Abstract
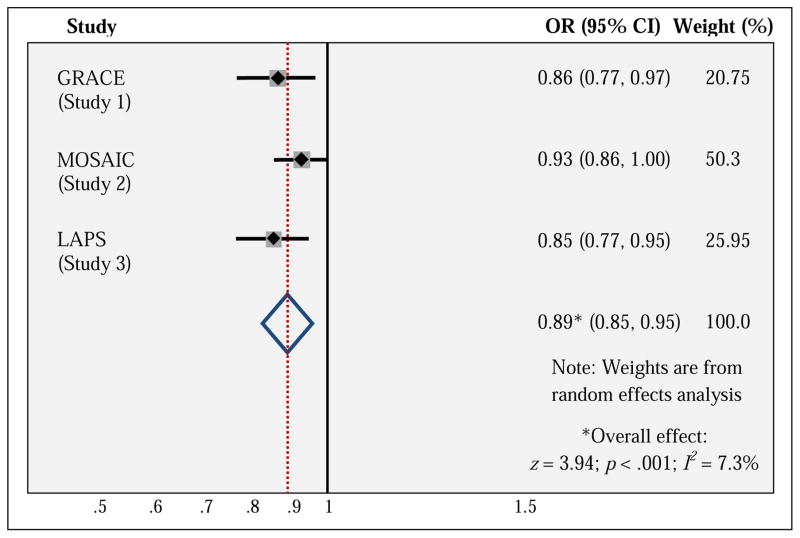
Optimism has been associated with reduced suicidal ideation, but there have been few studies in patients at high suicide risk. We analyzed data from three study populations (total N=319) with elevated risk of suicide: (1) patients with a recent acute cardiovascular event, (2) patients hospitalized for heart disease who had depression or an anxiety disorder, and (3) patients psychiatrically hospitalized for suicidal ideation or following a suicide attempt. For each study we analyzed the association between optimism (measured by the Life-Orientation Test-Revised) and suicidal ideation, and then completed an exploratory random effects meta-analysis of the findings to synthesize this data. The meta-analysis of the three studies showed that higher levels of self-reported optimism were associated with a lower likelihood of suicidal ideation (odds ratio [OR]=.89, 95% confidence interval [CI]=.85–.95, z=3.94, p<.001), independent of age, gender, and depressive symptoms. This association held when using the subscales of the Life Orientation Test-Revised scale that measured higher optimism (OR=.84, 95% CI=.76–.92, z=3.57, p<.001) and lower pessimism (OR=.83, 95% CI= .75–.92], z=3.61, p<.001). These results also held when suicidal ideation was analyzed as an ordinal variable. Our findings suggest that optimism may be associated with a lower risk of suicidal ideation, above and beyond the effects of depressive symptoms, for a wide range of patients with clinical conditions that place them at elevated risk for suicide.
Suicide is a major public health problem (e.g., Fleischmann and De Leo, 2014) and is responsible for 800,000 deaths worldwide each year (World Health Organization, 2014). Given the prevalence of suicide, much attention has been paid to identifying suicide risk factors, including specific demographic (e.g., age), social (e.g., unemployment), medical (e.g., pain), and psychological characteristics (e.g., psychosis; Hawton and van Heeringen, 2009). Among these risk factors, one of the most consistent findings is that individuals with chronic medical and psychiatric conditions have a substantially elevated risk of suicide (Hawton and van Heeringen, 2009, Kishi et al., 2001).
Along with identifying risk factors for suicide, however, it is critical to identify factors that may mitigate the risk of suicide (Knox et al., 2004, Wingate et al., 2006). Recent investigations suggest that some factors such as social support (Hirsch and Barton, 2011), meaning in life (Kleiman and Beaver, 2013), and positive affect (Hirsch et al., 2009) are associated with fewer suicidal thoughts and behaviors. Preliminary research regarding optimism (defined as generalized expectations for a positive future) consistently indicates that it is also inversely related to suicidal thoughts and behaviors (Bryan et al., 2013, Chang et al., 2013, Hirsch et al., 2007, O’Keefe and Wingate, 2013).
The beneficial effects of optimism on suicidal ideation may be distinguished from the adverse effects of depression and hopelessness. Low optimism is not synonymous with the presence of depression and hopelessness (Glanz et al., 1995, Rasmussen et al., 2009), and it may be a more durable trait (Glanz et al., 1995, Rasmussen and Wingate, 2011). Furthermore, empirical studies have found that optimism’s association with fewer suicidal thoughts has been independent of the effects of depression and hopelessness (Hirsch et al., 2007, O’Connor et al., 2008). Hirsch et al. (2007) found that among young college students, optimism was significantly associated with lower suicidal ideation on multivariable analysis including depression and hopelessness, and O’Connor et al. (2008) similarly found that positive future thinking was associated with lower risk for subsequent suicidal ideation, independent of depression, hopelessness, and baseline suicidal ideation in a population of patients hospitalized for suicidal self-harm.
To date, most investigations of the association between optimism and suicidal thoughts have studied young, healthy participants (Hirsch et al., 2006). Few studies regarding optimism’s association with suicide have included patients with medical or psychiatric conditions, a cohort at elevated risk for suicide (Amer and Hamdan-Mansour, 2014, Hawton and van Heeringen, 2009). Accordingly, we separately examined the association between optimism (measured via the Life Orientation Test-Revised [LOT-R]; Scheier et al., 1994) and suicidal ideation in three different study populations with elevated risk for suicide. These included a largely psychologically healthy population of patients with heart disease, a group of cardiac patients with mood or anxiety disorders, and a set of medically healthy patients who were hospitalized for suicidal ideation or attempted suicide. We assessed the connection between optimism and suicidal ideation in each cohort controlling for age, gender, and depressive symptoms. We then combined the findings from the three individual analyses in an exploratory meta-analysis. We hypothesized that greater optimism would be associated with lower suicidal ideation, independent of age, gender, and depression, across all three of these at-risk populations that have rather different overall risk for suicide.
Methods
Overview
This analysis examined a total of three studies, individually and via meta-analysis. All three studies in this report were carried out in accordance with the latest version of the Declaration of Helsinki, Institutional Board Review approval was obtained prior to study initiation, and written informed consent was obtained from all participants.
Study 1 was the Gratitude Research in Acute Coronary Events (GRACE) study (clinicaltrials.gov identifier NCT: 01709669), a 6-month observational study enrolling participants between September 2012 and January 2014. The GRACE study examined the impact of psychological constructs (e.g., optimism, gratitude) on subsequent outcomes (e.g., biomarkers, health behaviors, and rehospitalization) in patients with acute cardiac illness; methods and results have been described in detail elsewhere (Huffman et al., 2015a, Huffman et al., 2015b).
Study 2 was the Management of Sadness and Anxiety in Cardiology (MOSAIC) trial (clinicaltrials.gov identifier NCT: 01201967), a randomized controlled trial of a depression and anxiety collaborative care management intervention that enrolled patients who were hospitalized for acute cardiac illness at an urban academic medical center between September 2010 and December 2012. Participants were randomized to 24 weeks of the multipronged collaborative care intervention (utilizing a social work care manager to coordinate care) or to treatment as usual. Methods and main study results have been described in detail elsewhere (Huffman et al., 2013, Huffman et al., 2014b).
Study 3 was the Longitudinal Assessment of Positive States (LAPS) Study (clinicaltrials.gov identifier NCT: 01398891), a prospective observational study of 44 adults who were enrolled during hospitalization for suicidal thoughts or behavior between May 2011 and February 2013. Participants’ psychological status was measured via self-report assessments over 8 weeks.
After examining the relationship between optimism and suicidal ideation in each study, we performed an exploratory meta-analysis to synthesize the effects of optimism on suicidal ideation across these samples. Random effects models were used to examine associations between the LOT-R scale and suicidal ideation as measured by relevant items on scales used in the above studies; analyses were repeated using the LOT-R subscales.
Study 1 (GRACE)
Participants and procedures
Participants were patients who had been admitted to an urban academic medical center for an acute coronary syndrome (ACS), defined as myocardial infarction or unstable angina. Study exclusion criteria included an ACS occurring in the setting of another medical procedure, a comorbid terminal medical condition, inability to complete physical activity, and cognitive deficits diagnosed by a 6-item screening test (Callahan et al., 2002). As part of study procedures, self-report measures were administered at 2 weeks, 3 months, and 6 months after discharge. Participants’ baseline sociodemographic and medical characteristics were collected via patient self-report at enrollment and medical record review.
Measures
Dispositional optimism was assessed using the well-validated 6-item LOT-R. Example items include the positively worded “I expect more good things to happen to me than bad” and the negatively worded “I hardly ever expect things to go my way.” Participants responded to each item with the following scale: 4 = agree a lot, 3 = agree a little, 2 = neither agree nor disagree, 1 = disagree a little, and 0 = disagree a lot. Per convention (Scheier et al., 1994), a total optimism score was computed by reverse-scoring the negatively-worded items and summing the responses of all six items. The LOT-R has previously demonstrated acceptable convergent and discriminant validity (Scheier et al., 1994). The internal consistency of the LOT-R in the Study 1 sample (α = .85) was good, consistent with its demonstrated reliability in other samples (Scheier et al., 1994). In addition to the total optimism scale, the LOT-R contains two embedded 3-item optimism and pessimism subscales, with higher scores on each subscale representing higher optimism and lower pessimism, respectively. In our sample, Cronbach’s alpha for the optimism subscale (α = .75) and pessimism subscale (α = .83) were similar to previous estimates of reliability for each subscale (Vassar and Bradley, 2011).
Depression was measured using the first eight items (PHQ-8) of the nine-item Patient Health Questionnaire-9 (PHQ-9). The PHQ-9 asks about the nine core symptoms (each scored 0–3) of depression (American Psychiatric Association, 2013). For each item (e.g., “Trouble concentrating on things, such as reading the newspaper or watching television”), respondents were asked to report whether they had experienced the symptom “not at all” “several days,” “more than half of the days,” or “nearly every day” over the past two weeks. The PHQ-9 has been validated in medical populations (Kroenke et al., 2001), and its use is recommended by the American Heart Association to assess depression (Lichtman et al., 2008). The eight-item PHQ-8 (all depression items except suicidal ideation) is increasingly used in clinical settings as a stand-alone measure of depression. The PHQ-8 has itself been validated in large population-based cohorts (Kroenke et al., 2009, Wells et al., 2013) as well as in patients with coronary artery disease (Razykov et al., 2012) and heart failure (Pressler et al., 2011). In this and all studies in this report, validated scales, which are not equivalent to formal clinical diagnoses, were used to assess depression. The scales, rather than structured diagnostic interviews, were used because of their lesser burden on participants, increasing use in clinical practice, greater applicability to multiple settings (i.e., staff trained in full diagnostic interviews are not required), and good correlation with formal depression diagnoses. For example, elevated scores (>10) on the PHQ-8 are closely linked to formal diagnoses of major depression (Kroenke et al., 2009). Further supporting the use of this scale was the good internal consistency of the PHQ-8 in this sample (α = .81), consistent with prior studies of the PHQ-8 and PHQ-9 (α = .82–.89; Kroenke et al., 2009, Marks et al., 2005, Pressler et al., 2011).
Suicidal ideation was assessed via Item 9 of the PHQ-9, which inquires about “thoughts that you would be better off dead or of hurting yourself in some way.” According to convention and prior studies of suicide using Item 9 (Lossnitzer et al., 2009, Razykov et al., 2012, Shemesh et al., 2009), any positive response to this item (e.g., “several days”) was considered indicative of suicidal ideation. In addition to analyzing suicidal ideation as a dichotomous variable, in secondary analyses we also analyzed suicidal ideation (PHQ-9 Item 9) as an ordinal variable (0–3) to assess relationships between optimism and suicidal ideation when additionally considering the frequency of sucidal thoughts.
Analytic strategy
Generalized estimating equations with an exchangeable working correlation structure for observations within a subject and robust standard errors were used to assess associations between optimism and suicidal ideation at all assessments (2 weeks, 3 months, and 6 months post-discharge). Initial analyses examined associations between total optimism score (LOT-R) and suicidal ideation (PHQ-9 Item 9), controlling for age and gender. For the main analysis, depressive symptoms (PHQ-8) were also included in the model. Analyses were repeated using the optimism and pessimism subscales as the primary independent variable. Odds ratios and coefficients are larger for each one-point change on the LOT-R subscales compared to the total scale because of the smaller score range for the subscale (3 items) than for the total scale (6 items). For secondary analyses examining suicidal ideation as an ordinal variable, ordinal logistic regression was used; robust standard errors were used to account for clustering within subjects. For this study, and subsequent studies in this report, analyses were performed using Stata version 11.0 (StataCorp: College Station, TX), all tests were two-tailed, and statistical significance was set at p < .05.
Study 2 (MOSAIC)
Participants and procedures
Eligible patients were at least 18 years of age, fluent in English, admitted for a primary cardiac diagnosis of ACS, heart failure, or arrhythmia, and found to have a psychiatric diagnosis of clinical depression, generalized anxiety disorder, or panic disorder. Clinical depression was defined using the PHQ-9, with ≥5 symptoms—including either depressed mood or anhedonia—present for more than half the days over the prior 2 weeks. We did not require formal major depression based on a comprehensive diagnostic interview because elevated but subsyndromal levels of depressive symptoms in cardiac patients are still linked to an elevated risk of repeat cardiac events or mortality (Bush et al., 2001) and because our PHQ-9-based criteria already closely approximated the more time-consuming structured interview for major depression. Generalized anxiety disorder and panic disorder diagnoses were made using the Primary Care Evaluation of Mental Disorders anxiety modules for these two disorders (Spitzer et al., 1994).
Patients were excluded if they had a terminal medical condition, had cognitive disturbance on a 6-item cognitive screen (Callahan et al., 2002), had acute medical symptoms that precluded participation, or met psychiatric exclusion criteria (bipolar disorder, psychotic symptoms, active suicidal ideation with current intent or plan, or substance use disorder active within the past month). Bipolar disorder and psychotic symptoms were assessed using the appropriate modules of the Mini International Neuropsychiatric Interview (MINI; Pinninti et al., 2003). Substance abuse was assessed using the CAGE questionnaire; scores ≥2 resulted in exclusion (Mayfield et al., 1974). Acute suicidal ideation was assessed via a detailed suicide assessment (Suarez et al., 2015) prompted by a positive score on Item 9 of the PHQ-9.
Given that the MOSAIC trial was an intervention study with participants receiving different treatments post-enrollment, we utilized only baseline data for the purposes of this analysis. All baseline self-report measures (e.g., LOT-R) were administered pre-randomization by study staff at the time of enrollment. Baseline sociodemographic and medical data were collected via self-report and medical record review by blinded study staff.
Measures
The LOT-R was added to the MOSAIC assessment battery in September 2011, after 72 participants had been enrolled. Measures of optimism (LOT-R), depression (PHQ-8), and suicidality (Item 9 of the PHQ-9) were identical to Study 1. In this sample, internal consistency values for the total LOT-R (α = .85), optimism subscale (α = .71), and pessimism subscale (α = .87) at baseline were adequate. Internal consistency for the PHQ-8 was relatively low (α = .56); removing somatic items from the scale (sleep, appetite, concentration, and psychomotor items) based on previously published factor loading studies of the PHQ-9 (de Jonge et al., 2007) resulted in an improved but still low internal consistency (α = .64).
Analytic strategy
Multivariate logistic regression was used to assess the cross-sectional association between optimism and suicidality, controlling for age, gender, and depressive symptoms. As before, an initial analysis of the association between the total optimism scale and Item 9 was performed, controlling for age and gender. Depression (PHQ-8) was then added to the multivariate model for the primary analysis. Analyses were repeated using the optimism and pessimism subscales of the LOT-R. As in Study 1, we repeated analyses using Item 9 as an ordinal variable, using ordinal logistic regression.
The low internal consistency of the PHQ-8 in this hospitalized cardiac population may have been due to elevated somatic symptom scores related to the acute medical illness. For this reason, we repeated all analyses from this study using baseline PHQ-2 scores (Kroenke et al., 2003). The PHQ-2 contains the two cardinal symptoms of depression (depressed mood and anhedonia) and should be less prone to overlap with somatic symptoms.
Study 3 (LAPS)
Participants and procedures
Eligible patients were hospitalized on the inpatient psychiatric unit of an urban academic medical center for acute suicidal ideation or following a suicide attempt, confirmed by the patient’s primary psychiatric team. Patients were excluded if they were unable to read or speak English, had psychosis (as identified by the relevant Mini International Neuropsychiatric Inventory [MINI] module; Pinninti et al., 2003), or had cognitive impairment on a 6-item cognitive screen (Callahan et al., 2002). Baseline self-report assessments were conducted during hospitalization on the day prior to discharge; baseline sociodemographic and medical characteristics were obtained via patient report and medical record review. Study staff conducted follow-up assessments by phone at 2, 4, and 8 weeks post-discharge.
Measures
Optimism was again measured via the LOT-R. Internal consistency of the total LOT-R and subscales was good (αtotal = .91, αoptimism = .85, and αpessimism = .87). Depression was measured via the 16-item Quick Inventory of Depressive Symptomatology Self-Report (QIDS-SR; (Rush et al., 2003)), a well-validated instrument with high reliability and good internal consistency (α = .86; Rush et al., 2003, Trivedi et al., 2004). As with the PHQ-9, we used this self-report scale for this study rather than formal diagnostic interviews to reduce participant burden and given good correlation with interview-based major depression diagnoses. The QIDS-SR contains 16 questions (scored 0–3) that assess the nine Diagnostic and Statistical Manual-based criterion symptoms of depression (American Psychiatric Association, 2013). Scores of 0–5 indicate no depression; 6–10 indicate mild depression; 11–15 indicate moderate depression; 16–20 indicate severe depression; ≥21 indicate very severe depression (Rush et al., 2003). Internal consistency in this population, at baseline, was good (α = .82).
As with the PHQ-9, the QIDS-SR has a single question that asks directly about suicidal ideation (Item 12: “Thoughts of my own death or suicide”). This item has been used to assess self-reported suicidal ideation in prior studies of patients with depression (Gao et al., 2015, Laje et al., 2007, Zisook et al., 2009). As with the PHQ-9 in Studies 1 and 2, we split the QIDS-SR into a scale for depression (QIDS-SR-depression: 15 items) and the suicide item (QIDS-SR Item 12). The QIDS-SR-depression scale without the suicide item maintained good internal consistency (α = .81).
Analytic strategy
Generalized estimating equations with an exchangeable working correlation structure and robust standard errors were used to assess relationships between optimism and suicidal ideation (as assessed by QIDS-SR Item 12) at all study time points (baseline, 2 weeks, 4 weeks, and 8 weeks). Consistent with the previous studies in this report, initial analyses examined associations between optimism and suicidality controlling for age and gender. The main analysis added depression (QIDS-SR-depression scores) to the model. Analyses were repeated using the optimism and pessimism subscales of the LOT-R. For consistency with the Study 1 and 2 analyses, and based on prior studies using the QIDS-SR to examine suicidal ideation (Gao et al., 2015, Laje et al., 2007, Zisook et al., 2009), we analyzed the suicide item as a dichotomous variable, with all responses other than “I didn’t think of suicide or death” (score = 0) recorded as suicidal ideation. We again analyzed suicidal ideation as an ordinal variable (0–3 score on QIDS-SR Item 12) in secondary analyses, using ordinal logistic regression with robust standard errors.
Exploratory Meta-analysis
To synthesize the effects of optimism on suicidal ideation across these samples, we performed an exploratory meta-analysis. Random effects models were used to meta-analyze the results of the individual studies regarding the association between optimism (LOT-R) and suicidal ideation (PHQ-9 Item 9 or QIDS-SR Item 12), controlling for age, gender, and depressive symptoms. To obtain a global assessment of effect size as outlined by odds ratios (OR), the ORs in individual studies were weighted by the magnitude of the standard error to account for the precision of the OR estimate in each study. As in the individual study analyses, we repeated analyses with LOT-R subscale scores.
Study heterogeneity was explored using the chi-square test of heterogeneity (Q) and the I2 statistic derived from Q and the degrees of freedom. I2 estimates the degree of variance in a pooled effect size that can be accounted for by heterogeneity. Values of 25%, 50%, and 75% are considered low, moderate, and high, respectively (Higgins et al., 2003). As for the individual studies, analyses were performed in Stata 11.0, all tests were two-tailed, and p < .05 was considered significant.
Results
Study 1 (GRACE)
A total of 164 participants enrolled and provided LOT-R and PHQ-9 data. Of these, 164 (100%) provided data at 2 weeks, 163 (99%) at 3 months, and 156 (95%) at 6 months following discharge. Table 1 displays the age and gender of participants, as well as baseline optimism and depression scores; eTable 1 displays the full baseline characteristics of the study population. Overall, the mean age of the sample was 61.5 years (standard deviation [SD] = 10.5), 137 participants (83%) were men, the mean total LOT-R was 17.7 (SD = 5.6), similar to population-based norms (M = 16.1, SD = 4.1; Glaesmer et al., 2012), and the mean PHQ-8 was 4.2 (SD = 4.3), representing low levels of depression in most participants. Mean PHQ-8 score among those with a positive Item 9 (representing suicidal ideation) was 13.7 (SD = 5.4; range 5–24), compared to a mean of 3.4 (SD = 3.7; range 0–21) among those with a negative Item 9.
Table 1.
Participant characteristics across cohorts.
| Characteristic | GRACE (N = 164) | MOSAIC (N = 112) | LAPS (N = 44) |
|---|---|---|---|
| Age, years | 61.5 (10.5; 38–90) | 61.6 (11.7; 24–90) | 43.0 (14.7; 20–68) |
| Gender | |||
| Men, N (%) | 137 (84) | 53 (47) | 19 (43) |
| Women, N (%) | 27 (16) | 59 (53) | 25 (57) |
| Baseline LOT-R | 17.7 (5.6; 1–24) | 11.2 (7.3; 0–24) | 12.4 (6.7; 0–24) |
| Baseline LOT-R Optimism | 9.0 (2.9; 0–12) | 6.2 (3.8; 0–12) | 6.0 (3.6; 0–12) |
| Baseline LOT-R Pessimisma | 8.7 (3.3; 0–12) | 5.0 (4.3; 0–12) | 6.4 (3.6; 0–12) |
| Baseline depression | |||
| PHQ-8 | 4.2 (4.3; 0–23) | 15.4 (4.4; 4–24) | - |
| QIDS-SR-Depressionb | - | - | 10.1 (5.9; 1–24) |
Note. Data provided as M (SD; minimum-maximum) unless otherwise noted; LOT-R=Life Orientation Test—Revised; PHQ-8=Patient Health Questionnaire-8; QIDS-SR=Quick Inventory of Depressive Symptoms—Self-Report.
Convention for LOT-R subscales is that higher scores represent lower pessimism.
Includes all items except for suicidal ideation item (Item 12).
Controlling for age and gender, optimism measured via LOT-R total score was significantly and inversely related to suicidal ideation (β = −.29; 95% confidence interval [CI] [−.39, −.19], p < .001). Additionally controlling for depression measured via PHQ-8, optimism remained significantly associated with lower risk of suicidal ideation (β = −.15, 95% CI [−.26, −.05], p = .017).
Subscale analysis revealed that higher scores on both the LOT-R optimism subscale (β = −.46, 95% CI [−.66, −.27], p < .001) and pessimism subscale (β = −.46; 95% CI [−.65, .28], p < .001; higher scores represent lower pessimism) were associated with reduced risk of suicidal ideation, controlling for age and gender. These associations held when depressive symptoms were also added to the model (optimism subscale: β = −.26, 95% CI [−.49, −.02], p = .034; pessimism subscale: β = −.21, 95% CI [−.39, −.03], p = .020). Finally, when suicidal ideation was analyzed as an ordinal variable (see eTable 4), LOT-R total scores were significantly associated with suicidal ideation (β = −.16, 95% CI [−.30, −.014], p = .032) in the fully adjusted model, as were the optimism (β = −.28, 95% CI [−.55, −.014], p = .039) and the pessimism (β = −.22, 95% CI [−.44, −.004], p = .046) subscales.
Study 2 (MOSAIC)
A total of 112 participants had complete data for analysis (see Table 1 and eTable 2 for baseline characteristics). The mean age of the sample was 61.6 (SD = 11.7) years, and 53% were women. The mean total LOT-R score was 11.2 (SD = 7.3), substantially lower than in the general population, and mean PHQ-8 scores were 15.4 (SD = 4.4). Participants with positive Item 9 scores had mean baseline PHQ-8 scores of 17.3 (SD = 3.8; range 8–24), compared to 14.8 (SD = 4.5; range 4–24) among those with negative Item 9 scores.
Table 2 displays the results of the analyses examining associations between optimism and suicidal ideation. Controlling for age and gender, the total optimism score was significantly and inversely related to suicidal ideation (β = −.09, 95% CI [−.16, −.02], p = .012). After controlling for depression measured via the PHQ-8, the total optimism score remained inversely associated with suicidal ideation (β = −.08, 95% CI [−.15, −.004], p = .039). Controlling for age and gender, higher scores on both the optimism subscale (β = −.16, 95% CI [−.29, −.03], p = .014) and the pessimism subscale (β = −.13, 95% CI [−.24, −.007], p = .037) were associated with lower rates of suicidal ideation. When controlling for depressive symptoms in addition to age and gender, associations for both the optimism subscale (β = −.13, 95% CI [−.26, .002], p = .053) and pessimism subscale (β = −.11, 95% CI [−.23, .01], p = .072) persisted, but were marginally nonsignificant.
Table 2.
The association between optimism and suicidality across cohorts, controlling for age, gender, and depressive symptoms.
| Adjusted for Age and Gender | Coefficient (Standard Error in parentheses)
|
||
|---|---|---|---|
| Characteristic | GRACE (N = 165) | MOSAIC (N = 112) | LAPS (N = 44) |
| LOT-R Total Scale | −0.29*** (0.05) | −0.09* (0.04) | −0.25*** (0.05) |
| LOT-R Optimisma | −0.46*** (0.10) | −0.16* (0.07) | −0.35*** (0.09) |
| LOT-R Pessimismb | −0.46*** (0.09) | −0.13* (0.06) | −0.42*** (0.07) |
| Adjusted for Age, Gender, and Depressive Symptoms | Coefficient (Standard Error in parentheses)
|
||
|---|---|---|---|
| Characteristic | GRACE (N = 165) | MOSAIC (N = 112) | LAPS (N = 44) |
| LOT-R Total Scale | −0.15* (0.06) | −0.08* (0.04) | −0.16** (0.05) |
| LOT-R Optimisma | −0.26* (0.12) | −0.13~ (0.07) | −0.22* (0.09) |
| LOT-R Pessimismb | −0.21* (0.09) | −0.11~ (0.06) | −0.28*** (0.08) |
Note.
p ≤ .10,
p ≤ .05,
p ≤ .01,
p ≤ .001. LOT-R=Life Orientation Test—Revised.
Coefficients for subscales are larger than for the overall scale because coefficients measure the effect of a one-point change in the scale on suicide risk, and subscales have half the number of items.
Convention for LOT-R subscales is that higher scores represent lower pessimism.
When suicidal ideation was analyzed as an ordinal variable (eTable 4), results were highly similar. The LOT-R total score (β = −.077, 95% CI [−.15, −.006], p = .034) was associated with reduced suicidal ideation on fully adjusted analyses, and the optimism subscale scores (β = −.13, 95% CI [−.26, .003], p = .055), and pessimism subscale scores (β = −.12, 95% CI [−.24, .003], p = .057) were marginally nonsignificant.
Repeat analyses with the PHQ-2 were highly similar to those with the PHQ-8. Using the LOT-R total score, and accounting for age, gender, and depressive symptoms (PHQ-2), optimism was associated with suicidal ideation (β = −.08, 95% CI [−.15, −.01], p = .031). On subscale analyses using the PHQ-2 and adjusting for the same variables, the LOT-R optimism subscale (β = −.14, 95% CI [−.27, −.01], p = .034), but not the pessimism subscale (β = −.11, 95% CI [−.23, .01], p = .079), was significantly associated with suicidal ideation.
Study 3 (LAPS)
Of the 44 participants, all (100%) completed the initial assessment and 38 (86%) completed at least one follow-up assessment (n = 29 [66%] at 2 weeks, n = 26 [59%] at 4 weeks, n = 30 [68%] at 8 weeks). Table 1 and eTable 3 display the baseline characteristics of participants. Mean age of participants was 42.3 years (SD = 14.7); 57% were women. Mean total LOT-R scores at baseline (M = 12.4; SD = 6.7) were lower than population norms (M = 15.3; SD = 4.1) for this age group (Glaesmer et al., 2012), and QIDS-SR scores (M = 10.6; SD = 6.3) were consistent with mild to moderate depression.
Table 2 again displays the results of the main study analyses. Patients with suicidal ideation on QIDS-SR Item 12 had mean QIDS-SR-depression scores of 14.7 (SD = 5.5; range 3–24), compared to scores of 7.4 (SD = 4.1; range 1–20) in those without suicidal ideation. Controlling for age and gender, the total optimism score was significantly and inversely related to suicidal ideation (β = −.25, 95% CI [−.35, −.14], p < .001). Higher total optimism score remained significantly associated with less suicidal ideation when controlling for depression (β = −.16, 95% CI [−.27, −.06], p = .003). Both the optimism subscale (β = −.22, 95% CI [−.41, −.04], p = .017) and the pessimism subscale (β = −.28, 95% CI [−.44, −.11], p = .001) were likewise associated with risk of suicide, controlling for age, gender, and depression. When QIDS-SR Item 12 was re-analyzed as an ordinal variable (eTable 4), total LOT-R score (β = −.28, 95% CI [−.45, −.11], p = .001), optimism subscale score (β = −.22, 95% CI [−.42, −.02], p = .028), and pessimism subscale score (β = −.17, 95% CI [−.28, −.05], p = .004) were all associated with suicidal ideation controlling for age, gender, and depression.
Meta-analysis
Using the LOT-R total scores, the three populations (N = 319 participants) showed minimal heterogeneity (Q = 2.16, p = .34, I2 = 7.3%, estimate of between-study variance τ2 = .0002). Across the studies—controlling for age, gender, and depression—higher total optimism score was associated with significantly lower risk of suicidal ideation (OR = .89, 95% CI [.85, .95], z = 3.94, p < .001; Figure 1). Utilizing the LOT-R subscales, both the optimism subscale (OR = .84, 95% CI [.76, .92], z = 3.57, p < .001; eFigure 1) and pessimism subscale (OR = .83, 95% CI [.75, .92], z = 3.61, p < .001; eFigure 2) were significantly associated with suicidal ideation in the hypothesized direction. As previously noted, effects on the OR per one-point LOT-R change are larger for subscales because of the smaller number of items (by half) in each subscale.
Figure 1.
General Discussion
Optimism was consistently linked to lower suicidality among three distinct populations of patients with recent acute cardiac illness, clinically significant psychiatric conditions, or both. The analyzed studies were overall rather heterogeneous in their design: they utilized different measures of depression, different timing of follow-up assessments, and different primary study goals. Despite this heterogeneity, we observed consistent associations between greater levels of optimism and less suicidal ideation.
Furthermore, these relationships held when suicidal ideation was considered as both a dichotomous variable (i.e., as a yes/no variable such that any response greater than zero represented suicidal ideation) and an ordinal variable (i.e., as a numerical variable that represented the score on the item, such that more severe or frequent suicidal ideation received a higher score). This allowed us to assess the presence or absence of suicidal ideation, as well as the frequency and intensity of suicidal thoughts. The strength of the association between optimism and suicidal ideation was consistent across the studies, and our findings also generally held for both the LOT-R total scale and the LOT-R subscales, suggesting that both greater optimism and less pessimism are associated with less suicidal ideation.
Epidemiologically, there are different patterns of suicidal ideation and behavior across age and gender. For example, men have higher rates of completed suicide, while women have higher rates of suicidal ideation, and there are increases in suicidal thoughts and behaviors among both younger (18–24) and older (>65) populations (Centers for Disease Control and Prevention, Crosby et al., 2011, Kessler et al., 2005). In this study, the observed connections between optimism and lower suicidal ideation were independent of both age and gender, further suggesting that this is a consistent association across demographic characteristics that is not restricted to a single population group.
In addition to being independent of age and gender, the associations between optimism and suicidal ideation in our three studies were independent of depression, which is consistent with work in prior studies (Hirsch et al., 2007). Depression is a key factor in assessing suicide risk, and among people who die by suicide, depression is more common than any other psychological disorder (American Foundation for Suicide Prevention, 2015, Cavanagh et al., 2003). However, depression is not the only contributing factor to suicidal ideation. Indeed, we found that although depression scores were generally higher in patients with suicidal ideation, individuals with the highest depression scores did not universally have suicidal ideation, and some participants with low depression scores (e.g., PHQ-8 scores of 5–10 in Studies 1 and 2) had suicidal ideation. This further supports the concept that depression and suicidal ideation are not wholly linked and that additional factors such as optimism must be considered. Furthermore, optimism and depression do not simply represent opposite sides of the same continuum, as evidenced by their relatively weak inverse correlations (e.g., a relatively modest Pearson correlation (r) of −.30 in a meta-analysis of optimism and health; Rasmussen et al., 2009). This may explain why optimism and depression may have distinct, separate effects on suicidal ideation, and why we found that optimism’s association with lower risk of suicidal ideation was independent of depression in all three of our studies.
Finally, we found that these connections held when studied in patients with medical illness and in those with psychiatric illness, suggesting that the observed connections between optimism and suicidality likely apply to many important clinical populations. Our findings are consistent with the few existing studies focused on positive psychological constructs and suicide risk in medically ill persons. For example, in one study of individuals with diabetes, cardiovascular disease, or cancer, optimism was found to protect against suicidal ideation (Amer and Hamdan-Mansour, 2014). Studies 1 and 2 add to this literature by specifically examining a patient population (i.e., individuals who have cardiovascular illness) with elevated risk of suicide but without preexisting psychiatric illness (Larsen et al., 2010).
Optimism was also connected to suicidal ideation in patients with clinically relevant psychiatric illness. This is concordant with a pair of studies, in depressed older adults and suicidal inpatients, respectively, that found positive future orientation to be similarly associated with reduced suicidal ideation or behavior (Hirsch et al., 2006, O’Connor et al., 2008). Importantly, Study 2 was the first to examine connections between optimism and suicidal thoughts in patients who had both acute cardiac illness and clinical psychiatric conditions. Of note, the cohort of patients followed immediately post-discharge after hospitalization for suicidal ideation or behavior (Study 3), a population at exceedingly high risk for suicide compared to the general population (Appleby et al., 1999, Goldacre et al., 1993, Qin and Nordentoft, 2005), had the strongest associations between greater optimism and lower suicidal ideation. This suggests that the effects of optimism on lower suicidal ideation could be even more powerful in this clinical scenario.
Why might optimism reduce suicidal thoughts? In prior work, optimism has been associated with increased psychological well-being, fewer perceived stressors, reduced tendency to become depressed, and greater capacity for problem-solving, all of which have in turn been linked to reduced risk for suicidal ideation and behavior (Duberstein et al., 2004, Kroenke et al., 2009). Optimism may be relevant in the context of suicide because it is related to adaptive self-regulation. According to Carver and Scheier (1998), self-regulation involves being able to continually identify, pursue, and attain goals, which may be important in life purpose, meaning, and generativity, all of which may protect from suicidal thoughts.
Just as optimism is not at the opposite end of a continuum with depression, low optimism is also not identical to hopelessness. Hopelessness, defined as having negative thoughts about the future (Beck et al., 1975), is a common feature of depression and has also been linked with an increased risk of suicide (McMillan et al., 2007). Although moderately to strongly correlated (Eshun, 1999, Hirsch and Conner, 2006, Scheier and Carver, 1985), optimism and hopelessness are considered distinct constructs, and low ratings on hopelessness scales reflect a lack of hopelessness, not necessarily the presence of optimism (Glanz et al., 1995). Empirically, when positive future thinking and hopelessness were both used to predict suicidal ideation, positive future thinking but not hopelessness was associated with suicidal ideation (O’Connor et al., 2008, Scheier and Carver, 1985). For example, in a study of patients hospitalized for self-harm, positive future orientation was a stronger predictor of recurrent suicidality after discharge than global hopelessness (O’Connor et al., 2008). Optimism may therefore have beneficial effects on suicidal ideation that differ from the adverse effects of depression or hopelessness, given optimism’s emphasis on positive versus negative expectancies.
Overall, the strengths of these analyses included the use of validated tools to measure optimism, depressive symptoms, and suicidal ideation in real-world clinical populations. In addition, two of the studies allowed for repeated measurements of optimism over time. We were also able to control for key demographic and psychological factors in our individual and combined analyses. Finally, to our knowledge, this is the first report to quantitatively synthesize multiple studies examining optimism and suicidal ideation across distinct and varied high-risk populations of hospitalized patients using meta-analytic techniques.
There are also several important limitations of the studies and our analyses. These include the use of self-reported measures of suicide risk (rather than objective suicide-related outcomes such as self-harm or completed suicide) and the use of self-report assessments of optimism that require recall of emotional states in the preceding weeks, rather than other methods such as ecological momentary assessment, which typically inquire several times daily about emotional states and may provide greater accuracy and richness of data (Shiffman et al., 2008). In particular, the use of single items from the depression scales as metrics for suicidal ideation was an important limitation, as these items may not correlate closely with active suicidal ideation. For example, Item 9 on the PHQ-9 can non-specifically elicit suicidal ideation, behavior, or non-suicidal self-injury, and prior work in medically ill populations has found that the majority of persons who respond positively to this item are not at acute suicide risk (Razykov et al., 2012, Suarez et al., 2015).
Limitations related to the samples included recruitment from a single urban academic medical center and a high proportion of White patients in all studies, as well as a high proportion of men in Study 1 and a relatively small sample size in Study 3. Finally, the meta-analysis of the samples must be considered exploratory given the small number of studies that were included.
Despite these limitations, these findings suggest a unique contribution of higher optimism to reduced suicidal ideation in a wide range of clinical settings. Addressing depression (or hopelessness) alone may ignore distinct and durable beneficial effects of optimism, and developing specific interventions to promote optimism could represent a promising approach to high-suicide-risk patients. At the same time, given that optimism is often considered a trait (and that the LOT-R instrument associated with reduced suicidality is a measure of dispositional optimism), whether optimism is modifiable remains an open and important question. However, brief targeted interventions can improve optimism in patients at high risk for suicide (Huffman et al., 2014a), and at least one intervention study (Meevissen et al., 2011) found improvements in LOT-R scores over a short timeframe (2 weeks), suggesting that it may be possible to modify ‘trait’ optimism. Further study is needed to determine whether such interventions would modify optimism in these clinical populations, and whether successfully reducing optimism would, in turn, result in lower suicide risk.
Supplementary Material
Highlights.
Optimism and suicidal ideation were measured in three clinical cohorts
Higher optimism was associated with lower suicidal ideation in each cohort
These findings held when controlling for age, gender, and depressive symptoms
Promoting optimism may be a promising approach to reducing suicide risk
Acknowledgments
Role of funding source
This research and analysis time were funded by an American Heart Association Grant-in-Aid 10GRNT3450015, the Expanding the Science and Practice of Gratitude Project run by UC Berkeley’s Greater Good Science Center in partnership with UC Davis with funding from the John Templeton Foundation (grant ID 15627), and the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number R01HL113272, all to JH. The content is solely the responsibility of the authors and does not represent the official views of the funders.
Footnotes
Contributors
JH and BH were responsible for the study concept and design. SB, CD, and EB acquired the data. JH, JB, SB, and BH were responsible for the analysis and interpretation of data. JH and JB drafted the manuscript. SB, CD, EB, and BH contributed to critical revisions of the manuscript for important intellectual content. Finally, BH and JH were responsible for statistical analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amer NR, Hamdan-Mansour AM. Psychosocial predictors of suicidal ideation in patients diagnosed with chronic illnesses in Jordan. Issues Ment Health Nurs. 2014;35:864–71. doi: 10.3109/01612840.2014.917752. [DOI] [PubMed] [Google Scholar]
- American Foundation for Suicide Prevention. Understanding Suicide. 2015 Accessed at: https://www.afsp.org/understanding-suicide/frequently-asked-questions.
- American Psychiatric Association. Diagnostic and statistical manual of mental health disorders: DSM-5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J. 1999;318:1235–9. doi: 10.1136/bmj.318.7193.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Hopelessness and suicidal behavior. An overview. JAMA. 1975;234:1146–9. [PubMed] [Google Scholar]
- Bryan CJ, Ray-Sannerud BN, Morrow CE, Etienne N. Optimism reduces suicidal ideation and weakens the effect of hopelessness among military personnel. Cognit Ther Res. 2013;37:996–1003. [Google Scholar]
- Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, et al. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. Am J Cardiol. 2001;88:337–41. doi: 10.1016/s0002-9149(01)01675-7. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–81. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. Vol. 1998 New York, NY: Cambridge University Press; US; 1998. [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] National Center for Injury Prevention and Control, CDC (producer); 2013, 2011. Available from http://www.cdc.gov/injury/wisqars/index.html. 2013. [Google Scholar]
- Chang EC, Yu EA, Lee JY, Hirsch JK, Kupfermann Y, Kahle ER. An examination of optimism/pessimism and suicide risk in primary care patients: Does belief in a changeable future make a difference? Cognit Ther Res. 2013;37:796–804. [Google Scholar]
- Crosby AE, Han B, Ortega LA, Parks SE, Gfroerer J, et al. Centers for Disease C. Suicidal thoughts and behaviors among adults aged >/=18 years--United States, 2008–2009. MMWR Surveill Summ. 2011;60:1–22. [PubMed] [Google Scholar]
- de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med. 2007;69:735–9. doi: 10.1097/PSY.0b013e31815743ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y, Conner KR, Eberly S, Caine ED. Suicide at 50 years of age and older: perceived physical illness, family discord and financial strain. Psychol Med. 2004;34:137–46. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- Eshun S. Cross-Cultural Research. 1999. Cultural variations in hopelessness, optimism, and suicidal ideation: A study of Ghana and U. S. college samples; p. 33. [Google Scholar]
- Fleischmann A, De Leo D. The World Health Organization’s report on suicide: a fundamental step in worldwide suicide prevention. Crisis. 2014;35:289–91. doi: 10.1027/0227-5910/a000293. [DOI] [PubMed] [Google Scholar]
- Gao K, Wu R, Wang Z, Ren M, Kemp DE, Chan PK, et al. Disagreement between self-reported and clinician-ascertained suicidal ideation and its correlation with depression and anxiety severity in patients with major depressive disorder or bipolar disorder. J Psychosom Res. 2015;60:117–24. doi: 10.1016/j.jpsychires.2014.09.011. [DOI] [PubMed] [Google Scholar]
- Glaesmer H, Rief W, Martin A, Mewes R, Brahler E, Zenger M, et al. Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R) Br J Health Psychol. 2012;17:432–45. doi: 10.1111/j.2044-8287.2011.02046.x. [DOI] [PubMed] [Google Scholar]
- Glanz LM, Haas GL, Sweeney JA. Assessment of hopelessness in suicidal patients. Clin Psychol Rev. 1995;15:49–64. [Google Scholar]
- Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet. 1993;342:283–6. doi: 10.1016/0140-6736(93)91822-4. [DOI] [PubMed] [Google Scholar]
- Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JK, Barton AL. Positive social support, negative social exchanges, and suicidal behavior in college students. J Am Coll Health. 2011;59:393–8. doi: 10.1080/07448481.2010.515635. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Conner KR. Dispositional and explanatory style optimism as potential moderators of the relationship between hopelessness and suicidal ideation. Suicide Life Threat Behav. 2006;36:661–9. doi: 10.1521/suli.2006.36.6.661. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Conner KR, Duberstein PR. Optimism and suicide ideation among young adult college students. Arch Suicide Res. 2007;11:177–85. doi: 10.1080/13811110701249988. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein PR, Conner KR, Heisel MJ, Beckman A, Franus N, et al. Future orientation and suicide ideation and attempts in depressed adults ages 50 and over. Am J Geriatr Psychiatry. 2006;14:752–7. doi: 10.1097/01.JGP.0000209219.06017.62. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Duberstein PR, Unützer J. Chronic medical problems and distressful thoughts of suicide in primary care patients: Mitigating role of happiness. Int J Geriatr Psychiatry. 2009;24:671–9. doi: 10.1002/gps.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Beach SR, Suarez L, Mastromauro CA, Dubois CM, Celano CM, et al. Design and baseline data from the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized controlled trial. Contemp Clin Trials. 2013;36:488–501. doi: 10.1016/j.cct.2013.09.012. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Beale EE, Beach SR, Celano CM, Belcher AM, Moore SV, et al. Design and baseline data from the Gratitude Research in Acute Coronary Events (GRACE) study. Contemp Clin Trials. 2015a;44:11–9. doi: 10.1016/j.cct.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Beale EE, Celano CM, Beach SR, Belcher AM, Moore SV, et al. Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: the gratitude research in acute coronary events study. Circ Cardiovasc Qual Outcomes. 2015b doi: 10.1161/CIRCOUTCOMES.115.002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Healy BC, Boehm JK, Kashdan TB, Celano CM, et al. Feasibility and utility of positive psychology exercises for suicidal inpatients. Gen Hosp Psychiatry. 2014a;36:88–94. doi: 10.1016/j.genhosppsych.2013.10.006. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Mastromauro CA, Beach SR, Celano CM, DuBois CM, Healy BC, et al. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014b;174:927–35. doi: 10.1001/jamainternmed.2014.739. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–95. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kishi Y, Robinson RG, Kosier JT. Suicidal ideation among patients with acute life-threatening physical illness: patients with stroke, traumatic brain injury, myocardial infarction, and spinal cord injury. Psychosomatics. 2001;42:382–90. doi: 10.1176/appi.psy.42.5.382. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Beaver JK. A meaningful life is worth living: meaning in life as a suicide resiliency factor. Psychiatry Res. 2013;210:934–9. doi: 10.1016/j.psychres.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health. 2004;94:37–45. doi: 10.2105/ajph.94.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114:163–73. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Laje G, Paddock S, Manji H, Rush AJ, Wilson AF, Charney D, et al. Genetic markers of suicidal ideation emerging during citalopram treatment of major depression. Am J Psychiatry. 2007;164:1530–8. doi: 10.1176/appi.ajp.2007.06122018. [DOI] [PubMed] [Google Scholar]
- Larsen KK, Agerbo E, Christensen B, Sondergaard J, Vestergaard M. Myocardial infarction and risk of suicide: a population-based case-control study. Circulation. 2010;122:2388–93. doi: 10.1161/CIRCULATIONAHA.110.956136. [DOI] [PubMed] [Google Scholar]
- Lichtman JH, Bigger JT, Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–75. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- Lossnitzer N, Muller-Tasch T, Lowe B, Zugck C, Nelles M, Remppis A, et al. Exploring potential associations of suicidal ideation and ideas of self-harm in patients with congestive heart failure. Depress Anxiety. 2009;26:764–8. doi: 10.1002/da.20587. [DOI] [PubMed] [Google Scholar]
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part II) Health Promotion Practice. 2005;6:148–56. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- McMillan D, Gilbody S, Beresford E, Neilly L. Psychol Med. 2007. Can we predict suicide and non-fatal self-harm with the Beck Hopelessness Scale? A meta-analysis; p. 37. [DOI] [PubMed] [Google Scholar]
- Meevissen YM, Peters ML, Alberts HJ. Become more optimistic by imagining a best possible self: effects of a two week intervention. J Behav Ther Exp Psychiatry. 2011;42:371–8. doi: 10.1016/j.jbtep.2011.02.012. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Fraser L, Whyte MC, Machale S, Masterton G. A comparison of specific positive future expectancies and global hopelessness as predictors of suicidal ideation in a prospective study of repeat self-harmers. J Affect Disord. 2008;110:207–14. doi: 10.1016/j.jad.2008.01.008. [DOI] [PubMed] [Google Scholar]
- O’Keefe VM, Wingate LR. The role of hope and optimism in suicide risk for American Indians/Alaska Natives. Suicide Life Threat Behav. 2013;43:621–33. doi: 10.1111/sltb.12044. [DOI] [PubMed] [Google Scholar]
- Pinninti NR, Madison H, Musser E, Rissmiller D. MINI International Neuropsychiatric Schedule: clinical utility and patient acceptance. Eur Psychiatry. 2003;18:361–4. doi: 10.1016/j.eurpsy.2003.03.004. [DOI] [PubMed] [Google Scholar]
- Pressler SJ, Subramanian U, Perkins SM, Gradus-Pizlo I, Kareken D, Kim J, et al. Measuring depressive symptoms in heart failure: validity and reliability of the patient health questionnaire-8. Am J Crit Care. 2011;20:146–52. doi: 10.4037/ajcc2010931. [DOI] [PubMed] [Google Scholar]
- Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62:427–32. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: A meta-analytic review. Ann Behav Med. 2009;37:239–56. doi: 10.1007/s12160-009-9111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen KA, Wingate LR. The role of optimism in the interpersonal-psychological theory of suicidal behavior. Suicide Life Threat Behav. 2011;41:137–48. doi: 10.1111/j.1943-278X.2011.00022.x. [DOI] [PubMed] [Google Scholar]
- Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8--is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. J Psychosom Res. 2012;73:163–8. doi: 10.1016/j.jpsychores.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54:573–83. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–47. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. 1994;67:1063–78. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Shemesh E, Annunziato RA, Rubinstein D, Sultan S, Malhotra J, Santra M, et al. Screening for depression and suicidality in patients with cardiovascular illnesses. Am J Cardiol. 2009;104:1194–7. doi: 10.1016/j.amjcard.2009.06.033. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. J Am Med Assoc. 1994;272:1749–56. [PubMed] [Google Scholar]
- Suarez L, Beach SR, Moore SV, Mastromauro CA, Januzzi JL, Celano CM, et al. Use of the Patient Health Questionnaire-9 and a detailed suicide evaluation in determining imminent suicidality in distressed patients with cardiac disease. Psychosomatics. 2015;56:181–9. doi: 10.1016/j.psym.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34:73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Vassar M, Bradley G. A reliability generalization study of coefficient alpha for the Life Orientation Test. J Pers Assess. 2011;92:362–70. doi: 10.1080/00223891.2010.482016. [DOI] [PubMed] [Google Scholar]
- Wells TS, Horton JL, LeardMann CA, Jacobson IG, Boyko EJ. A comparison of the PRIME-MD PHQ-9 and PHQ-8 in a large military prospective study, the Millennium Cohort Study. J Affect Disord. 2013;148:77–83. doi: 10.1016/j.jad.2012.11.052. [DOI] [PubMed] [Google Scholar]
- Wingate LR, Burns AB, Gordon KH, Perez M, Walker RL, Williams FM, et al. Suicide and positive cognitions: Positive psychology applied to the understanding and treatment of suicidal behavior. In: Ellis TE, editor. Cognition and Suicide: Theory, Research, and Therapy. Washington, DC, US: American Psychological Association; 2006. pp. 261–83. [Google Scholar]
- World Health Organization. Preventing Suicide: A Global Imperative. 2014 Accessed at http://apps.who.int/iris/bitstream/10665/131056/1/9789241564779_eng.pdf?ua=1&ua=1.
- Zisook S, Trivedi MH, Warden D, Lebowitz B, Thase ME, Stewart JW, et al. Clinical correlates of the worsening or emergence of suicidal ideation during SSRI treatment of depression: an examination of citalopram in the STAR*D study. J Affect Disord. 2009;117:63–73. doi: 10.1016/j.jad.2009.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.