Abstract
The poor physical health faced by people with mental illness has been the subject of growing attention, but there has been less focus on the issue of oral health even though it is an important part of physical health. This article discusses the two-way association between oral and mental health. In one direction, the prospect of dental treatment can lead to anxiety and phobia. In the other, many psychiatric disorders, such as severe mental illness, affective disorders, and eating disorders, are associated with dental disease: These include erosion, caries, and periodontitis. Left untreated, dental diseases can lead to teeth loss such that people with severe mental illness have 2.7 times the likelihood of losing all their teeth, compared with the general population. Possible interventions include oral health assessments using standard checklists that can be completed by nondental personnel, help with oral hygiene, management of iatrogenic dry mouth, and early dental referral.
Keywords: eating disorders, anorexia nervosa, bulimia, severe mental illness, depression, oral health, dental disease, dental erosion, caries, periodontal disease
Abstract
La mauvaise santé physique qui afflige les personnes souffrant de maladie mentale a fait l’objet d’une attention croissante mais la question de la santé buccodentaire n’a pas retenu autant l’attention, même si c’est une part importante de la santé physique. Cet article de « Perspectives » discute de l’association bilatérale entre la santé buccodentaire et la santé mentale. D’un côté, la perspective d’un traitement dentaire peut entraîner l’anxiété et la phobie. De l’autre, bien des troubles psychiatriques, comme une maladie mentale grave, les troubles alimentaires et affectifs sont associés à la maladie dentaire, notamment l’érosion, les caries et les périodonties. Non traitées, les maladies dentaires peuvent mener à la perte des dents de sorte que les personnes souffrant de maladie mentale grave sont 2,7 fois plus susceptibles de perdre toutes leurs dents. Les interventions possibles sont entre autres les évaluations de la santé buccodentaire à l’aide des listes de contrôle standards qui peuvent se faire par du personnel autre que dentaire, l’aide à l’hygiène buccale, la prise en charge de la bouche sèche iatrogène, et une référence dentaire précoce.
The poor physical health faced by people with severe mental illness has been the focus of growing attention, particularly in relation to diabetes, cardiovascular disease, chronic lung disease, and cancer.1 Less attention has been paid to the issue of oral health even though it is an important part of physical health2 and is linked to many of the above chronic diseases.3–12 Poor oral health can also affect eating, speech, and other social and psychological areas of life.2 This paper reviews the association between psychological disorders and oral health and makes recommendations for management at the patient and system level.
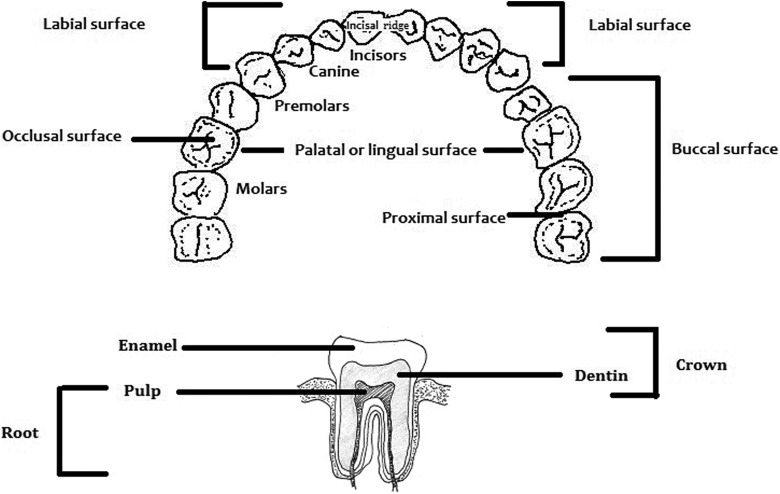
Humans have 32 permanent teeth with surfaces named according to the direction in which the surfaces face (Figure 1). Front teeth have 4 surfaces and back teeth have 5 because of the additional chewing (occlusal) area of posterior teeth (Figure 1). Each tooth is divided into the crown (the portion above the gum) and root (the portion within the gum) (Figure 1).
Figure 1.
Human dentition and tooth structure.
Before the 17th century, medical care and dental care were more or less integrated.13 Dentistry then emerged as a discrete discipline, separate from doctors, alchemists, or barbers, who regularly pulled teeth. By the late 19th century, dentistry was an independent profession in Great Britain and North America.13
A strong interaction exists between oral health and mental health. In one direction, about one half of all dental patients experience some anxiety about their dental visits, and in some cases this leads to dental phobia, a form of specific phobia.14,15 Perception of dental pain may also be exacerbated by depression or anxiety, regardless of the degree of oral pathology. For example, burning mouth syndrome is a somatic symptom disorder in people with clinically healthy oral mucosa that is often associated with depression or anxiety.16
In the other direction, psychiatric illness can lead to poor oral health, which is the focus of the present paper. People with mental illness, particularly severe mental illness, are at greater risk of oral health problems because of poor nutrition and oral hygiene; the heavy consumption of sugary drinks; comorbid substance misuse including tobacco, alcohol, or psychostimulants; and financial or other barriers to accessing dental care.17–19 Dry mouth (xerostomia) is a major risk factor for oral health problems and is often compounded by opportunistic gingivitis as a result of nutritional deficiencies secondary to psychosis or anorexia nervosa.20 Changes in salivary secretion due to parotid gland pathology have been described in patients with bulimia.21 Finally, xerostomia may be a side effect of commonly used psychotropic medications, particularly those with anticholinergic effects.21–23
The most common diseases that affect oral health are dental erosion, caries (tooth decay), and periodontal (gum) diseases. The end-stage of these is tooth loss, which can involve the whole dentition (edentulism).14 Another possible consequence of the long-term neglect of dental health is oral cancer.14 This is because oral cancer and dental disease share common risk factors such as alcohol, smoking, and, possibly, poor oral hygiene.24 Lack of dental care means that potentially cancerous lesions are not identified.14
Erosion and Caries
Dental erosion or pathological wear on tooth surfaces is defined as loss of dental tissue without the involvement of bacteria.22 This loss can be due to attrition (the action of one tooth grinding upon another, such as in bruxism), abrasion (where the surface is worn by another agent, such as a toothbrush), or erosion (where there is chemical dissolution of the tooth).14 Risk factors for the latter include the consumption of large amounts of citrus fruit, soft drinks, and sports drinks as well as the presence of gastric reflux or frequent vomiting. The pattern of erosion is described by the direction in which the tooth surface faces (Figure 1).
By contrast, dental caries is the result of bacterial action.22 Organic acids produced by microorganisms in dental plaque cause demineralisation of enamel and dentin with cavitation of specific sites on the tooth surface. Caries is assessed by the number of decayed, missing, and filled teeth or surfaces (DMFT or DMFS).25 In both, an increased score means greater decay. DMFS scores reflect damage to the surfaces of each tooth rather than counting the tooth as a single unit (Figure 1). The maximum possible DMFT is therefore 32, while the maximum DMFS is 148: (12 front teeth × 4 surfaces) + (20 back teeth × 5 surfaces) = (48 + 100) = 148.
Gum Disease
Periodontal diseases occur only in the presence of dental plaque, and they begin with gingivitis. Signs include bleeding gums and pockets where the gums become detached from the teeth. Inflammation then spreads to the periodontal ligament, with destruction of connective tissues and surrounding (alveolar) bone. In more advanced disease, there is exposure of tooth roots with destruction of the periodontal tissue (periodontitis), at which point the disease is irreversible.26 These symptoms and signs are often associated with halitosis (bad breath).
Eating Disorders
The association between eating disorders and oral health problems was initially reported in the late 1970s.27,28 The most common diagnosis is erosion due to acidic fruit and drinks, as well as the presence of gastric reflux or frequent vomiting. Between 35% and 38% of patients with eating disorders suffer from tooth erosion.29 Patients with self-induced vomiting (SIV) are most at risk, and wear is greatest on palatal surfaces (Figure 1).22,30 In a meta-analysis of 10 studies (N = 1112), patients with eating disorders had 5 times the odds of dental erosion compared with controls. In patients with SIV, the erosion rate was 7 times higher.31
Dental caries is less common than erosion partly because patients with anorexia, in particular, are more prone to obsessional personality traits and therefore more fastidious in their oral hygiene. However, a meta-analysis of 4 studies showed that patients with anorexia had significantly more decayed, missing, and filled surfaces than controls.31 Again, this was more of an issue with SIV.30,31
Mood Disorders
Attrition commonly occurs in depression largely due to comorbid issues with smoking, alcohol, and bruxism.29 High levels of tobacco and alcohol use can cause erosion through gastro-oesophageal reflux.
Patients with depression can develop caries, partly due to poor oral hygiene secondary to self-neglect and partly from xerostomia secondary to antidepressants.32,33 This again can be exacerbated by heavy caffeine and tobacco use. In addition, prostheses may no longer fit or may be lost. Poor oral health hygiene can result in total tooth loss. Using data from the Behavioural Risk Factor Surveillance System, a study of partial and full edentulism in U.S. adults showed that patients with depression were 20 to 30% more likely to have lost all their teeth.34
Patients with bipolar affective disorder face additional problems.33 In the manic phase, overzealous brushing or flossing may cause dental abrasion as well as mucosal or gingival lacerations. Lithium has been associated with xerostomia and stomatitis.23,33
Severe Mental Illnesses
People with severe mental illnesses such as dementia and schizophrenia have increased decay and gum disease as a consequence of bacterial infection rather than erosion, attrition, or abrasion. The reasons are the same as for other psychiatric disorders. These include side effects of psychotropic medication like antipsychotics, antidepressants, and mood stabilizers.35 Other contributions include barriers to dental care; alcohol, substance, and tobacco use; and diet, including the consumption of carbonated drinks.17–19
People with severe mental illnesses in Western countries have DMFT scores of more than 20, of a possible maximum of 32.36 However, DMFT scores in countries with non-Western diets such as Ethiopia and India are considerably lower.37,38 Surface (DMFS) scores (of a maximum of 148) show a similar pattern, with the highest score from Italy (88.6)39 and the lowest (2.5) from India.38
People with severe mental illnesses are more likely to have periodontal disease. In one study of psychiatric inpatients from Italy, 99% had gum diease.39 Left unchecked, periodontal decease leads to the development of pockets where the gum retreats from the tooth. In one Australian study, 59% of psychiatric outpatients had at least moderate pockets.40 In 3 further studies, 15% to 28% of inpatients had deep pockets.39,41,42 In a meta-analysis of 4 studies, patients with severe mental illness were almost 50 times as likely to have periodontal disease (95% CI, 3.43 to 702; N = 482).43
The end-stage of both untreated dental caries and periodontal disease is tooth loss, which can involve the whole dentition (edentulousness). In a meta-analysis of 25 studies, people with severe mental illness had 2.7 times the likelihood of having lost all their teeth compared with the general community.38 However, there was the suggestion that the presence of fluoride in drinking water helped to reduce the disparity between psychiatric patients and the general population.44
Implications
Forty years of data are available concerning the poor oral health of people with mental illness, yet it still remains a largely forgotten problem. Interestingly, no Canadian studies were found in 4 systematic reviews and meta-analyses of the topic. Even in countries with universal health care, coverage does not comprehensively include dental treatment. The move to care in the community may have had the unintended effect of reducing access to dental care, because many long-stay psychiatric hospitals previously had visiting dental professionals. One study reported that the need for dental care was lower in a hospital that was described as having such a dental service.45
Oral health has significant consequences for the quality of life of patients. Painful, unsightly dentition or ill-fitting dentures can exacerbate social withdrawal, isolation, and low self-esteem as well as cause problems with both speaking and eating. In addition, there is an association between dental disease, coronary heart disease, stroke, diabetes, and respiratory disease.3–12 This is partly attributable to common risk factors such as tobacco or alcohol but also results because poor oral hygiene leads to intermittent bacteraemia and secondary immune complexes that result in inflammatory responses in arteries and distal organs.12
For mental health clinicians, consideration of oral health should be part of a comprehensive assessment of people with severe mental illness. Standard checklists are available that can be completed by nondental personnel.46–48 For instance, nursing care plans for hospital admissions should include the recording of factors known to cause oral ill health, such as psychotropic medication and tobacco or substance use, as well as the supply of tooth brushes and denture baths.49 Following a patient’s discharge to the community, case management should include the identification of and referral to dentists who are willing to see people with severe mental illness. The contribution of psychotropic medication to xerostomia should be considered, monitored, and managed. Patients should be asked whether their saliva seems decreased and whether they have any trouble swallowing, speaking, or eating dry foods.50 Additional questions include the presence of lip dryness, cracking, halitosis, and mouth sores.50
Closer collaboration between mental health clinicians and dentists is important to remove barriers to care, whether these are psychosocial or financial. A dentist may be the first clinician to suspect a diagnosis of eating disorder given the reluctance of some patients to present for psychiatric treatment.20 Oral hygienists can help through education in the use of artificial salivary products (to address xerostomia), mouthwashes, and topical fluoride applications. Patients should be advised to reduce their intake of acidic drinks and citrus fruit as well as the use of alcohol and tobacco. Avoidance of caffeinated beverages reduces xerostomia, while sugar-free chewing gum helps to stimulate salivary flow. Frequent sips of water throughout the day also relieve symptoms.33 Last, patients with eating disorders should avoid vigorous brushing after SIV because the softened, demineralised surface is more susceptible to abrasion.51
Decision makers should consider providing free, accessible dental care for people with mental illness. An Australian example is the “Dental as anything” programme.40 This is an assertive outreach collaboration between mental and oral health services whereby teams take mental and oral health services to hard-to-reach settings such as rooming houses and supported residential services. At a population level, tentative findings suggest that there is less of a gap in oral health between people with severe mental illness and the general population in areas where fluoride is present in the water supply.44 Perhaps addressing the poorer oral health of marginalised sections of the community, such as those with severe mental illness, should be given greater prominence in the debate on fluoridation.
In conclusion, the increased focus on the physical health of people with severe mental illness should include consideration of oral health. Interventions should include help with oral hygiene, management of iatrogenic dry mouth, and early dental referral.
Acknowledgements
Toni Kisely contributed to the drawing of Figure 1.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Lawrence D, Jablensky AV, Holman CD, Pinder TJ. Mortality in Western Australian psychiatric patients. Soc Psychiatry Psychiatr Epidemiol. 2000;35(8):341–347. [DOI] [PubMed] [Google Scholar]
- 2. Mirza RD, Phelan M, Wulff-Cochrane V. Oral health of psychiatric in-patients. Psychiatr Bull. 2001;25:143–145. [Google Scholar]
- 3. Cullinan MP, Ford PJ, Seymour GJ. Periodontal disease and systemic health: current status. Aust Dent J. 2009;54(Suppl 1):S62–S69. [DOI] [PubMed] [Google Scholar]
- 4. Chapple IL. The impact of oral disease upon systemic health—symposium overview. J Dent. 2009;37(8):S568–S571. [DOI] [PubMed] [Google Scholar]
- 5. Haumschild MS, Haumschild RJ. The importance of oral health in long-term care. J Am Med Dir Assoc. 2009;10(9):667–671. [DOI] [PubMed] [Google Scholar]
- 6. Williams RC, Barnett AH, Claffey N, et al. The potential impact of periodontal disease on general health: a consensus view. Curr Med Res Opin. 2008;24(6):1635–1643. [DOI] [PubMed] [Google Scholar]
- 7. Humphrey LL, Fu R, Buckley DI, Freeman M, Helfand M. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med. 2008;23(12):2079–2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Desvarieux M, Demmer RT, Rundek T, et al. Relationship between periodontal disease, tooth loss, and carotid artery plaque: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Stroke. 2003;34(9):2120–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shultis WA, Weil EJ, Looker HC, et al. Effect of periodontitis on overt nephropathy and end-stage renal disease in type 2 diabetes. Diabetes Care. 2007;30(2):306–311. [DOI] [PubMed] [Google Scholar]
- 10. Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. J Periodontol. 2006;77(9):1465–1482. [DOI] [PubMed] [Google Scholar]
- 11. Rai B. Systemic effect of oral disease. The Internet Journal of Family Practice. 2006;5(1). [Google Scholar]
- 12. Scannapieco FA. Systemic effects of periodontal diseases. Dent Clin North Am. 2005;49(3):533–550. [DOI] [PubMed] [Google Scholar]
- 13. Adams T. Dentistry and medical dominance. Soc Sci Med. 1999;48(3):407–420. [DOI] [PubMed] [Google Scholar]
- 14. Cormac I, Jenkins P. Understanding the importance of oral health in psychiatric patients. Adv Psychiatr Treat. 1999;5(1):53–60. [Google Scholar]
- 15. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 16. Coculescu E, Radu A, Coculescu B. Burning mouth syndrome: a review on diagnosis and treatment. J Med Life. 2014;7(4):512–515. [PMC free article] [PubMed] [Google Scholar]
- 17. Bardow A, Nyvad B, Nauntofte B. Relationships between medication intake, complaints of dry mouth, salivary flow rate and composition, and the rate of tooth demineralization in situ. Arch Oral Biol. 2001;46(5):413–423. [DOI] [PubMed] [Google Scholar]
- 18. Lewis S, Jagger RG, Treasure E. The oral health of psychiatric in-patients in South Wales. Spec Care Dentist. 2001;21(5):182–186. [DOI] [PubMed] [Google Scholar]
- 19. Ramon T, Grinshpoon A, Zusman SP, Weizman A. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. 2003;18(3):101–105. [DOI] [PubMed] [Google Scholar]
- 20. Russo L, Campisi G, Di Fede O, et al. Oral manifestations of eating disorders: a critical review. Oral Dis. 2008;14(6):479–484. [DOI] [PubMed] [Google Scholar]
- 21. Milosevic A. Eating disorders and the dentist. Br Dent J. 1999;186(3):109–113. [DOI] [PubMed] [Google Scholar]
- 22. Bretz W. Oral profiles of bulimic women: diagnosis and management: what is the evidence? J Evid Based Dent Pract. 2002;2(4):267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Page M, Somerville-Brown L. Psychotropic drugs and dentistry. Australian Prescriber. 2007;30(4):98. [Google Scholar]
- 24. Warnakulasuriya S. Causes of oral cancer—an appraisal of controversies. Br Dent J. 2009;207(10):471–475. [DOI] [PubMed] [Google Scholar]
- 25. Slade GD, Spencer AJ, Roberts-Thomson KF. Australia’s dental generations: the national survey of adult oral health 2004-06. Canberra: Australian Institute of Health and Welfare; 2007. [Google Scholar]
- 26. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809–1820. [DOI] [PubMed] [Google Scholar]
- 27. Hellstrom I. Oral complications in anorexia nervosa. Scand J Dent Res. 1977;85(1):71–86. [DOI] [PubMed] [Google Scholar]
- 28. Hurst PS, Lacey LH, Crisp AH. Teeth, vomiting and diet: a study of the dental characteristics of seventeen anorexia nervosa patients. Postgrad Med J. 1977;53(620):298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ahmed KE. The psychology of tooth wear. Spec Care Dentist. 2013;33(1):28–34. [DOI] [PubMed] [Google Scholar]
- 30. Frydrych AM, Davies GR, McDermott BM. Eating disorders and oral health: a review of the literature. Aust Dental J. 2005;50(1):6–15. [DOI] [PubMed] [Google Scholar]
- 31. Kisely S, Baghaie H, Lalloo R, Johnson NW. A systematic review and meta-analysis of the association between poor oral health and eating disorders. Br J Psychiatry. 2015;207(4):299–305. [DOI] [PubMed] [Google Scholar]
- 32. Little JW. Dental implications of mood disorders. Gen Dent. 2004;52(5):442–450. [PubMed] [Google Scholar]
- 33. Clark DB. Dental care for the patient with bipolar disorder. J Can Dent Assoc. 2003;69(1):20–24. [PubMed] [Google Scholar]
- 34. Saman DM, Lemieux A, Arevalo O, Lutfiyya MN. A population-based study of edentulism in the US: does depression and rural residency matter after controlling for potential confounders? BMC Public Health. 2014;14(1):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lalloo R, Kisely S, Amarasinghe H, Perera R, Johnson N. Oral health of patients on psychotropic medications: a study of outpatients in Queensland. Australas Psychiatry. 2013;21(4):338–342. [DOI] [PubMed] [Google Scholar]
- 36. Adam H, Preston AJ. The oral health of individuals with dementia in nursing homes. Gerodontology. 2006;23(2):99–105. [DOI] [PubMed] [Google Scholar]
- 37. Kumar M, Chandu GN, Shafiulla MD. Oral health status and treatment needs in institutionalized psychiatric patients: one year descriptive cross sectional study. Indian J Dent Res. 2006;17(4):171–177. [DOI] [PubMed] [Google Scholar]
- 38. Kisely S, Baghaie H, Lalloo R, Siskind D, Johnson NW. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom Med. 2015;77(1):83–92. [DOI] [PubMed] [Google Scholar]
- 39. Angelillo IF, Nobile CG, Pavia M, et al. Dental health and treatment needs in institutionalized psychiatric patients in Italy. Community Dent Oral Epidemiol. 1995;23(6):360–364. [DOI] [PubMed] [Google Scholar]
- 40. Burchell A, Fembacher S, Lewis R, Neil A. “Dental as anything.” Inner south community health service dental outreach to people with a mental illness. Aust J Prim Health. 2006;12(2):75–82. [Google Scholar]
- 41. Rekha R, Hiremath SS. Oral health status and treatment requirements of confectionery workers in Bangalore city: a comparative study. Indian J Dent Res. 2002;13(3-4):161–165. [PubMed] [Google Scholar]
- 42. Tang WK, Sun FC, Ungvari GS, O’Donnell D. Oral health of psychiatric in-patients in Hong Kong. Int J Soc Psychiatry. 2004;50(2):186–191. [DOI] [PubMed] [Google Scholar]
- 43. Kisely S. A systematic review and meta-analysis of the oral health of psychiatric patients. Aust N Z J Psychiatry (Suppl). 2009;43:A30–A31. [Google Scholar]
- 44. Kisely S, Quek LH, Pais J, et al. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. 2011;199(3):187–193. [DOI] [PubMed] [Google Scholar]
- 45. Barnes GP, Allen EH, Parker WA, et al. Dental treatment needs among hospitalized adult mental patients. Spec Care Dentist. 1988;8(4):173–177. [DOI] [PubMed] [Google Scholar]
- 46. Griffiths J, Jones V, Leeman I, et al. Oral health care for people with mental health problems: guidelines and recommendations. London: British Society for Disability and Oral Health; 2000. [cited 2016 February 2]. Available from: https://www.academia.edu/7695445/Oral_Health_Care_for_People_with_Mental_Health_Problems_Guidelines_and_Recommendations [Google Scholar]
- 47. Chalmers JM, King PL, Spencer AJ, Wright FAC, Carter KD. The Oral Health Assessment Tool—validity and reliability. Aust Dent J. 2005;50(3):191–199. [DOI] [PubMed] [Google Scholar]
- 48. Chalmers JM, Spencer AJ, Carter KD, King PL, Wright C. Caring for oral health in Australian residential care: AIHW; 2009. [cited 2015 June 1]. http://www.adelaide.edu.au/arcpoh/downloads/publications/reports/dental-statistics-research-series/2009-2010-residential-care.pdf
- 49. Australian Research Centre for Population Oral Health, The University of Adelaide Oral Health Promotion Clearinghouse. Adelaide. [cited 2015 June 1]. Available from: https://www.adelaide.edu.au/oral-health-promotion/.
- 50. Swager LW, Morgan SK. Psychotropic-induced dry mouth: don’t overlook this potentially serious side effect. Curr Psychiatry. 2011;10(12):54. [Google Scholar]
- 51. Milosevic A, Slade PD. The orodental status of anorexics and bulimics. Br Dent J. 1989;167(2):66–70. [DOI] [PubMed] [Google Scholar]