Abstract
Little is known about how optimism differs by age and changes over time, particularly among older adults. Even less is known about how changes in optimism are related to changes in physical health. We examined age differences and longitudinal changes in optimism in 9,790 older adults over a four-year period. We found an inverted U-shaped pattern between optimism and age both cross-sectionally and longitudinally, such that optimism generally increased in older adults before decreasing. Increases in optimism over a four-year period were associated with improvements in self-rated health and fewer chronic illnesses over the same time frame. The findings from the current study are consistent with changes in emotion regulation strategies employed by older adults and age-related changes in well-being.
Keywords: optimism, aging, health, positivity effect, socioemotional selectivity theory
Dispositional optimism, the generalized expectation that good things will happen, has been linked with an array of positive health outcomes, including fewer sick days after major stressful events (e.g., death or major illness in family), enhanced immune response after an influenza vaccination, and a reduced risk of heart disease, stroke, and mortality (Boehm & Kubzansky, 2012; Chida & Steptoe, 2008; Kim, Park, & Peterson, 2011; Kim, Smith, & Kubzansky, 2014; Kivimaki et al., 2005; Tindle et al., 2009). Although a large and growing body of observational studies link optimism with better health, the vast majority of research examining this link has either used cross-sectional data or examined how optimism at one time point is associated with health at a later time. Few studies have examined how changes in optimism are associated with simultaneous changes in health.
Further, no study to our knowledge has examined whether optimism changes over time among older adults. Personality is typically thought to become more consistent by older adulthood (Roberts, Walton, & Viechtbauer, 2006). However, optimism may be more malleable during this time, as some theoretical perspectives suggest that changes in older adults’ personality may be more dramatic in some contexts (Specht et al., 2014). Optimism is an individual attribute that is about 25% heritable but can also be learned and shaped by social influences (Brunwasser, Gillham, & Kim, 2009; Hanssen, Peters, Vlaeyen, Meevissen, & Vancleef, 2013; Heinonen, Räikkönen, & Keltikangas-Järvinen, 2005; Meevissen, Peters, & Alberts, 2011; Peters, Flink, Boersma, & Linton, 2010; Plomin, Scheier, Bergeman, & Pedersen, 1992; Segerstrom, 2007).
Personality continues to be malleable beyond young adulthood (Srivastava, John, Gosling, & Potter, 2003). Social role theories suggest that personality change is often a product of the changes an individual implements when he or she starts a new social role (Roberts, Wood, & Smith, 2005). The expectations of new social roles motivate an individual to change their behavior to meet the demands of a situation, leading to personality change. Many transitions in social roles happen in older adulthood. In older adulthood, individuals may become grandparents, retire from full-time work, or even take up new hobbies. Many older adults also experience several challenges, including declines in mobility and health, requiring them to evaluate their position in society and within their families. As such, their dispositions and expectations about the future are subject to change as well.
Although trajectories of change in optimism have not been explored among older adults, researchers examining how other facets of psychological well-being (e.g., life satisfaction and positive affect) change over time may provide some direction in making predictions about optimism’s developmental trajectory. Earlier in life (through the final years of middle age), well-being reflects a U-shaped pattern, such that well-being is higher in younger and older adulthood, but lower in mid-life (Blanchflower & Oswald, 2008). This U-shaped pattern is also found across 72 different countries as well as lifespan study on the great apes (Weiss, King, Inoue-Murayama, Matsuzawa, & Oswald, 2012). However, numerous studies examining well-being among older adults have found that an inverted U-shaped trajectory of well-being emerges in older adulthood, such that well-being increases in older age and then starts to decline (Baird, Lucas, & Donnellan, 2010; Mroczek & Spiro, 2005; Netuveli, Wiggins, Hildon, Montgomery, & Blane, 2006; Zaninotto, Falaschetti, & Sacker, 2009). What might explain this inverted U-shape that is repeatedly found in older adulthood?
Socioemotional selectivity theory and the positivity effect may help explain the initial upward trajectory among older adults. Socioemotional selectivity theory states that as people age, they become increasingly aware of their shortening future time horizon. This awareness then leads older adults to prioritize emotional meaning, emotion regulation, and well-being (Carstensen, 2006; Reed & Carstensen, 2012). Further, the positivity effect helps explain the common finding that older adults, when compared to younger adults, pay more attention to and remember more positively valenced stimuli (Carstensen, 2006). Initially, the processes of socioemotional selectivity theory and the positivity effect may help buffer against declines in well-being and lead to initial increases in optimism in older adults. Both socioemotional selectivity theory and the positivity effect may help explain the initial upward trajectory in well-being. Thus, based on predictions from these two perspectives, we hypothesized that optimism would initially increase as people age.
However, as people age, they may ultimately be overwhelmed by mortality-related processes later in life. Aging, especially among the oldest-old, is often associated with declining health, fewer social connections, and declining material resources. Therefore, declines in psychological well-being and optimism may be expected as people age. Terminal decline and “sobering up theory” may explain the eventual decline in well-being that is observed in many studies. For example cognitive functioning can decline rapidly as death approaches (Bäckman & MacDonald, 2006). Therefore, changes in well-being in later life may be more closely related to mortality-related processes rather than age-related processes (Gerstorf et al., 2008; Gerstorf, Ram, Röcke, Lindenberger, & Smith, 2008).
Sobering up theory may also help explain the eventual decline in well-being as people age (Sweeny & Krizan, 2013). Though sobering up theory was built upon a literature in which people predicted their personal performance on various challenging tasks (e.g., a test or recital), the theory may offer insight into why well-being declines in later life. The theory posits that people tend to lower their expectations as the time of feedback approaches. Among older adults, the point of feedback in this case would be death. The theory also states that people use preventive affect management and lower their expectations as a way to alleviate current feelings of anxiety (Sweeny & Krizan, 2013). When an event is far away, people tend to focus on what they would like to ideally happen (Trope & Liberman, 2003). In contrast, when an event is near, people’s well-being may decline because they have to consider more concrete and low-level details about their lives (Trope & Liberman, 2003). Thus, based on research on terminal decline and sobering up theory, we hypothesized that optimism would decline among the oldest participants in our sample.
Finally, Self-Determination Theory may help explain the inverted U-shape of psychological well-being that is observed as people age. The theory states that psychological well-being is a result of feeling competent, the ability to succeed in a valued area, and a sense of belonging or connection to others (Deci & Ryan, 2000). As adults advance in their careers, they may have an increasing sense of competency, success in a valued domain (or career), and a sense of belonging or connection with their co-workers. However as people age into older adulthood and retire, they may lose that sense of competency, success, and social resources that were built over a course of several decades. All of these factors may contribute to declines in well-being. Thus, based on Self-Determination Theory, we hypothesized that optimism would initially increase in older adulthood but decline among the oldest participants.
Examining Correlated Changes between Optimism and Health over Time
Overall, optimists differ on several processes that are foundational to health across the lifespan. For example, optimists generally have better health knowledge, health behaviors, social support networks, and coping mechanisms. As optimism fluctuates, these assets may rise and fall over time. Optimists generally know more about health risks and process health risks more deeply. For example, one study found that optimists knew more about cardiovascular risk factors and had higher self-awareness of their cardiovascular risk status even after adjusting for potential confounding factors, such as level of education (Radcliffe & Klein, 2002). Optimists also act in healthier ways. Optimists exercise more, smoke less, and eat healthier diets (e.g., more fruits, vegetables, whole grains, salads, and fruit; Giltay, Geleijnse, Zitman, Buijsse, & Kromhout, 2007; Kelloniemi, Ek, & Laitinen, 2005). Optimists are also more persistent, effective, and successful at achieving their goals, but also know when it’s healthier to disengage from unattainable goals and find new goals to pursue (Carver, Scheier, & Segerstrom, 2010; Nes & Segerstrom, 2006; Rasmussen, Wrosch, Scheier, & Carver, 2006).
Despite these associations between mean levels of optimism and health, previous research has not examined whether changes in optimism are associated with changes in health over time. Considering the mechanisms hypothesized to link higher levels of optimism to higher levels of health, increases in optimism may be associated with better health over time, similar to effects found among other personality traits linked to health and well-being (Allemand, Schaffhuser, & Martin, 2015; Takahashi, Edmonds, Jackson, & Roberts, 2013). We hypothesized that increases in optimism would be associated with increases in self-reported health and fewer chronic illnesses over the same time frame.
Method
Sample and Procedure
The Health and Retirement Study (HRS) is a nationally representative and prospective panel study that has surveyed more than 22,000 Americans aged 51+ every two years (HRS, 2006; Wallace & Herzog, 1995). Data have been collected since 1992. We report on psychological, health, and covariate data collected in 2006, 2008, 2010, and 2012. The University of Michigan’s Institute for Social Research is responsible for the study and provides extensive documentation about the protocol, instrumentation, sampling strategy, and statistical weighting procedures. The HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
In 2006, a random 50% of HRS respondents were selected and then visited for an enhanced face-to-face interview. In 2008, the remaining 50% of HRS respondents were visited for an enhanced face-to-face interview. Respondents received a self-report psychosocial questionnaire every other wave (every four years) that they completed and mailed to the University of Michigan. Thus, two distinct cohorts were formed that had two psychosocial assessments four years apart (i.e., Cohort 1:Assessed in 2006 and 2010; Cohort 2:Assessed in 2008 and 2012). Among people who were interviewed, the response rate for the leave-behind questionnaire was 90%. The two cohorts did not differ with respect to self-reported health (p=.17), chronic health conditions (p=.59), optimism at Wave 1 (measured in 2006 or 2008; p=.26), or optimism at Wave 2 (measured in 2010 or 2012; p=.79). Therefore, the cohorts were combined into one sample for the present analyses to increase statistical power and precision; cohort source did not moderate any of the effects reported below. Because we were interested in changes in optimism predicting health, we limited data to the 9,790 respondents who had full data on all the measures of interest (optimism and health) on two occasions, which we call Wave 1 and Wave 2. Thus, all available optimism data from the HRS was used, and all available data on these individuals were included for the present analysis.
The final sample of 9,790 participants (59.1% Female) ranged in age from 51 to 97 (M=67.95, SD=9.09) at Wave 1. The number of participants was high in each age group (e.g., 50–54 yrs:603; 55–59 yrs:1,527; 60–64:1,410; 65–69 yrs:2,060; 70–74 yrs:1,814; 75–79 yrs:1,270; 80–84 yrs:701; 85+ yrs:405). Median level of education was a high school education (15.6% had less than a high school education, 56.4% had a high school education, 28% reported having at least some college education). The current sample differed from the broader sample on several variables of interest, albeit these differences were small or negligible. Specifically, the current sample was more optimistic (dWave1=.07; dWave2=.04), had higher self-rated health (dW1=.18; dW1=.09), fewer chronic conditions at Wave 1 (dW1=.05), more chronic conditions at wave 2 (dW2=−.22), and were younger on average (dW1=.07) compared to the broader HRS sample.
The covariates used in each model involving changes in health (i.e., age, gender, education) were chosen a priori and are consistent with other studies of personality and health involving the HRS sample (Weston & Jackson, 2015). All interrelationships between optimism and health were identical regardless of whether these covariates were included in the model; thus, they were included in the models presented below.
Measures
Optimism
Optimism was measured at both waves using the Life Orientation Test-Revised (LOT-R). Studies have shown that the revised LOT-R has good reliability and validity (Scheier, Carver, & Bridges, 1994; Tindle, et al., 2009). The measure has also been demonstrated to have good discriminant and convergent validity (Scheier, et al., 1994). A sample item is, “In uncertain times, I usually expect the best.” Participants are asked to rate the extent to which they agree with each item on a scale ranging from 1(strongly disagree) to 6(strongly agree). In total, six items were used to assess optimism (αW1=.75; αW2=.76). Three negatively worded items were reverse scored, and then all of the items were averaged to create a scale for optimism. Means and standard deviations for optimism at each wave are available in Table 1.
Table 1.
Correlations among primary study variables
| Mean (SD) | Wave 1
|
Wave 2
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| Wave 1 | 1. Gender | ||||||||
| 2. Age | 67.95 (9.09) | −.04** | |||||||
| 3. Optimism | 4.52 (.96) | .05** | .02 | ||||||
| 4. Health | 3.30 (1.05) | −.01 | −.08** | .31** | |||||
| 5. Conditions | 2.03 (1.39) | .02* | .24** | −.17** | −.46** | ||||
| Wave 2 | 6. Optimism | 4.50 (.96) | .06** | −.03* | .61** | .29** | −.18** | ||
| 7. Health | 3.19 (1.05) | .01 | −.11** | .29** | .64** | −.41** | .31** | ||
| 8. Conditions | 2.43 (1.47) | .01 | .23** | −.18** | −.46** | .87** | −.20** | −.46** | |
Note. N = 9790.
p < .05
p < .001.
Gender: −1 = male, 1 = female.
Health Measurements
Health was assessed at each wave using two different measurements at both waves. First, self-rated health was assessed with a single item, “Would you say your health is excellent, very good, good, fair, or poor?” Participants rated their health on a scale ranging from 1 (poor) to 5 (excellent). Means and standard deviations from health at each wave are available in Table 1.
Second, an index of eight major chronic illnesses was computed for each participant at each wave. Participants were asked to report if he or she was diagnosed by a physician with any of the following: (1)high blood pressure, (2)diabetes, (3)cancer or a malignant tumor of any kind, (4)lung disease, (5)coronary heart disease including heart attacks, angina, and congestive heart failure, (6)emotional, nervous, or psychiatric problems, (7)arthritis or rheumatism, and (8)stroke. The number of major health problems was summed so that higher values reflect more health problems. The means and standard deviations of chronic conditions at each wave are available in Table 1.
Self-rated health (negatively) and chronic illnesses (positively) were both skewed, such that a large number of participants reported good self-rated health and few chronic illnesses. In a set of supplementary analyses conducted post-hoc, root and inverse root transformations were applied to these variables and the analyses in the current study were re-run. Results from these analyses were in the same direction, significance, and magnitude as those presented below.
Results
Preliminary Analyses
Descriptive statistics and correlations among primary study variables are presented in Table 1. Optimism was associated with better self-rated health and fewer chronic health illnesses cross-sectionally within each wave. Also, optimism at Wave 1 was prospectively associated with better self-rated health and fewer chronic health conditions at Wave 2. Older age was associated with worse self-rated health and more chronic health conditions at each wave and lower optimism at Wave 2 only, although this association was small. Self-rated health and chronic illnesses were significantly correlated both within and between each wave. People with more chronic illnesses reported worse self-rated health on average. Further, women were younger than men in our sample and reported higher optimism at both waves.
The test-retest correlation for optimism over a four year period was .61, which is larger than the correlations found in the few studies that examined optimism’s stability over time. For example, optimism showed a 10-year test-retest stability of .35 among 61 law school students (Segerstrom, 2007). In a different sample of 30 subjects, “optimistic explanatory style” had a test-retest correlation of .13 over a 52-year period (Burns & Seligman, 1989). Our correlation may be larger because we examined people in older adulthood, a time when personality is more stable. Further, the time interval between assessments was shorter in this study, which typically translates into greater stability estimates due to autoregressivity (Fraley & Roberts, 2005).
Cross-Sectional Age Differences in Optimism at Time 1
We first examined how age was associated with optimism cross-sectionally given the wide age range (50–97 yrs old) of the sample. To formally model the associations between age and optimism, we conducted hierarchical multiple regression analyses predicting optimism at Wave 1 from the linear (age), quadratic (age2), and cubic effects of age (age3) at Wave 1, following the practice of other investigations of age differences in personality (Chopik, Edelstein, & Fraley, 2013; Srivastava, et al., 2003). Age was mean-centered prior to analysis, and the centered age term was used to compute the higher-order terms. Prior research suggests that the most complex age-personality relationships that can be meaningfully interpreted involve cubic terms (i.e., third-order terms; see Terracciano, McCrae, Brant, & Costa, 2005), so we did not test for more complex models.
We found that the quadratic effect of age was the best fit to the data for optimism, β= −.04, R=.04, F(2, 9,787)=7.02, p<.001. After including age2, the linear effect of age became significant, β=.02, p=.03, suggesting that the linear effect of optimism is positive at the average age. The inclusion of the cubic effect of age was not significant, p=.14. Gender did not moderate any of the associations between age and optimism (all ps>.41) nor did the associations between age and optimism change before or after controlling for gender.
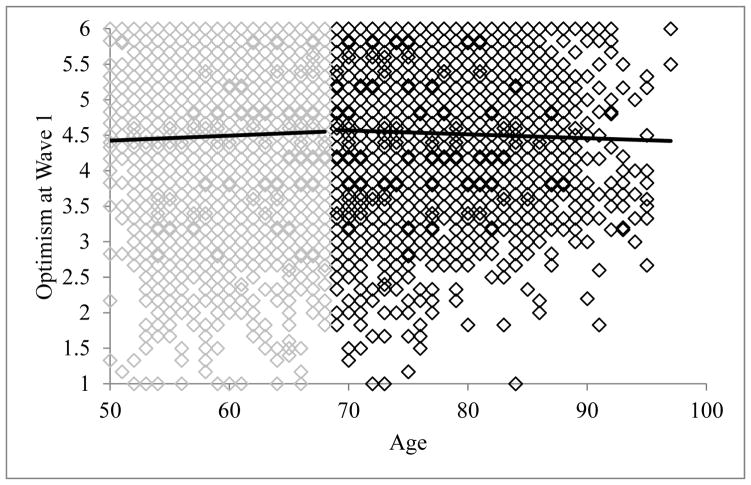
To probe whether the quadratic effect of age indeed yielded an inverted U-shape (such that optimism was positively associated with age until a certain point, after which it was negatively associated with age), we employed an approach recommended by Nelson and Simohnson (2014) to find the “xmax” or the age at which this association switches sign from positive to negative (creating a U-shape). These analyses constitute a “second look” at the data to find the point at which the U-shape “maxes out” and involves running additional linear regressions on the same data. Using their equation, the age at which the direction of the association changes was calculated to be 68.28 years. Indeed, among individuals age 68 and younger, the association between age and optimism was positive and significant, β=.04, p=.01. Among individuals older than 68, the association between age and optimism was negative and significant, β= −.03, p=.03. In Figure 1, the raw data are plotted and regression lines are fitted for individuals aged 68 and younger and individuals aged 69 and older, revealing that the data resembled an inverted U-shape pattern.
Figure 1.
Age differences in optimism at Time 1. Shading of the raw data is different before and after age 68—the identified xmax point of the quadratic function. Regression lines are linear slopes of age differences before and after age 68.
Moderated Latent Change and Correlated Change Models
Age differences in changes in optimism
We next examined whether different age groups changed in optimism at different rates from Wave 1 to Wave 2. This analysis provides an indirect test of whether the cross-sectional patterns observed between age and optimism are a result of developmental processes or special circumstances specific to any age/cohort group. Based on our cross-sectional results, we expected adults approximately age 68 and younger to increase in optimism from Wave 1 to Wave 2, as there is a plateau in optimism around that age group. Further, we expected the individuals over the age of 68 should decrease in optimism from Wave 1 to Wave 2, as optimism is lower in individuals over the age of 68. This pattern of increasing and then decreasing optimism would be captured in the curvilinear relationship we observed between age and optimism at Wave 1.
To examine age differences in the rates of change in optimism, we employed a moderated latent change approach (see Specht, Egloff, & Schmukle, 2011, for a similar approach as the current study). Recent innovations in modeling changes in personality as a latent intercepts and slopes in an SEM framework have supplanted simpler regression-based approaches (e.g., using difference scores and/or residualized change scores). This latent change approach has several benefits: the modeling of measurement invariance, the use of complete data (via full-information maximum likelihood (FIML) estimation), and the ability to selectively free and restrict estimated paths of interest (Hertzog & Nesselroade, 2003; Jackson & Allemand, 2014). Importantly, this latent change framework enabled us to test age differences in changes in optimism and whether changes in optimism were associated with changes in health (our next empirical question) within a single structural model. In this way, we were able to integrate two similar types of analyses—latent moderated change regression models (Specht, et al., 2011) and correlated change models (Allemand, et al., 2015; Takahashi, et al., 2013) into one framework to test both (a) moderators of changes in optimism and (b) the associations between changes in optimism and changes in health.
To test these hypotheses, we fit a latent moderated correlated change model using AMOS 22 (Arbuckle, 2014). Intercepts and slopes from two assessment waves were estimated for optimism (Specht, et al., 2011). Because health/illnesses were measured with single items, a latent intercept and slope factors were not generated for these outcomes. Thus, a separate path model was created in which health/illness at Time 1 predicted health/illness at Time 2 and the resulting error term was then related to the latent intercept and slope of optimism. The terms of age, age2, age3, gender, and education were entered into the model and were used as predictors of the intercepts and slopes of optimism and health/illnesses (at Time 1 and the error at Time 2). The overall fit for the models of self-rated health (CFI=.93, RMSEA=.06) and chronic conditions (CFI=.90, RMSEA=.08) were acceptable.
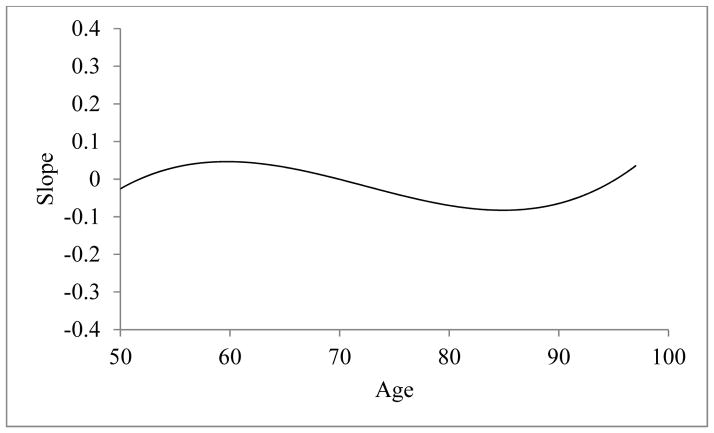
As in previous research (Allemand, Zimprich, & Hertzog, 2007), the intercept and slope for optimism were negatively related, r=−.38, p<.001, 95% CI[−.40, −.36]. This negative association indicates that participants with high scores on optimism at Time 1 showed less pronounced changes over time. The effects of age (β= −.07, p<.001) and age3 (β= −.04, p=.006) were significant predictors of the slope in optimism over the 4-year period. The effect of age2 was marginally significant, (β=.03, p=.07). The predicted values of the latent slope from age 50 to 97 are presented in Figure 2 (Specht, et al., 2011). The slope of changes in optimism was positive from age 50 to (approximately) age 70, depicting an increase in optimism over a four-year period among individuals aged 50 to 70. The slope of changes in optimism was negative after age 70, depicting a decrease in optimism over a four-year period among individuals over the age of 70. There was some evidence for small increases in optimism among the oldest participants (+95 years), but the sample sizes at these ages are relatively small, so caution should be used when interpreting this particular finding.
Figure 2.
Standardized age differences in mean-level change (latent slope) of optimism over 4 years, controlling for gender and education. Positive values indicate mean-level increases over the 4 year period; negative values indicate mean-level decreases over the 4 year period.
Correlated changes between optimism and health
As predicted, latent changes in optimism was correlated with changes in both health (r = .06, p < .001, 95% CI[.04, .08]) and chronic illnesses (r = −.03, p = .03, 95% CI[−.05, −.01]). These relationships suggest that increases in optimism were associated with higher levels of self-rated health and lower levels of chronic illnesses over a four-year period. Latent intercepts of optimism were also associated with changes in both health (r = .13, p < .001, 95% CI[.11, .15]) and chronic illnesses (r = −.08, p < .001, 95% CI[−.10, −.06]). These relationships demonstrate that individuals with higher levels of optimism at Time 1 had better self-rated health and fewer chronic illnesses over time.
Discussion
Our findings revealed that optimism progressively increased in adults from the age of 50 to about 70 years old, then decreased in adults over the age of 70, suggesting that optimism peaks at approximately this age (~age 68 in the cross-sectional analyses). Moreover, increases in optimism over a four-year period were associated with increases in self-reported health and fewer chronic illnesses over the same time frame. Although prior research alludes to some of these findings, this is the first study to examine how optimism changes in older adults and how these changes in optimism are related to changes in health.
Might changes in health be causing changes in optimism?
The analytic methods used in this study did not allow us to disentangle the causal direction of the association between changes in optimism and changes in health. However, based on a growing body of research, we believe that changes in optimism are contributing to changes in health. For example, experimentally induced optimism causes decreased pain sensation (Hanssen, et al., 2013). Optimism also remains stable before and after diagnoses of chronic illnesses, as well as before and after treatment, suggesting that changes in health do not cause changes in optimism (Schou, Ekeberg, Sandvik, & Ruland, 2005; Stanton & Snider, 1993; Stiegelis et al., 2003). Further, people do not biologically become healthier as they age, which would lead to the prediction that optimism would linearly decline throughout this period if optimism was just a proxy measure for forecasting one’s future health.
The causal arrow, however, may point in the other direction as well. We hypothesize that changes in optimism and health synergistically influence one another and move in upward or downward spirals, much like the broaden and build theory (Fredrickson, 2001). As Segerstrom (2007) suggests, future studies that have multi-wave and experimental designs will help isolate the causal relationships between optimism and health. As future waves of data are collected by the HRS, multi-wave analyses will become possible and future researchers should investigate this idea.
Another consideration is that there are a host of factors related to both optimism and health that were not included in the current report. For example, the current results (changes in optimism and changes in health being correlated) could also be partially explained by changes in subjective well-being, life circumstances, or another personality trait not modeled in the current analyses (Duckworth, Tsukayama, & May, 2010; Howell, Kern, & Lyubomirsky, 2007). Further, there is other research suggesting that personality and well-being change dramatically in response to life events and changes in health (Jokela, Hakulinen, Singh-Manoux, & Kivimaki, 2014; Lucas, 2007; Specht, et al., 2011). Worth noting, however, is that there is some evidence demonstrating that optimism has unique predictive effects, separate from other personality traits, life satisfaction, depression, affect, and a select number of life events (Carver, 2014; Kim, Chopik, & Smith, 2014; Kim, et al., 2011; Kim, Smith, et al., 2014; Schou, et al., 2005; Stanton & Snider, 1993; Stiegelis, et al., 2003). Nevertheless, future researchers should model simultaneous changes in several indicators of personality and well-being and then examine how these changes are related to changes in health and an individual’s life events and transitions (Jokela, et al., 2014; Specht, et al., 2011).
Strengths, Limitations, and Future Directions
Some of the effect sizes in this study were small to moderate. However, there are many examples where small effect sizes translate into meaningful outcomes. Therefore, findings should be interpreted in light of how constructs operate in the real world and how they may lead to the accumulation of positive assets across the lifespan (Abelson, 1985; Roberts, et al., 2006). Thus, the effects of optimism on health are most likely cumulative in nature. We previously discussed the potential mechanisms by which optimism may enhance health (e.g., enhanced health knowledge, health behaviors, social support, coping styles). The health enhancing effects that these mechanisms provide most likely accumulate over a period of years; therefore the amount of time that people were tracked in this study—four years—may be too short to allow these mechanisms to exact their influence on an individual across the lifespan. It is also plausible (and likely) that inter-individual differences exist in the link between optimism and health. There may be different subgroups of people who follow different trajectories of optimism, different rates of change in optimism, and as a result, different trajectories of health. Further, increases in optimism do not always translate to increases in health over time. The determinants and consequences of changes in optimism are also an area for future research.
Despite these limitations, our study also has several strengths. The HRS is one of the only nationally representative samples of older adults in the United States. Further, the few studies that have examined how optimism changes over time used correlations to compare optimism at one time point to optimism at a second, follow-up time point. We built upon the important work of these earlier studies by using latent change analyses to examine how optimism changes over time, how these changes differ by age, and the implications of these changes for health outcomes among older adults. We hope the preliminary findings in this study, combined with past studies linking optimism with enhanced health and health behaviors, will spark further conversations and research in this area. Further research down this avenue may reveal innovative ways of helping older adults not only live longer lives, but longer lives filled with good health and well-being.
Acknowledgments
Funding
The Health and Retirement Study is sponsored by the National Institute on Aging (NIA U01AG09740) and is conducted by the University of Michigan. Jacqui Smith’s contribution to this paper was partially supported by NIA U01AG09740
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abelson RP. A variance explanation paradox: When a little is a lot. Psychological Bulletin. 1985;97:129–133. [Google Scholar]
- Allemand M, Schaffhuser K, Martin M. Long-term correlated change between personality traits and perceived social support in middle adulthood. Personality and Social Psychology Bulletin. 2015;41:420–432. doi: 10.1177/0146167215569492. [DOI] [PubMed] [Google Scholar]
- Allemand M, Zimprich D, Hertzog C. Cross-sectional age differences and longitudinal age changes of personality in middle adulthood and old age. Journal of Personality. 2007;75:323–358. doi: 10.1111/j.1467-6494.2006.00441.x. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. AMOS. Vol. 22. Chicago: SPSS Inc; 2014. [Google Scholar]
- Bäckman L, MacDonald SWS. Death and cognition: Synthesis and outlook. European Psychologist. 2006;11:224–235. [Google Scholar]
- Baird BM, Lucas RE, Donnellan MB. Life satisfaction across the lifespan: Findings from two nationally representative panel studies. Social Indicators Research. 2010;99:183–203. doi: 10.1007/s11205-010-9584-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Social Science & Medicine. 2008;66:1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychological Bulletin. 2012 doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. Journal of Consulting and Clinical Psychology. 2009;77:1042–1054. doi: 10.1037/a0017671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns MO, Seligman ME. Explanatory style across the life span: Evidence for stability over 52 years. Journal of Personality and Social Psychology. 1989;56:471–477. doi: 10.1037//0022-3514.56.3.471. [DOI] [PubMed] [Google Scholar]
- Carstensen LL. The influence of a sense of time on human development. Science. 2006;312:1913–1915. doi: 10.1126/science.1127488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. Self-control and optimism are distinct and complementary strengths. Personality and Individual Differences. 2014;66:24–26. [Google Scholar]
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clinical psychology review. 2010;30:879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Chopik WJ, Edelstein RS, Fraley RC. From the cradle to the grave: Age differences in attachment from early adulthood to old age. Journal of Personality. 2013;81:171–183. doi: 10.1111/j.1467-6494.2012.00793.x. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. The ‘what’ and ‘why’ of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry. 2000;11:227–268. [Google Scholar]
- Duckworth AL, Tsukayama E, May H. Establishing causality using longitudinal hierarchical linear modeling: An illustration predicting achievement from self-control. Social Psychological and Personality Science. 2010;1:311–317. doi: 10.1177/1948550609359707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, Roberts BW. Patterns of continuity: A dynamic model for conceptualizing the stability of individual differences in psychological constructs across the life course. Psychological Review. 2005;112:60–74. doi: 10.1037/0033-295X.112.1.60. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Estabrook R, Schupp J, Wagner GG, Lindenberger U. Life satisfaction shows terminal decline in old age: Longitudinal evidence from the German Socio-Economic Panel Study (SOEP) Developmental Psychology. 2008;44:1148–1159. doi: 10.1037/0012-1649.44.4.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Röcke C, Lindenberger U, Smith J. Decline in life satisfaction in old age: Longitudinal evidence for links to distance-to-death. Psychology and Aging. 2008;23:154–168. doi: 10.1037/0882-7974.23.1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. Journal of Psychosomatic Research. 2007;63:483–490. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Hanssen MM, Peters ML, Vlaeyen JWS, Meevissen YMC, Vancleef LMG. Optimism lowers pain: Evidence of the causal status and underlying mechanisms. Pain. 2013;154:53–58. doi: 10.1016/j.pain.2012.08.006. [DOI] [PubMed] [Google Scholar]
- NIA, tranlator; I. f. S. Research, editor. Health and Retirement Study Data Files 2006. Ann Arbor: University of Michigan; 2006. [Google Scholar]
- Heinonen K, Räikkönen K, Keltikangas-Järvinen L. Dispositional optimism: Development over 21 years from the perspectives of perceived temperament and mothering. Personality and Individual Differences. 2005;38:425–435. [Google Scholar]
- Hertzog C, Nesselroade JR. Assessing psychological change in adulthood: An overview of methodological issues. Psychology and Aging. 2003;18:639. doi: 10.1037/0882-7974.18.4.639. [DOI] [PubMed] [Google Scholar]
- Howell RT, Kern ML, Lyubomirsky S. Health benefits: Meta-analytically determining the impact of well-being on objective health outcomes. Health Psychology Review. 2007;1:83–136. [Google Scholar]
- Jackson JJ, Allemand M. Moving personality development research forward: Applications using structural equation models. European Journal of Personality. 2014;28:300–310. [Google Scholar]
- Jokela M, Hakulinen C, Singh-Manoux A, Kivimaki M. Personality change associated with chronic diseases: pooled analysis of four prospective cohort studies. Psychological Medicine. 2014;44:2629–2640. doi: 10.1017/S0033291714000257. [DOI] [PubMed] [Google Scholar]
- Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45:169–176. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Kim ES, Chopik WJ, Smith J. Are people healthier if their partners are more optimistic? The dyadic effect of optimism on health among older adults. Journal of Psychosomatic Research. 2014;76:447–453. doi: 10.1016/j.jpsychores.2014.03.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Park N, Peterson C. Dispositional optimism protects older adults from stroke: the Health and Retirement Study. Stroke. 2011;42:2855–2859. doi: 10.1161/STROKEAHA.111.613448. [DOI] [PubMed] [Google Scholar]
- Kim ES, Smith J, Kubzansky LD. A prospective study of the association between dispositional optimism and incident heart failure. Circulation: Heart Failure. 2014 doi: 10.1161/CIRCHEARTFAILURE.113.000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimaki M, Vahtera J, Elovainio M, Helenius H, Singh-Manoux A, Pentti J. Optimism and pessimism as predictors of change in health after death or onset of severe illness in family. Health Psychol. 2005;24:413–421. doi: 10.1037/0278-6133.24.4.413. [DOI] [PubMed] [Google Scholar]
- Lucas RE. Adaptation and the set-point model of subjective well-being: Does happiness change after major life events? Current Directions in Psychological Science. 2007;16:75–79. [Google Scholar]
- Meevissen YMC, Peters ML, Alberts HJEM. Become more optimistic by imagining a best possible self: Effects of a two week intervention. Journal of Behavior Therapy and Experimental Psychiatry. 2011;42:371–378. doi: 10.1016/j.jbtep.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A., III Change in life satisfaction during adulthood: Findings from the Veterans Affairs Normative Aging Study. Journal of Personality and Social Psychology. 2005;88:189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- Nelson LD, Simohnson U. Thirty somethings are shrinking and other u-shaped challenges. 2014 Sep 17; Retrieved from http://datacolada.org/2014/09/17/27-thirty-somethings-are-shrinking-and-other-u-shaped-challenges/
- Nes LS, Segerstrom SC. Dispositional optimism and coping: A meta-analytic review. Personality and Social Psychology Review. 2006;10:235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- Netuveli G, Wiggins RD, Hildon Z, Montgomery SM, Blane D. Quality of life at older ages: Evidence from the English longitudinal study of aging (wave 1) Journal of Epidemiology and Community Health. 2006;60:357–363. doi: 10.1136/jech.2005.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters ML, Flink IK, Boersma K, Linton SJ. Manipulating optimism: Can imagining a best possible self be used to increase positive future expectancies? The Journal of Positive Psychology. 2010;5:204–211. [Google Scholar]
- Plomin R, Scheier MF, Bergeman CS, Pedersen NL. Optimism, pessimism and mental health: A twin/adoption analysis. Personality and Individual Differences. 1992;13:921–930. [Google Scholar]
- Radcliffe NM, Klein WMP. Dispositional, unrealistic and comparative optimism: Differential relations with the knowledge and processing of risk information and beliefs about personal risk. Personality and Social Psychology Bulletin. 2002;28:836–846. [Google Scholar]
- Rasmussen HN, Wrosch C, Scheier MF, Carver CS. Self-regulation processes and health: The importance of optimism and goal adjustment. Journal of Personality. 2006;74:1721–1747. doi: 10.1111/j.1467-6494.2006.00426.x. [DOI] [PubMed] [Google Scholar]
- Reed AE, Carstensen LL. The theory behind the age-related positivity effect. Frontiers in Psychology. 2012;3 doi: 10.3389/fpsyg.2012.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Wood D, Smith JL. Evaluating Five Factor Theory and social investment perspectives on personality trait development. Journal of Research in Personality. 2005;39:166–184. [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Schou I, Ekeberg Ø, Sandvik L, Ruland CM. Stability in optimism-pessimism in relation to bad news: A study of women with breast cancer. Journal of Personality Assessment. 2005;84:148–154. doi: 10.1207/s15327752jpa8402_04. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC. Optimism and resources: Effects on each other and on health over 10 years. Journal of Research in Personality. 2007;41:772–786. doi: 10.1016/j.jrp.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Specht J, Bleidorn W, Denissen JJA, Hennecke M, Hutteman R, Kandler C, … Zimmermann J. What drives adult personality development? A comparison of theoretical perspectives and empirical evidence. European Journal of Personality. 2014;28:216–230. [Google Scholar]
- Specht J, Egloff B, Schmukle SC. Stability and change of personality across the life course: The impact of age and major life events on mean-level and rank-order stability of the Big Five. Journal of Personality and Social Psychology. 2011;101:862–882. doi: 10.1037/a0024950. [DOI] [PubMed] [Google Scholar]
- Srivastava S, John OP, Gosling SD, Potter J. Development of personality in early and middle adulthood: Set like plaster or persistent change? Journal of Personality and Social Psychology. 2003;84:1041–1053. doi: 10.1037/0022-3514.84.5.1041. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Snider PR. Coping with a breast cancer diagnosis: A prospective study. Health Psychology. 1993;12:16–23. doi: 10.1037//0278-6133.12.1.16. [DOI] [PubMed] [Google Scholar]
- Stiegelis HE, Hagedoorn M, Sander-man R, van der Zee KI, Buunk BP, van den Bergh ACM. Cognitive adaptation: A comparison of cancer patients and healthy references. British Journal of Health Psychology. 2003;8:303–318. doi: 10.1348/135910703322370879. [DOI] [PubMed] [Google Scholar]
- Sweeny K, Krizan Z. Sobering up: A quantitative review of temporal declines in expectations. Psychological Bulletin. 2013;139:702–724. doi: 10.1037/a0029951. [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Edmonds GW, Jackson JJ, Roberts BW. Longitudinal correlated changes in conscientiousness, preventative health-related behaviors, and self-perceived physical health. Journal of Personality. 2013;81:417–427. doi: 10.1111/jopy.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, McCrae RR, Brant LJ, Costa PT. Hierarchical linear modeling analyses of NEO-PI-R scales in the Baltimore Longitudinal Study of Aging. Psychology and Aging. 2005;20:493–506. doi: 10.1037/0882-7974.20.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, … Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120:656–662. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trope Y, Liberman N. Temporal construal. Psychological Review. 2003;110:403–421. doi: 10.1037/0033-295x.110.3.403. [DOI] [PubMed] [Google Scholar]
- Wallace RB, Herzog AR. Overview of the health measures in the Health and Retirement Study. The Journal of Human Resources. 1995;30:S84–S107. [Google Scholar]
- Weiss A, King JE, Inoue-Murayama M, Matsuzawa T, Oswald AJ. Evidence for a midlife crisis in great apes consistent with the U-shape in human well-being. PNAS Proceedings of the National Academy of Sciences of the United States of America. 2012;109:19949–19952. doi: 10.1073/pnas.1212592109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston SJ, Jackson JJ. Identification of the healthy neurotic: Personality traits predict smoking after disease onset. Journal of Research in Personality. 2015;54:61–69. [Google Scholar]
- Zaninotto P, Falaschetti E, Sacker A. Age trajectories of quality of life among older adults: Results from the English longitudinal study of ageing. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. 2009;18:1301–1309. doi: 10.1007/s11136-009-9543-6. [DOI] [PubMed] [Google Scholar]