Abstract
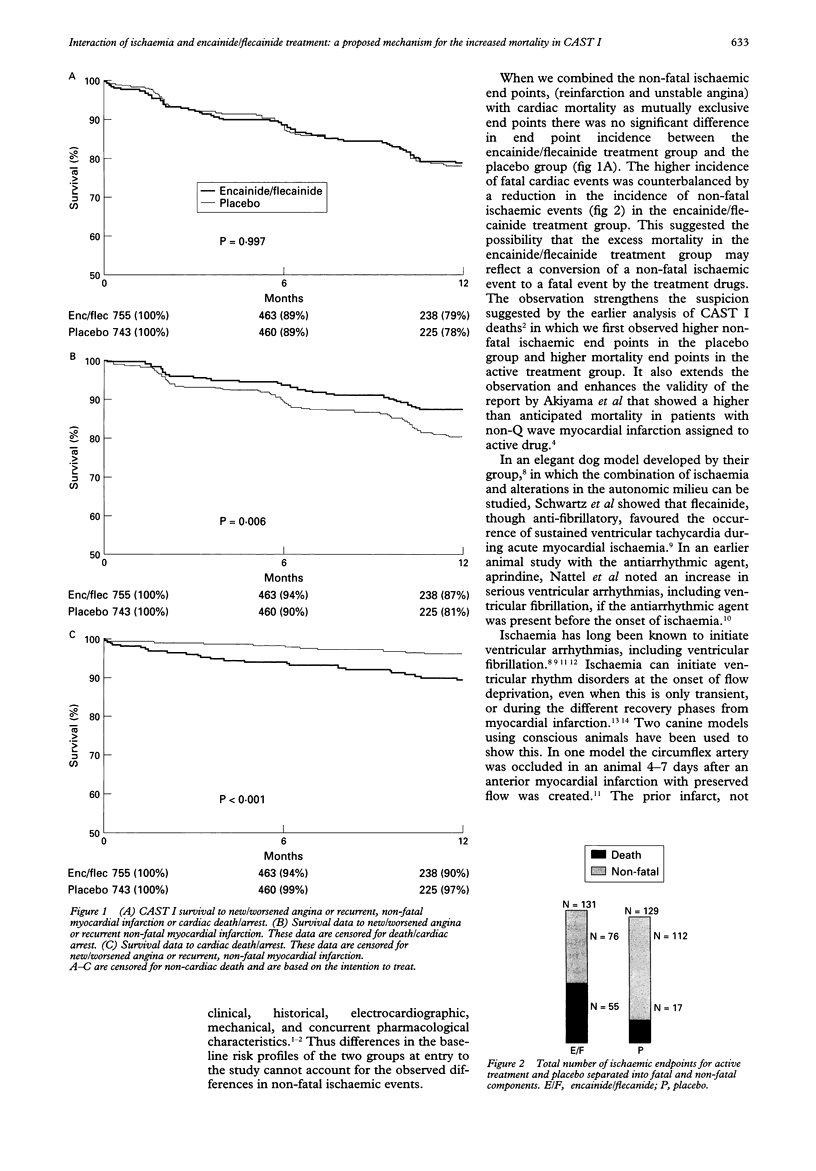
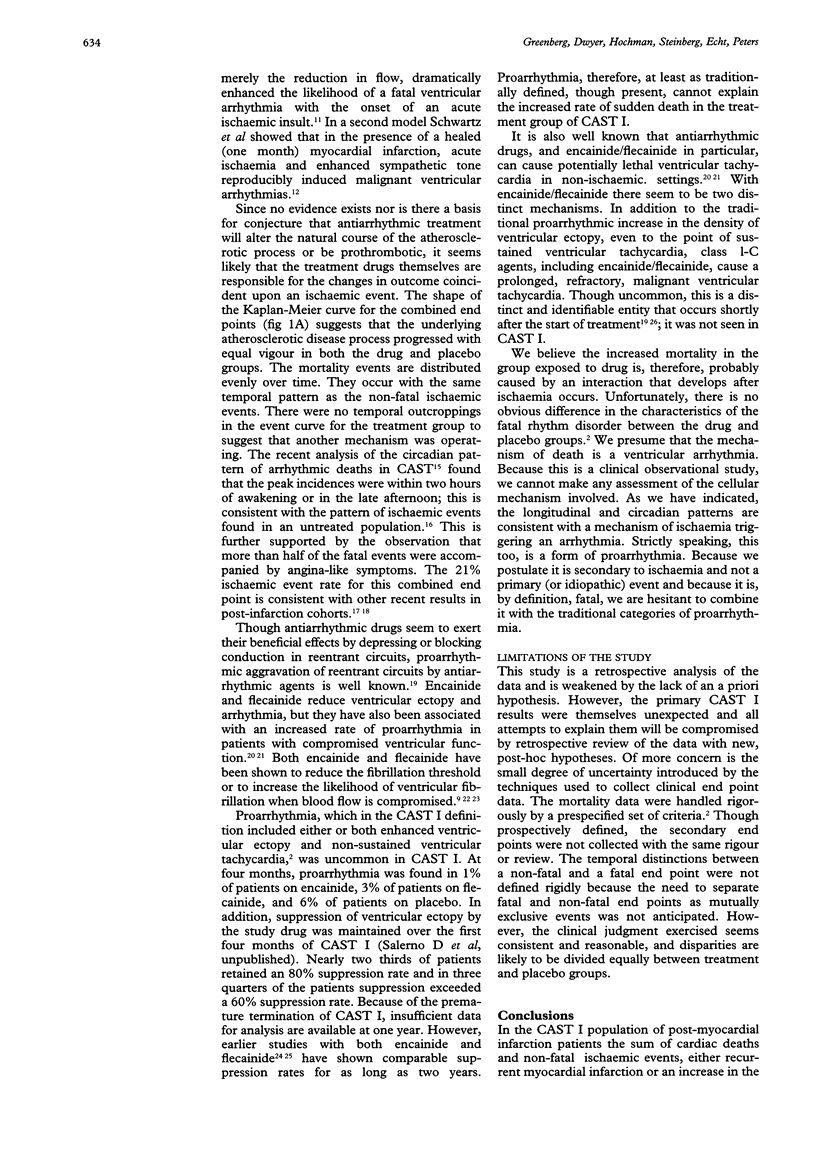
OBJECTIVE--To determine whether an interaction between encainide or flecainide and intercurrent ischaemia could account for the observed increase in cardiac and sudden deaths in the study group in the Cardiac Arrhythmia Suppression Trial (CAST) I. DESIGN--CAST I was a randomised, double blind, placebo controlled study in which patients received the drug which suppressed at least 6 premature ventricular contractions per minute by 80% or episodes of non-sustained ventricular tachycardia by 90%. Arrhythmic sudden death or aborted sudden death were the study end points. Measured secondary end points included recurrent myocardial infarction, new or increasing angina pectoris, congestive heart failure, and syncope. The CAST I database was analysed to determine which of three end points occurred first--cardiac death or cardiac arrest, angina pectoris, or non-fatal recurrent infarction. They were regarded as mutually exclusive end points. The triad of cardiac or sudden arrhythmic death plus congestive heart failure and syncope was similarly analysed. RESULTS--It was assumed that recurrent non-fatal infarction and new or increasing angina pectoris were ischaemic in origin. The sum of these non-fatal ischaemic end points and sudden death were nearly identical in the placebo group (N = 129) and the treatment group (N = 131). The one year event rate in each group was 21%. However, the treatment group had a much greater fatality rate (55 v 17; P < 0.0001) than the placebo group. The same relation was found when the data were examined on the basis of drug exposure rather than intention to treat. The temporal and circadian events were similar in each group and were consistent with an ischaemic pattern. No such patterns emerged from analysis of the presumed non-ischaemic end points of congestive heart failure and syncope. CONCLUSIONS--These data suggest that the interaction between active ischaemia and treatment with encainide or flecainide may have been responsible for the increased mortality seen in the treatment group in CAST I. This conversion of a non-fatal to a fatal event emphasises the need for future antiarrhythmic drugs to be screened in ischaemic models.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akhtar M., Breithardt G., Camm A. J., Coumel P., Janse M. J., Lazzara R., Myerburg R. J., Schwartz P. J., Waldo A. L., Wellens H. J. CAST and beyond. Implications of the Cardiac Arrhythmia Suppression Trial. Task Force of the Working Group on Arrhythmias of the European Society of Cardiology. Circulation. 1990 Mar;81(3):1123–1127. doi: 10.1161/01.cir.81.3.1123. [DOI] [PubMed] [Google Scholar]
- Akiyama T., Pawitan Y., Greenberg H., Kuo C. S., Reynolds-Haertle R. A. Increased risk of death and cardiac arrest from encainide and flecainide in patients after non-Q-wave acute myocardial infarction in the Cardiac Arrhythmia Suppression Trial. CAST Investigators. Am J Cardiol. 1991 Dec 15;68(17):1551–1555. doi: 10.1016/0002-9149(91)90308-8. [DOI] [PubMed] [Google Scholar]
- Hodges M., Salerno D. M., Granrud G. Flecainide versus quinidine: results of a multicenter trial. Am J Cardiol. 1984 Feb 27;53(5):66B–71B. doi: 10.1016/0002-9149(84)90505-8. [DOI] [PubMed] [Google Scholar]
- Kou W. H., Nelson S. D., Lynch J. J., Montgomery D. G., DiCarlo L., Lucchesi B. R. Effect of flecainide acetate on prevention of electrical induction of ventricular tachycardia and occurrence of ischemic ventricular fibrillation during the early postmyocardial infarction period: evaluation in a conscious canine model of sudden death. J Am Coll Cardiol. 1987 Feb;9(2):359–365. doi: 10.1016/s0735-1097(87)80389-3. [DOI] [PubMed] [Google Scholar]
- Muller J. E., Tofler G. H., Stone P. H. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989 Apr;79(4):733–743. doi: 10.1161/01.cir.79.4.733. [DOI] [PubMed] [Google Scholar]
- Nattel S., Pedersen D. H., Zipes D. P. Alterations in regional myocardial distribution and arrhythmogenic effects of aprindine produced by coronary artery occlusion in the dog. Cardiovasc Res. 1981 Feb;15(2):80–85. doi: 10.1093/cvr/15.2.80. [DOI] [PubMed] [Google Scholar]
- Patterson E., Holland K., Eller B. T., Lucchesi B. R. Ventricular fibrillation resulting from ischemia at a site remote from previous myocardial infarction. A conscious canine model of sudden coronary death. Am J Cardiol. 1982 Dec;50(6):1414–1423. doi: 10.1016/0002-9149(82)90484-2. [DOI] [PubMed] [Google Scholar]
- Peters R. W., Mitchell L. B., Brooks M. M., Echt D. S., Barker A. H., Capone R., Liebson P. R., Greene H. L. Circadian pattern of arrhythmic death in patients receiving encainide, flecainide or moricizine in the Cardiac Arrhythmia Suppression Trial (CAST). J Am Coll Cardiol. 1994 Feb;23(2):283–289. doi: 10.1016/0735-1097(94)90408-1. [DOI] [PubMed] [Google Scholar]
- Salerno D. M., Fifield J., Hodges M. Antiarrhythmic drug therapy for suppression of ventricular arrhythmia: experience with 122 patients treated for two years. J Clin Pharmacol. 1990 Mar;30(3):226–234. doi: 10.1002/j.1552-4604.1990.tb03466.x. [DOI] [PubMed] [Google Scholar]
- Schwartz P. J., Billman G. E., Stone H. L. Autonomic mechanisms in ventricular fibrillation induced by myocardial ischemia during exercise in dogs with healed myocardial infarction. An experimental preparation for sudden cardiac death. Circulation. 1984 Apr;69(4):790–800. doi: 10.1161/01.cir.69.4.790. [DOI] [PubMed] [Google Scholar]
- Schwartz P. J., Vanoli E., Zaza A., Zuanetti G. The effect of antiarrhythmic drugs on life-threatening arrhythmias induced by the interaction between acute myocardial ischemia and sympathetic hyperactivity. Am Heart J. 1985 May;109(5 Pt 1):937–948. doi: 10.1016/0002-8703(85)90233-9. [DOI] [PubMed] [Google Scholar]
- Soyka L. F. Safety of encainide for the treatment of ventricular arrhythmias. Am J Cardiol. 1986 Aug 29;58(5):96C–103C. doi: 10.1016/0002-9149(86)90111-6. [DOI] [PubMed] [Google Scholar]
- Stanton M. S., Prystowsky E. N., Fineberg N. S., Miles W. M., Zipes D. P., Heger J. J. Arrhythmogenic effects of antiarrhythmic drugs: a study of 506 patients treated for ventricular tachycardia or fibrillation. J Am Coll Cardiol. 1989 Jul;14(1):209–217. doi: 10.1016/0735-1097(89)90074-0. [DOI] [PubMed] [Google Scholar]
- Stramba-Badiale M., Lazzarotti M., Facchini M., Schwartz P. J. Malignant arrhythmias and acute myocardial ischemia: interaction between flecainide and the autonomic nervous system. Am Heart J. 1994 Nov;128(5):973–982. doi: 10.1016/0002-8703(94)90597-5. [DOI] [PubMed] [Google Scholar]
- Winkle R. A., Mason J. W., Griffin J. C., Ross D. Malignant ventricular tachyarrhythmias associated with the use of encainide. Am Heart J. 1981 Nov;102(5):857–864. doi: 10.1016/0002-8703(81)90036-3. [DOI] [PubMed] [Google Scholar]



