orthopedic training, external fixators). Incorporating training into humanitarian preparation (e.g., surgical sepsis care, ultrasound-guided drainage procedures) and ensuring adequate resources for the care of surgical infections are necessary components for providing essential surgical care during crisis.
Acknowledgments
We thank the dedicated national and international staff that provided the expertise and care for these patients. In addition, we thank all of those involved in data collection and management for their contribution to those who will require humanitarian surgical care in the future. Routine data collection was performed with funds from Médecins Sans Frontières Operations Centre Brussels. Data analysis and manuscript preparation undertaken by B.T.S. was done with funding from the Fogarty International Center through the Northern Pacific Global Health Research Fellows Training Consortium under grant number R25TW009345.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Luboga S, Macfarlane SB, von Schreeb J, et al. Increasing access to surgical services in sub-Saharan Africa: Priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med 2009;6:e1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grimes CE, Henry JA, Maraka J, et al. Cost-effectiveness of surgery in low- and middle-income countries: A systematic review. World J Surg 2014;38:252–263 [DOI] [PubMed] [Google Scholar]
- 3.Groen RS, Samai M, Stewart KA, et al. Untreated surgical conditions in Sierra Leone: A cluster randomised, cross-sectional, countrywide survey. Lancet 2012;380:1082–1087 [DOI] [PubMed] [Google Scholar]
- 4.Mock C. Confronting the global burden of surgical disease. World J Surg 2013;37:1457–1459 [DOI] [PubMed] [Google Scholar]
- 5.Stewart B, Khanduri P, McCord C, et al. Global disease burden of conditions requiring emergency surgery. Br J Surg 2014;101:e9–22 [DOI] [PubMed] [Google Scholar]
- 6.Bickler S, Ozgediz D, Gosselin R, et al. Key concepts for estimating the burden of surgical conditions and the unmet need for surgical care. World J Surg 2010;34:374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galukande M, von Schreeb J, Wladis A, et al. Essential surgery at the district hospital: A retrospective descriptive analysis in three African countries. PLoS Med 2010;7: e1000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kushner AL. A proposed matrix for planning global surgery interventions. World J Surg 2014;38:3039–3040 [DOI] [PubMed] [Google Scholar]
- 9.Ozgediz D, Jamison D, Cherian M, et al. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ 2008;86:646–647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong EG, Trelles M, Dominguez L, et al. Surgical skills needed for humanitarian missions in resource-limited settings: Common operative procedures performed at Medecins Sans Frontieres facilities. Surgery 2014;156:642–649 [DOI] [PubMed] [Google Scholar]
- 11.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–2128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.IHME. Data Visualizations. Global Burden of Disease Cause Patterns 2013. www.vizhub.healthdata.org/gbd-cause-patterns/ (Last accessed December7, 2014)
- 13.Balint GA. Selected gastrointestinal pathologies in tropical sub-Saharan Africa. Bull World Health Organ 1998;76:207–212 [PMC free article] [PubMed] [Google Scholar]
- 14.Eastwood GL, Reilly PC., Jr Tropical peptic ulcer disease: An endoscopic study from rural Haiti. J Clin Gastroenterol 1986;8(3 Pt 2):385–388 [DOI] [PubMed] [Google Scholar]
- 15.Huang GK, Johnson PD. Epidemiology and management of Buruli ulcer. Expert Rev Anti Infect Ther 2014;12:855–865 [DOI] [PubMed] [Google Scholar]
- 16.Grimes CE, Bowman KG, Dodgion CM, Lavy CB. Systematic review of barriers to surgical care in low-income and middle-income countries. World J Surg 2011;35:941–950 [DOI] [PubMed] [Google Scholar]
- 17.LeBrun DG, Chackungal S, Chao TE, et al. Prioritizing essential surgery and safe anesthesia for the Post-2015 Development Agenda: Operative capacities of 78 district hospitals in 7 low- and middle-income countries. Surgery 2014;155:365–373 [DOI] [PubMed] [Google Scholar]
- 18.Noji EK. Public health in the aftermath of disasters. BMJ 2005;330:1379–1381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters. Emerg Infect Dis 2007;13:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giannou C, Baldan M. War Surgery: Working with Limited Resources in Armed Conflict and Other Situations of Violence, Volume 1 Geneva, Switzerland: International Committee of the Red Cross, 2010 [Google Scholar]
- 21.Edwards MJ, Lustik M, Carlson T, et al. Surgical interventions for pediatric blast injury: An analysis from Afghanistan and Iraq 2002 to 2010. J Trauma Acute Care Surg 2014;76:854–858 [DOI] [PubMed] [Google Scholar]
- 22.Gupta S, Wong EG, Mahmood U, et al. Burn management capacity in low and middle-income countries: A systematic review of 458 hospitals across 14 countries. Int J Surg, 2014;12:1070–1073 [DOI] [PubMed] [Google Scholar]
- 23.Turza KC, Campbell CA, Rosenberger LH, et al. Options for closure of the infected abdomen. Surg Infect 2012;13:343–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Godat L, Kobayashi L, Costantini T, Coimbra R. Abdominal damage control surgery and reconstruction: World Society of Emergency Surgery position paper. World J Emerg Surg 2013;8:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oliverson BG, Suhocki P, Lungren MP, et al. Interventional radiology in the developing world: Challenges and opportunities. J Vasc Intervent Radiol 2013;24:S129 [Google Scholar]
- 26.Civardi G, Di Candio G, Giorgio A, et al. Ultrasound guided percutaneous drainage of abdominal abscesses in the hands of the clinician: A multicenter Italian study. Eur J Ultrasound 1998;8:91–99 [DOI] [PubMed] [Google Scholar]
- 27.Saleem M, Ahmad N, Ahsan I. Ultrasound guided percutaneous drainage of abdominal abscesses. J Pak Med Assoc 2000;50:50–53 [PubMed] [Google Scholar]
- 28.Groen RS, Leow JJ, Sadasivam V, Kushner AL. Review: Indications for ultrasound use in low- and middle-income countries. Trop Med Int Health 2011;16:1525–1535 [DOI] [PubMed] [Google Scholar]
- 29.Finn TP, Stewart BT, Reid HL, et al. Integrated rapid mapping of neglected tropical diseases in three states of South Sudan: Survey findings and treatment needs. PLoS One 2012;7:e52789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart BT, Jacob J, Finn T, et al. , Cystic echinococcosis in Mundari tribe-members of South Sudan. Pathog Glob Health 2013;107:293–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ekenze SO, Anyanwu PA, Ezomike UO, Oguonu T. Profile of pediatric abdominal surgical emergencies in a developing country. Int Surg 2010;95:319–324 [PubMed] [Google Scholar]
- 32.Wolinsky H. Tropical travel medicine. A growing interest in tropical medicine reflects the increasing incidence of tropical disease in the Western world. EMBO Rep 2008;9:714–716 [DOI] [PMC free article] [PubMed] [Google Scholar]