Abstract
Objective
Motor vehicle crash (MVC)-related spinal injuries result in significant morbidity and mortality in children. The objective was to identify MVC-related injury causation scenarios for spinal injuries in restrained children.
Methods
This was a case series of occupants in MVCs from the Crash Injury Research and Engineering Network (CIREN) data set. Occupants aged 0–17 years old with at least one Abbreviated Injury Scale (AIS) 2+ severity spinal injury in vehicles model year 1990+ that did not experience a rollover were included. Unrestrained occupants, those not using the shoulder portion of the belt restraint, and those with child restraint gross misuse were excluded. Occupants with preexisting comorbidities contributing to spinal injury and occupants with limited injury information were also excluded. A multidisciplinary team retrospectively reviewed each case to determine injury causation scenarios (ICSs). Crash conditions, occupant and restraint characteristics, and injuries were qualitatively summarized.
Results
Fifty-nine cases met the study inclusion criteria and 17 were excluded. The 42 occupants included sustained 97 distinct AIS 2+ spinal injuries (27 cervical, 22 thoracic, and 48 lumbar; 80 AIS-2, 15 AIS-3, 1 AIS-5, and 1 AIS-6), with fracture as the most common injury type (80%). Spinal-injured occupants were most frequently in passenger cars (64%), and crash direction was most often frontal (62%). Mean delta-V was 51.3 km/h ± 19.4 km/h. The average occupant age was 12.4 ± 5.3 years old, and 48% were 16- to 17-year-olds. Thirty-six percent were right front passengers and 26% were drivers. Most occupants were lap and shoulder belt restrained (88%). Non-spinal AIS 2+ injuries included those of the lower extremity and pelvis (n = 56), head (n = 43), abdomen (n = 39), and thorax (n = 36). Spinal injury causation was typically due to flexion or lateral bending over the lap and or shoulder belt or child restraint harness, compression by occupant’s own seat back, or axial loading through the seat pan. Nearly all injuries in children <12 years occurred by flexion over a restraint, whereas teenage passengers had flexion, direct contact, and other ICS mechanisms. All of the occupants with frontal flexion mechanism had injuries to the lumbar spine, and most (78%) had associated hollow or solid organ abdominal injuries.
Conclusions
Restrained children in nonrollover MVCs with spinal injuries in the CIREN database are most frequently in high-speed frontal crashes, of teenage age, and have vertebral fractures. There are age-specific mechanism patterns that should be further explored. Because even moderate spinal trauma can result in measurable morbidity, future efforts should focus on mitigating these injuries.
Keywords: children, spine injury, injury mechanism, crash, disability
Introduction
Motor vehicle crashes (MVCs) are the most common mechanism of spinal injury in children (Cirak et al. 2004; Polk-Williams et al. 2008), and spinal cord injuries, either alone or in combination with other injuries, result in the most residual physical disability in children following discharge from inpatient rehabilitation (Zonfrillo et al. 2013). A recent analysis of MVC adult occupants using 2 NHTSA databases (the Crash Injury Research and Engineering Network [CIREN] and the NASS-CDS) demonstrated that, after controlling for potential confounders, occupants ≥65 years, in rollovers, or with an airbag-only restraint system resulted in increased odds of spinal cord injury when compared to younger individuals, those not in rollovers, or restrained with a belt with or without an airbag (Stein et al. 2011). Other prior research has shown that risk factors for MVC-related spinal cord injury in children include single-vehicle crashes, rollover crashes, and ejection of occupants (Rasouli et al. 2011). Less is known about patterns of injuries and their associated causation scenarios for restrained child occupants, and understanding this information is critical for further development of restraint system countermeasures. Therefore, the goal of this analysis was to identify MVC-related injury causation scenarios for spinal injuries in restrained children in order to gain insight into how loads of the crash and restraint system are transferred to the spinal column.
Methods
This case series of crash investigations were identified from the CIREN database, operated by the NHTSA. CIREN obtains detailed crash investigation data from crashes involving a convenience sample of patients admitted to a network of level 1 trauma centers in the United States with at least one Abbreviated Injury Scale (AIS) score of 3+ injury or 2 AIS 2+ injuries, who are subsequently selected for a detailed crash investigation (NHTSA 2013). Cases included child occupants <18 years old with at least one AIS 2+ spinal injury (as indicated by an AIS score value of 6xxxxx.2, 6xxxxx.3, 6xxxxx.4, 6xxxxx.5, or 6xxxxx.6) from vehicles model year 1990 and newer. Only patients properly restrained in a harness child restraint system, belt-positioning booster seat, or lap and shoulder belt were included. Rollover crashes were excluded, given the extreme kinematics and variable mechanisms of injury.
CIREN crash investigation teams used a standard protocol to measure and document the details of the crash, including evidence from the crash scene such as points of impact and vehicle final rest positions; damage to the interior and exterior of the study vehicle, including any occupant contact points; and detailed occupant and injury information. Crash investigators examined the interior and exterior of the vehicles involved, looking for evidence of occupant contact, including scuff marks and transfer of tissue, hair, bodily fluid, and clothing. Occupant contact points on the interior side structure were identified by photographs and included in the detailed crash report. The scene investigations were supplemented by information from crash occupants, witnesses, police reports, emergency medical service personnel, physicians, and hospital medical records. To determine injury causation scenarios, a multidisciplinary Case Review Team including emergency medicine physicians, engineers, crash investigation specialists, and database analysts reviewed each crash in detail. The case review process included review of crash conditions, restraint and occupant characteristics, occupant injuries (including radiologic evidence, listing of injuries, and medical treatment), and occupant contact points within the vehicle.
Measurements—Exposures
From the gathered information, reports were generated that included estimates of the vehicle dynamics and occupant kinematics during the crash and detailed descriptions of the injuries sustained in the crash by body region, type of injury, and severity of injury. Crash information sources included scene diagram, vehicle type, direction of impact, delta V calculations (the instantaneous change in velocity, an accepted measure of crash severity), vehicle crush, occupant compartment intrusion, occupant contact points, and restraint usage evidence.
Measurements—Outcomes
The multidisciplinary case review process included a review of crash conditions, restraint and occupant characteristics, occupant injuries, and occupant contact points within the vehicle. AIS version 2005/2008 was used for all analyses (AAAM 2008). If cases were originally coded in AIS 1990 or AIS 1998, they were manually remapped to version 2005/2008 by a certified AIS coder. For crashes within the CIREN database after 2005, injuries with AIS 2 and greater were analyzed using the CIREN Biomechanics Tab (BioTab) methodology to describe the injury causation scenario (ICS; Schneider et al. 2011). BioTab methodology documents the details of the factors involved in injury causation, specifically identifying the physical components (or occupants) within the vehicle that contributed to the injury, regional and organ mechanism of injury (such as bending, shear, compression, or tension), and any additional contributing factors (such as the occupant’s precrash position, intrusion into the occupant space, or past medical history). Each ICS included “involved physical components” (structures external to the occupant) that contacted the occupants and caused the injury. Confidence levels of “certain,” “probable,” and “possible” were assigned to each ICS and involved physical components. The BioTab method also allowed for the documentation of multiple scenarios in cases where a single scenario could not be determined with certainty.
For this study, cases meeting the inclusion criteria were subject to a preliminary quality control review including checks for sufficient information on occupant injuries, vehicle dynamics and damage, and interior contact points. Each case was further reviewed by the authors to confirm the ICS and involved physical components. For those cases that met the inclusion criteria but were not previously analyzed via the BioTab method, a full BioTab analysis was conducted.
Statistical Methods and Data Analysis
Standard descriptive summaries were used to summarize crash data and injury data.
Results
Fifty-nine cases met the study inclusion criteria. Seventeen were excluded from the analysis: 6 cases did not have detailed injury information, 5 were restrained by child seats with gross misuse or seats that are no longer considered best practice (including T-shield harnesses and trayshields), 4 occupants had spinal injuries that resulted from posterior loading by loose cargo or unrestrained occupants rather than crash forces, 1 had unknown restraint status, and 1 had a preexisting comorbidity (osteogenesis imperfecta) predisposing the occupant to fractures. The remaining 42 cases were reviewed and included in the analyses.
Table 1 shows the crash and occupant characteristics. The most common vehicle was a passenger car (64%) and the most frequent area of vehicle damage was the front (62%). Nearly all the cases in side-impact crashes (14 of 15) were ages 13–17. Delta V was calculated for 30 of the 42 cases, and the average resultant delta V was 51.3 km/h ± 19.4 km/h. The average occupant age was 12.4 years ± 5.3 years. Nearly half (48%) of included occupants were in the 16- to 17-year-old age range. Occupants were most often seated in the right front passenger seat (36%) and driver’s seat (26%). A lap/shoulder belt was used by 88% of occupants and the remaining 12% were restrained in a forward-facing car seat, a belt-positioning booster seat, or an unknown child restraint system.
Table 1.
Crash and occupant characteristics
| Occupants (total N = 42) | Spinal injuries (total N = 97) |
|||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Age | Age | Age | Age | |||||
| Total N
= 42 |
0–4 | 5–8 | 9–12 | 13–17 | ||||
|
|
||||||||
| N | % | N | N | N | N | N | % | |
| Vehicle type | ||||||||
| Minivan | 5 | 12 | 2 | 1 | — | 2 | 15 | 15 |
| Passenger car | 27 | 64 | 4 | 3 | 2 | 18 | 57 | 59 |
| Pickup | 3 | 7 | — | — | — | 3 | 4 | 4 |
| Sport utility | 7 | 17 | 1 | — | 2 | 4 | 21 | 22 |
| vehicle | ||||||||
| Crash direction | ||||||||
| Rear | 1 | 2 | — | — | — | 1 | 1 | 1 |
| Front | 26 | 62 | 7 | 4 | 3 | 12 | 66 | 68 |
| Left | 5 | 12 | — | — | — | 5 | 5 | 5 |
| Right | 10 | 24 | — | — | 1 | 9 | 25 | 26 |
| Delta V (km/h) | ||||||||
| Less than 20 | 0 | 0 | — | — | — | — | — | 0 |
| 20 to 29 | 1 | 2 | — | — | 1 | — | 1 | 1 |
| 30 to 39 | 10 | 24 | 1 | 1 | 1 | 7 | 17 | 18 |
| 40 to 49 | 5 | 12 | 1 | — | 1 | 3 | 7 | 7 |
| 50 to 59 | 4 | 10 | 1 | — | — | 3 | 18 | 19 |
| 60 to 69 | 6 | 14 | 2 | — | 1 | 3 | 18 | 19 |
| 70 to 79 | 2 | 5 | 1 | — | — | 1 | 7 | 7 |
| 80+ | 2 | 5 | — | — | — | 2 | 3 | 3 |
| Unknown | 12 | 29 | 1 | 3 | — | 8 | 26 | 27 |
| Age (years) | ||||||||
| 0–2 | 1 | 2 | 1 | — | — | — | 2 | 2 |
| 3–5 | 7 | 17 | 6 | 1 | — | — | 13 | 13 |
| 6–8 | 3 | 7 | — | 3 | — | — | 6 | 6 |
| 9–12 | 4 | 10 | — | — | 4 | — | 12 | 12 |
| 13–15 | 7 | 17 | — | — | — | 7 | 28 | 29 |
| 16–17 | 20 | 48 | — | — | — | 20 | 36 | 37 |
| Seating position | ||||||||
| Row 1 left (driver) | 11 | 26 | — | — | — | 11 | 20 | 21 |
| Row 1 right | 15 | 36 | 1 | 1 | 1 | 12 | 41 | 42 |
| Row 2 left | 6 | 14 | 2 | 1 | 2 | 1 | 19 | 20 |
| Row 2 middle | 2 | 5 | 2 | — | — | — | 4 | 4 |
| Row 2 right | 5 | 12 | 1 | 1 | — | 3 | 7 | 7 |
| Row 3 left | 2 | 5 | — | 1 | 1 | — | 4 | 4 |
| Row 3 right | 1 | 2 | 1 | — | — | — | 2 | 2 |
| Restraint | ||||||||
| Forward-facing | 2 | 5 | 2 | — | — | — | 4 | 4 |
| restraint system | ||||||||
| Booster | 2 | 5 | 2 | — | — | — | 4 | 4 |
| Lap/shoulder | 37 | 88 | 3 | 3 | 4 | 27 | 101 | 91 |
| belt | ||||||||
| Unknown child | 1 | 2 | 1 | — | — | — | 2 | 2 |
| restraint system | ||||||||
Figure 1 shows the injury distribution by severity and body region. By nature of the inclusion criteria, the spine was the most frequently injured AIS 2+ body region (n = 94 injuries), followed by the lower extremity including the pelvis (n = 56 injuries), head (n = 43), abdomen (n = 39), and thorax (n = 36). Of the spinal injuries, 80 were AIS 2, 15 were AIS 3, 1 was AIS 5, and 1 was AIS 6. Figure 2 shows the spinal injury distribution by injury type and spinal region, with fractures as the most frequent injury overall (n = 78) and in each spinal region. Figure 3 shows the spinal fracture distribution by vertebral location and spinal region, with vertebral body fractures and transverse process fractures most frequently seen in the cervical and thoracic/lumbar spine, respectively.
Fig. 1.
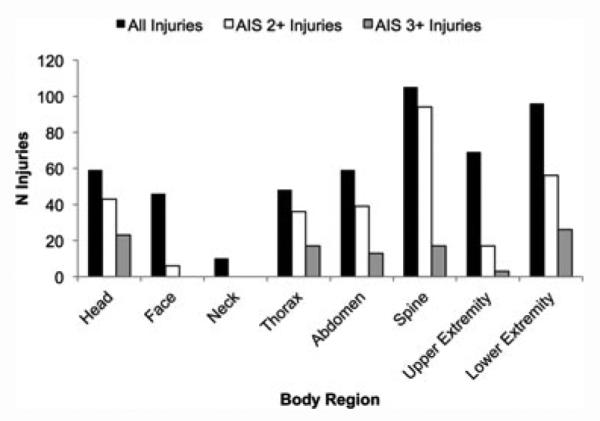
Injury distribution by severity and body region.
Fig. 2.
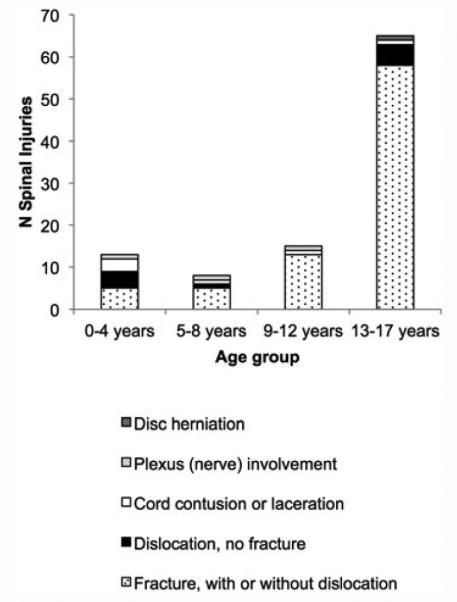
Spinal injury distribution by injury type and age group.
Fig. 3.
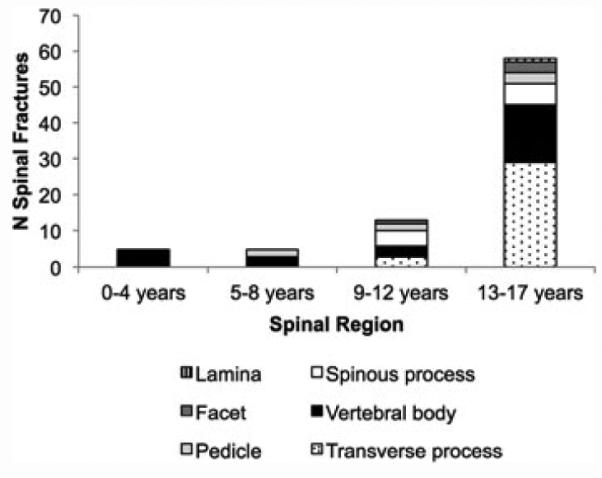
Spinal fracture distribution by vertebral location and age group.
Excluding 2 subjects who were dead on arrival to the hospital, the average number of days hospitalized was 15.3 days ± 16.3 days. Hospital stays ranged from 1 to 82 days with a median stay of 9 days. Two additional subjects succumbed to their injuries after hospitalization. For those subjects with known ICU visits, the average ICU stay was 5.4 days ± 9.4 days, with a range from 0–44 days and a median of 2 days
Tables 2–4 show the ICSs overall for specific age ranges (Table 2), for crash directionality (Table 3), and specific spinal regions (Table 4). ICSs included flexion, lateral bending, direct/transmitted contact, and axial loading. Some injuries had multiple ICSs and some occupants had multiple spinal locations injured. Injuries most frequently occurred from flexion over the lap belt (lumbar), flexion over the shoulder belt (cervical and thoracic), and direct contact to the torso from interior vehicle structures (thoracic and lumbar). All of the spinal injuries for children < 9 years occurred by flexion over the harness (3 occupants ages 21–24 months with 6 C-spine injuries), shoulder belt (4 occupants ages 3–5 years with 7 C-spine injuries), or lap belt (3 occupants all 7 years old, with 6 L-spine injuries). Nearly all of the spinal injuries (87%) in children ages 9–12 were from flexion over the lap belt, and the oldest children had more of a distribution of ICS including direct contact (46%), direct contact (24%), and transmitted contact (22%). All of the flexion injuries over the belt were in frontal crashes, whereas those from direct contact to the spine were near-side (69%) or frontal (31%). All of the occupants with frontal flexion mechanism had injuries to the lumbar spine, and most (78%) had associated hollow or solid organ abdominal injuries without pelvic fractures. In contrast, patients with lumbar spine injuries and pelvic fractures were predominantly from lateral bending or direct contact with vehicle structures.
Table 2.
Distribution of AIS 2+ spinal injuries by age and injury causation scenario
| AIS 2+ spinal injuries (N) | |||||
|---|---|---|---|---|---|
|
|
|||||
| Injury causation scenario | Scenarios (N) | Age 0–4 years | Age 5–8 years | Age 9–12 years | Age 13–17 years |
| Flexion | |||||
| Over lap belt | 9 | — | 6 | 13 | 9 |
| Over shoulder belt | 7 | 5 | 2 | 1 | 7 |
| Over Child Restraint System (CRS) harness | 3 | 6 | — | — | — |
| Lateral bending | |||||
| Over lap belt | 2 | — | — | — | 2 |
| Over shoulder belt | 1 | — | — | — | 1 |
| Direct contact to the spine—load applied to torso | |||||
| Side interior (e.g., door, B-pillar) | 9 | — | — | 1 | 21 |
| Other interior component (e.g., shoulder belt, steering wheel, seatback) | 3 | — | — | — | 10 |
| Transmitted load to the spine—load applied to head or limbs | |||||
| Front interior (e.g., instrument panel) | 2 | — | — | — | 2 |
| Airbag | 2 | — | — | 2 | 5 |
| Side interior (e.g., door, B-pillar, roof, roof side rail) | 5 | — | — | — | 5 |
| Other interior component (e.g., seatback) | 2 | — | — | — | 2 |
| Object exterior to vehicle (e.g., wall) | 1 | — | — | — | 1 |
| Axial loading | |||||
| Vertically through seatpan | 2 | — | — | — | 3 |
| Totalsa | 48 | 11 | 8 | 17 | 68 |
Injuries from ICS are higher than injuries in total due to multiple ICSs for some injuries.
Table 4.
Distribution of injuries by injury causation scenario
| Scenarios | Cervical | Thoracic | Lumbar | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| N | Occupants | Injuries | Occupants | Injuries | Occupants | Injuries | |
| Flexion | |||||||
| Over lap belt | 9 | — | — | 1 | 1 | 9 | 27 |
| Over shoulder belt | 7 | 5 | 11 | 3 | 4 | — | — |
| Over CRS harness | 3 | 3 | 5 | 1 | 1 | — | — |
| Lateral bending | |||||||
| Over lap belt | 2 | — | — | — | — | 2 | 2 |
| Over shoulder belt | 1 | — | 1 | — | — | 1 | — |
| Direct contact to the spine—load applied to torso | |||||||
| Side interior (e.g., door, B-pillar) | 9 | 1 | 1 | 2 | 9 | 7 | 12 |
| Other interior component (e.g., shoulder belt, steering wheel, seatback) | 3 | — | — | 3 | 7 | 2 | 3 |
| Transmitted load to the spine—load applied to head or limbs | |||||||
| Front interior (e.g., instrument panel) | 2 | 1 | 1 | — | — | 1 | 1 |
| Airbag | 2 | 2 | 7 | — | — | — | — |
| Side interior (e.g., door, B-pillar, roof, roof side rail) | 5 | 5 | 5 | — | — | — | — |
| Other interior component (e.g., seatback) | 2 | 2 | 2 | — | — | — | — |
| Object exterior to vehicle (e.g., wall) | 1 | 1 | 1 | — | — | — | — |
| Axial loading | |||||||
| Vertically through seatpan | 2 | — | — | — | — | 2 | 3 |
| Totalsa,a | 48 | 20 | 34 | 10 | 22 | 24 | 48 |
Injuries from ICS are higher than injuries in total due to multiple ICSs for some injuries.
Occupants in ICS are higher than total number occupants due to multiple injury locations for some occupants.
Table 3.
Distribution of crash directionality by injury causation scenario
| AIS 2+ spinal injuries (N) | |||||
|---|---|---|---|---|---|
|
|
|||||
| Injury causation scenario | Scenarios (N) | Rear | Front | Far-side | Near-side |
| Flexion | |||||
| Over lap belt | 9 | — | 28 | — | — |
| Over shoulder belt | 7 | — | 15 | — | — |
| Over Child Restraint System (CRS) harness | 3 | 6 | |||
| Lateral bending | |||||
| Over lap belt | 2 | 2 | |||
| Over shoulder belt | 1 | 1 | |||
| Direct contact to the spine—load applied to torso | |||||
| Side interior (e.g., door, B-pillar) | 9 | 4 | 18 | ||
| Other interior component (e.g., shoulder belt, steering wheel, seatback) | 3 | 6 | 4 | ||
| Transmitted load to the spine—load applied to head or limbs | |||||
| Front interior (e.g., instrument panel) | 2 | 1 | 1 | ||
| Airbag | 2 | 7 | |||
| Side interior (e.g., door, B-pillar, roof, roof side rail) | 5 | 1 | 4 | ||
| Other interior component (e.g., seatback) | 2 | 1 | 1 | ||
| Object exterior to vehicle (e.g., wall) | 1 | 1 | |||
| Axial loading | |||||
| Vertically through seatpan | 2 | 3 | |||
| Totalsa | 48 | 1 | 71 | 3 | 29 |
Injuries from ICS are higher than injuries in total due to multiple ICSs for some injuries.
Discussion
This case series of restrained pediatric crash occupants with spinal injuries provided insight into the patterns of causation scenarios under which these injuries occur. Spinal injuries predominantly occurred in high-speed frontal crashes of passenger cars with front-row teenage occupants who sustained non-fatal vertebral fractures from flexion over the belt or harness (seen in all ages but as the sole mechanism in younger children) or direct contact from the vehicle interior (seen mostly in teenage occupants).
The majority of the crashes were frontal (62%), which might suggest that increased excursions in crashes are needed to provide the required loads for failure of the vertebral column. This is also supported by the relatively high speed of the crashes, with an average delta V of 51 km/h, which is greater than mean delta V s in another CIREN cohort focused on more severe spinal injuries in adults (Smith et al. 2005).
Our findings show that among a restrained group of MVC occupants, spinal AIS 2+ injuries were most frequently identified in teenage drivers and passengers. This is in contrast to a prior analysis of hospital data for all child occupants in crashes, regardless of restraint or rollover status, where those <12 years old were more likely to have serious spinal injuries in crashes compared to those 12–16 years (Brown and Bilston 2009). As previously mentioned, this is likely related to the inclusion of occupants with gross restraint misuse/nonuse and rollover crashes, which were all excluded in our study. Our relative lack of younger children in this subcohort of the CIREN database may suggest that the natural flexibility (Arbogast et al. 2009; Seacrist et al. 2012) and pseudo-subluxation, defined as pronounced but normal anterior displacement of a vertebra relative to its inferior adjacent vertebra resembling injury, in the younger cohort may allow management of the crash energy without fracture or injury. Concerns about spinal injuries to children restrained in forward-facing child restraints in high-speed crashes were not supported by these data.
Although this cohort included any patients with spinal injuries, and the CIREN database has more severely injured patients in general, there were relatively few deaths, disabling spinal cord injuries, or concurrent severe head injuries. This may be due to the study sample, because unrestrained occupants and rollover crashes children were excluded. However, there is still notable morbidity for these patients. A median hospital stay of 9 days is significant for children, and many of these cases required surgery for their spinal and extremity injuries, which can predispose patients to chronic pain or infection. Additionally, vertebral fractures of any severity may lead to issues with quality of life and premature disc degeneration (Kerttula et al. 2000; Sellin et al. 2014).
The most frequent concomitant injuries were those in the lower extremities. Eight of 22 occupants with lumbar spine injury had associated pelvic injuries from either belt loading, lateral loading from the vehicle structures, or axial loads through the knee. This association may suggest that once the support structure of the lumbar spine from the pelvis is compromised, the loss of integrity in the spine may not be able to manage the crash loads adequately and fracture occurs, particularly with higher velocity crashes. However, it is also possible that these lumbar spine injuries occurred independently from (i.e., not as a direct result from) the pelvic injuries and rather from direct forces. Even with the detailed information available in CIREN, it is challenging to fully understand the etiologies of these injuries, particularly with the smaller sample size of this case series. Further laboratory research is necessary, particularly with cadaveric crash testing, in order to more comprehensively understand whether or not any such associations of pelvic and lumbar spine injuries in these crash patterns are causal. Regardless of the mechanism, these associations are consistent with prior research using CIREN that showed more frequent spine and extremity injuries in frontal crashes, versus head and thorax injuries in side-impact crashes (Brown et al. 2006). Intrusion and contact with the vehicle interior also led to spinal and extremity injuries in our case series, which was also demonstrated in a prior NASS-CDS analysis of higher severity crashes (Bilston et al. 2011).
There are notable differences in patterns of spinal injury in children when compared to adults, which is related to the anatomical development throughout childhood. Cervical vertebrae do not completely fuse until early school age, and the ligamentous structure are more lax than that of adults with corresponding increased flexibility. Additionally, the facet angles are initially horizontal with limited restriction of subluxation. Younger children also have a larger head-to-body ratio, leading to a higher location of and more severe cervical spine injuries (Clarke 2012). Consequentially, spinal cord injuries in children are more likely to occur without fracture or radiographic abnormality (Martin et al. 2004). Bilston et al. (2011) examined age effects and found that children younger than 16 years were less likely than adults to sustain spinal injuries in all crashes except in frontal crashes (where the odds were similar). Though children sustain more severe and fatal spinal cord injury compared to adults, younger occupants more likely to favorably recover from nonfatal but disabling spinal cord injuries (Clarke 2012). This is likely due to fewer comorbidities and more favorable chances to neuroplasticity in children. In this analysis, teenage occupants had mostly vertebral fractures from flexion over the lap or shoulder belt. This is similar to other analyses using CIREN data that have demonstrated the predilection for this mechanism and injury pattern in older children and young adults <30 years (Rao et al. 2014; Stein et al. 2011).
There are some potential strategies to mitigate spinal injuries in children, and these should be targeted to specific ageassociated mechanisms. Inflatable belts have the potential to mitigate cervical injuries given the protection from the bladder on the shoulder belt in a crash (Kent et al. 2011; Sundararajan et al. 2011). Similarly, head support systems primarily designed to keep children in position in their restraint could also potentially provide supplemental neck support in a crash (Lopez-Valdes et al. 2013). Modifying pretensioners and load limiters may also help reduce belt loads but possibly at the cost of increased head excursion.
This study did have limitations that should be noted. Seven of the 17 excluded cases had inadequate injury or crash details, which could have affected the patterns of injury identified. However, the available information for these cases did not otherwise differ from the included sample. Additionally, CIREN by design captures more severely injured occupants that present to a trauma center and is therefore not representative of all crashes, nor can it be used to calculate risk of injury.
This study describes the pattern of spinal injuries and causation scenarios in children and aligns with prior work showing that occupants who are restrained and in nonrollover crashes with spinal trauma sustain mostly vertebral fractures and relatively few cord injuries. Although these fractures are less disabling, they still result in hospitalization and measurable morbidity. These crashes were predominantly high-speed and in teenage occupants, which has important implications for prevention strategies and countermeasures. Future work should focus on additional means of further mitigating MVC-related spinal trauma in children while continuing to limit head excursion and resultant injuries.
Acknowledgments
We also would like to thank the reviewers at Traffic Injury Prevention for their thoughtful peer review of the manuscript drafts. The views presented are those of the authors and not necessarily the views of the NIH, CHOP, OSU, the NSF, or the IAB members.
Funding
This project was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (NIH) grant 5K08HD073241-02. The authors acknowledge the National Science Foundation (NSF) Center for Child Injury Prevention Studies at the Children’s Hospital of Philadelphia (CHOP) and the Ohio State University (OSU) for additional support this study and its Industry Advisory Board (IAB) members for their support, valuable input, and advice.
References
- Arbogast KB, Balasubramanian S, Seacrist T, et al. Comparison of kinematic responses of the head and spine for children and adults in low-speed frontal sled tests. Stapp Car Crash J. 2009;53:329–372. doi: 10.4271/2009-22-0012. [DOI] [PubMed] [Google Scholar]
- Bilston LE, Clarke EC, Brown J. Spinal injury in car crashes: crash factors and the effects of occupant age. Inj Prev. 2011;17:228–232. doi: 10.1136/ip.2010.028324. [DOI] [PubMed] [Google Scholar]
- Brown JK, Bilston LE. Spinal injury in motor vehicle crashes: elevated risk persists up to 12 years of age. Arch Dis Child. 2009;94:546–548. doi: 10.1136/adc.2008.138818. [DOI] [PubMed] [Google Scholar]
- Brown JK, Jing Y, Wang S, Ehrlich PF. Patterns of severe injury in pediatric car crash victims: Crash Injury Research Engineering Network database. J Pediatr Surg. 2006;41:362–367. doi: 10.1016/j.jpedsurg.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Cirak B, Ziegfeld S, Knight VM, et al. Spinal injuries in children. J Pediatr Surg. 2004;39:607–612. doi: 10.1016/j.jpedsurg.2003.12.011. [DOI] [PubMed] [Google Scholar]
- Clarke EC. Contrasting adult and paediatric traumatic spinal cord injuries. In: Martin AA, Jones JE, editors. Spinal Cord Injuries: Causes, Risk Factors and Management. 5th Nova Science Publishers, Inc; Hauppauge, NY: 2012. pp. 1349–1360. [Google Scholar]
- Kent R, Lopez-Valdes FJ, Dennis NJ, et al. Assessment of a three-point restraint system with a pre-tensioned lap belt and an inflatable, forcelimited shoulder belt. Stapp Car Crash J. 2011;55:141–159. doi: 10.4271/2011-22-0007. [DOI] [PubMed] [Google Scholar]
- Kerttula LI, Serlo WS, Tervonen OA, Paakko EL, Vanharanta HV. Post-traumatic findings of the spine after earlier vertebral fracture in young patients: clinical and MRI study. Spine (Phila Pa 1976) 2000;25:1104–1108. doi: 10.1097/00007632-200005010-00011. [DOI] [PubMed] [Google Scholar]
- Lopez-Valdes FJ, Forman JL, Ash JH, et al. Assessment of a head support system to prevent pediatric out-of-position: an observational study. Ann Adv Automot Med. 2013;57:297–310. [PMC free article] [PubMed] [Google Scholar]
- Martin BW, Dykes E, Lecky FE. Patterns and risks in spinal trauma. Arch Dis Child. 2004;89:860–865. doi: 10.1136/adc.2003.029223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHTSA Crash Injury Research and Engineering Network (CIREN) 2013 Available at: http://www.nhtsa.gov/CIREN. Accessed September 1, 2013. [Google Scholar]
- Polk-Williams A, Carr BG, Blinman TA, et al. Cervical spine injury in young children: a National Trauma Data Bank review. J Pediatr Surg. 2008;43:1718–1721. doi: 10.1016/j.jpedsurg.2008.06.002. [DOI] [PubMed] [Google Scholar]
- Rao RD, Berry C, Yoganandan N, Agarwal A. Occupant and crash characteristics in thoracic and lumbar spine injuries resulting from motor vehicle collisions. Spine J. 2014 doi: 10.1016/j.spinee.2014.01.038. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasouli MR, Rahimi-Movaghar V, Maheronnaghsh R, Yousefian A, Vaccaro AR. Preventing motor vehicle crashes related spine injuries in children. World J Pediatr. 2011;7:311–317. doi: 10.1007/s12519-011-0327-z. [DOI] [PubMed] [Google Scholar]
- Schneider LW, Rupp JD, Scarboro M, et al. BioTab—a new method for analyzing and documenting injury causation in motor-vehicle crashes. Traffic Inj Prev. 2011;12:256–265. doi: 10.1080/15389588.2011.560500. [DOI] [PubMed] [Google Scholar]
- Seacrist T, Saffioti J, Balasubramanian S, et al. Passive cervical spine flexion: the effect of age and gender. Clin Biomech (Bristol, Avon) 2012;27:326–333. doi: 10.1016/j.clinbiomech.2011.10.012. [DOI] [PubMed] [Google Scholar]
- Sellin JN, Shaikh K, Ryan SL, et al. Clinical outcomes of the surgical treatment of isolated unilateral facet fractures, subluxations, and dislocations in the pediatric cervical spine: report of eight cases and review of the literature. Childs Nerv Syst. 2014;30:1233–1242. doi: 10.1007/s00381-014-2395-6. [DOI] [PubMed] [Google Scholar]
- Smith JA, Siegel JH, Siddiqi SQ. Spine and spinal cord injury in motor vehicle crashes: a function of change in velocity and energy dissipation on impact with respect to the direction of crash. J Trauma. 2005;59:117–131. doi: 10.1097/01.ta.0000171534.75347.52. [DOI] [PubMed] [Google Scholar]
- Stein DM, Kufera JA, Ho SM, et al. Occupant and crash characteristics for case occupants with cervical spine injuries sustained in motor vehicle collisions. J Trauma. 2011;70:299–309. doi: 10.1097/TA.0b013e3181f8aa91. [DOI] [PubMed] [Google Scholar]
- Sundararajan S, Rouhana SW, Board D, et al. Biomechanical assessment of a rear-seat inflatable seatbelt in frontal impacts. Stapp Car Crash J. 2011;55:161–197. doi: 10.4271/2011-22-0008. [DOI] [PubMed] [Google Scholar]
- Zonfrillo MR, Durbin DR, Winston FK, Zhao H, Stineman MG. Physical disability after injury-related inpatient rehabilitation in children. Pediatrics. 2013;131:e206–213. doi: 10.1542/peds.2012-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]


