Abstract
Background:
Evidence regarding longer-term psychiatric, psychological, and behavioural outcomes (for example, anxiety, mood disorders, depression, and attention disorders) following mild traumatic brain injury (mTBI) in children and adolescents has not been previously synthesized.
Objective:
To conduct a systematic review of the available evidence examining psychiatric, psychological, and behavioural outcomes following mTBI in children and adolescents.
Materials and Methods:
Nine electronic databases were systematically searched from 1980 to August 2014. Studies selected met the following criteria: original data; study design was a randomized controlled trial, quasi-experimental design, cohort or historical cohort study, case-control study, or cross-sectional study; exposure included mTBI (including concussion); population included children and adolescents (<19 years) at the time of mTBI, as well as a comparison group (for example, healthy children, children with orthopaedic injuries); and included psychiatric, psychological, or behavioural outcomes (for example, anxiety, mood disorders, depression, attention disorders). Two authors independently assessed the quality and level of evidence with the Downs and Black (DB) criteria and Oxford Centre of Evidence-Based Medicine (OCEBM) model, respectively, for each manuscript.
Results:
Of 9472 studies identified in the initial search, 30 were included and scored. Heterogeneity in methodology and injury definition precluded meta-analyses. The median methodological quality for all 30 studies, based on the DB criteria, was 15/33 (range 6 to 19). The highest level of evidence demonstrated by all reviewed studies was level 2b based on OCEBM criteria, with the majority (28/30 studies) classified at this level. Based on the literature included in this systematic review, psychological and psychiatric problems in children with a history of mTBI were found to be more prevalent when mTBI is associated with hospitalization, when assessment occurs earlier in the recovery period (that is, resolves over time), when there are multiple previous mTBIs, in individuals with preexisting psychiatric illness, when outcomes are based on retrospective recall, and when the comparison group is noninjured healthy children (as opposed to children with injuries not involving the head).
Conclusions:
Overall, few rigorous prospective studies have examined psychological, behavioural, and psychiatric outcomes following mTBI. In the absence of true reports of preinjury problems and when ideally comparing mild TBI to non-TBI injured controls, there is little evidence to suggest that psychological, behavioural, and/or psychiatric problems persist beyond the acute and subacute period following an mTBI in children and adolescents.
Keywords: mild traumatic brain injury, concussion, psychological outcomes, psychiatric outcomes, behaviour outcomes
Abstract
Contexte:
Les données probantes concernant les résultats psychiatriques, psychologiques et comportementaux à long terme (p. ex., l’anxiété, les troubles de l’humeur, la dépression, et les troubles de l’attention) par suite d’un traumatisme cranio-cérébral bénin (TCCb) chez les enfants et les adolescents n’ont pas été synthétisées antérieurement.
Objectif:
Mener une revue systématique des données probantes disponibles qui examinent les résultats psychiatriques, psychologiques et comportementaux d’un TCCb chez les enfants et les adolescents.
Matériel et méthodes:
Neuf bases de données électroniques ont été systématiquement recherchées de 1980 au mois d’août 2014. Les études retenues satisfaisaient aux critères suivants: des données originales; la méthode de l’étude était un essai randomisé contrôlé, une méthode quasi-expérimentale, une étude de cohorte ou de cohorte historique, une étude cas-témoin ou transversale; l’exposition incluse dans le TCCb (y compris la commotion); la population comprenait des enfants et adolescents (< 19 ans) au moment du TCCb, ainsi qu’un groupe de comparaison (p. ex., des enfants en santé; des enfants ayant des blessures orthopédiques); et comprenait des résultats psychiatriques, psychologiques ou comportementaux (p. ex., l’anxiété, les troubles de l’humeur, la dépression, et les troubles de l’attention). Deux auteurs ont évalué indépendamment la qualité et le niveau des données probantes à l’aide des critères de Downs et Black (DB) et du modèle Oxford Centre of Evidence-Based Medicine (OCEBM), respectivement, pour chaque manuscrit.
Résultats:
Sur les 9 472 études repérées dans la recherche initiale, 30 ont été incluses et notées. L’hétérogénéité de la méthodologie et la définition du traumatisme excluaient les méta-analyses. La qualité méthodologique moyenne pour les 30 études, selon les critères DB, était de 15/33 (écart 6-19). Le niveau le plus élevé des données probantes démontré par toutes les études examinées était le niveau 2b, selon les critères de l’OCEBM, la majorité des études (28/30) étant classées à ce niveau. D’après la littérature incluse dans cette revue systématique, les problèmes psychiatriques et psychologiques des enfants ayant des antécédents de TCCb se sont révélés plus prévalents quand le TCCb est associé à une hospitalisation, quand l’évaluation a lieu plus tôt dans la période de rétablissement (c.-à-d., qui se résout avec le temps), quand il y a de multiples TCCb passés, chez des personnes souffrant d’une maladie psychiatrique préexistante, quand les résultats sont basés sur la mémoire rétrospective, et quand le groupe de comparaison est formé d’enfants en santé non blessés (par opposition aux enfants blessés mais non à la tête).
Conclusions:
En général, peu d’études prospectives rigoureuses ont examiné les résultats psychologiques, comportementaux et psychiatriques d’un TCCb. En l’absence de rapports fiables de problèmes pré-traumatisme et en comparant idéalement des sujets ayant subi un TCCb avec des témoins n’ayant pas subi de TCC, il y a peu de données probantes qui suggèrent que les problèmes psychologiques, comportementaux et/ou psychiatriques persistent au-delà de la période aiguë et subaiguë suivant un TCCb chez les enfants et les adolescents.
Background
Mild traumatic brain injuries (mTBI), including concussions, are very common in children and adolescents and therefore pose a significant public health burden. Annually, at least 700 000 youth ages 0 to 19 years seek hospital-based medical care for TBI in the United States, and 80% to 90% of these injuries are mild in severity.1 No comparable figures are available for mTBI in Canada, but data from 8 Canadian pediatric emergency departments indicate that 1 out of every 70 to 220 visits is for concussion.2,3 Moreover, more than 500,000 youth are registered hockey players in Canada, and 10% to 20% of hockey players aged 9 to 17 years report at least 1 head injury annually.4–6 Thus, mTBI likely affects thousands of Canadian children each year.
It can be difficult to detect and diagnose mTBI. They are typically defined as injuries to the brain resulting from external physical forces and identified clinically by Glasgow Coma Scale scores of 13 to 15, disorientation or other mental status changes, loss of consciousness for no longer than 30 minutes, and/or posttraumatic amnesia lasting no longer than 24 hours.7 They may be associated with visible lesions on neuroimaging but most commonly are not.8 Common mechanisms of mTBI in children and adolescents include sport and recreation–related injury (typically referred to as sport-related concussion), falls, and motor vehicle collision.9
The outcomes of mTBI in children and adolescents have historically been controversial.10,11 Research on outcomes is imperative given the decreasing rate of hospitalization among children with mTBI.12 This trend places a substantial burden on health care providers in emergency medicine and outpatient care settings to make evidence-based decisions regarding the management of mTBI in children and adolescents.13 Accurate information about outcomes is of paramount importance for this purpose.
Although long-term deficits on standardized cognitive testing are rare following mTBI,14,15 several prospective cohort studies have shown that children with mTBI display persistent postconcussive symptoms (PCS) as compared with children with other types of injuries. PCS involve a variety of cognitive, somatic, behavioural, and emotional complaints, the most common of which include headaches, dizziness, poor concentration or memory, and moodiness. Although in most cases symptoms resolve during the first few weeks following injury, they can persist for months and sometimes years in some children. In 2 large prospective cohort studies in Alberta, 12% to 14% of children sustaining mTBI still displayed symptoms 3 months following injury.16,17
In contrast, the extent to which mTBI results in psychopathology more generally, and specifically in new-onset psychiatric disorders, remains uncertain. In previous studies, the rate of psychiatric disorders in children with mTBI has varied widely (between 10% and 100%) depending on study design.18–34 The range of new-onset disorders reported in the subset of studies that consecutively recruited children with mTBI is narrower.18–29 However, many previous studies have not included control groups. Thus, the relative risk for new-onset psychiatric disorder among children with mTBI as compared to children with injuries not involving the head or to healthy controls is not clear.
Most previous studies have also not assessed psychiatric outcomes in depth. Assessment using semistructured interviews with parent and child, supplemented by input from collateral sources such as school teachers, provides a “best estimate” diagnosis that is considered the gold standard for psychiatric evaluation.35 Few studies of pediatric mTBI have followed this procedure. Instead, the measurement of psychiatric and behavioural outcomes after mTBI has often been limited to questionnaires and rating scales, typically completed only by parents. Comprehensive reviews of psychiatric, psychological, and behavioural outcomes must necessarily encompass such studies despite their limitations.
Previous systematic reviews have examined psychosocial outcomes after paediatric TBI,36,37 but they have encompassed the entire spectrum of TBI injury severity including adult populations. We are aware of only 1 previous systematic review in the literature regarding psychiatric, psychological, and behavioural outcomes specifically in children with mTBI.38 That review was limited to 6 papers published from 2001 to 2012 that met specific eligibility criteria and were judged to be scientifically acceptable based on judgments of likelihood of bias. The authors conceded the limited evidence base in their review but concluded that most children with mTBI demonstrate a good prognosis, despite acknowledging that 3 studies concerned with psychiatric outcomes found a positive association between childhood mTBI and subsequent psychiatric diagnoses.
The objective of the current systematic review was to synthesize the available evidence regarding psychiatric, psychological, and behavioural outcomes following mTBI in children and adolescents. We intended to build on Keightley’s (2014)38 previous review by searching for all relevant studies published from 1980 to August 2014 that met a priori criteria and including all identified studies without restrictions based on judgments of risk of bias. Instead, we incorporated all studies meeting our inclusion criteria but assessed the quality and level of evidence for each. The current review adds to the literature by reporting on a broader range of studies than summarized by Keightley and her colleagues,38 thereby providing a more comprehensive picture of the extant evidence base.
Methods
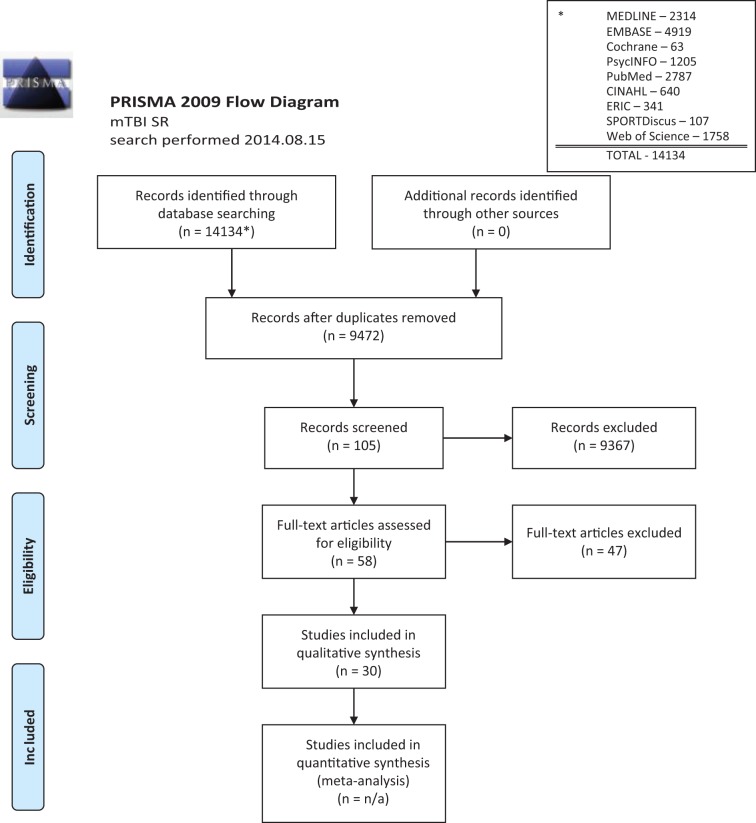
The review was conducted according to the PRISMA guidelines.39
Data Sources and Search
Relevant studies were identified by searching OVID MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, PsycINFO, PubMed, SPORTDiscus, CINAHL, ERIC, and Web of Science. All searches were conducted on August 15, 2014, using a combination of subject headings and text words (Table 1), with results limited to publication dates between 1990 and 2014 and to English language.
Table 1.
Evaluation of Psychiatric, Psychological, and Behavioural Outcomes Following Mild Traumatic Brain Injury (mTBI) in Children and Adolescents: Search Results of a Systematic Review.
| MEDLINE | EMBASE | Cochrane | PsycINFO | PubMed | CINAHL | ERIC | SPORTDiscus | WoS | |
|---|---|---|---|---|---|---|---|---|---|
| mTBI | 157 829 | 358 560 | 240 | 37 042 | — | 67 063 | 5758 | 6868 | 101 431 |
| Psychiatric, etc. | 953 102 | 1 410 394 | 3081 | 769 053 | — | 450 572 | 121 386 | 63 442 | 1 173 453 |
| Pediatric | 2 798 187 | 2 693 621 | 4492 | 690 | — | 691 292 | 92 904 | 137 093 | 1 506 614 |
| mTBI and psychiatric and pediatric | 3472 | 6723 | 63 | 690 492 | 3878 | 5250 | 364 | 110 | 1 827 |
| Limit to humans | 3404 | 6488 | — | 1912 | — | 5187 (1990–) | — | — | — |
| Limit to English | 2 862 | 5 468 | — | 1695 | — | 5177 (English) | — | 108 | 1 777 |
| Limit to 1990– | 2314 | 4919 | 63 | 1205 | 2787 | 2778 (humans) | 341 | 107 | 1 758 |
| Limit to not MEDLINE | — | — | — | — | — | 640 (not MEDLINE) | — | — | — |
| Total citations | 14 134 | ||||||||
| After duplicates removed | 9472 | ||||||||
| After screening | 105 | ||||||||
| After eligibility | 58 | ||||||||
| Articles included | 30 | ||||||||
To be included in this systematic review, the published manuscript needed to contain all necessary data, as authors were not contacted for additional data or clarification.
Study Selection
We used the following inclusion criteria: 1) The study design included randomized controlled trial, quasi-experimental design, cohort or historical cohort study, case-control study, or cross-sectional study. Systematic reviews or meta-analyses were used to identify additional relevant studies. 2) Children/adolescents were <19 years of age at the time they sustained the mTBI. 3) Brain injury severity studied was restricted to mTBI (although varying definitions were accepted, including traditional definitions such as a postresuscitation Glasgow Coma Scale score of 13 to 15, posttraumatic amnesia period of less than 24 hours, duration of loss of consciousness of less than 30 minutes). 4) Any mechanism of traumatic brain injury, including assault, with the exception of infantile nonaccidental trauma. 5) Each study must include a control or comparison population. This must be a comparable healthy population, or comparable populations with other medical conditions not involving brain injury (for example, orthopaedic injuries). 5) The study outcome must be a psychiatric, psychological, or behavioural outcome.
We used the following exclusion criteria: 1) The control population is selected for a specific psychiatric disorder or any other neurological disorder. 2) Infantile nonaccidental trauma. 3) Nontraumatic mechanisms of injury, such as inflammation, infection, or autoimmunity.
Independently and in duplicate, 2 investigators (A.V.-R. and V.G.) reviewed all potentially relevant titles after removing duplicates to determine which abstracts to review. Then, 6 investigators (B.L.B., K.M.B., C.A.E., V.G., K.S., K.O.Y.) reviewed the abstracts to select final full manuscripts for review. The abstract review was performed in pairs, with arbitration performed by a second pair.
Data Extraction and Study Rating Process
A data extraction form was used to summarize the following features of each study: study design, study location, population, exposure variable definitions (for example, mTBI and control group), psychiatric/psychological/behavioural outcome (definition), effect estimates (for example, odds ratio [OR], risk ratio, d), or other relevant statistics if no effect estimate reported. The extracted data were then reviewed for completeness and utility by 2 authors and categorized by psychiatric or behavioural outcome for use in the systematic review. Two authors (2/6 total) independently assessed the quality and level of evidence of each study. The quality of evidence was evaluated based on criteria for internal validity (study design, quality of reporting, presence of selection and misclassification bias, potential confounding) and external validity (generalizability) using the Downs and Black (DB) quality assessment tool, which assigns an individual score calculated out of 33 total points for each study (Supplemental online Table S1). The level of evidence represented by each study was categorized based on the Oxford Centre of Evidence Based Medicine (OCEBM) model.40 As per study exclusion criteria, levels 1a, 2a, 3a (systematic reviews), 4 (case series), and 5 (opinion-based papers) were not included. Discrepancies in DB scoring or OCEBM categorization were resolved first by consensus between the 2 reviewers who rated the study and, if required, by a second pair of reviewers.
Data Synthesis
Extracted data and quality and level of evidence were summarized for each study.
Results
Identification of Studies
An overview of the study identification process is provided in Figure 1. A detailed breakdown of the search process is summarized in Table 1. The initial search yielded 14 134 manuscripts; 4663 duplicates were removed, leaving 9472 potentially relevant articles. Following title and abstract review by 2 authors (A.V.-R, V.G.) to identify potential relevant records, 105 abstracts were selected and reviewed by 1 additional pair of authors (2/6 authors) for relevance and inclusion, resulting in a total of 58 full manuscripts. These 58 manuscripts were divided among 3 pairs of reviewers (6 reviewers) and further narrowed to 30 full manuscripts that were included in the systematic review based on inclusion/exclusion criteria.24,27,31,32,41–66
Figure 1.
Study Identification Process.
Study Characteristics
Characteristics of the 30 studies are summarized in Table S1. They consisted of 2 quasi-experimental, 26 cohort, and 2 case-control studies, drawn from 6 different countries. The median number of participants per study was 226 (range 48 to 3182).
Effect Estimates
Descriptions of effect estimates are presented in Table S1.
Quality and Level of Evidence
The median methodological quality score for all 30 studies, based on the DB criteria, was 15/33 (range 6 to 19). Because the included studies were primarily observational in nature, 7 items (4, 8, 14, 19, 23, 24, and 27; totalling 11 points) on the DB checklist were not applicable for 28/30 studies. Therefore, most studies could not achieve a full score. Several limitations were characteristic of most of the included studies: incomplete description of how the sample was representative of the population of interest (for example, recruitment strategy unclear), limited description of the characteristics of those lost to follow-up, use of unreliable or invalid measures (or failure to report on reliability and/or validity), insufficient reporting of how participants lost to follow-up and differing length of follow-up were accounted for in statistical analyses, inadequate sample size, and lack of adjustment for potential modification and confounding by factors such as exposure and previous injury. Further, several of the studies that report a matched design did not account for matching in their analyses.
The highest level of evidence demonstrated by all reviewed studies was level 2b (defined as an individual cohort study by the OCEBM Levels of Evidence Working Group, 2011),40 with the majority (28/30) of studies classified at this level.
Synthesis of Results
The most commonly investigated behavioural/psychological/psychiatric outcomes that were included in multiple studies were attention problems, depression and mood disorders, anxiety, oppositional defiant disorder (ODD)/disruptive behaviours, and posttraumatic stress disorder (PTSD). In addition, autism/pervasive developmental disorder, schizophrenia, and substance abuse were evaluated in 1 study each.
Attention Problems and Hyperactivity
Attention problems and hyperactivity are the most commonly studied psychological/psychiatric/behavioural outcomes of mTBI in youth. The findings are fairly consistent, with higher rates of inattentive/hyperactive symptoms reported 1) in those who are hospitalized versus not hospitalized for mTBI and 2) when comparing youth with mTBI to healthy (noninjured) controls.
Several studies reported that children and adolescents who are hospitalized for mTBI display more symptoms of inattention and hyperactivity than those who are not hospitalized or healthy controls.44,46–48 Hawley et al44 reported a relative risk of 6.34 for attention problems in youth who were hospitalized for a mTBI, but the comparison group was composed of healthy controls, and problems were reported based on parents’ retrospective recall more than 2 years after the injury.
The comparison group used for examining psychological/behavioural symptoms in children with mTBI is key for many studies, especially those focused on attention/hyperactivity. When youth with mTBI are compared with healthy noninjured controls, secondary attention-deficit hyperactivity disorder (ADHD) is found in a higher proportion of the children with mTBI (for example, Schachar et al50 reported that 36% of mTBI and 12% of noninjured controls have secondary ADHD). Youth who sustain any type of injury are more likely to display attention problems; thus, using a noninjured comparison group is likely to overestimate group differences in secondary ADHD by failing to adequately account for preinjury status. Basson et al54 found that youth who sustain multiple trauma, with or without mTBI, are more likely to have attention problems (plus other psychological issues) than youth who present to the emergency department for nontrauma medical care. Max et al45 reported that the prevalence of primary ADHD was not significantly different in a sample of youth with mTBI (5/24) and a sample of youth with an orthopaedic injury (4/24). When considering the prevalence of secondary ADHD in their sample, Max et al45 reported no significant differences between the mTBI group (3/19) and the orthopaedic injury control group (1/20), χ2(1) = 1.00, P = 0.317.
Depression/Withdrawal/Mood Problems
Both mood disorder diagnoses and elevated mood symptoms as rated on questionnaires are reported in youth with mTBI. Luis and Mittenberg27 reported that children (mean 10.5 years, SD 3.3) who were 6 months post-mTBI were 9.3 times more likely to have a diagnosis of depression, χ2(1) = 2.83, P = 0.016, compared with the orthopaedic injury control group. Hawley et al suggested that a higher relative risk (RR) for mood swings (RR 8.16, 95% CI 1.16 to 57.30),44 but not necessarily depression (RR 0.42, 95% CI 0.01 to 20.04), was found more than 2 years after mTBI.43 Young children between 4 and 6 years of age who sustain an mTBI when they are younger than 3 years are more likely to be withdrawn (OR or RR not available), although not necessarily depressed.58 Interestingly, mean symptom scores (and their standard deviations) were solidly within the broadly normal range for those with an mTBI, suggesting that significantly more symptoms in young children do not necessarily translate to clinically meaningful elevations. Trauma itself may be associated with elevations in mood symptoms,54 as is a history of multiple mTBIs.63 Despite multiple studies suggesting significantly higher symptoms of depression, mood problems, and withdrawal in children with mTBI, O’Connor et al49 reported equivocal differences between mTBI and control and Barker-Collo53 reported that children with mTBI actually had lower mood symptom ratings than the control group.
Anxiety
The evidence suggests that youth who sustain a single mTBI may be more likely to have elevated anxiety soon after their injury but not necessarily as a long-term outcome. At 6 months postinjury, Luis and Mittenberg27 reported that children with mTBI were 4.3 times more likely (95% CI 1.1 to 17.6) to have a new-onset anxiety disorder diagnosis compared with orthopaedically injured controls, χ2(1) = 6.06, P = 0.014. However, when considering long-term anxiety symptoms after an injury, children with mTBI are unlikely to have elevated levels compared with controls at 1 year53 (mTBI had fewer symptoms than controls) or 2 years43,44 (95% CIs for RR crosses 1.0) post-mTBI. Children with multiple mTBIs are 2.24 (95% CI 1.13 to 4.46) times more likely to have significantly higher levels of anxiety symptoms,63 but the sample in this study was limited to young children who were injured when very young. Similar to studies on depression/mood, the mean ratings of anxiety in Liu and Li63 were well within the broadly normal range for all groups, suggesting that significantly higher symptoms in young children do not necessarily translate to clinically meaningful elevations.
ODD/Conduct Disorder/Disruptive Behaviours
Several studies have examined disruptive behaviours in youth with mTBI, but specific diagnoses of behaviour disorders are relatively understudied. Regarding ODD and conduct disorder (CD), hospitalization for mTBI appears to be a common factor associated with these diagnoses. McKinlay and colleagues48 reported that adolescents who were previously hospitalized after mTBI were more likely than noninjured controls to have an ODD diagnosis (OR 4.9, 95% CI 1.8 to 13.4). Adolescents who were injured early in life (<5 years of age) and hospitalized for their mTBI also had significantly more problems associated with ODD/CD than those not hospitalized for their mTBI or noninjured controls, although this finding was based on symptom reporting rather than structured diagnostic interviews. Max and colleagues31 reported that adolescents with mTBI were more likely than controls to have disruptive behaviours, including 1 or more of ADHD, undifferentiated attention deficit disorder, ODD, and/or CD (OR 2.2, 95% CI 1.0 to 5.0).
Most research on disruptive behaviours in children with mTBI has considered a broad range of problems, such as elevated ratings on scales measuring broad externalizing behaviours or concerns with rage, emotional reactivity, or aggression. The existing research is mixed, however, with the presence of preinjury behavioural concerns,56,62 trauma with or without mTBI,54 multiple mTBIs,63 and hospitalization for the injury47,48 appearing to be factors associated with disruptive behaviours in children and adolescents who have sustained an mTBI.
PTSD
The limited available literature presents mixed findings regarding the presence of PTSD or its symptoms in children who sustain mTBI. Hajek et al42 reported that the likelihood of children and adolescents having elevated PTSD symptoms (parent rated) at 1 to 2 weeks, 3 months, and 12 months post-mTBI was not different from an orthopaedically injured control group, suggesting that injury in general (and not specifically mTBI) may be related to PTSD symptoms. In contrast, O’Connor et al49 reported that youth with mTBI self-reported significantly more PTSD symptoms than orthopaedically injured youth, with higher PTSD symptoms early after an injury being related to poorer school functioning at 1 and 2 years postinjury.
Autism/Pervasive Developmental Disorder
The possibility of a relationship between mTBI in youth and subsequent autism/pervasive developmental disorders has been the focus of very little research. In one study, Max and colleagues32 reported that youth who sustain mTBI are significantly less likely to have a Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised, diagnosis of autism or a pervasive developmental disorder. In children with mTBI, 3 of 64 were identified historically based on unstructured diagnostic interviewing as falling on this spectrum as compared with 10 of 64 controls, χ2(1) = 4.20, P = 0.04 (OR 3.8, 95% CI 0.9 to 18.3).
Schizophrenia
One study to date suggests that mTBI may be associated with a diagnosis of schizophrenia.41 The association seems to be present if there is a familial predisposition for the disorder. The authors also suggested that the risk of schizophrenia after mTBI is a function of age at injury, with the odds of having schizophrenia being greater if the injury occurs before 11 years of age (OR 2.35, 95% CI 1.03 to 5.36).41
Substance Abuse
Very little research has considered whether youth who sustain mTBI are more likely to have a substance abuse problem. In a cohort study that involved adolescents who had previously sustained an mTBI between 0 and 5 years of age, McKinlay et al48 reported that those who were hospitalized for the mTBI had a 3-fold increase (95% CI 1.1 to 8.5) in the likelihood of a substance abuse diagnosis using a semistructured interview (Diagnostic Interview Schedule for Children) compared with uninjured controls. However, children who were not hospitalized for their mTBI did not differ in substance abuse diagnoses.
Discussion
MTBI affects a large number of children and adolescents each year in Canada, through both sport-related and non–sport-related mechanisms. Although the vast majority of children with mTBI recover relatively quickly and with few sequelae,16,17 a small proportion displays persistent problems, often leading to a delayed return to school, a need for academic accommodations, a delayed return to sport, and an increased level of health care services. Although somatic symptoms (for example, headaches, dizziness) are often the focus following mTBI and a key marker of recovery,17,67 psychological/psychiatric recovery is also an important aspect of postinjury outcome and recovery for children and adolescents. Based on our systematic review, the evidence for increased psychological, behavioural, and psychiatric problems following a mTBI is mixed, most often based on symptom ratings (not actual diagnosis) and founded on a small number of studies characterized by multiple methodological limitations. Overall, some evidence supports an increased prevalence of psychological, behavioural, and psychiatric problems (that is, symptoms) when 1) mTBI is associated with hospitalization,48 2) the injury occurs early in life (<6 years old),48,58,63 3) outcomes are assessed earlier after injury (that is, suggesting resolution over time),27 4) there are multiple previous mTBIs,63 5) individuals have preexisting psychiatric illness,56,62 6) outcomes are based on retrospective recall,44 and 7) the comparison group is noninjured healthy children rather than children with nonhead injuries.50
A recent systematic review of psychosocial outcomes in children and adolescents with mTBI reached similar conclusions. Keightley et al38 reported an increased likelihood of psychological or psychiatric problems in the short term following a mTBI in youth (that is, specifically increased risk of mood disturbance and hyperactivity; no increased risk of PTSD) but did not find evidence for long-term psychological or psychiatric problems. Keightley et al’s systematic review contained some of the same publications as this one but was more limited in scope, including only 6 studies.38 The current systematic review was based on a wider time frame for literature searching and a broader perspective on outcome but yielded similar conclusions about early psychosocial problems that resolve with time. Previous reviews of psychosocial outcomes have suggested more long-term difficulties after pediatric TBI but have based their conclusions on studies that include children with more severe TBI, rather than limiting their review to studies specifically of mTBI.36,37
In many studies of psychological, behavioural, and psychiatric outcomes, comparison groups were composed of healthy noninjured youth. Like all research on mTBI, the comparison group is key to properly interpreting results. Studies that compare children with mTBI to healthy controls are more likely to find significantly elevated rates of psychological and psychiatric problems than studies that compare children with mTBI to children with orthopaedic injuries. The use of a healthy control group fails to control for the nonspecific effects of sustaining an injury or the risk of sustaining an injury based on preexisting risk factors. In fact, comparisons that are significant when based on a healthy control group50 may disappear when comparisons are made to controls with orthopaedic injuries (for example, Max et al45). The use of children with nonhead injuries as a comparison group represents a more appropriate and rigorous methodology for understanding outcomes following pediatric mTBI.
Another key methodological distinction should be drawn between significantly higher symptom ratings after mTBI versus significantly higher rates of psychological/psychiatric diagnoses. The former has much more support at present than the latter. The current systematic review highlighted the use of both methods for studying psychological/behavioural/psychiatric outcomes. Both are worthy methods for studying outcome, but results can differ across the 2 approaches, and the interpretation of findings varies accordingly. Significantly higher symptom ratings do not necessarily translate into clinically elevated levels of problems or formal diagnosis. For example, significantly higher levels of symptoms of withdrawal were reported for children who sustained mTBI early in life58; however, the mean scores were still well within the normal range. Similar findings were reported for anxiety symptoms in young children with multiple prior mTBIs,63 where significantly higher group means were still well within the normal range. Moreover, even when elevated, symptoms are not necessarily diagnostic, and considerable overlap exists between many psychological symptoms and the most common postconcussive symptoms. The only study comparing semistructured psychiatric interview diagnoses with questionnaire-based symptom ratings when both were administered to the same children with TBI (mild to severe) found a higher sensitivity of the former method in detecting significant psychopathology.68 These findings may be useful in guiding interpretation of clinically significant findings when questionnaire methods rather than psychiatric interviews are used to assess psychological, behavioural, and psychiatric problems.
The literature to date is insufficient for proving a causal link between mTBI and psychological/behavioural/psychiatric problems. Asking youth or their parents to provide retrospective recall of preinjury functioning, particularly at times far removed from the injury, is not a methodologically sound approach to controlling for preinjury status, as recall can be heavily influenced by retrospective biases.69,70 More research is needed to determine if psychological/behavioural/psychiatric problems are the result of an mTBI, are altered by an mTBI, are risk factors for sustaining an mTBI, or are preinjury predictors of outcome.
Limitations
Meta-analyses were not possible because of inconsistent methodology and heterogeneity of outcome measures and research design methodologies. The inclusion of English-only studies may also have led to selection bias. Inadequate reporting and control for potential confounders (for example, multiple concussion history, age, sex) may have led to bias in study results presented. In some studies, the inability to consider potential confounding was related to smaller sample sizes. Recruitment of study participants was not random in most studies, and selection bias may be associated with differences in participants selected for the study and those not selected (for example, presenting to a large emergency department vs. a primary care setting). Significant losses to follow-up also increased the likelihood of selection bias in many studies. Reliance on self-report measures and questionable validity of other measures also introduced measurement bias in many studies. Given significant concerns with internal validity, generalizability is also questionable in this body of literature.
Recommendations
More research is needed to tease out the complex interplay of preexisting and new-onset psychological/behavioural/psychiatric problems and mTBI. These studies should employ suitable control groups including children with non-TBI injuries. Further, distinctions should be made between elevated symptoms of psychological illness and psychiatric illness.
Conclusions
Although psychological, behavioural, and psychiatric problems can occur early in the recovery phase following mTBI, these resolve in most cases. Children at risk for longer-term problems are those with multiple previous mTBI or preexisting psychiatric illness.
What Are the New Findings?
Early psychological problems may occur following mTBI but appear to resolve with time.
The level of evidence of studies investigating psychological and behavioural and psychiatric outcome of pediatric mTBI is primarily level 2 evidence, largely involving historical cohort studies.
Future research should focus on high-quality prospective longitudinal cohort studies to evaluate change over time in psychological, behavioural, and psychiatric outcomes following pediatric concussion.
Supplementary Material
Footnotes
Authors’ Note: Brian L. Brooks, RPsych, PhD, is a principal investigator, co-investigator, or collaborator on several grants relating to the study of mild TBI/concussion in youth. He receives royalties for the sales of a pediatric forensic textbook and pediatric neuropsychological tests. Jeffrey E. Max, MBBCh, has received funding from the National Institutes of Health to study mTBI and provides expert testimony in cases of TBI, including mTBI, on an ad hoc basis for plaintiffs and defendants on a more or less equal ratio. This activity constitutes approximately 5% of his professional activities.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Carolyn A. Emery, PT, PhD, holds a Chair in Pediatric Rehabilitation supported by the Alberta Children’s Hospital Foundation. Keith Owen Yeates, PhD, holds a Chair in Paediatric Brain Injury supported by the Alberta Children’s Hospital Foundation. These sponsors had no involvement with respect to design, collection or data analyses, interpretation, writing or submission.
Supplemental Material: The supplemental table cited in this article is available online at http://cpa.sagepub.com/supplemental.
References
- 1. Faul M, Xu L, Wald M, et al. Traumatic brain injury in the United States: national estimates of prevalence and incidence, 2002–2006. Injury Prevention. 2010;16(Suppl 1):A268 –A. [Google Scholar]
- 2. Zemek R, Duval S, Dematteo C. Guidelines for Diagnosing and Managing Pediatric Concussion. Toronto, ON: Ontario Neurotrauma Foundation; 2014. [cited 2015]. Available from: www.onf.org/documents/guidelines-for-pediatric-concussion. [Google Scholar]
- 3. Meehan WP, Mannix R. Pediatric concussions in United States emergency departments in the years 2002 to 2006. J Pediatr. 2010;157(6):889–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Emery C, Kang J, Shrier I, et al. Risk of injury associated with bodychecking experience among youth hockey players. Can Med Assoc J. 2011;183(11):1249–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Emery CA, Kang J, Shrier I, et al. Risk of injury associated with body checking among youth ice hockey players. JAMA. 2010;303(22):2265–2272. [DOI] [PubMed] [Google Scholar]
- 6. Schneider KJ, Emery CA, Kang J, et al. Examining Sport Concussion Assessment Tool ratings for male and female youth hockey players with and without a history of concussion. British J Sports Med. 2010;44(15):1112–1117. [DOI] [PubMed] [Google Scholar]
- 7. Prins M, Greco T, Alexander D, et al. The pathophysiology of traumatic brain injury at a glance. Dis Model Mech. 2013;6(6):1307–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Osmond MH, Klassen TP, Wells GA, et al. CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. Can Med Assoc J. 2010;182(4):341–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bazarian JJ, Mcclung J, Shah MN, et al. Mild traumatic brain injury in the United States, 1998-2000. Brain Injury. 2005;19(2):85–91. [DOI] [PubMed] [Google Scholar]
- 10. McKinlay A. Controversies and outcomes associated with mild traumatic brain injury in childhood and adolescence. Child Care Health Dev. 2010;36(1):3–21. [DOI] [PubMed] [Google Scholar]
- 11. Yeates KO. Mild traumatic brain injury and postconcussive symptoms in children and adolescents. J Int Neuropsychol Soc. 2010;16(06):953–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bowman SM, Bird TM, Aitken ME, et al. Trends in hospitalizations associated with pediatric traumatic brain injuries. Pediatrics. 2008;122(5):988–993. [DOI] [PubMed] [Google Scholar]
- 13. Kamerling SN, Lutz N, Posner JC, Vanore M. Mild traumatic brain injury in children: practice guidelines for emergency department and hospitalized patients. Pediatr Emerg Care. 2003;19(6):431–440. [DOI] [PubMed] [Google Scholar]
- 14. Brooks BL, McKay CD, Mrazik M, et al. Subjective, but not objective, lingering effects of multiple past concussions in adolescents. J Neurotrauma. 2013;30(17):1469–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mannix R, Iverson GL, Maxwell B, et al. Multiple prior concussions are associated with symptoms in high school athletes. Ann Clin Transl Neurol. 2014;1(6):433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barlow KM, Crawford S, Brooks BL, et al. The incidence of postconcussion syndrome remains stable following mild traumatic brain injury in children. Pediatr Neurol. 2015;25(6):491–497. [DOI] [PubMed] [Google Scholar]
- 17. Barlow KM, Crawford S, Stevenson A, et al. Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics. 2010;126(2):e374–e381. [DOI] [PubMed] [Google Scholar]
- 18. Brown G, Chadwick O, Shaffer D, et al. A prospective study of children with head injuries: III. Psychiatric sequelae. Psychol Med. 1981;11(1):63–78. [DOI] [PubMed] [Google Scholar]
- 19. Max JE, Schachar RJ, Landis J, et al. Psychiatric disorders in children and adolescents in the first six months after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2013;25(3):187–197. [DOI] [PubMed] [Google Scholar]
- 20. Max JE, Pardo D, Hanten G, et al. Psychiatric disorders in children and adolescents six-to-twelve months after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2013;25(4):272–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Max JE, Friedman K, Wilde EA, et al. Psychiatric disorders in children and adolescents 24 months after mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2015;27(2):112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Max JE, Wilde EA, Bigler ED, et al. Psychiatric disorders after pediatric traumatic brain injury: a prospective, longitudinal, controlled study. J Neuropsychiatry Clin Neurosci. 2012;24(4):427–436. [DOI] [PubMed] [Google Scholar]
- 23. Max JE, Robin DA, Lindgren SD, et al. Traumatic brain injury in children and adolescents: psychiatric disorders at two years. J Am Acad Child Adolesc Psychiatry. 1997;36(9):1278–1285. [DOI] [PubMed] [Google Scholar]
- 24. Massagli TL, Fann JR, Burington BE, et al. Psychiatric illness after mild traumatic brain injury in children. Arch Phys Med Rehabil. 2004;85(9):1428–1434. [DOI] [PubMed] [Google Scholar]
- 25. Black P, Jeffries JJ, Blumer D, et al. The posttraumatic syndrome in children: characteristics and incidence. In: Walker AE, Caveness WF, Critchley M; Research Group on Head Injuries, editors. The late effects of head injury Springfield (IL: ): C. C. Thomas; 1969. p 142–149. [Google Scholar]
- 26. Hjern B. Acute head injuries in children: traumatology, therapy and prognosis. Stockholm, Sweden: Almqvist & Wiksells Boktryckeri AB; 1964. [Google Scholar]
- 27. Luis CA, Mittenberg W. Mood and anxiety disorders following pediatric traumatic brain injury: a prospective study. J Clin Exp Neuropsychol. 2002;24(3):270–279. [DOI] [PubMed] [Google Scholar]
- 28. Bloom DR, Levin HS, Ewing-Cobbs L, et al. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Adolesc Psychiatry. 2001;40(5):572–579. [DOI] [PubMed] [Google Scholar]
- 29. Lehmkuhl G, Thoma W. Development in children after severe head injury. In: Rothenberger A, editor. Brain and Behavior in Child Psychiatry Berlin (Germany: ): Springer-Verlag; 1990. p 267–282. [Google Scholar]
- 30. Max JE, Koele SL, Smith WL, Jr, et al. Psychiatric disorders in children and adolescents after severe traumatic brain injury: a controlled study. J Am Acad Child Adolesc Psychiatry. 1998;37(8):832–840. [DOI] [PubMed] [Google Scholar]
- 31. Max JE, Lindgren SD, Knutson C, et al. Child and adolescent traumatic brain injury: psychiatric findings from a paediatric outpatient specialty clinic. Brain Injury. 1997;11(10):699–711. [DOI] [PubMed] [Google Scholar]
- 32. Max JE, Sharma A, Qurashi MI. Traumatic brain injury in a child psychiatry inpatient population: a controlled study. J Am Acad Child Adolesc Psychiatry. 1997;36(11):1595–1601. [DOI] [PubMed] [Google Scholar]
- 33. Max JE, Dunisch DL. Traumatic brain injury in a child psychiatry outpatient clinic: a controlled study. J Am Acad Child Adolesc Psychiatry. 1997;36(3):404–411. [DOI] [PubMed] [Google Scholar]
- 34. Otto U. The postconcussion syndrome in children [in German]. Acta Paedopsychiatrica. 1960;27:6–20. [PubMed] [Google Scholar]
- 35. Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39(8):879–883. [DOI] [PubMed] [Google Scholar]
- 36. Trenchard SO, Rust S, Bunton P. A systematic review of psychosocial outcomes within 2 years of paediatric traumatic brain injury in a school-aged population. Brain Injury. 2013;27(11):1217–1237. [DOI] [PubMed] [Google Scholar]
- 37. Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev Med Child Neurol. 2013;55(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Keightley ML, Côté P, Rumney P, et al. Psychosocial consequences of mild traumatic brain injury in children: results of a systematic review by the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehab. 2014;95(3):S192–S200. [DOI] [PubMed] [Google Scholar]
- 39. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Plos Med. 2009;6(7):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Howick J, Chalmers I, Glasziou P, et al. The Oxford Levels of Evidence 2: Oxford Centre for Evidence-Based Medicine (OCEBM). Available from: http://www.cebm.net/index.aspx?o=5653.
- 41. AbdelMalik P, Husted J, Chow EW, et al. Childhood head injury and expression of schizophrenia in multiply affected families. Arch Gen Psychiatry. 2003;60(3):231–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hajek CA, Yeates KO, Gerry Taylor H, et al. Relationships among post-concussive symptoms and symptoms of PTSD in children following mild traumatic brain injury. Brain Injury. 2010;24(2):100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hawley CA. Reported problems and their resolution following mild, moderate and severe traumatic brain injury amongst children and adolescents in the UK. Brain Injury. 2003;17(2):105–129. [DOI] [PubMed] [Google Scholar]
- 44. Hawley CA, Ward AB, Magnay AR, et al. Outcomes following childhood head injury: a population study. J Neurol Neurosurg Psychiatry. 2004;75(5):737–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Max JE, Lansing AE, Koele SL, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25(1–2):159–177. [DOI] [PubMed] [Google Scholar]
- 46. McKinlay A, Dalrymple-Alford J, Horwood L, et al. Long term psychosocial outcomes after mild head injury in early childhood. J Neurol Neurosurg Psychiatry. 2002;73(3):281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. McKinlay A, Grace R, Horwood L, et al. Prevalence of traumatic brain injury among children, adolescents and young adults: prospective evidence from a birth cohort. Brain Injury. 2008;22(2):175–181. [DOI] [PubMed] [Google Scholar]
- 48. McKinlay A, Grace R, Horwood J, et al. Adolescent psychiatric symptoms following preschool childhood mild traumatic brain injury: evidence from a birth cohort. J Head Trauma Rehabil. 2009;24(3):221–227. [DOI] [PubMed] [Google Scholar]
- 49. O’Connor SS, Zatzick DF, Wang J, et al. Association between posttraumatic stress, depression, and functional impairments in adolescents 24 months after traumatic brain injury. J Trauma Stress. 2012;25(3):264–271. [DOI] [PubMed] [Google Scholar]
- 50. Schachar R, Levin HS, Max JE, et al. Attention deficit hyperactivity disorder symptoms and response inhibition after closed head injury in children: do preinjury behavior and injury severity predict outcome? Dev Neuropsychol. 2004;25(1–2):179–198. [DOI] [PubMed] [Google Scholar]
- 51. Anderson VA, Catroppa C, Dudgeon P, et al. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20(1):42. [DOI] [PubMed] [Google Scholar]
- 52. Antshel KM, Malhotra A, Seigers D. Attributions of behavior in the pediatric mild closed head injury (CHI) population. Psychol Health Med. 2007;12(1):48–63. [DOI] [PubMed] [Google Scholar]
- 53. Barker-Collo SL. Behavioural profiles and injury severity following childhood traumatic brain injury. Brain Impair. 2007;8(1):22–30. [Google Scholar]
- 54. Basson MD, Guinn JE, McElligott J, et al. Behavioral disturbances in children after trauma. J Trauma Acute Care Surg. 1991;31(10):1363–1368. [DOI] [PubMed] [Google Scholar]
- 55. Bijur PE, Haslum M, Golding J. Cognitive and behavioral sequelae of mild head injury in children. Pediatrics. 1990;86(3):337–344. [PubMed] [Google Scholar]
- 56. Catroppa C, Anderson VA, Morse SA, et al. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI). J Pediatr Psychol. 2008;33(7):707–718. [DOI] [PubMed] [Google Scholar]
- 57. Catroppa C, Crossley L, Hearps SJ, et al. Social and behavioral outcomes: pre-injury to six months following childhood traumatic brain injury. J Neurotrauma. 2015;32(2):109–115. [DOI] [PubMed] [Google Scholar]
- 58. Crowe LM, Catroppa C, Babl FE, et al. Intellectual, behavioral, and social outcomes of accidental traumatic brain injury in early childhood. Pediatrics. 2012;129(2):e262–e268. [DOI] [PubMed] [Google Scholar]
- 59. Fay GC, Jaffe KM, Polissar NL, et al. Outcome of pediatric traumatic brain injury at three years: a cohort study. Arch Phys Med Rehabil. 1994;75(7):733–741. [PubMed] [Google Scholar]
- 60. Hawley CA. Behaviour and school performance after brain injury. Brain Injury. 2004;18(7):645–659. [DOI] [PubMed] [Google Scholar]
- 61. Kaldoja M-L, Kolk A. Social-emotional behaviour in infants and toddlers with mild traumatic brain injury. Brain Injury. 2012;26(7–8):1005–1013. [DOI] [PubMed] [Google Scholar]
- 62. Light R, Asarnow R, Satz P, et al. Mild closed-head injury in children and adolescents: Behavior problems and academic outcomes. J Consult Clin Psychol. 1998;66(6):1023. [DOI] [PubMed] [Google Scholar]
- 63. Liu J, Li L. Parent-reported mild head injury history and behavioural performance in children at 6 years. Brain Injury. 2013;27(11):1263–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ponsford J, Willmott C, Rothwell A, et al. Cognitive and behavioral outcome following mild traumatic head injury in children. J Head Trauma Rehabil. 1999;14(4):360–372. [DOI] [PubMed] [Google Scholar]
- 65. Ponsford J, Willmott C, Rothwell A, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics. 2001;108(6):1297–1303. [DOI] [PubMed] [Google Scholar]
- 66. Tlustos SJ, Chiu C-YP, Walz NC, et al. Emotion labeling and socio-emotional outcomes 18 months after early childhood traumatic brain injury. J Int Neuropsychol Soc. 2011;17(06):1132–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zemek R, Osmond MH, Barrowman N. Predicting and preventing postconcussive problems in paediatrics (5P) study: protocol for a prospective multicentre clinical prediction rule derivation study in children with concussion. BMJ Open. 2013;3(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wassenberg R, Max JE, Koele SL, et al. Classifying psychiatric disorders after traumatic brain injury and orthopaedic injury in children: adequacy of K-SADS versus CBCL. Brain Injury. 2004;18(4):377–390. [DOI] [PubMed] [Google Scholar]
- 69. Brooks BL, Kadoura B, Turley B, et al. Perception of recovery after pediatric mild traumatic brain injury is influenced by the “good old days” bias: tangible implications for clinical practice and outcomes research. Arch Clin Neuropsychol. 2014;29(2):186–193. [DOI] [PubMed] [Google Scholar]
- 70. Iverson GL, Brooks BL, Holdnack JA. Misdiagnosis of cognitive impairment. In: Heilbronner R, editor. Neuropsychology in the courtroom: expert analysis of reports and testimony New York (NY: ): Guilford Press; 2008. p 243–266. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.