Abstract
Our objective was to obtain an in-depth understanding of autistic adults’ experiences with healthcare and their recommendations for improving care. Our academic-community partnership used a community based participatory research (CBPR) approach to conduct semi-structured, open-ended interviews with 39 autistic adults and 16 people who had experience supporting autistic adults in healthcare settings. Participants identified patient-level, autism-related factors that impact healthcare interactions, including verbal communication skills, sensory sensitivities, challenges with body awareness, slow processing speed, atypical non-verbal communication, and challenges with organization. However, the success of healthcare interactions largely depended on the interplay between patient- and provider-level factors, as well as on the larger context in which patients were receiving care. Provider-level factors included providers’ knowledge about autism in adults, incorrect assumptions about individual patients, willingness to allow written communication, use of accessible language, openness to providing other accommodations, and skill in appropriately incorporating supporters. System-level factors included the availability of supporters, complexity of the healthcare system, accessibility of healthcare facilities, and stigma about autism. Further efforts are needed to empower patients, adequately train providers, increase the accessibility of the healthcare system, and decrease discrimination.
BACKGROUND
The prevalence of autism in adults is estimated at 1% (Brugha et al., 2011). Though this prevalence is similar to that reported in younger populations, most autism research and services have focused on children, with little attention to the needs of adults (Shattuck et al., 2012). A small but growing literature identifies important gaps in healthcare services for autistic adults1. Studies have pointed to inadequate training of healthcare providers about autism in adults (Bruder et al., 2012; Kuhlthau et al., 2014), a lack of adequate healthcare transition services (Cheak-Zamora et al., 2013; Singh et al., 2008), and decreased use of medical and mental health services as autistic youth transition out of high school (Shattuck et al., 2011).
Though a stronger literature documents the cascade of healthcare disparities experienced by adults with intellectual disability (Krahn et al., 2006), less is known about the healthcare experiences of autistic adults. In our prior online survey of 209 autistic adults and 228 non-autistic adults, autistic participants reported significantly greater unmet healthcare needs, greater emergency department use, lower use of preventive services such as Papanicolaou smears, lower healthcare self-efficacy, and lower satisfaction with patient-provider communication.(Nicolaidis et al., 2013) Even less is known about why these disparities exist and how to address them. Our objective was to use a community-based participatory research (CBPR) approach to obtain an in-depth understanding of autistic adults’ experiences with healthcare and their recommendations for improving care.
Methods
Community-Academic Partnership
This study was conducted by the Academic Autism Spectrum Partnership in Research and Education (www.aaspire.org), a community-academic partnership comprised of academic researchers, autistic individuals, family members, disability services professionals, and healthcare providers. We used a CBPR approach, whereby academic and community members served as equal partners in every phase of the project. The academic and community co-principal investigators (Co-PIs, CN and DR respectively) bring overlapping perspectives: CN as a physician, health services researcher, and parent of an autistic teenager; DR as an autistic individual and systems scientist. The full team participated in choosing the research question; designing the study; creating accessible recruitment, consent, and data collection materials; interpreting findings; and co-authoring this manuscript. Details of our collaboration process are described elsewhere.(Nicolaidis et al., 2011)
Participants, recruitment, and eligibility
Our intent was to obtain rich, qualitative data from a wide range of participants who could help us understand the healthcare experiences of autistic adults. Participants had to be US residents, at least 18 years of age, and communicate in written or spoken English or American Sign Language,. Additionally, the primary sample needed to report a formal diagnosis of autism, Asperger’s, pervasive developmental disorder not otherwise specified, or autism spectrum disorder. Given the large number of autistic adults who do not have formal diagnoses (Brugha et al., 2011), we reserved four spots for individuals without a formal diagnosis who identified as being on the autism spectrum and scored 32 or higher on the Autism Quotient (Woodbury-Smith et al., 2005; Baron-Cohen et al., 2001). Our secondary sample consisted of people who had experience supporting autistic adults in healthcare settings.
Given the heterogeneity of the autism spectrum, we used maximum variation sampling (Creswell and Clark, 2011), a purposive sampling strategy which increases depth of understanding by selecting a diverse group of individuals who may have different perspectives. We purposively sampled participants to maximize diversity in age, gender, race, ethnicity, educational attainment, living situation, need for assistance with healthcare visits, Internet use, and communication mode used during healthcare visits. We recruited autistic participants from a national sample who had completed our online healthcare survey (Nicolaidis et al., 2013) and from disability agencies, autism-related organizations, group homes, local healthcare clinics, and word of mouth. We recruited supporters via local and national autism-related organizations and disability services professional groups. We oversampled supporters who noted they “had been responsible for the majority of the communication with the healthcare provider during the adult’s healthcare visit”. Our final sample of 39 autistic adults and 16 supporters had a wide range of demographic characteristics and support needs (see Tables 1 and 2.)
Table 1.
Participant Demographics, Autistic Adults (N=39)
| Interview Mode | N (%) |
|---|---|
| In-person | 10 (26%) |
| Telephone | 8 (21%) |
| 18 (46%) | |
| Instant messenger | 3 (8%) |
| Age (in years) | Mean 35 (range 19–64) |
| Gender | |
| Male | 22 (56%) |
| Female | 17 (44%) |
| Race/Ethnicity | |
| Non-Hispanic White | 25 (64%) |
| Latino | 3 (8%) |
| Multiracial | 7 (18%) |
| Asian | 1 (3%) |
| African-American | 2 (5%) |
| Native | 1 (3) |
| Healthcare Insurance | |
| None | 2 (5%) |
| Government only* | 15 (39%) |
| Private | 21 (55%) |
| Other | 1 (3%) |
| Educational Attainment | |
| High school or less | 10 (25%) |
| Some college or university | 17 (44%) |
| Bachelor’s degree | 8 (20%) |
| Graduate degree | 4 (10%) |
| Living Situation | |
| Rent/own home | 19 (49%) |
| Live in family member’s home | 15 (38%) |
| Group or foster home | 5 (13%) |
| Receives assistance from others to obtain healthcare | 21 (54%) |
| Primary Communication mode during healthcare visits | |
| Speech | 35 (87%) |
| Other (e.g. Alternative and Augmentative Communication) |
5 (13%) |
Table 2.
Participant Characteristics, Supporters (N=16)
| Interview Mode | N (%) |
|---|---|
| In-person | 7 (44%) |
| Telephone | 9 (56%) |
| Age (in years) | Mean 52 (range 28–74) |
| Gender | |
| Female | 15 (94%) |
| Male | 1 (6%) |
| Race/Ethnicity | |
| Non-Hispanic White | 15 (94%) |
|
Relationship to autistic adult(s) being supported (Could have multiple roles) |
|
| Family member | 12 (75%) |
| Disability services provider | 8 (50%) |
|
Number of autistic adults participant has supported in healthcare settings |
|
| 1 | 7 (44%) |
| 2–9 | 5 (31%) |
| 10 or more | 4 (25%) |
Data Collection and Accommodations
This study was approved by the Institutional Review Board at Oregon Health & Science University. We obtained data for purposive sampling from participants’ answers to our prior online survey (Nicolaidis et al., 2013) or a brief screening survey. We used multiple strategies to ensure the study was as accessible as possible. To accommodate communication needs, we allowed participants to choose participation mode (telephone, instant messenger, email, or in-person). Academic and community partners co-created the interview guide, with attention to making questions concrete and specific without compromising the open-ended nature of the interview. To help people understand the types of rich responses we desired, we included a preface with instructions such as “To the best of your ability, use your responses to show us a ‘mini-movie’ of your healthcare experiences. Vivid accounts can help us teach doctors how to provide better care.” We offered all participants a copy of the interview questions in advance, noting that they would also be asked follow-up questions. We encouraged participants to take breaks during interviews. For in-person interviews, we encouraged participants to have a supporter present, if desired.
Interview topics focused on positive and negative experiences with healthcare, perceptions of how being on the spectrum affected care, and recommendations for improving care. In email interviews, the interviewer sent all questions to the participant, awaited a response, and then sent follow-up emails with additional probes. In the other types of interviews, the interviewer asked a question and followed up with additional probes in real-time. The academic Principal Investigator (PI) conducted all email interviews and a portion of the other types of interviews. She trained an autistic community partner (EA) to conduct interviews with autistic participants via instant messenger, and a disability services provider to conduct the supporter and in-person autistic participant interviews.
Data analysis
We conducted a thematic analysis (Braun and Clarke, 2006), with an inductive approach, at a semantic level, using Text Analysis Markup System Software (Version 4.47, http://tamsys.sourceforge.net/). The academic and community PIs used an iterative process to create a preliminary coding scheme, code transcripts, and revise codes. They collaboratively identified common themes that had clinical or policy implications related to healthcare for autistic adults. The full team discussed preliminary findings on multiple occasions and finalized themes.
Results
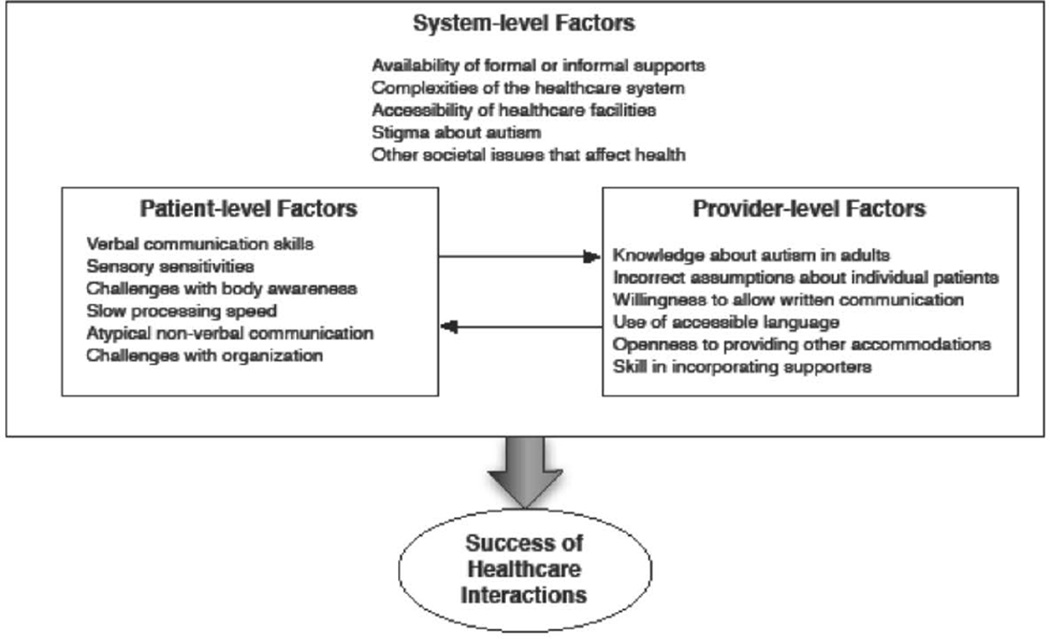
Participants expressed a wide range of satisfaction with healthcare. However, what differentiated positive and negative experiences almost always related to the interplay among patient-, provider-, and system-level factors, with patient and provider levels having direct feedback with each other while simultaneously being constrained or facilitated by the larger systems in which they operated (Figure 1). We identified common themes on each of these levels.
Figure 1.
Patient-, provider-, and system-level factors affecting the participants’ experiences with healthcare
Autism-related factors affecting healthcare
Participants identified numerous patient-level, autism-related factors that affect healthcare interactions. Challenges related to verbal communication skills were prominent across the sample, but differed in nature depending on the individual’s communication needs and strengths. For example, one supporter described how her son’s literal interpretation of language detracted from his ability to respond to questions: “They asked him, ‘On the level of one to ten, where is your pain?’ …He said, ‘Um, how do you weigh your pain?’” An autistic participant described, “It is always hard for me because I don't have the words that normal people have to communicate with. I don't always know how to respond properly to questions from health care providers.”
Sensory sensitivities were also particularly prominent. Both patients and supporters stressed that sensory sensitivities directly impacted patients’ ability to have successful healthcare interactions. An autistic participant described her experience as follows:
“The lights in the office are very bright and that is exacerbated by the white walls. Sometimes the waiting rooms are crowded and I cannot filter out the background of people talking or shuffling magazines. I feel disoriented by being led down long hallways to different rooms…. I am not able to bring up my concerns because it is all I can manage to figure out what the doctor is saying so I can respond to his questions. But he refills my usual meds and I go on my way.”
Sensory issues were not limited to sensitivities or overstimulation. Participants also often described how challenges with body awareness impacted care. For example, this participant explained, “Like when they ask if pain is shooting or stabbing or burning, it's like, I don't know, it just feels funny.” Another explained: “The problem is it is difficult for me to isolate specific sources of pain and identify duration and intensity. It's sort of like the equivalent to white noise.”
Many other known autism-related characteristics affected care, including patients' need for consistency, slow processing speed, atypical non-verbal communication, and challenges with organization. For example, a participant explained, “with my autism it is very difficult for me to understand and follow all the different appointments and procedures I have to schedule and how to do it, and no one will help me since apparently people magically become competent at these things before they turn 21.”
Provider-level factors interplaying with patient-level factors
Participants described ways in which these patient-level factors interacted dynamically with provider-level factors. Autistic adults and supporters almost uniformly complained about providers’ lack of knowledge about autism in adults. As one participant describes, “I have gotten the distinct impression that all of the physicians I have seen have had no clue what autism means or entails or how that should change how they treat me.” Or as another states, “I thought doctors would understand my autism. I thought saying, ‘well, I have autism’ would be a suitable explanation for why I have age-inappropriate troubles with managing my healthcare, but it's not.” Similarly, supporters related that they regularly had to teach providers about autism, including reminding them not to over-attribute behaviors to autism. “People attribute behaviors to the autism rather than looking for an illness first. Oh that's her autism, she's banging her head against the wall because that's her autism. Nobody thinks, ‘Oh gosh! Maybe she has a migraine!’ …They forget to realize that she can't verbally express it so she uses behavior instead.”
Participants attributed many negative experiences with healthcare to providers’ incorrect assumptions about individual patients’ skills or needs. For example, an autistic participant explained, “I have used my Alphasmart [portable communication device] when my speech is too slow or difficult to understand for medical appointments. Some of the doctors have been really great, but others have acted really condescending when I used it, also immediately assuming I couldn't be alone, had to have had parents there too … So I try to go without, even when my speech is in a poorer shape.” Or as another related, “Usually when I demonstrate a large vocabulary or some fundamentals, my needs especially around communication are then ignored. My choice is then to pretend to be less intelligent and accept their infantilism, or to be confused, frustrated, and stressed out.”
Providers’ unwillingness to allow patients to communicate in writing served as a particularly common explanation of why patients felt they had received poor care. As this patient describes, “I prefer and find it easier to communicate in text…. But with every doctor I speak to, they wave away the note-card and look at me to ask the same question I have just answered and interpret my confusion as my being non-compliant with the medicine. I wish health care providers would read the notes I make for them.” Providers also often failed to use accessible language. For example, this supporter explained, “But they talk to him in the same words that they'd use if they were talking to me…. If they're gonna talk to him… they need to say it how he can understand it.” Failure to communicate in an accessible way then often led to decreased patient autonomy. For example, an autistic participant exclaimed, “Just because I might need more information to understand things, it doesn't mean they can or should just talk to me like a child or leave me without knowledge of my own health. My body is my body, and my experiences and wishes about my body are MINE TO MAKE!”
Both patients and supporters offered many examples of how providers’ openness to considering accommodations influenced the success of healthcare interactions. For example, this supporter described a positive experience saying, “And they were very happy to accommodate all of her sensory and communication needs, including communicating with her by email ahead of time, and giving her descriptions of who would be there, what the process would be, how long it would take… I believe that they even supplied her with photographs of all of the staff and their names.”
Finally, providers’ skill in incorporating supporters greatly influenced care. Both patients and supporters described decreased patient autonomy due to healthcare providers communicating with supporters instead of patients. For example, one autistic participant explained, “The triage person kept speaking to the person who brought me rather than me. The lady could have spoken directly to me.” There were also examples from both patients and supporters of ineffective care due to providers not including supporters when they were needed or desired. Appropriate supporter involvement increased the patient's satisfaction with healthcare. For example, a participant described a positive experience by saying “[my mother] would say the things, or answer the things that I don't know--like insurance things--and I would answer other things”.
System-level factors interplaying with patient- and provider-level factors
Participants’ healthcare interactions often could not be separated from the larger context in which they lived and received care; these system-level factors surrounded and simultaneously influenced the interplay of patient- and provider-level factors. Experiences with care often appeared tied to the availability of informal or formal supports as well as to the complexities of the healthcare system. Many positive experiences had necessitated the help of family members or disability services professionals. Conversely, participants perceived lack of support as an important barrier. As one participant explained, “I wish they understood how easy it is to get confused with all the administrative hoops a patient has to jump through to get help. It sounds pathetic at my age, but I need someone to hold my hand. I don't know what I am doing. But nobody understands that I need that, and there is definitely nobody willing to do it.”
The accessibility of healthcare facilities also played an important role. Participants described negative experiences in loud, sensory-stimulating waiting rooms, and conversely attributed positive experiences to quiet offices with natural lighting or the availability of private waiting areas. As one supporter suggested, “It really doesn't take a whole lot to modify things so that you can meet the needs for most of the people on the spectrum. Right now, those offices are set up for the physicians. They are not set up for the patients.”
Participants also described how stigma about autism entered into healthcare interactions. Some autistic participants were hesitant to disclose their diagnosis to providers due to fear of discrimination: “I am very careful when it comes to disclosing my [autism] diagnosis to my healthcare providers, because I fear it's gonna affect my healthcare.” Others worried that providers would share common misconceptions about autism. For example, a participant expressed concern that providers would assume autistic individuals cannot experience empathy: “I break into tears at the drop of a hat. So what I've learned to do is to shut down. When I'm feeling empathy, I go ‘Oh, no, no, you're gonna fall apart, so shut down now. Just shut down, because you don't want to look like you're a crazy woman. So shut down.’ So instead of looking like a crazy woman… I look like a cold-hearted bitch.” Similarly, a supporter expressed her frustration with providers’ acceptance of common myths about autism. “I think one of the myths is that they are some kind of sociopaths who don't care about other people's needs. Another one is that they're dangerous people.”
Finally, autistic patients in our sample noted many challenges related to other societal issues that are well known to affect health (e.g., poverty and disparities in health insurance), which they in turn often attributed to disability-related challenges to obtaining or sustaining employment.
Recommendations for improving care
Participants offered hundreds of practical ideas for how to improve care. They almost uniformly asked for increased provider training on autism. They had many recommendations for providers, ranging from general recommendations (e.g., “respect the way I need to communicate with you”) to specific ideas for strategies and accommodations to facilitate care (e.g., "dim your lights in the exam room you take me into" or “avoid open ended or vague questions as these are often difficult to answer”). Recognizing the great heterogeneity of patients on the autism spectrum (e.g., “Each of us on the spectrum are different”), they also wanted to have a way to give providers personalized information about their accommodation needs. They urged other autistic patients and supporters to advocate for patients’ rights. Finally, participants asked for resources and information to improve their health and healthcare self-efficacy, including information on how to navigate the healthcare system, aids to help prepare for visits, tools to help follow providers’ recommendations, links to credible sources of medical information, and information about rights in healthcare.
Discussion
In trying to understand the healthcare experiences of autistic adults, we found patient-, provider-, and system-level factors together contributed to whether or not a healthcare interaction was successful. At the patient-level, the issues participants described are well-known characteristics of autism, and are included in the diagnostic criteria for Autism Spectrum Disorder (American Psychiatric Association, 2013). However, the success of healthcare interactions largely depended on providers’ knowledge, attitudes, skill, and behaviors in working with patients on the spectrum, as well as on the larger context in which patients were receiving care. The nature of the interactions between the three levels determined if patients received necessary accommodations and supports, communicated effectively, maintained autonomy, were treated with respect, and had their medical needs met. Our study advances the literature both by offering concrete illustrations of how autism characteristics can affect healthcare, and by illuminating the mechanisms that determine the degree and nature of that effect in healthcare settings.
Our prior online survey found that autistic adults experience significant healthcare disparities.(Nicolaidis et al., 2013) The current study not only helps explain why such disparities may exist, but also points to potential leverage points for improving care. One leverage point is the healthcare provider. Providers’ knowledge, attitudes, skills, and behaviors factored prominently throughout the interviews as explanations for the success of interactions. The general sense that healthcare providers lacked knowledge about autism in adults is consistent with other studies identifying gaps in provider knowledge (Bruder et al., 2012; Kuhlthau et al., 2014). However, many of the themes at the provider-level pointed to a larger issue concerning how providers approached interactions: Did they recognize a patient’s individual strengths and challenges? Were they willing or able to alter how they communicate with patients? Were they open to changing their workflow to accommodate needs? Did they treat patients with respect? Gernsbacher writes about the importance of true reciprocity in interactions with autistic individuals, noting that although autism is commonly characterized by a lack of social or emotional reciprocity, it is often clinicians, researchers, and family members who neglect the true meaning of reciprocity (Gernsbacher, 2006). Many of the provider-level themes support the notion that successful healthcare interactions depend on providers’ reciprocity; that is, their willingness and ability to modify their own behavior to meet patient needs and treat them with respect.
Participants also discussed numerous system-level factors affecting care, including the complexity of the healthcare system and the availability of formal and informal support systems. Though the pediatric patient-centered medical home has been proposed as a potential solution for providing coordinated care to children with special needs, (Cooley and Sagerman, 2011) it is unclear what that might look like in the adult healthcare world, where medical home models typically focus on the needs of patients with chronic medical conditions or high utilizers (Bitton et al., 2010). Our study highlights the importance of addressing the support and care coordination needs of autistic adults--a group that may have a particularly difficult time navigating the healthcare system.
With respect to the system-level factors around attitudes, numerous studies have explored how other forms of discrimination such as racism can impact healthcare (Shavers et al., 2012). More recently, disability studies scholars and activists have drawn attention to the discrimination experienced by autistic individuals and the ableism that exists in our society (e.g., (Billawala and Wolbring, 2014)). Our study suggests that autistic patients and supporters are concerned about how negative societal views about autism may affect care and points to a need for programs to reduce stigma and ableism.
Our study has several strengths and limitations. Our use of a CBPR approach allowed us to obtain rich, qualitative data from a wide range of autistic participants and to translate our findings into practical tools for improving care. Supplementing data from autistic individuals with data from supporters allowed us to explore healthcare issues related to individuals who may not have been able to participate in the study on their own, even with accommodations and supports. Given the many challenges with proxy reporting, we focused on the supporters’ own experiences and observations. We did not design this study to compare patient and supporter views, nor to compare results from participants with varying strengths or challenges. Similarly, we did not design the study to distinguish which findings are exclusively related to autism or to describe the scale of the problem. Instead, we focused on common themes with clinical or policy implications related to improving healthcare for autistic adults. To maximize participation and to include as diverse a sample as possible, we conducted interviews in a variety of modes. We do not feel that it distracted from the goals of our analysis, and we obtained rich information from all modes.
As with most qualitative studies, we prioritized depth of understanding over generalizability. We used a maximal variation sampling technique to maximize the richness of our data. As such, our sample does not represent a random sample of the population and there is no meaningful participation or response rate. Our sample of supporters was predominantly non-Latino white; findings may not transfer to supporters from racial and ethnic minorities. Additionally, our study was limited to participants living in the US, so results may not transfer to healthcare experiences in other countries.
Our study has important implications. First, it serves as an example of how using a CBPR approach can enable autistic individuals to participate as equal partners in all phases of a research project, and how their involvement can positively impact the relevance, accessibility, and utility of the research. Second, healthcare providers need additional training about autism in adults. Such training must focus not only on knowledge about autism, but also on the attitudes, skills, and behaviors necessary to provide respectful, effective healthcare. Trainings need to teach providers to assume competence, increase providers’ respect for autistic patients, and demonstrate the importance of offering accommodations. Trainings also need to increase practical skills, including those needed to communicate effectively with patients with communication disabilities and to appropriately incorporate supporters into healthcare interactions. Third, though participants’ recommendations were thoughtful and practical, they were specific to each person’s individual needs, highlighting the need for individualized accommodations and strategies. Fourth, our study points to the potential utility of resources, tools, and programs to increase patient self-efficacy. Fifth, our study emphasizes the need for greater system-level changes. Healthcare systems need to consider ways to make healthcare facilities and processes more accessible to autistic adults; policy-makers need to address ways to decrease healthcare inequities and increase formal supports available to autistic individuals across the entire spectrum; and, as a society, we need to find ways to decrease the stigma associated with autism and reduce discrimination.
We have used findings from this study, in combination with our team’s experience, to create a toolkit for healthcare providers, patients, and supporters available at http://autismandhealth.org. Future research is needed to test whether patient and provider tools, provider trainings, changes in care delivery systems, and policies help reduce healthcare disparities and improve health outcomes for autistic adults.
Acknowledgments
We would like to thank the study participants and all AASPIRE team members, past and present, for their invaluable insights. We also thank Angie Mejia and Marcie Tedlow for help with data collection and project coordination. We thank Jennifer Stevenson for her support during the early stages of this project. Finally, we thank the Autistic Self Advocacy Network, the Autism Society of Oregon, and many other community organizations for their help with recruitment efforts.
This study was funded by the National Institute of Mental Health (R34MH092503) and the Oregon Clinical and Translational Research Institute (OCTRI), grant number UL1 RR024140 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
We use terms such as “autistic adults” as many individuals on the autism spectrum prefer the use of identity-first language to person-first language. For more information, see http://autisticadvocacy.org/identity-first-language/.
REFERENCES
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 5th. Washington, DC: APA; 2013. [Google Scholar]
- Baron-Cohen S, Wheelwright S, Skinner R, et al. The Autism-Spectrum Quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. Journal of Autism and Developmental Disorders. 2001;31:5–17. doi: 10.1023/a:1005653411471. [DOI] [PubMed] [Google Scholar]
- Billawala A, Wolbring G. Analyzing the discourse surrounding Autism in the New York Times using an ableism lens. Disability Studies Quarterly. 2014;34 Available at: http://dsq-sds.org/article/view/3348/3524. [Google Scholar]
- Bitton A, Martin C, Landon BE. A nationwide survey of patient centered medical home demonstration projects. Journal of General Internal Medicine. 2010;25:584–592. doi: 10.1007/s11606-010-1262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. [Google Scholar]
- Bruder MB, Kerins G, Mazzarella C, et al. Brief report: the medical care of adults with autism spectrum disorders: identifying the needs. Journal of Autism and Developmental Disorders. 2012;42:2498–2504. doi: 10.1007/s10803-012-1496-x. [DOI] [PubMed] [Google Scholar]
- Brugha TS, McManus S, Bankart J, et al. Epidemiology of autism spectrum disorders in adults in the community in England. Archives of General Psychiatry. 2011;68:459–465. doi: 10.1001/archgenpsychiatry.2011.38. [DOI] [PubMed] [Google Scholar]
- Cheak-Zamora NC, Yang X, Farmer JE, et al. Disparities in transition planning for youth with autism spectrum disorder. Pediatrics. 2013;131:447–454. doi: 10.1542/peds.2012-1572. [DOI] [PubMed] [Google Scholar]
- Cooley WC, Sagerman PJ. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Clark VLP. Collecting data in mixed methods research. In: Creswell JW, Clark VLP, editors. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications; 2011. pp. 171–202. [Google Scholar]
- Gernsbacher MA. Toward a behavior of reciprocity. Journal of Developmental Processes. 2006;1:139–152. [PMC free article] [PubMed] [Google Scholar]
- Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Mental retardation and Developmental Disabilities Research Reviews. 2006;12:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- Kuhlthau KA, Warfield ME, Hurson J, et al. Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: current strategies and promising new directions. Autism. 2014 doi: 10.1177/1362361313518125. Epub ahead of print 4 February 2014. [DOI] [PubMed] [Google Scholar]
- Nicolaidis C, Raymaker D, McDonald K, et al. Collaboration strategies in non-traditional community-based participatory research partnerships: lessons from an academic–community partnership with autistic self-advocates. Progress in Community Health Partnerships. 2011;5:143–150. doi: 10.1353/cpr.2011.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis C, Raymaker D, McDonald K, et al. Comparison of healthcare experiences in autistic and non-autistic adults: a cross-sectional online survey facilitated by an academic-community partnership. Journal of general internal medicine. 2013;28:761–769. doi: 10.1007/s11606-012-2262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Roux AM, Hudson LE, et al. Services for adults with an autism spectrum disorder. Canadian Journal of Psychiatry. 2012;57:284–291. doi: 10.1177/070674371205700503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Wagner M, Narendorf S, et al. Post-high school service use among young adults with an autism spectrum disorder. Archives of Pediatrics & Adolescent Medicine. 2011;165:141–146. doi: 10.1001/archpediatrics.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL, Fagan P, Jones D, et al. The state of research on racial/ethnic discrimination in the receipt of health care. American Journal of Public Health. 2012;102:953–966. doi: 10.2105/AJPH.2012.300773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh SP, Paul M, Ford T, et al. Transitions of care from child and adolescent mental health services to adult mental health services (TRACK study): a study of protocols in Greater London. BMC Health Services Research. 2008;8:135. doi: 10.1186/1472-6963-8-135. Available at: http://www.biomedcentral.com/1472-6963/8/135/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodbury-Smith MR, Robinson J, Wheelwright S, et al. Screening adults for Asperger Syndrome using the AQ: a preliminary study of its diagnostic validity in clinical practice. Journal of Autism and Developmental Disorders. 2005;35:331–335. doi: 10.1007/s10803-005-3300-7. [DOI] [PubMed] [Google Scholar]