Abstract
Background
Fractures are common in childhood, and there is considerable variation in the reported incidence across European countries, but few data relating to ethnic and geographic differences within a single country. We therefore aimed to determine the incidence of childhood fractures in the United Kingdom (UK), and to describe age-, ethnicity- and region-specific variations.
Methods
The Clinical Practice Research Datalink (CPRD) contains anonymised electronic health records for approximately 7% of the UK population. The occurrence of a fracture between 1988-2012 was determined from the CPRD for all individuals <18 years of age, and used to calculate fracture incidence rates for age, sex and ethnicity. Regional fracture incidence rates were also calculated based on general practitioner location within 14 Strategic Health Authorities (SHA) within the UK.
Results
The overall fracture incidence rate was 137 per 10,000 person-years (py). This was higher in boys (169 per 10,000 py) than girls (103 per 10,000 py) and white children (150 per 10,000 py) compared to those of black (64 per 10,000 py) and South Asian (81 per 10,000 py) ethnicity. Marked geographic variation in incidence was observed. The highest fracture rates were observed in Wales, where boys and girls had 1.82 and 1.97 times greater incidence than those residing in Greater London, respectively.
Conclusion
In the period 1988-2012, there was marked geographic and ethnic variation in childhood fracture incidence across the UK. These findings also implicate lifestyle and socio-economic differences associated with location and ethnicity, and are relevant to policy makers in the UK and internationally.
Keywords: Fracture, children, epidemiology, osteoporosis, ethnicity, CPRD
Introduction
Fractures are common in childhood and adolescence, and can result in significant periods of inactivity,[1] missed schooling and parental time off work.[2] Furthermore, there is evidence from some, but not all studies,[3] to suggest that sustaining a fracture in childhood is associated with lower indices of bone strength[4] and an increased risk of fracture in adulthood.[5] Previous studies have found considerable variation in incidence rates of childhood fracture across European countries, ranging from 120 to 361 per 10,000 person years (Table 1) [1, 6-17], although recent epidemiological studies from Scandinavia have suggested that overall childhood fracture incidence increased from the mid to late 20th century and has been followed by a more recent plateau or decline.[6, 8, 15] It is well recognised that childhood fractures are more common in boys than girls [12], and peak in incidence during the puberty [12], however, there are few published data pertaining to geographic or ethnic variation in fracture rates within a single country. Knowledge of these detailed epidemiological patterns could enable regional and/or ethnicity specific targeting of advice to prevent childhood fractures and promote bone health. In the present study we therefore aimed to document childhood fracture incidence by age and sex across the UK, stratifying by ethnicity and geographic location.
Table 1.
Previously reported fracture incidence rates in children
| Author | Country | Study Period | Age | Fracture incidence rate (per 10,000 per year) |
|---|---|---|---|---|
| Landin, 1983 [6] | Sweden | 1950-1979 | 0-16 years | 212 |
| Worlock, 1986 [7] | England | 1981 | 0-12 years | 160 |
| Kopjar, 1998 [1] | Norway | 1992-1995 | 0-12 years | 128 |
| Tiderius, 1999 [8] | Sweden | 1993-1994 | 0-16 years | 235 |
| Lyons, 2000 [9] | Wales | 1996 | 0-14 years | 361 |
| Finland | 178 | |||
| Sweden | 155 | |||
| Norway | 169 | |||
| Moustaki, 2001 [10] | Greece | 1996-1998 | 0-14 years | 120 |
| Brudvik, 2003 [11] | Norway | 1998 | 0-16 years | 245 |
| Cooper, 2004 [12] | UK | 1988-1998 | 0-18 years | 133 |
| Rennie, 2007 [13] | Scotland | 2000 | 0-16 years | 202 |
| Hedstrom, 2010 [14] | Sweden | 1993-2007 | 0-19 years | 201 |
| 0-16 years | 208 | |||
| Mayranpaa, 2010 [15] | Finland | 2005-2006 | 0-16 years | 163 |
| Randsborg, 2014 [16] | Norway | 2010-2011 | 0-16 years | 180 |
| Ramaesh, 2015 [17] | Scotland | 2000 | 0-16 years | 201 |
Materials and Methods
The information for this study was obtained from the Clinical Practice Research Datalink (CPRD). CPRD contains the anonymised electronic health records from General Practitioners (GP) in the UK. GPs play a key role in the healthcare system of the UK, as they are responsible for primary healthcare and specialist referrals. The population in the CPRD reflects the wide distribution of contained General Practices across the UK (providing around 6.9% national coverage), rather than individualised recruitment, and has been shown to be broadly representative of the UK population as a whole [18]. Clinical data are stored and retrieved by means of READ codes for disease or causes of morbidity or mortality, which are cross referenced to the International Classification of Diseases, 9th edition (ICD-9). From the data collected we were able to extract information on patient demographics including ethnicity, clinical events, prescriptions, referrals, hospital admissions and their major outcomes. The capture of ethnic group information in routine health records is recognized in the UK as a necessary pre-requisite to addressing inequalities in health service usage and outcomes. Within primary care, the incentivization of ethnicity recording under the Quality and Outcomes Framework (QOF)11–13 between 2006/07 and 2011/12 dramatically improved the completeness of ethnicity data for newly registered patients. QOF results data show that over 90% of UK general practices are now recording ethnicity for all of their newly registered patients, and ethnicity is also recorded by hospital staff when an individual is admitted to hospital[19]. Since there is no standard, in our study, we used the ethnicity classification as developed and tested by Mathur[19], for which a high level of concordance within and across NHS sources was found in an analysis of CPRD records of ethnicity.
The study population consisted of all permanently registered individuals aged < 18 years who had a fracture recorded in their medical record during the period of time from the enrolment date of their practice in CPRD until the end of data collection. The data collection period was 1988 to 2012. Children were followed from entry into the database to the occurrence of fracture or censoring (death, withdrawal from the database, reaching age 18 years or the end of data collection), whichever came first. The fractures were classified into the following categories: skull, vertebra, rib, pelvis, clavicle, scapula, humerus, radius/ulna, carpus, femur or hip, patella, tibia/fibula, ankle, foot, or unspecified.
This research was conducted in accordance with the principles of the Helsinki declaration and the protocol for this study was approved by CPRD’s Independent Scientific Advisory Committee. All data on patients were stored anonymously in CPRD and, therefore, informed consent was not required for this study.
Statistical Analysis
The fracture incidence rates were calculated by dividing the number of children with a fracture by the total person-years of follow-up. The total person-years was the sum of the number of people registered on the database at July 1 of each calendar year from 1988 to 2012. In CPRD, as in many similar datasets, differentiation of 2 distinct fracture events at the same site, from one fracture event recorded twice, is extremely difficult. In order to prevent double counting, the incidence analyses were therefore based on the first-ever occurrence of a fracture at a particular location. If a child had multiple records of fractures at the same location, only the first record was used in the incidence rate calculation. Children were censored if there was a record without details on location of the fracture (unspecified type). The incidence analyses were stratified by age, sex, ethnicity and geographic region. Geographic regions were defined based on GP location within one of 14 strategic health authorities (SHA) within the UK. The incidence rates in different regions in the UK were compared using Cox proportional hazards regression. These analyses were adjusted for age and calendar year.
Results
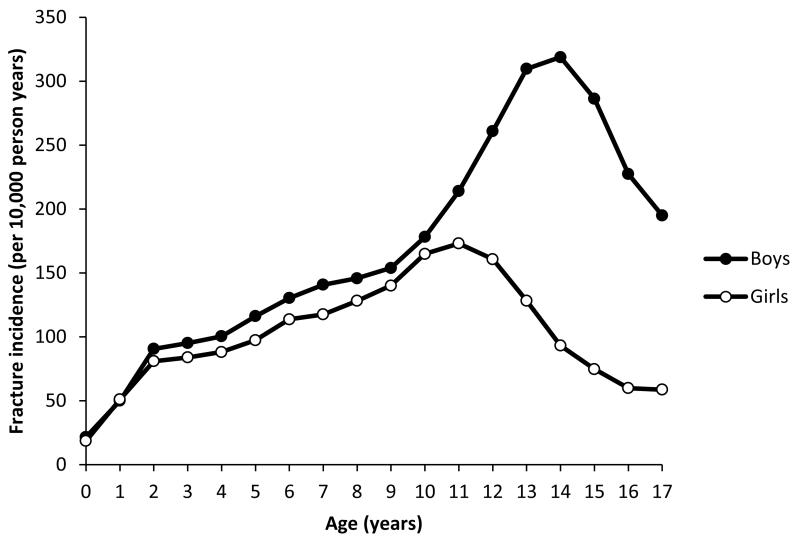
There were a total of 195,791 fractures during the 25 year follow-up period, equating to a rate of 137 fractures per 10,000 person-years (py). Figure 1 shows the age and sex standardised rates for all fractures. Overall fracture rates were higher in boys (169 per 10,000 py) than girls (103 per 10,000 py), and this was true for all age groups apart from 1.0-1.99 years, when fracture rates were similar in girls (51 per 10,000 py) and boys (50 per 10,000 py). Fracture rates increased with age in both boys and girls to reach a peak at age 14-14.99 years in males and 11-11.99 years in females, before subsequent decline. For both boys and girls, the most common site of fracture was the radius/ulna, followed by the carpal bones and humerus (Tables 2 & 3). Fractures of the lower limb were less common.
Figure 1.
Age and sex specific incidence rates of fractures at any sites, 1998-2012
Table 2.
Fracture rates in boys in the UK 1988-2012, stratified by ethnicity. Shown as rate per 10,000 person-years.
| All children | Stratified by Ethnicity | |||||
|---|---|---|---|---|---|---|
| White | Black | South Asian | Mixed | Other | ||
| Any | 168.5 | 184.2 | 83.3 | 99.6 | 112.8 | 121.5 |
| Radius/Ulna | 43.5 | 47.4 | 15.6 | 24.2 | 25.1 | 28.7 |
| Carpal | 39.3 | 42.4 | 19.3 | 17.2 | 21.6 | 24.5 |
| Humerus | 19.8 | 22.9 | 10.7 | 16.6 | 16.4 | 15.9 |
| Clavicle | 13.7 | 14.5 | 3.5 | 7.4 | 10.2 | 9.5 |
| Foot | 13.2 | 14.4 | 5.7 | 6.4 | 8.7 | 8.9 |
| Tibia/Fibula | 11.3 | 13.5 | 6.5 | 5.8 | 8.8 | 6.9 |
| Skull | 8.6 | 9.6 | 3.1 | 5.5 | 5.5 | 7.1 |
| Ankle | 6.7 | 7.3 | 3.7 | 2.6 | 4.3 | 4.4 |
| Femur/Hip | 2.5 | 3.2 | 1.1 | 1.8 | 2.0 | 1.7 |
| Scapula | 0.7 | 0.7 | 0.3 | 0.1 | 0.8 | 0.6 |
| Patella | 0.6 | 0.6 | 0.4 | 0.1 | 0.0 | 0.5 |
| Rib(s) | 0.5 | 0.6 | 0.2 | 0.3 | 0.3 | 0.3 |
| Clinical Vertebral | 0.4 | 0.5 | 0.2 | 0.1 | 0.2 | 0.0 |
| Pelvis | 0.4 | 0.4 | 0.7 | 0.1 | 0.3 | 0.3 |
Table 3.
Fracture rates in girls in the UK 1988-2012, stratified by ethnicity. Shown as rate per 10,000 person-years.
| All children | Stratified by Ethnicity | |||||
|---|---|---|---|---|---|---|
| White | Black | South Asian | Mixed | Other | ||
| Any | 103.3 | 115.0 | 44.8 | 62.2 | 72.8 | 65.8 |
| Radius/Ulna | 29.7 | 32.3 | 9.9 | 13.7 | 19.3 | 13.8 |
| Carpal | 16.8 | 18.9 | 6.4 | 6.3 | 10.7 | 10.5 |
| Humerus | 15.5 | 17.5 | 6.0 | 14.7 | 10.3 | 13.0 |
| Clavicle | 6.1 | 6.7 | 3.3 | 3.8 | 4.8 | 4.5 |
| Foot | 8.8 | 9.9 | 2.7 | 4.3 | 5.4 | 4.5 |
| Tibia/Fibula | 6.4 | 7.7 | 4.2 | 3.4 | 6.1 | 4.6 |
| Skull | 2.9 | 3.2 | 0.8 | 3.1 | 2.0 | 1.7 |
| Ankle | 4.2 | 4.8 | 2.4 | 2.6 | 4.4 | 4.8 |
| Femur/Hip | 1.1 | 1.4 | 0.9 | 0.9 | 1.3 | 0.7 |
| Scapula | 0.3 | 0.3 | 0.2 | 0.1 | 0.2 | 0.2 |
| Patella | 0.2 | 0.2 | 0.1 | 0.2 | 0.2 | 0.0 |
| Rib(s) | 0.3 | 0.3 | 0.1 | 0.1 | 0.2 | 0.0 |
| Clinical Vertebral | 0.3 | 0.3 | 0.1 | 0.0 | 0.0 | 0.0 |
| Pelvis | 0.2 | 0.2 | 0.1 | 0.1 | 0.0 | 0.2 |
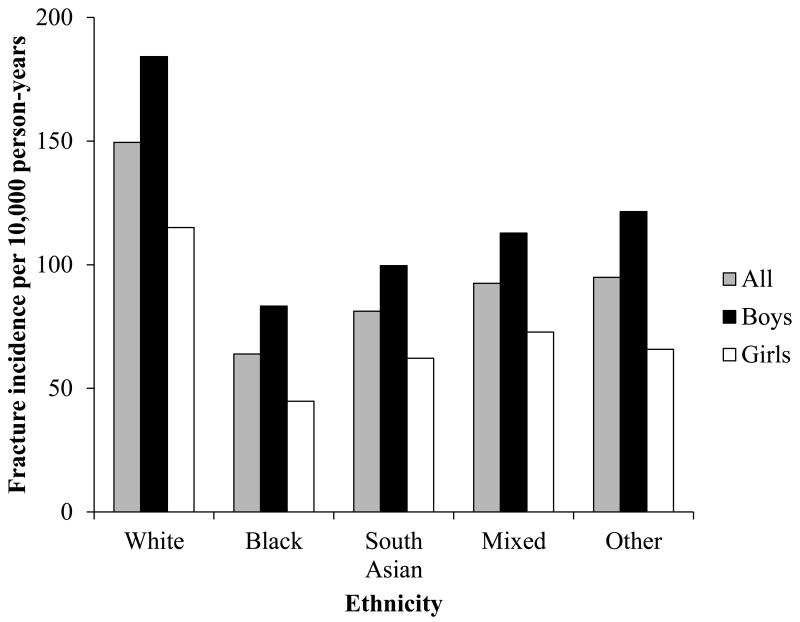
Fracture incidence by ethnicity
The child’s ethnicity was known for 45.5% of the fractures that occurred during the follow-up period. Fracture rates were lowest in those of black ethnicity (63.9 per 10,000 py), and highest in white children (149.5 per 10,000 py). Children of South Asian (81.2 per 10,000 py) and mixed (92.9 per 10,000 py) ethnicity had a lower fracture rate than white children, but higher than black children (Figure 2). A similar pattern of fracture rates by ethnicity was observed when boys and girls were analysed separately, and across most fracture sites (Tables 1 & 2). Only pelvic fractures were more common in boys of black ethnicity (0.7 per 10,000 py) than those of white ethnicity (0.4 per 10,000 py).
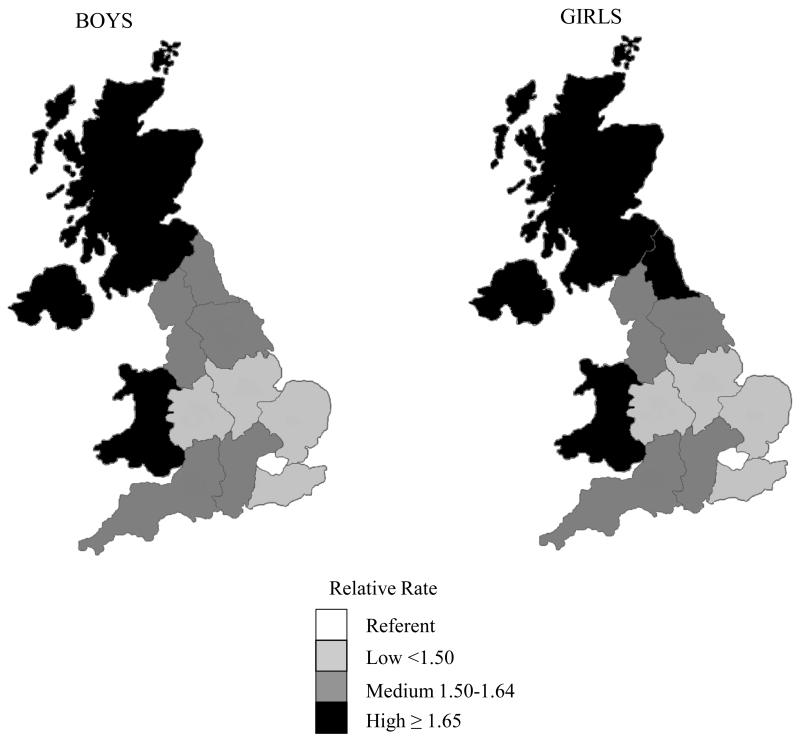
Figure 2.
Regional variation in fracture incidence in boys and girls within the UK, shown as relative rate of fractures for each sex compared to that observed in Greater London.
Regional variation in fracture incidence
There were regional variations in fracture incidence rates in both boys and girls (Table 4). The highest fracture incidence rates were observed in children living in Wales, and were nearly twice those of children living in London, where the lowest rates were observed. The pattern of regional variation was similar in boys and girls (Figure 3).
Table 4.
Fracture incidence rates in children in the UK stratified by sex and region
| Boys | Girls | |||
|---|---|---|---|---|
| Incidence rate (per 10,000 py) | Relative risk (95% CI) | Incidence rate (per 10,000 py) | Relative risk (95% CI) | |
| London | 109.9 | Reference | 65.7 | Reference |
| West Midlands | 154.1 | 1.36 (1.32, 1.40) | 93.5 | 1.39 (1.34, 1.44) |
| South East Coast | 157.4 | 1.40 (1.36, 1.44) | 95.4 | 1.43 (1.38, 1.48) |
| East of England | 158.5 | 1.42 (1.38, 1.45) | 96.6 | 1.44 (1.39, 1.49) |
| East Midlands | 170.1 | 1.49 (1.44, 1.54) | 99.8 | 1.48 (1.41, 1.54) |
| South Central | 170.0 | 1.53 (1.49, 1.57) | 108.6 | 1.63 (1.57, 1.68) |
| North West | 176.2 | 1.56 (1.52, 1.60) | 108.1 | 1.60 (1.55, 1.65) |
| South West | 182.2 | 1.62 (1.58, 1.67) | 108.6 | 1.63 (1.57, 1.69) |
| Yorkshire & The Humber | 185.7 | 1.63 (1.57, 1.68) | 108.1 | 1.60 (1.53, 1.67) |
| North East | 187.5 | 1.64 (1.57, 1.71) | 113.8 | 1.68 (1.59, 1.77) |
| Northern Ireland | 188.8 | 1.65 (1.59, 1.71) | 117.0 | 1.72 (1.64, 1.80) |
| Scotland | 195.4 | 1.73 (1.69, 1.78) | 123.2 | 1.84 (1.78, 1.91) |
| Wales | 205.4 | 1.82 (1.77, 1.87) | 132.4 | 1.97 (1.90, 2.04) |
Figure 3.
Childhood fracture incidence stratified by ethnicity in the UK, 1988-2012
Discussion
In this study, we have presented a detailed description of the epidemiology of childhood fractures in the UK by ethnicity and geographic location. The overall incidence of fractures up to the age of 18 years between 1988 and 2012 was 137 per 10,000 py, and we noted marked ethnic and geographic variations, with fracture rates higher in white than black or Asian children, and higher in Wales and Scotland than in England. Overall, fracture rates were higher in males than females, and the most frequent site of fracture was the forearm, representing nearly 29% of all childhood fractures. From these data, it would be expected that approximately 30% of boys and 19% of girls will sustain a fracture before their 18th birthday.
Ethnic variation in fracture rates in children in the UK has not previously been investigated. However, our finding of higher fracture rates in children of white ethnicity than those of black, South Asian or mixed ethnicity are consistent with data from the USA [20] and South Africa [21]. Black African children have higher bone mineral content (BMC) and bone mineral density (BMD) than white children when measured by DXA [22-24] , whereas several studies have suggested that children of Asian ethnicity have lower BMD than white children [22, 25]. Appendicular bone cross-sectional area and strength strain index (SSI) at the radius and tibia are also reported to be higher in black than white children [26-28]. Case-control and prospective cohort studies suggest that children who sustain fractures have lower BMD, compared to non-fracturing controls [29-33], and geometric properties of bone have been associated with failure load ex vivo [34]. Thus, it is likely that these differences in BMD and bone geometry contribute to the lower fracture risk observed in black children. However, it is also recognised that BMD alone is a poor predictor of fracture in children [35], and other risks factors can modify the relationship between BMD and fracture. Indeed, children who are more physically active typically have higher BMD, but are also at increased fracture risk [20, 36], which is likely due to the exposure to potentially fracturing events during sporting activities. Differences in risk-taking behaviour may also contribute [37]. Whilst the available evidence does not consistently suggest that physical activity levels differ between white and black children and adolescents [38, 39], lower physical activity levels in children of Asian ethnicity living in the UK compared to white children have been reported [39, 40]. This difference could therefore result in both the lower BMD previously described, and our finding of a lower fracture incidence in South Asian children. Furthermore it has been shown that children of South Asian ethnicity in the UK are less likely to both self-report, and utilize hospital services for, accidental injuries [41]. Given that a bony fracture is unlikely to be something that would be treated at home, these findings might reflect a reduced exposure to fracture precipitating events compared with white children.
Overall, the incidence of fractures in children in the UK is similar to that reported previously for 1988-1998 using similar methodology [12], and remains one of the lowest reported in European populations, although care must be taken in comparing studies due to the differing age ranges included (Table 1). However, we did identify marked geographic variation in fracture rates across the UK, with incidence rates in Wales nearly twice that of Greater London. Interestingly, a previous study similarly found a markedly higher fracture rate in children in South Wales (361 per 10,000 per year) compared to Scandinavian populations (155-178 per 10,000 per year) in 1996.[9] The degree of ethnic diversity of a region might contribute to the geographic variation in fracture incidence. In 2011, the proportion of residents in London identifying themselves as of white ethnicity was 59.8%, compared with over 80% in other regions of England and Wales.[42] This could therefore account for the much lower fracture incidence in Greater London compared to other UK regions. Overall, there appears to be a north-south gradient in fracture risk within the UK, and there are several possible explanations that might contribute to this:
Firstly, childhood overweight and obesity has been associated with a higher risk of fracture,[43, 44] although there is some evidence that this might vary by fracture site.[45, 46] Excluding Greater London, which has the highest prevalence of obesity in England but lowest fracture rates, the pattern of childhood fracture incidence is similar to that of the prevalence of overweight and obesity.[46, 47] In Wales and Scotland, where fracture incidences are highest in the UK, the prevalence of childhood obesity is higher than England.[48] However, it remains possible these geographic trends reflect a common factor, and indeed social deprivation has been associated with both increased childhood fracture risk[17] and obesity.[47] Similarly, children residing in Scotland have lower 25-hydroxyvitamin D [25(OH)D] levels than those in southern England,[49] but there is currently little evidence that 25(OH)D status contributes to fracture risk in childhood.[50]
The strength of this study is the large free-living population based cohort included as the CPRD contains data for approximately 7% of the UK population, including a geographically diverse areas and a range of patient demographics [18]. However, there are a number of limitations to this study. Firstly, the proportion of children aged 0-4 years included in CPRD is lower than that in the UK Census 2011 [18]. However, as the incidence is expressed relative to the number of person-years within the CRPD, this is unlikely to affect the incidence reporting. Secondly, ethnicity was only available for approximately half of the children with fractures. However, as incidence rates were calculated relative to children in whom ethnicity is reported within the CPRD, it is unlikely that this would lead to an error in the calculation of ethnicity specific incidence rates. Thirdly, we relied on the accuracy of the data within the CPRD. There is therefore the potential for ascertainment and classification bias if a soft tissue injury has been incorrectly coded as a fracture, or vice versa, and we are reliant on the fracture site being correctly coded. Fourthly, subsequent fractures at the same site were excluded from the outcome of interest because it cannot be determined from CPRD whether a record relates to an incident fracture or to a consultation or referral for a previous fracture. This approach is likely to result in an underestimate of the fracture incidence. Finally, CPRD does not contain any measures of habitual physical activity, and therefore it was not possible to explore any potential contribution of physical activity to geographic or ethnic differences in fracture incidence.
Although our study is based in the UK, the demonstration of variation in childhood fracture incidence by geographic location and ethnicity clearly has relevance for other countries. As described above, ethnic differences in fracture risk have been documented in other countries, including USA and South Africa [20][21], but geographic differences in fracture risk remain much less frequently reported globally. Furthermore, interaction between ethnicity and geographic location have been poorly characterised in childhood, although in terms of adult fracture there is evidence for migrant fracture risk tending to become more like that of the indigenous population with time [51-53]. The factors contributing to the geographic variations in childhood fracture are clearly multiple (for example socioeconomic status, obesity, physical activity and 25(OH)-vitamin D status) and are all indices which vary considerably across most countries worldwide. Our findings may therefore be helpful in the development of approaches to identification of children at high fracture risk in many countries other than the United Kingdom.
In conclusion, we have demonstrated marked variations in childhood fracture incidence across the UK by ethnicity and geographic location. Although the mechanisms underlying these differences remain partly unexplained and are likely to be multifactorial, our findings clearly inform the provision of healthcare resource nationwide and globally, and may be used to target bone health advice in high risk geographic areas and ethnic groups in the UK and internationally.
Summary.
We have documented the epidemiology of childhood fracture in the UK between 1988 and 2012, demonstrating marked differences in site-specific fracture incidence by age, sex, geographic location and ethnicity.
Acknowledgements
This work was supported by grants from the National Osteoporosis Society, Medical Research Council, British Heart Foundation, Arthritis Research UK, International Osteoporosis Foundation, National Institute for Health Research (NIHR), Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, and NIHR Musculoskeletal Biomedical Research Unit, University of Oxford. The work leading to these results was support by the European Union's Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreements nos 289346 and 613977.
Footnotes
Disclosure statement: All authors state that they have no conflicts of interests.
References
- [1].Kopjar B, Wickizer TM. Fractures among children: incidence and impact on daily activities. Inj Prev. 1998;4:194–7. doi: 10.1136/ip.4.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Morris MWJ, Bell MJ. The socio-economical impact of paediatric fracture clinic appointments. Injury. 2006;37:395–397. doi: 10.1016/j.injury.2005.12.010. [DOI] [PubMed] [Google Scholar]
- [3].Pye SR, Tobias J, Silman AJ, Reeve J, O'Neill TW. Childhood Fractures Do Not Predict Future Fractures: Results From the European Prospective Osteoporosis Study. J Bone Miner Res. 2009;24:1314–1318. doi: 10.1359/jbmr.090220. [DOI] [PubMed] [Google Scholar]
- [4].Chevalley T, Bonjour JP, van Rietbergen B, Rizzoli R, Ferrari S. Fractures in healthy females followed from childhood to early adulthood are associated with later menarcheal age and with impaired bone microstructure at peak bone mass. J Clin Endocrinol Metab. 2012;97:4174–81. doi: 10.1210/jc.2012-2561. [DOI] [PubMed] [Google Scholar]
- [5].Amin S, Melton LJ, Achenbach SJ, Atkinson EJ, Dekutoski MB, Kirmani S, Fischer PR, Khosla S. A distal forearm fracture in childhood is associated with an increased risk for future fragility fractures in adult men, but not women. J Bone Miner Res. 2013;28:1751–1759. doi: 10.1002/jbmr.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1–109. [PubMed] [Google Scholar]
- [7].Worlock P, Stower M. Fracture patterns in Nottingham children. J Pediatr Orthop. 1986;6:656–60. doi: 10.1097/01241398-198611000-00003. [DOI] [PubMed] [Google Scholar]
- [8].Tiderius CJ, Landin L, Duppe H. Decreasing incidence of fractures in children: an epidemiological analysis of 1,673 fractures in Malmo, Sweden, 1993-1994. Acta Orthop Scand. 1999;70:622–626. doi: 10.3109/17453679908997853. [DOI] [PubMed] [Google Scholar]
- [9].Lyons RA, Sellstrom E, Delahunty AM, Loeb M, Varilo S. Incidence and cause of fractures in European districts. Arch Dis Child. 2000;82:452–5. doi: 10.1136/adc.82.6.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Moustaki M, Lariou M, Petridou E. Cross country variation of fractures in the childhood population. Is the origin biological or “accidental”? Inj Prev. 2001;7:77. doi: 10.1136/ip.7.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Brudvik C, Hove LM. Childhood fractures in Bergen, Norway: identifying high-risk groups and activities. J Pediatr Orthop. 2003;23:629–34. doi: 10.1097/00004694-200309000-00010. [DOI] [PubMed] [Google Scholar]
- [12].Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19:1976–1981. doi: 10.1359/JBMR.040902. [DOI] [PubMed] [Google Scholar]
- [13].Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38:913–22. doi: 10.1016/j.injury.2007.01.036. [DOI] [PubMed] [Google Scholar]
- [14].Hedstrom EM, Svensson O, Bergstrom U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81:148–53. doi: 10.3109/17453671003628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mayranpaa MK, Makitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: A population-based study. J Bone Miner Res. 2010;25:2752–9. doi: 10.1002/jbmr.155. [DOI] [PubMed] [Google Scholar]
- [16].Randsborg PH, Gulbrandsen P, Saltyte Benth J, Sivertsen EA, Hammer OL, Fuglesang HF, Aroen A. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am. 2013;95:e42. doi: 10.2106/JBJS.L.00369. [DOI] [PubMed] [Google Scholar]
- [17].Ramaesh R, Clement ND, Rennie L, Court-Brown C, Gaston MS. Social deprivation as a risk factor for fractures in childhood. Bone Joint J. 2015;97-b:240–5. doi: 10.1302/0301-620X.97B2.34057. [DOI] [PubMed] [Google Scholar]
- [18].Herrett E, Gallagher AM, Bhaskaran K, Forbes H, Mathur R, van Staa T, Smeeth L. Data Resource Profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015 doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mathur R, Bhaskaran K, Chaturvedi N, Leon DA, vanStaa T, Grundy E, Smeeth L. Completeness and usability of ethnicity data in UK-based primary care and hospital databases. J Public Health (Oxf) 2014;36:684–92. doi: 10.1093/pubmed/fdt116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wren TA, Shepherd JA, Kalkwarf HJ, Zemel BS, Lappe JM, Oberfield S, Dorey FJ, Winer KK, Gilsanz V. Racial disparity in fracture risk between white and nonwhite children in the United States. J Pediatr. 2012;161:1035–40. doi: 10.1016/j.jpeds.2012.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Thandrayen K, Norris SA, Pettifor JM. Fracture rates in urban South African children of different ethnic origins: the Birth to Twenty cohort. Osteoporos Int. 2009;20:47–52. doi: 10.1007/s00198-008-0627-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bachrach LK, Hastie T, Wang MC, Narasimhan B, Marcus R. Bone mineral acquisition in healthy Asian, Hispanic, black, and Caucasian youth: a longitudinal study. J Clin Endocrinol Metab. 1999;84:4702–12. doi: 10.1210/jcem.84.12.6182. [DOI] [PubMed] [Google Scholar]
- [23].Horlick M, Thornton J, Wang J, Levine LS, Fedun B, Pierson RN., Jr. Bone mineral in prepubertal children: gender and ethnicity. J Bone Miner Res. 2000;15:1393–1397. doi: 10.1359/jbmr.2000.15.7.1393. [DOI] [PubMed] [Google Scholar]
- [24].Wang MC, Aguirre M, Bhudhikanok GS, Kendall CG, Kirsch S, Marcus R, Bachrach LK. Bone mass and hip axis length in healthy Asian, black, Hispanic, and white American youths. J Bone Miner Res. 1997;12:1922–35. doi: 10.1359/jbmr.1997.12.11.1922. [DOI] [PubMed] [Google Scholar]
- [25].McKay HA, Petit MA, Khan KM, Schutz RW. Lifestyle determinants of bone mineral: a comparison between prepubertal Asian- and Caucasian-Canadian boys and girls. Calcif Tissue Int. 2000;66:320–4. doi: 10.1007/s002230010067. [DOI] [PubMed] [Google Scholar]
- [26].Wetzsteon RJ, Hughes JM, Kaufman BC, Vazquez G, Stoffregen TA, Stovitz SD, Petit MA. Ethnic differences in bone geometry and strength are apparent in childhood. Bone. 2009;44:970–5. doi: 10.1016/j.bone.2009.01.006. [DOI] [PubMed] [Google Scholar]
- [27].Warden SJ, Hill KM, Ferira AJ, Laing EM, Martin BR, Hausman DB, Weaver CM, Peacock M, Lewis RD. Racial differences in cortical bone and their relationship to biochemical variables in Black and White children in the early stages of puberty. Osteoporos Int. 2013;24:1869–1879. doi: 10.1007/s00198-012-2174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Gilsanz V, Skaggs DL, Kovanlikaya A, Sayre J, Loro ML, Kaufman F, Korenman SG. Differential effect of race on the axial and appendicular skeletons of children. J Clin Endocrinol Metab. 1998;83:1420–7. doi: 10.1210/jcem.83.5.4765. [DOI] [PubMed] [Google Scholar]
- [29].Clark EM, Ness AR, Bishop NJ, Tobias JH. Association between bone mass and fractures in children: a prospective cohort study. J Bone Miner Res. 2006;21:1489–1495. doi: 10.1359/jbmr.060601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Mayranpaa MK, Viljakainen HT, Toiviainen-Salo S, Kallio PE, Makitie O. Impaired bone health and asymptomatic vertebral compressions in fracture-prone children: a case-control study. J Bone Miner Res. 2012;27:1413–1424. doi: 10.1002/jbmr.1579. [DOI] [PubMed] [Google Scholar]
- [31].Farr JN, Amin S, Melton LJ, Kirmani S, McCready LK, Atkinson EJ, Müller R, Khosla S. Bone Strength and Structural Deficits in Children and Adolescents With a Distal Forearm Fracture Resulting From Mild Trauma. J Bone Miner Res. 2014;29:590–599. doi: 10.1002/jbmr.2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Clark EM, Ness AR, Tobias JH. Bone fragility contributes to the risk of fracture in children, even after moderate and severe trauma. J Bone Miner Res. 2008;23:173–9. doi: 10.1359/jbmr.071010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Clark EM, Tobias JH, Ness AR. Association between bone density and fractures in children: a systematic review and meta-analysis. Pediatrics. 2006;117:e291–7. doi: 10.1542/peds.2005-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Liu D, Manske SL, Kontulainen SA, Tang C, Guy P, Oxland TR, McKay HA. Tibial geometry is associated with failure load ex vivo: a MRI, pQCT and DXA study. Osteoporos Int. 2007;18:991–7. doi: 10.1007/s00198-007-0325-0. [DOI] [PubMed] [Google Scholar]
- [35].Rauch F, Plotkin H, DiMeglio L, Engelbert RH, Henderson RC, Munns C, Wenkert D, Zeitler P. Fracture Prediction and the Definition of Osteoporosis in Children and Adolescents: The ISCD 2007 Pediatric Official Positions. J Clin Densitom. 2008;11:22–28. doi: 10.1016/j.jocd.2007.12.003. [DOI] [PubMed] [Google Scholar]
- [36].Clark EM, Ness AR, Tobias JH. Vigorous physical activity increases fracture risk in children irrespective of bone mass: a prospective study of the independent risk factors for fractures in healthy children. J Bone Miner Res. 2008;23:1012–1022. doi: 10.1359/jbmr.080303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Pressley JC, Kendig TD, Frencher SK, Barlow B, Quitel L, Waqar F. Epidemiology of bone fracture across the age span in blacks and whites. J Trauma. 2011;71:S541–8. doi: 10.1097/TA.0b013e31823a4d58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Eyre EL, Duncan MJ. The impact of ethnicity on objectively measured physical activity in children. ISRN Obes. 2013;2013:757431. doi: 10.1155/2013/757431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Owen CG, Nightingale CM, Rudnicka AR, Cook DG, Ekelund U, Whincup PH. Ethnic and gender differences in physical activity levels among 9-10-year-old children of white European, South Asian and African-Caribbean origin: the Child Heart Health Study in England (CHASE Study) Int J Epidemiol. 2009;38:1082–93. doi: 10.1093/ije/dyp176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Duncan MJ, Birch S, Al-Nakeeb Y, Nevill AM. Ambulatory physical activity levels of white and South Asian children in Central England. Acta Paediatr. 2012;101:e156–62. doi: 10.1111/j.1651-2227.2011.02566.x. [DOI] [PubMed] [Google Scholar]
- [41].Tobin MD, Milligan J, Shukla R, Crump B, Burton PR. South Asian ethnicity and risk of childhood accidents: an ecological study at enumeration district level in Leicester. J Public Health Med. 2002;24:313–8. doi: 10.1093/pubmed/24.4.313. [DOI] [PubMed] [Google Scholar]
- [42].Office for National Statistics Ethnicity and National Identity in England and Wales 2011. 2012.
- [43].Adams AL, Kessler JI, Deramerian K, Smith N, Black MH, Porter AH, Jacobsen SJ, Koebnick C. Associations between childhood obesity and upper and lower extremity injuries. Inj Prev. 2013;19:191–7. doi: 10.1136/injuryprev-2012-040341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Goulding A, Jones IE, Taylor RW, Williams SM, Manning PJ. Bone mineral density and body composition in boys with distal forearm fractures: a dual-energy x-ray absorptiometry study. J Pediatr. 2001;139:509–515. doi: 10.1067/mpd.2001.116297. [DOI] [PubMed] [Google Scholar]
- [45].Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res. 2013;471:1199–207. doi: 10.1007/s11999-012-2621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Moon RJ, Lim A, Farmer M, Segaran A, Clarke NM, Dennison EM, Harvey NC, Cooper C, Davies JH. Differences in childhood adiposity influence upper limb fracture site. Bone. 2015;79:88–93. doi: 10.1016/j.bone.2015.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47]. Public Health England Slide sets: Child Slide Set. updated April 2015. 2015. [Google Scholar]
- [48].Public Health England Child Obesity: UK Prevalence. 2015.
- [49].Davies PS, Bates CJ, Cole TJ, Prentice A, Clarke PC. Vitamin D: seasonal and regional differences in preschool children in Great Britain. Eur J Clin Nutr. 1999;53:195–198. doi: 10.1038/sj.ejcn.1600697. [DOI] [PubMed] [Google Scholar]
- [50].Moon RJ, Harvey NC, Davies JH, Cooper C. Vitamin D and skeletal health in infancy and childhood. Osteoporos Int. 2014;25:2673–84. doi: 10.1007/s00198-014-2783-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Johansson H, Oden A, Lorentzon M, McCloskey E, Kanis JA, Harvey NC, Karlsson MK, Mellstrom D. Is the Swedish FRAX model appropriate for Swedish immigrants? Osteoporos Int. 2015;26:2617–22. doi: 10.1007/s00198-015-3180-4. [DOI] [PubMed] [Google Scholar]
- [52].Albin B, Hjelm K, Elmstahl S. Lower prevalence of hip fractures in foreign-born individuals than in Swedish-born individuals during the period 1987-1999. BMC Musculoskelet Disord. 2010;11:203. doi: 10.1186/1471-2474-11-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Lauderdale DS, Jacobsen SJ, Furner SE, Levy PS, Brody JA, Goldberg J. Hip fracture incidence among elderly Asian-American populations. Am.J.Epidemiol. 1997;146:502–509. doi: 10.1093/oxfordjournals.aje.a009304. [DOI] [PubMed] [Google Scholar]