Abstract
Purpose
Identifying factors that contribute to optimal childhood bone development could help pinpoint strategies to improve long term bone health. A healthy diet positively influences bone health from before birth and during childhood. This study addressed a gap in the literature by examining the relationship between residential neighbourhood food environment and bone mass in infants and children.
Methods
1107 children participating in the Southampton Women’s Survey, United Kingdom, underwent measurement of bone mineral density (BMD) and bone mineral content (BMC) at birth and four and/or six years by Dual-energy X-ray Absorptiometry (DXA). Cross-sectional observational data describing food outlets within the boundary of each participant’s neighbourhood were used to derive three measures of the food environment: the counts of fast food outlets, healthy speciality stores and supermarkets.
Results
Neighbourhood exposure to fast food outlets was associated with lower BMD in infancy (β=−0.23(z-score): 95% CI −0.38, −0.08), and lower BMC after adjustment for bone area and confounding variables (β=−0.17(z-score): 95% CI −0.32, −0.02). Increasing neighbourhood exposure to healthy speciality stores was associated with higher BMD at four and six years (β=0.16(z-score): 95% CI 0.00, 0.32 and β=0.13(z-score): 95% CI −0.01, 0.26 respectively). The relationship with BMC after adjustment for bone area and confounding variables was statistically significant at four years but not at six years.
Conclusions
The neighbourhood food environment pregnant mothers and young children are exposed to may effect bone development during early childhood. If confirmed in future studies, action to reduce access to fast food outlets could have benefits for childhood development and long term bone health.
Keywords: general population studies, DXA, nutrition, developmental modelling, epidemiology
1. Introduction
There is increasing evidence that the neighbourhood food environment is an important determinant of dietary behaviour and weight status.[1,2] Across high-income countries, increasing neighbourhood deprivation has been associated with a higher density of fast food outlets.[3] There is also evidence that greater access to fast food outlets is related to higher levels of overweight and obesity, and to poorer dietary behaviours.[4,1] A recent study from the United Kingdom (UK) showed that children who lived near a large variety of fast food and takeaway outlets were more likely to be overweight or obese.[5] The results also showed that children were less likely to be overweight or obese if they had greater access to healthier food outlets, such as greengrocers (retail trader in fruit and vegetable) and butchers, within their neighbourhoods. While evidence for an association between the neighbourhood food environment and the health of children is growing, no study to date has examined how food outlet density relates to childhood bone health.
Improving the dietary behaviours of children is an important public health issue.[6-8] Dietary patterns adopted in childhood track to adolescence and into adulthood.[9,10] Furthermore, healthier dietary patterns are associated with lower risks of chronic diseases such as cardiovascular disease, type-2 diabetes and osteoporosis.[11-13] A healthy dietary pattern, including an adequate intake of protein, calcium, vitamin D, fruits and vegetables, has a positive influence on bone health.[13] The effect of diet on bone health commences early - in utero, and during infancy and childhood.[14-16] Bone growth in early life has been shown to be an important predictor of adult bone health with bone size and density tracking throughout childhood to peak bone mass achieved in early adulthood.[17,18] Peak bone mass is a major determinant of osteoporosis in later life.[19] Thus, identifying factors that contribute to less optimal childhood bone growth could lead to the development of strategies to improve long term bone health. Investigating the relationship between the local neighbourhood food environment and bone measures at several stages in early childhood will assist in developing the evidence base for the role of food environment factors on bone development.
This study aimed to address a gap in the literature by examining the relationship between the local food environment and bone mass in infancy and childhood. We explored the relationships between counts of supermarkets, healthy specialty stores (greengrocers, health food stores, farm shops and butchers) and fast food outlets (fast food chains and takeaway outlets) in children’s residential neighbourhood and their bone mineral density (BMD) and bone mineral content (BMC) at birth and four and/or six years.
2. Materials and Methods
2.1 Participants
The Southampton Women’s Survey (SWS) is a prospective cohort of 12,583 women recruited between 1998 and 2002 when aged 20-34 years. At enrolment, women were asked questions about their home postcode, smoking status (yes/no) and frequency of strenuous physical activity in the past week. Women’s dietary behaviours over the preceding three months were assessed using a 100-item food frequency questionnaire. Standardised diet scores, with a mean of zero and standard deviation of one, were developed for each woman using the prudent diet pattern method.[20] Women’s height and weight measurements were taken by trained research nurses and were used to characterise each woman’s body mass index (BMI).[21] Over three thousand (3,158) women went on to become pregnant and were followed up throughout their pregnancy. Their babies were assessed at birth and then periodically throughout childhood; sub-samples of the cohort were seen at four and six years of age. Approval for each stage of the study was obtained from the Southampton and South West Hampshire Local Research Ethics Committee.
Within two weeks of birth, a subset of 666 infants underwent a dual-energy X-ray absorptiometry (DXA) with mother’s written consent (Lunar DPX-L instrument using neonatal scan mode, GE-Lunar, Madison, Wisconsin, USA). Infants were fed and pacified prior to the scan in order to reduce any movement during the assessment.[22] The instrument underwent daily quality control, and was calibrated against a water phantom weekly. Infants were placed in a standard position on the scanner and their total BMD and total BMC were recorded. The exposure of the infant to radiation was a maximum of 8.9 microsieverts for whole body measurement, equivalent to three day’s exposure to normal background radiation. Infants’ crown-heel lengths were measured using a neonatometer (CMS Ltd, London, UK) and home postcode was reported to assess whether the family had moved since the initial interview.
At four years and six years, subsets of 555 and 703 participants respectively, underwent a whole body DXA scan with written parental consent. A Hologic Discovery instrument (Hologic Inc., Bedford, MA, US) in paediatric scan mode was used and an age appropriate DVD was shown to children to encourage compliance.[23,24] The total radiation dose was 4.7 microsieverts for whole body measurement. The child’s height was measured using a Leicester height measure (Seca Ltd.) and home postcode was reported to assess whether the family had moved since the initial interview.
2.2 Stores
A list of all food retail stores and their postcodes in six council boundaries (Southampton, Eastleigh, Fareham, Gosport, Havant, Portsmouth) within Hampshire, UK, was compiled in July and August 2010. Store information was obtained from council Food Safety Registers and on-line business directories (yellow-pages and yell.com). Between July 2010 and June 2011 trained fieldworkers ‘ground-truthed’ the study area and confirmed existence of all supermarkets, greengrocers, health food stores, farm shops (retail outlet that sells fresh produce directly from a farm), butchers and fast food chains and takeaway outlets. Fast food chains and takeaway outlets were grouped as ‘fast food outlets’, and greengrocers, health food stores, farm shops and butchers were grouped as ‘healthy speciality stores’ in a similar approach to that used in previous food environment research.[25] A count of fast food outlets, healthy speciality stores and supermarkets within the boundary of each participant’s neighbourhood was calculated.
2.3 Neighbourhood
The definition of residential neighbourhood applied in this study was Lower Super Output Area (LSOA), small areas constructed from the 2001 English census that are socially homogenous and have a population size between 1000-1500 residents.[26]
LSOAs also provide the geographical basis for neighbourhood deprivation in the UK. Home postcode reported in the initial survey was used to identify residential LSOA and level of neighbourhood deprivation in the infant models using the 2004 Index of Multiple Deprivation (IMD). Home postcode reported at four and six years was used to identify residential LSOA and level of neighbourhood deprivation, in the four and six year models, was the 2007 English Index of Deprivation (ID) ‘income domain’. The 2007 IMD was not appropriate because of circularity with the new ‘access to services domain’ which included ‘access to grocery stores’.
2.4 Statistical analysis
All analyses were cross-sectional. Analyses of BMD and BMC were limited to the subset of boys and girls who had undergone DXA scanning at birth, 4 year or 6 years (n=666, 555 and 703 respectively). BMD and BMC were standardised using z-scores to increase comparability across age groups. Participants’ characteristics were summarised using means and standard deviations (SD) for continuous variables and numbers, medians and inter-quartile range for non-normally distributed variables, and percentages for binary and categorical variables. Linear regression analysis was used to assess the relationship between the outcome measures: i) BMD and ii) BMC and the predictor variables: i) fast food outlets, ii) healthy speciality stores and iii) supermarkets. All DXA measures in infancy and six years were adjusted for age at scan. DXA measures at four years were not adjusted for age at scan because all children underwent DXA scan within close proximity of their birthday. Infant models were also adjusted for gestational age. All models for BMC were adjusted for bone area and additional adjustments was made for covariates that were considered potentially confounding factors in the relationships of interest including: child’s gender, level of neighbourhood deprivation, maternal smoking status, maternal physical activity, maternal dietary quality and maternal BMI. Size adjustment was conducted for regression models for BMC using bone area, height and weight measurements. Given the observational nature of this study, together with the substantial collinearity amongst both predictors and outcomes, testing for multiple comparisons was judged to be inappropriate. Sensitivity analyses involved comparing regression models for the total sample with those of the sub-set of participants who had not moved neighbourhood since the initial survey according to the three age groups. Differences in characteristics between the total sample and the sub-sample who had not moved neighbourhood were tested using t-tests, Fisher’s exact and Wilcoxon Rank-Sum. All statistical analyses were conducted using Stata statistical software package version 13.0.[27]
3. Results
3.1 Characteristics of study participants and food environment
In total, 1107 children (585 boys and 522 girls), residing within 225 neighbourhoods (LSOAs), had at least one DXA scan. Table 1 presents the characteristics of the children and their mothers. Girls were slightly lighter and shorter than boys at birth but weight and height between boys and girls at age four and six years were comparable. Approximately 72% did not smoke before their pregnancy, 41% had undertaken strenuous physical activity in the past week, and 59% of mothers had a healthy pre-pregnancy body mass index (20-25). The mean diet score for this sample of mothers was 0.04 (SD: 0.99). Sensitivity analyses identified few significant differences in the characteristics of children or mothers who had not moved neighbourhood since the pre-conception survey (n=345) and those who had moved neighbourhood (n=762); only maternal smoking pre-pregnancy and child weight at four years showed a significant difference between groups. Mothers who had not moved neighbourhood were less likely to smoke (p<0.001) and their children were lighter at four years than those who had moved neighbourhood (p=0.02).
Table 1. Characteristics of participants and their mothers’ by gender.
| Boys | Girls | All | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ( n (max) = 585 ) | ( n (max) = 522 ) | ( n (max) = 1107 ) | ||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| Child characteristics | ||||||||||
| Birth weight (g) | 578 | 3565.6 | 538.5 | 521 | 3402.2 | 543.4 | 1099 | 3488.1 | 546.7 | |
| Weight at 4 year (kg) | 302 | 17.5 | 2.1 | 251 | 17.5 | 2.4 | 553 | 17.5 | 2.2 | |
| Weight at 6 year (kg) | 363 | 24.1 | 3.7 | 333 | 24.3 | 4.5 | 696 | 24.2 | 4.1 | |
| Crown-heel length at birth (cm) | 568 | 50.4 | 2.1 | 510 | 49.5 | 2.1 | 1078 | 49.9 | 2.2 | |
| Height at 4 year DXA (cm) | 302 | 104.1 | 3.7 | 253 | 103.9 | 4.1 | 555 | 104 | 3.9 | |
| Height at 6 year DXA (cm) | 365 | 122 | 5.1 | 334 | 121.3 | 5.7 | 699 | 121.6 | 5.4 | |
| Mothers characteristics | ||||||||||
| Mother’s height (cm) | 576 | 163.2 | 7.1 | 512 | 162.7 | 6.9 | 1088 | 163 | 7 | |
| n | Median | Interquartile range | Median | Interquartile range | n | Median | Interquartile range | |||
| Mother’s weight (kg) | 500 | 57.2 | 52.2-63.6 | 438 | 56.7 | 50.8-61.2 | 938 | 57 | 50.8-63.0 | |
| Pre-pregnancy BMI | 578 | 24.7 | 22.3-27.7 | 519 | 24.1 | 22.0-27.2 | 1097 | 24.4 | 22.1-27.5 | |
| Frequency of strenuous exercise per week | 583 | 0.3 | 0.0-1.5 | 519 | 0.3 | 0.0-1.5 | 1102 | 0.3 | 0.0-1.5 | |
| Smoking status before pregnancy | n | % | n | % | n | % | ||||
| No | 434 | 74.2 | 367 | 70.3 | 801 | 72.4 | ||||
| Yes | 151 | 25.8 | 155 | 29.7 | 306 | 27.6 | ||||
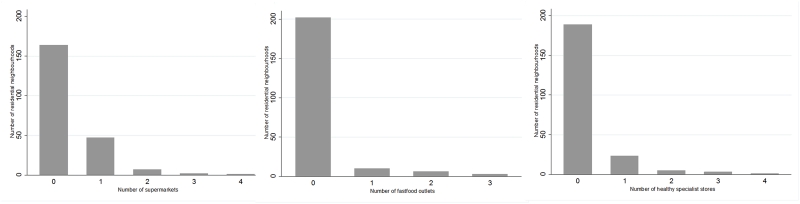
The distribution of supermarkets, healthy speciality stores and fast food outlets in neighbourhoods is shown in Figure 1. A large number of neighbourhoods had no supermarkets (n=164), healthy specialty stores (n=189) or fast food outlets (n=202). Some neighbourhoods had up to four supermarkets or healthy speciality stores; the maximum number of fast food outlets was three.
Figure 1. Frequency of supermarkets, healthy speciality stores and fast food outlets within residential neighbourhoods.
3.2 Relationship between food environment and bone mass
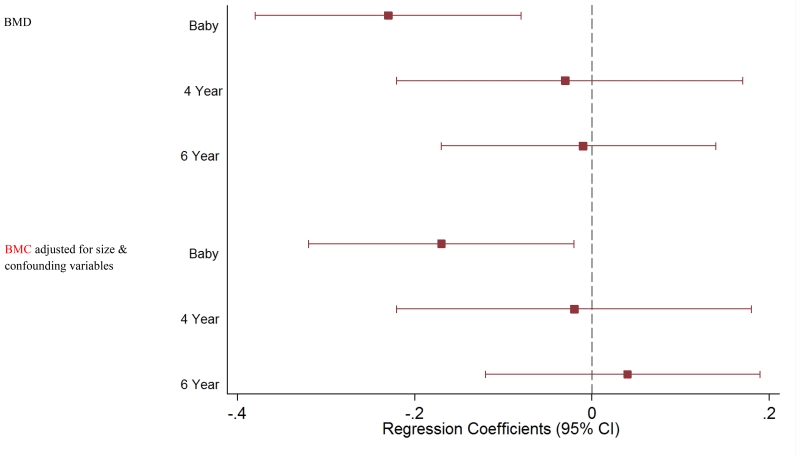
Increasing counts of fast food outlets in neighbourhoods were associated with lower BMD and BMC among infants (p<0.01 and p=0.06 respectively). Univariate regression models that were adjusted for size (BMC adjusted for bone area, height and weight) revealed a similar trend (p=0.07; Table 2). In the model where BMC was adjusted for bone area and confounding variables, each additional fast food outlet was associated with a 0.17 decrease in BMC adjusted for bone area (p=0.03; Figure 2). Associations between fast food outlet exposure and bone measures at four or six years of age were not statistically significant (p>0.1). Reanalysis using arbitrary cut-points for categorisation of number of fast food outlets (0-1 or 2-3) showed consistent results. Among participants who had not moved neighbourhood, the relationship between the number of fast food outlets and BMD among infants had a comparable effect size to the total population, however this relationship was not statistically significant (β=−0.23(z-score): 95% CI −0.53, 0.07). In this sub-group, there were no statistically significant associations between fast food outlet counts and bone measures at four or six years of age (p>0.1).
Table 2. Regression analysis assessing food environment as a predictor of bone health in the total sample.
| Bone Mineral Density | Bone Mineral Content – adjusted for bone area, height and weight | Bone Mineral Content - adjusted for bone area & confounders1 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Number within LSOA | Infant | 4 year | 6 year | Infant | 4 year | 6 year | Infant | 4 year | 6 year |
| Fast food outlets | |||||||||
| Beta | −0.23** | −0.03 | −0.01 | −0.14 | −0.07 | 0.01 | −0.17* | −0.02 | 0.04 |
| 95% C.I | (−0.38,−0.08) | (−0.22,0.17) | (−0.17,0.14) | (−0.29,0.01) | (−0.26,0.13) | (−0.14,0.17) | (−0.32,−0.02) | (−0.22,0.18) | (−0.12,0.19) |
| p-value | <0.01 | 0.78 | 0.87 | 0.07 | 0.49 | 0.88 | 0.03 | 0.85 | 0.66 |
|
| |||||||||
| Healthy specialty stores | |||||||||
| Beta | −0.03 | 0.16* | 0.13 | 0.04 | 0.16 | 0.14 | 0.00 | 0.17* | 0.11 |
| 95% C.I | (−0.18,0.11) | (−0.00,0.32) | (−0.01,0.26) | (−0.10,0.19) | (−0.01,0.32) | (0.01,0.28) | (−0.14,0.15) | (0.00,0.33) | (−0.03,0.24) |
| p-value | 0.67 | 0.05 | 0.06 | 0.58 | 0.06 | 0.03 | 0.98 | 0.05 | 0.12 |
|
| |||||||||
| Supermarkets | |||||||||
| Beta | −0.05 | 0.13 | 0.03 | −0.03 | 0.09 | 0.02 | −0.03 | 0.10 | −0.03 |
| 95% C.I | (−0.17,0.08) | (−0.01,0.28) | (−0.10,0.15) | (−0.10,0.15) | (−0.05,0.24) | (−0.11,0.15) | (−0.15,0.10) | (−0.05,0.25) | (−0.15,0.10) |
| p-value | 0.48 | 0.08 | 0.69 | 0.68 | 0.21 | 0.72 | 0.68 | 0.18 | 0.69 |
Confounding variables included: neighbourhood deprivation, maternal smoking status, maternal physical activity levels, maternal diet score, maternal body mass index (BMI) and child gender; infant models additionally adjusted for gestational age and age at scan; 6 year models additionally adjusted for age at scan.
p<0.05
p<0.01
p<0.001
Figure 2. Regression coefficients expressing the relationship between child BMD and number of fast food outlets in their neighbourhood after adjustment for size and confounding variables.
Confounding variables included: neighbourhood deprivation, maternal smoking status, maternal physical activity levels, maternal diet score, maternal body mass index (BMI) and child gender; infant models additionally adjusted for gestational age and age at scan; 6 year models additionally adjusted for age at scan.
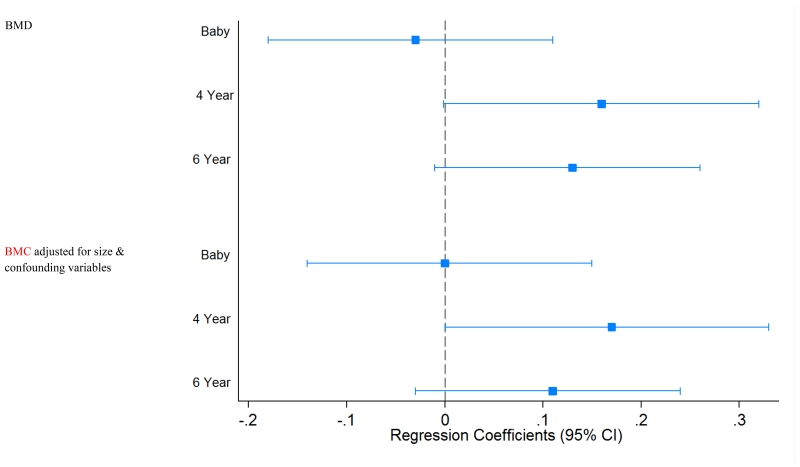
There were positive univariate relationships between the number of healthy speciality stores and DXA measures of BMD at four and six years of age (p=0.05 and p=0.06 respectively; Table 2 and Figure 3). Trends were similar in the four and six year univariate regression models that were adjusted for size (BMC adjusted for bone area, height and weight) (p=0.06 and p=0.03 respectively).The models of BMC adjusted for bone area and confounding variables showed that each additional healthy speciality store in a child’s home neighbourhood was associated with a 0.17 SD increase in BMC adjusted for bone area (p=0.05) among children aged four years. The relationship attenuated in the adjusted six year model (Table 2 and Figure 3). The sensitivity analysis showed that, among children aged four and six years who had not moved neighbourhood, associations between healthy specialty store access and BMD had comparable effect sizes to the total population however they were not statistically significant (β=0.13(z-score): 95% CI −0.18, 0.44 and β=0.11(z-score): 95% CI −0.14, 0.35 respectively).
Figure 3. Regression coefficients expressing the relationship between child BMD and number of healthy specialty stores in their neighbourhood after adjustment for size and confounding variables.
Confounding variables included: neighbourhood deprivation, maternal smoking status, maternal physical activity levels, maternal diet score, maternal body mass index (BMI) and child gender; infant models additionally adjusted for gestational age and age at scan; 6 year models additionally adjusted for age at scan.
Univariate regression analyses indicated a weak association between higher count of supermarkets in neighbourhood and greater BMD and BMC at four years of age (p=0.08 and p=0.08 respectively), however, these relationships attenuated after adjustment for confounding variables (p=0.18; Table 2). No relationships were observed in infancy or at six years of age (p>0.1). No relationships were observed in the univariate regression models that were adjusted for size (BMC adjusted for bone area, height and weight) (all p>0.1)
4. Discussion
4.1 Summary of findings
This study is the first, to the knowledge of the authors, to investigate the effects of the neighbourhood food environment on bone mass in children from birth to six years of age. Our results showed that greater access to fast food outlets within residential neighbourhoods was associated with lower BMC adjusted for bone area in infancy and remained robust after adjustment for confounding factors. There were no significant associations between fast food outlet exposure and bone measures at four or six years of age. We also found that that greater access to healthy speciality stores within residential neighbourhood, such as greengrocers, farm shops and butchers, was associated with higher BMD at four and six years of age. Findings for BMC were similar after adjustment for bone area and confounding factors at four years, though attenuated after adjustment at six years. The direction and effect sizes of these relationships between bone growth measures and count of fast food outlets and healthy speciality stores were largely consistent between children who had not moved neighbourhood since their mothers completed the initial survey and the total sample. There was little evidence that exposure to supermarkets within a child’s home neighbourhood related to their bone mass or density.
4.2 Comparison with previous research
Previous research examining the effects of the local food environment on health has largely focused on weight or dietary outcomes. Research in Australia identified no association between fruit and vegetable intake of children and the number of greengrocers within 800m radius of residential address.[28] Our study showed that a greater count of healthier specialty stores, such as greengrocers, farm shops and butchers, within residential neighbourhood was positively associated with child bone health. The Australian study also showed no relationship between supermarket accessibility in home neighbourhood and fruit and vegetable intake. Similarly, numbers of grocery stores per capita were not associated with changes in weight status of primary school children in the United States.[29] The lack of evidence for an effect of supermarket and grocery store accessibility on weight and dietary outcomes is consistent with the lack of an association between supermarket access and bone outcome measures in our study. The large variety of both healthy fresh produce and unhealthy processed food products on sale in supermarkets suggests that they can be classified as neither healthy nor unhealthy.[1] The healthy and unhealthy effects that supermarkets can have on dietary outcomes were illustrated in previous UK research which measured supermarket density per square kilometre within an 800 metre radius of home.[30] The findings of that study showed that greater density of supermarkets was associated with higher vegetable consumption but also higher intakes of sweets, sugary drinks and white bread.
More recent research in the UK examined the relationship between weight measures from the English National Child Monitoring Programme in relation to food outlet counts within Middle Super Output Areas (MSOA). MSOAs are similar to but larger than LSOAs and have a population density of approximately 7500 compared to 1500 of LSOAs. Findings showed that greater combined counts of greengrocers, butchers, supermarkets, cafes and restaurants were associated with lower rates of overweight and obesity in children aged four to five years,[5] although this relationship was not significant among children aged 10 to 11 years. Greater exposure to fast food outlets was, however, associated with increased prevalence of overweight and obesity among the older children but the opposite relationship was observed for fast food outlet exposure among the younger children. In the present study, we also found that the relationship between the local food environment and bone density differed across age groups. The strongest relationship between greater fast food exposure and lower bone density was observed in infancy, whereas relationships between greater exposure to healthy specialty stores and bone density were seen at four and six years of age.
There are a number of ways in which the neighbourhood food environment might influence bone development during childhood. Previous research has demonstrated that the quality of maternal diet during pregnancy is associated with childhood bone development such that children of mothers with better dietary quality have higher bone density at nine years of age.[15] The findings of the current study suggest that, during the preconceptional period, poorer access to fast food outlets and greater access to healthy specialty stores related to higher bone density at birth and during childhood. Thus, exposure to a more healthy food environment might optimise childhood bone development through its influence on maternal dietary quality. It is also possible that the local food environment contributes to dietary choices during childhood. A healthy diet during childhood, with adequate protein, calcium, vitamin D, fruits and vegetables, has a positive influence on bone health.[13] Mothers exposed to less healthy food environments might find it difficult to access healthy foods for their children and this in turn could lead to lead to less optimal bone development.
4.3 Strengths and limitations
A strength of this study was the consideration of both healthy and less healthy types of food outlets and the finding that these outlets have opposing associations on measures of bone growth. Another strength was the use of DXA which allowed detailed assessment of bone outcome measures. The sensitivity analysis comparing families that had moved home since the initial interview and the total sample demonstrated similar trends between groups. However, the small sample size of the group who had not moved neighbourhood was a drawback that meant that although many of the effect sizes of these relationships appeared similar, they were not statistically significant.
The use of LSOA boundaries as the area measure of residential neighbourhood is a limitation of this study. Administrative boundaries such as LSOAs and census tracts are unlikely to be entirely accurate in representing an individual’s unique spatial experience.[31] Uniform representation of environmental exposures is provided for individuals whether they reside near the centre or the boundary, and natural boundaries such as railway lines in adjacent units are not considered.[32] In addition, this study considered exposure to the neighbourhood food environment but did not have sufficient data to allow consideration of the influence of food outlets to which mothers and children may have been exposed during their daily activities such as when they are en route to school or childcare.[33-35] These limitations of using LSOA areas may have contributed to the large number of neighbourhoods within our study that had no supermarket, healthy specialty store or fast food outlet. However, associations between food outlets access and bone health were observed in this study. Further research will use the SWS participant data to examine how food outlet density in buffer zones around school and home are associated with body composition in primary school aged children. The body composition and food outlet data were collected at different time points and it is possible that the spread of food outlets may have changed from the time the women and children were surveyed. This is a common consideration in food environment research[36] and was somewhat accounted for by considering the differences in exposure-outcome associations between children who had moved neighbourhood since the initial survey was completed and those who had not. We did not examine change in food environment exposures over time and there is some evidence to suggest that food outlet locations do change.[37]
4.4 Public health implications
There has been an increased recognition that local authorities can take action to improve food environments and support their communities to make healthier food choices. For example, Public Health England in collaboration with the Local Government Association has released guidance encouraging local authorities to take action where appropriate to limit the number of fast food and takeaway outlets within their boundaries (especially near schools).[38] Some local authorities have already taken action in this area by introducing planning laws to ban outlets selling hot takeaway food within 400 metres of schools as well as putting general restrictions on the clustering of takeaways.[39] With public health responsibilities devolved to local authorities, there is real potential for more local authorities to align public health priorities with other internal sectors such as urban planning. The results of this study provide some evidence to support the introduction of zoning policies to increase the number of healthier speciality retailers within neighbourhoods and to decrease the number of fast food chains and takeaway outlets. Financial constraints may hinder the introduction of such policies, therefore further evidence from observational, intervention or natural experiment research could help to support more widespread action by local authorities.[40]
4.5 Conclusion
In conclusion, our findings suggest that the neighbourhood food environment that mothers and young children are exposed to relates to bone development during early childhood. If confirmed in further populations and in different settings, action to reduce access to fast food outlets could have benefits for childhood health and development.
Acknowledgements
We thank the mothers who gave us their time; and the team of dedicated research nurses and ancillary staff for their assistance. We also thank Miss Jamie Lawrence for her assistance ground-truthing the neighbourhood food environment. This work was supported by grants from the Medical Research Council, British Heart Foundation, Arthritis Research UK, Dunhill Medical Trust, Food Standards Agency, National Osteoporosis Society, International Osteoporosis Foundation, NIHR Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, and the European Union’s Seventh Framework Programme (FP7/2007-2013), project EarlyNutrition under grant agreement n°289346. Christina Vogel was supported by a United Kingdom National Institute for Health Research (NIHR) Doctoral Research Fellowship. The views in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health or other funders.
Footnotes
Disclosures
Christina Vogel, Camille Parsons, Sian Robinson and Hazel Inskip have no conflicts of interests to declare. Janis Baird has received grant research support from Danone Nutricia Early Life Nutrition however the study in this manuscript is not related to this relationship.
Keith Godfrey has received reimbursement for speaking at conferences sponsored by companies selling nutritional products, and is part of an academic consortium that has received research funding from Abbott Nutrition, Nestec and Danone. Nicholas Harvey has received consultancy, lecture fees and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, Consilient Healthcare and Internis Pharma. Cyrus Cooper has received consultancy, lecture fees and honoraria from AMGEN, GSK, Alliance for Better Bone Health, MSD, Eli Lilly, Pfizer, Novartis, Servier, Medtronic and Roche.
References
- 1.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health & Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holsten JE. Obesity and the community food environment: a systematic review. Public Health Nutr. 2009;12(3):397–405. doi: 10.1017/S1368980008002267. [DOI] [PubMed] [Google Scholar]
- 3.Black C, Moon G, Baird J. Dietary inequalities: What is the evidence for the effect of the neighbourhood food environment? Health & Place. 2014;27:229–242. doi: 10.1016/j.healthplace.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fraser LK, Edwards KL, Cade J, Clarke GP. The geography of Fast Food outlets: a review. International Journal of Environmental Research & Public Health. 2010;7(5):2290–2308. doi: 10.3390/ijerph7052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cetateanu A, Jones A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: Evidence from a cross sectional England-wide study. Health & Place. 2014;27C:68–76. doi: 10.1016/j.healthplace.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health UK . Healthy Lives, Healthy People: Our strategy for public health in England. London: 2010. [Google Scholar]
- 7.Department of Health UK [Accessed 6/10/2013];Reducing obesity and improving diet. 2013 https://www.gov.uk/government/policies/reducing-obesity-and-improving-diet. 2013.
- 8.US National Institutes of Health . Strategic Plan for NIH Obesity Research. Washington DC: 2011. [Google Scholar]
- 9.Northstone K, Emmett PM. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. The British journal of nutrition. 2008;100(5):1069–1076. doi: 10.1017/S0007114508968264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mikkila V, Rasanen L, Raitakari OT, Pietinen P, Viikari J. Consistent dietary patterns identified from childhood to adulthood: the cardiovascular risk in Young Finns Study. The British journal of nutrition. 2005;93(6):923–931. doi: 10.1079/bjn20051418. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation . Diet, Nutrition and the Prevention of Chronic Disease: Report of a joint WHO/FAO Expert Consultation. Geneva: 2003. WHO Technical Report Series. [Google Scholar]
- 12.Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020; World Health Organisation European Ministerial Conference; Regional Office for Europe. 2013. [Google Scholar]
- 13.Levis S, Lagari VS. The role of diet in osteoporosis prevention and management. Current osteoporosis reports. 2012;10(4):296–302. doi: 10.1007/s11914-012-0119-y. [DOI] [PubMed] [Google Scholar]
- 14.Devlin MJ, Bouxsein ML. Influence of pre- and peri-natal nutrition on skeletal acquisition and maintenance. Bone. 2012;50(2):444–451. doi: 10.1016/j.bone.2011.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole ZA, Gale CR, Javaid MK, Robinson SM, Law C, Boucher BJ, Crozier SR, Godfrey KM, Dennison EM, Cooper C. Maternal dietary patterns during pregnancy and childhood bone mass: a longitudinal study. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2009;24(4):663–668. doi: 10.1359/jbmr.081212. [DOI] [PubMed] [Google Scholar]
- 16.Cashman KD. Diet, nutrition, and bone health. J Nutr. 2007;137(11 Suppl):2507S–2512S. doi: 10.1093/jn/137.11.2507S. [DOI] [PubMed] [Google Scholar]
- 17.Cooper C, Cawley M, Bhalla A, Egger P, Ring F, Morton L, Barker D. Childhood growth, physical activity, and peak bone mass in women. JBone MinerRes. 1995;10(6):940–947. doi: 10.1002/jbmr.5650100615. [DOI] [PubMed] [Google Scholar]
- 18.Dennison EM, Syddall HE, Sayer AA, Gilbody HJ, Cooper C. Birth weight and weight at 1 year are independent determinants of bone mass in the seventh decade: the Hertfordshire cohort study. PediatrRes. 2005;57(4):582–586. doi: 10.1203/01.PDR.0000155754.67821.CA. [DOI] [PubMed] [Google Scholar]
- 19.Hernandez CJ, Beaupre GS, Carter DR. A theoretical analysis of the relative influences of peak BMD, age-related bone loss and menopause on the development of osteoporosis. OsteoporosInt. 2003;14(10):843–847. doi: 10.1007/s00198-003-1454-8. [DOI] [PubMed] [Google Scholar]
- 20.Robinson SM, Crozier SR, Borland SE, Hammond J, Barker DJ, Inskip HM. Impact of educational attainment on the quality of young women’s diets. European Journal of Clinical Nutrition. 2004;58(8):1174–1180. doi: 10.1038/sj.ejcn.1601946. [DOI] [PubMed] [Google Scholar]
- 21.Inskip HM, Godfrey KM, Robinson SM, Law CM, Barker DJ, Cooper C. Cohort profile: The Southampton Women’s Survey. IntJEpidemiol. 2006;35(1):42–48. doi: 10.1093/ije/dyi202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harvey NC, Javaid MK, Poole JR, Taylor P, Robinson SM, Inskip HM, Godfrey KM, Cooper C, Dennison EM. Paternal skeletal size predicts intrauterine bone mineral accrual. JClinEndocrinolMetab. 2008;93(5):1676–1681. doi: 10.1210/jc.2007-0279. [DOI] [PubMed] [Google Scholar]
- 23.Crozier SR, Harvey NC, Inskip HM, Godfrey KM, Cooper C, Robinson SM. Maternal vitamin D status in pregnancy is associated with adiposity in the offspring: findings from the Southampton Women’s Survey. American Journal of Clinical Nutrition. 2012;96(1):57–63. doi: 10.3945/ajcn.112.037473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harvey NC, Mahon PA, Kim M, Cole ZA, Robinson SM, Javaid K, Inskip HM, Godfrey KM, Dennison EM, Cooper C. Intrauterine growth and postnatal skeletal development: findings from the Southampton Women’s Survey. PaediatrPerinatEpidemiol. 2012;26(1):34–44. doi: 10.1111/j.1365-3016.2011.01237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rundle A, Neckerman KM, Freeman L, Lovasi GS, Purciel M, Quinn J, Richards C, Sircar N, Weiss C. Neighborhood food environment and walkability predict obesity in New York City. Environmental Health Perspectives. 2009;117(3):442–447. doi: 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noble M, McLennan D, Wilkinson K, Whitworth A, Barnes H, Dibben C. English Indices of Deprivation 2007. London: 2008. [Google Scholar]
- 27. Statacorp Stata Statistical Software: Release 13. 11 edn. College Station, Texas: 2013. [Google Scholar]
- 28.Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, Crawford D. Children’s fruit and vegetable intake: associations with the neighbourhood food environment. PrevMed. 2008;46(4):331–335. doi: 10.1016/j.ypmed.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 29.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Skidmore P, Welch A, van SE, Jones A, Harvey I, Harrison F, Griffin S, Cassidy A. Impact of neighbourhood food environment on food consumption in children aged 9-10 years in the UK SPEEDY (Sport, Physical Activity and Eating behaviour: Environmental Determinants in Young people) study. Public Health Nutr. 2010;13(7):1022–1030. doi: 10.1017/S1368980009992035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perchoux C, Chaix B, Cummins S, Kestens Y. Conceptualization and measurement of environmental exposure in epidemiology: accounting for activity space related to daily mobility. Health & Place. 2013;21:86–93. doi: 10.1016/j.healthplace.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 32.Diez Roux AV. Next steps in understanding the multilevel determinants of health. Journal of Epidemiology and Community Health. 2008;62(11):957–959. doi: 10.1136/jech.2007.064311. [DOI] [PubMed] [Google Scholar]
- 33.Ball K, Thornton L. Food environments: measuring, mapping, monitoring and modifying. Public Health Nutrition. 2013;16(7):1147–1150. doi: 10.1017/S1368980013001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaix B, Merlo J, Evans D, Leal C, Havard S. Neighbourhoods in eco-epidemiologic research: delimiting personal exposure areas. A response to Riva, Gauvin, Apparicio and Brodeur. Social Science & Medicine. 2009;69(9):1306–1310. doi: 10.1016/j.socscimed.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 35.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Social Science & Medicine. 2007;65(9):1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 36.Charreire H, Casey R, Salze P, Simon C, Chaix B, Banos A, Badariotti D, Weber C, Oppert JM. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutrition. 2010;13(11):1773–1785. doi: 10.1017/S1368980010000753. [DOI] [PubMed] [Google Scholar]
- 37.Burgoine T, Lake AA, Stamp E, Alvanides S, Mathers JC, Adamson AJ. Changing foodscapes 1980-2000, using the ASH30 Study. Appetite. 2009;53(2):157–165. doi: 10.1016/j.appet.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 38.Public Health England . Obesity and the environment: regulating the growth of fast food outlets. London: 2013. [Google Scholar]
- 39.Burgoine T, Forouhi NG, Griffin SJ, Wareham NJ, Monsivais P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ. 2014;348:g1464. doi: 10.1136/bmj.g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ni Mhurchu C, Vandevijvere S, Waterlander W, Thornton LE, Kelly B, Cameron AJ, Snowdon W, Swinburn B. Monitoring the availability of healthy and unhealthy foods and non-alcoholic beverages in community and consumer retail food environments globally. Obesity Reviews. 2013;14(Suppl 1):108–119. doi: 10.1111/obr.12080. [DOI] [PubMed] [Google Scholar]