Abstract
Background
Although nurses are the most likely first responders to witness an in-hospital cardiac arrest (IHCA) and provide treatment, little research has been undertaken to determine what features of nursing are related to cardiac arrest outcomes.
Objectives
To determine the association between nurse staffing, nurse work environments, and IHCA survival.
Research Design
Cross-sectional study of data from: (1) the American Heart Association’s Get With The Guidelines-Resuscitation database; (2) the University of Pennsylvania Multi-State Nursing Care and and Patient Safety; and (3) the American Hospital Association annual survey. Logistic regression models were used to determine the association of the features of nursing and IHCA survival to discharge after adjusting for hospital and patient characteristics.
Subjects
A total of 11,160 adult patients aged 18 and older between 2005 and 2007 in 75 hospitals in 4 states (Pennsylvania, Florida, California, and New Jersey).
Results
Each additional patient per nurse on medical-surgical units was associated with a 5% lower likelihood of surviving IHCA to discharge (odds ratio = 0.95; 95% confidence interval, 0.91–0.99). Further, patients cared for in hospitals with poor work environments had a 16% lower likelihood of IHCA survival (odds ratio = 0.84; 95% confidence interval, 0.71–0.99) than patients cared for in hospitals with better work environments.
Conclusions
Better work environments and decreased patient-to-nurse ratios on medical-surgical units are associated with higher odds of patient survival after an IHCA. These results add to a large body of literature suggesting that outcomes are better when nurses have a more reasonable workload and work in good hospital work environments. Improving nurse working conditions holds promise for improving survival following IHCA.
Keywords: nursing, in-hospital cardiac arrest, cardiopulmonary resuscitation
Despite the resources and opportunity to intervene early when a cardiac arrest occurs in the hospital, fewer than a quarter of patients survive to discharge.1 Some hospitals, however, have been much more successful than others at improving survival following an in-hospital cardiac arrest (IHCA).2–6 One study showed that the odds on survival differed by as much as 42% for similar patients treated in different hospitals with similar characteristics.2 There is little evidence, however, to help explain why patients cared for in one hospital can fare so much better than a similar patient in another hospital, and importantly, what could be done to improve things
One possible explanation for the range in outcomes is variation in the identification of IHCA and initiation of an appropriate and timely response—the first link in the “chain of survival.”4,7–9 Nurses are the primary surveillance system in the highly complex hospital environment.10 Close patient observation and evaluation are defining characteristics of professional nursing.10 Nurses are at the bedside 24 hours a day, everyday; they are responsible for early warning system monitoring, they have direct knowledge of patient condition and changes in condition, and they are often the first on the scene of a cardiac arrest, initiate treatment, and coordinate the activities of others to save a patient’s life. Thus, nurses are ideally positioned to identify IHCA and mobilize lifesaving interventions.11–13
Research over the past decade has shown that sufficient nurse staffing levels and favorable work environments facilitate nurses’ effectiveness as a surveillance system. Staffing is important to surveillance because sufficient numbers of nurses are necessary to manage complex patient care needs, identify when something has gone wrong, and intervene rapidly to save patients’ lives. Nurses in good work environments have greater autonomy, control over their practice and resources, and excellent working relationships and communication with physicians, all of which can empower nurses’ ability and agency to act on behalf of patients. One example of this is the research on failure to rescue (FTR)—a measure created to assess a hospital’s ability to rescue patients who have developed serious complications. Measures of FTR have been endorsed by the National Quality Forum as nursing sensitive14 and by the Agency for Healthcare Research and Quality as a patient safety indicator.15 A significant body of evidence has shown that patients cared for in hospitals with better nurse staffing16–19 and better nurse work environments18–20 have lower odds of FTR.
Very few studies have examined any aspect of hospital nursing and the relationship with outcomes of cardiac arrest. Nurse staffing is the only nursing variable that has been studied. However, these studies have limitations. Chen et al21 found that nurse staffing was the only modifiable hospital factor associated with both decreased cardiac arrest incidence and improved survival to discharge. Although Chen and colleagues used the same patient data that we use, they were limited by having a measure of nurse staffing based on American Hospital Association (AHA) data, which have well-documented limitations,22 including the inability to distinguish bedside nurses from other registered nurses who do not provide direct patient care. Needleman et al16 found that better staffing was associated with lower rates of cardiac arrest using a better staffing measure but only had administrative patient data. Although standard administrative patient data files can be used to identify cardiac arrhythmias and cardiopulmonary resuscitation, they do not allow for patient risk adjustment based on detailed characteristics of the cardiac arrest event, such as the initial cardiac rhythm and whether the event was witnessed or not. No paper had a measure of the nurse work environment and thus, no studies have evaluated the relationship between nursing and IHCA outcomes using detailed measures of nurse staffing and nurse work environment linked with detailed patient registry data as we do in this study.
The aim of this study was to assess the relationship of nurse staffing and nursing work environment with survival following IHCA. We hypothesized that patients cared for in hospitals with lower patient to nurse ratios and better nursing environments would have better odds of survival to discharge following IHCA.
METHODS
This cross-sectional study linked data from 3 sources: (1) the American Heart Association’s Get With The Guidelines In-Hospital Cardiac Arrest-Resuscitation database (GWTG-R) (from which data on the characteristics and outcomes for patients who suffered IHCAs were obtained); (2) the University of Pennsylvania Multi-State Nursing Care and Patient Safety Survey (from which data on hospital nursing were obtained)23; and (3) the AHA’s annual survey of hospitals (from which hospital characteristics were obtained). Hospitals included in this study participated in the GWTG-R clinical registry between the years 2005 and 2007, responded to the 2006 AHA survey, and were in the 4 states studied in the nurse survey—Pennsylvania, New Jersey, California, and Florida. These states represent over 20% of hospital admissions nationally, and hospitals in these states are reasonably representative of hospitals nationally.23
Get With the Guidelines Resuscitation
Data for IHCA came from GWTG-R which is a large, prospective, national quality-improvement registry of IHCA sponsored by the American Heart Association. Trained quality-improvement hospital personnel enroll all patients with a cardiac arrest treated with resuscitation. Cases are identified by a centralized collection of cardiac arrest flow sheets, hospital paging system log reviews, routine code cart checks, pharmacy drug records, and hospital billing for resuscitation medications. The registry uses standardized Utstein-style24,25 definitions for all patient variables and outcomes to facilitate uniform reporting across hospitals. Data accuracy is ensured by rigorous certification of data abstractors and use of standardized software with data checks for accuracy and completeness with an error rate of 2.4%.26 Outcome Sciences Inc. serves as the data collection and coordination center for GWTG-R. The University of Pennsylvania serves as the data analytic center and has an agreement to prepare the data for research purposes. Further detail can be found in previous descriptions.27
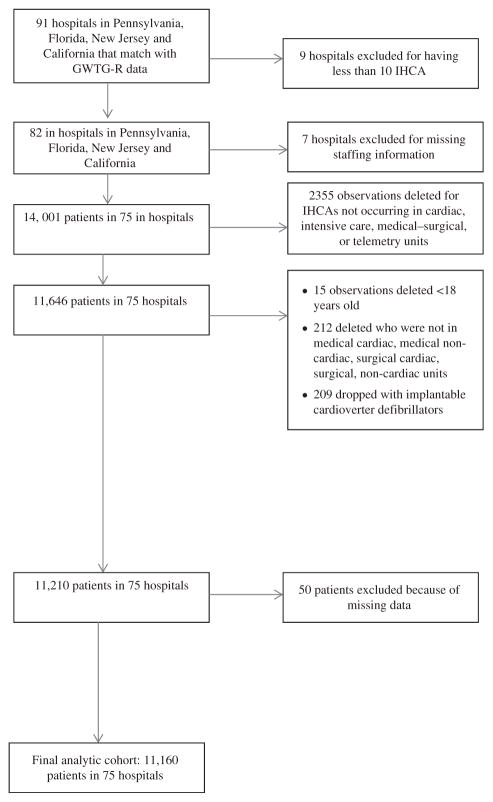
The patient population for the study was limited to patients on inpatient units at the time of IHCA who had initial documented rhythms of pulseless electrical activity, asystole, ventricular tachycardia, and ventricular fibrillation. Exclusion criteria included: (1) patients under the age of 18 (resuscitation guidelines differ for children); (2) unit type [obstetrics, pediatrics, psychiatry, rehabilitation, emergency departments, and procedural areas are excluded because our focus is on intensive care unit (ICU) and general medical-surgical areas]; and (3) patients with implantable cardioverter-defibrillators (a cardiac arrest primary prevention measure). The final analytic sample consisted of 11,160 adult patients in 75 hospitals that had information from all 3 data sources on patient characteristics, resuscitation outcomes, nursing resources, and hospital characteristics (Fig. 1). Analyses were restricted to hospitals with ≥ 10 cardiac arrests events in 2005–2007.
FIGURE 1.
Study cohort exclusion/inclusion criteria.
Multistate Nursing Survey
Nurse survey data were collected previously for another study in Pennsylvania, California, and New Jersey between September 2005 and August 2006 and in Florida between November 2007 and April 2008. More than 100,000 nurses responded to the survey, which was mailed to a large random sample in all 4 states. Their responses were aggregated by employing hospital, providing detailed information on 650 acute care hospitals, or almost all hospitals of over 100 beds in the 4 states; 601 hospitals had the required data on variables of interest from the nurse and AHA surveys. A full description of the survey method is described elsewhere.23
Measures
Each nurse surveyed reported the number of patients and the number of nurses on their last shift. We then created our aggregate measures of medical-surgical and adult ICU staffing for each hospital by dividing the average number of patients reported by nurses on their unit on their last shift by the average number of nurses on the unit for that same shift. We have found our direct survey measure of staffing to be superior to other data sources in predicting patient outcomes, possibly because it includes only bedside nurses.23,28
The 31-item Practice Environment Scale of the Nursing Work Index (PES-NWI)29 was used to measure the nurse work environment. The PES-NWI has been widely used in previous research,18,30,31 has established reliability and validity, and is an endorsed measure by the National Quality Forum.14 The scale indicates the degree (1 = strongly disagree to 4 = strongly agree) to which numerous organizational features are present in the current practice setting. Hospital-level measures were created by aggregating nurses’ responses to items comprising 4 of the 5 subscales: nurse participation in hospital affairs, nursing foundations for quality care, nurse manager ability, leadership, and support of nurses, nurse-physician relations. The Cronbach α for the subscales ranged from 0.71 to 0.84. The staffing/resource adequacy subscale was omitted because it was correlated with, and conceptually similar to, the direct measure of staffing. We then used these subscales to classify hospitals as having “poor,” “mixed,” and “good” work environments based on the number of work environment subscales that were above the median for all hospitals, where 0–1 subscales above the median represents a poor work environment, 2–3 above the median represents a mixed environment, and all 4 above the median represents a good work environment. Thus, hospitals in the “poor” category are those with work environments that are below the median on nearly every dimension, hospitals in the “good” category are those with work environments that are above the median for all hospitals on every dimension, and hospitals in the “mixed” category are the remainder, or those which are above the median on 2 or 3 dimensions.
We used additional control variables pertaining to hospital characteristics in our models adapted from the 2006 AHA hospital survey, which have been shown in previous research to be associated with patient outcomes.2,28,32 Hospital size was measured by number of beds to differentiate between hospitals with <250 beds, 251–500 beds, and >500 beds. Teaching status was categorized into nonteaching (no residents or fellows), minor teaching (≤ 1:4 residents/fellow to bed ratio), and major teaching (> 1:4). High-technology hospitals were identified by whether they had facilities for open-heart surgery, major organ transplants, or both. For-profit hospitals were distinguished from nonprofit hospitals. We created an indicator for hospitals in the top decile for the Medicaid percentage of inpatient days. We used an indicator for hospital state and whether the hospital was in an urban versus rural area. We also included a variable indicating whether the hospital was part of a multihospital system.
Our key outcome was a binary variable indicating whether a patient did or did not survive IHCA to hospital discharge. Our risk-adjustment approach was based on the model developed and validated by Chan et al33 that includes controls for age, select conditions present before IHCA (malignancy, septicemia, hepatic insufficiency, and hypotension), pre-IHCA critical care interventions (vasopressors, assisted/mechanical ventilation, and cardiac monitoring), and initial IHCA rhythm, all of which are strongly associated with IHCA survival.33 We also included variables indicating whether the arrest occurred in an ICU and for whether the arrest was monitored or witnessed.
Data Analysis
Hospital-level measures of nursing were derived from the nurse survey data and merged with categorical hospital characteristic data derived from the AHA annual survey and patient-level data from GWTG-R patient data, using common hospital identifiers. All data were deidentified before being returned to the investigators for analysis. The resulting analytic file included individual patient and event characteristics, as well as the nursing and organizational characteristics of the hospitals from which they were discharged. We first provide a description of the hospitals in the GWTG-R sample used in our analyses (n = 75). We also compared the characteristics of those hospitals with the hospitals that were represented in the nurse survey data but not in GWTG-R (n = 526). We then compared characteristics of the patients who survived to discharge with those who died before discharge using χ2 tests to determine the significance of the differences between them. Finally, logistic regression models that accounted for the clustering of patients within hospitals34 were used to estimate the size and significance of the associations between nurse staffing, nurse work environment, and patient survival following IHCA. Estimated odds ratios (ORs) from adjusted models show the effects of medical-surgical and ICU staffing, and poor work environment on the likelihood of surviving to discharge. Models were fit sequentially; the first model was a bivariate test of the effects of ICU staffing, medical-surgical staffing, and poor work environments on survival separately, without controlling for patient and hospital characteristics. The second model estimated the effects of nursing factors simultaneously, while also adjusting for hospital and patient characteristics.
RESULTS
Table 1 provides comparison information on the characteristics of the 75 GWTG-R hospitals and the other hospitals in the multistate sample (n = 526) to determine whether and how GWTG-R hospitals differed from hospitals in general. GWTG-R hospitals were significantly larger and more likely to be high-technology hospitals. GWTG-R hospitals were not significantly different from other hospitals with respect to teaching status, state, urban/rural location, system membership, for-profit status, or high Medicaid, nor with respect to nurse staffing levels and nurse work environments, which were the factors of greatest concern. Staffing in hospital medical-surgical units varied considerably (mean medical-surgical staffing = 7 patients per nurse, SD = 2.8). Staffing was less variable across hospital ICU settings (mean = 2.3, SD = 0.6).
TABLE 1.
Comparison of Hospital Characteristics in Get With the Guidelines (GWTG-R) Hospitals and Other Hospitals in the Multistate Hospital Sample
| Hospital Characteristics | N (%)
|
Significance (P) | ||
|---|---|---|---|---|
| GWTG-R Hospitals (N = 75) | Other Hospitals (N = 526) | Total (N = 601) | ||
| Beds | ||||
| ≤250 | 30 (40.0) | 310 (58.9) | 340 (56.6) | 0.008 |
| 251–500 | 35 (46.7) | 168 (31.9) | 203 (33.8) | |
| ≥501 | 10 (13.3) | 48 (9.1) | 58 (9.7) | |
| Technology status | ||||
| Not high | 34 (45.3) | 306 (58.1) | 340 (56.6) | 0.036 |
| High | 41 (54.7) | 220 (41.8) | 261 (43.4) | |
| Teaching status | ||||
| None | 31 (41.3) | 267 (50.7) | 298 (49.6) | 0.195 |
| Minimum | 35 (46.7) | 220 (41.8) | 255 (42.4) | |
| Major | 9 (12.0) | 39 (7.4) | 48 (7.9) | |
| Ownership | ||||
| Nonprofit | 60 (80.0) | 425 (80.7) | 485 (80.7) | 0.885 |
| For-profit | 15 (20.0) | 101 (19.2) | 116 (19.3) | |
| State | ||||
| California | 23 (30.7) | 212 (19.2) | 235 (39.1) | 0.461 |
| Florida | 23 (30.7) | 136 (25.9) | 159 (26.5) | |
| New Jersey | 10 (13.3) | 61 (11.6) | 71 (11.8) | |
| Pennsylvania | 19 (25.3) | 117 (22.2) | 136 (22.6) | |
| Location | ||||
| Urban | 71 (94.7) | 473 (89.9) | 544 (90.5) | 0.190 |
| Rural | 4 (5.3) | 53 (10.1) | 57 (9.5) | |
| System | ||||
| System member | 58 (77.3) | 362 (69.0) | 420 (69.9) | 0.133 |
| Not in system | 17 (22.7) | 164 (31.2) | 181 (30.1) | |
| % Medicaid | ||||
| High | 7 (90.7) | 59 (11.2) | 66 (10.9) | 0.626 |
| Not high | 68 (9.3) | 467 (88.7) | 535 (89.0) | |
| Work environment | ||||
| Poor | 28 (37.3) | 236 (44.9) | 264 (43.9) | 0.277 |
| Mixed | 22 (29.3) | 158 (30.0) | 180 (29.9) | |
| Good | 25 (33.3) | 132 (25.1) | 157 (26.1) | |
| ICU staffing | ||||
| < 2 patients/nurse | 23 (30.7) | 160 (30.4) | 183 (30.5) | 0.242 |
| 2–2.5 patients/nurse | 35 (46.7) | 201 (38.1) | 236 (39.3) | |
| > 2.5 patients/nurse | 17 (22.7) | 165 (31.4) | 182 (30.3) | |
| Medical-surgical staffing | ||||
| < 5 patients/nurse | 13 (17.3) | 105 (19.9) | 118 (19.6) | 0.238 |
| 5–7 patients/nurse | 36 (48.0) | 199 (37.8) | 235 (39.1) | |
| > 7 patients/nurse | 26 (34.7) | 222 (42.2) | 248 (41.3) | |
Significance (P) is the probability associated with the χ2 test to see whether the different hospital characteristics are identical in the 2 groups of hospitals.
GWTG-R indicates Get With The Guidelines-Resuscitation; ICU, intensive care unit.
Table 2 shows characteristics of the 11,160 IHCA patients in the 75 study hospitals. The mean patient age was 68 ± 15.6 years, 56% were male, and 17% were black. Overall, 15% of IHCA patients survived to discharge. Over half of IHCA occurred in the ICU, over 80% were witnessed, and 88% were monitored. Hypotension was the most common condition present before cardiac arrest. A shockable rhythm was initially present for 15% of patients. The likelihood of surviving to discharge was significantly related to all of the characteristics listed in the table.
TABLE 2.
Characteristics of IHCA Patients Who Died Before Discharge Versus Surviving to Discharge
| Patient Characteristics | N (%)
|
Significance (P) | ||
|---|---|---|---|---|
| Died Before Discharge (n = 9539) | Survived to Discharge (n = 1621) | Total (N = 11,160) | ||
| Arrest location | ||||
| Medical surgical unit | 3274 (82.2) | 711 (17.8) | 3985 (35.7) | < 0.001 |
| Intensive care unit | 6265 (87.3) | 910 (12.7) | 7175 (64.3) | |
| Monitored | ||||
| No | 1218 (88.2) | 163 (11.8) | 1381 (12.4) | < 0.001 |
| Yes | 8321 (85.1) | 1458 (14.9) | 9779 (87.6) | |
| Witnessed | ||||
| No | 1618 (86.8) | 246 (13.2) | 1864 (16.7) | 0.009 |
| Yes | 7921 (85.2) | 1375 (14.8) | 9296 (83.3) | |
| Initial shockable rhythm | ||||
| No | 8359 (88.4) | 1092 (11.6) | 9451 (84.7) | < 0.001 |
| Yes | 1180 (69.0) | 529 (31.0) | 1709 (15.3) | |
| Mechanical ventilation | ||||
| No | 5187 (81.0) | 1219 (19.0) | 6406 (57.4) | < 0.001 |
| Yes | 4352 (91.5) | 402 (8.5) | 4754 (42.6) | |
| Septicemia | ||||
| No | 7407 (83.7) | 1442 (16.3) | 8849 (79.3) | < 0.001 |
| Yes | 2132 (92.3) | 179 (7.7) | 2311 (20.7) | |
| Hepatic insufficiency | ||||
| No | 8609 (84.8) | 1540 (15.2) | 10149 (90.9) | < 0.001 |
| Yes | 930 (92.0) | 81 (8.0) | 1011 (9.1) | |
| Hypotension | ||||
| No | 6511 (82.9) | 1346 (17.1) | 7857 (70.4) | < 0.001 |
| Yes | 3028 (91.7) | 275 (8.3) | 3303 (29.6) | |
| Metastatic or hematologic malignancy | ||||
| No | 8201 (84.5) | 1499 (15.5) | 9700 (86.9) | < 0.001 |
| Yes | 1338 (91.6) | 122 (8.4) | 1460 (13.1) | |
| Intravenous vasopressor | ||||
| No | 6015 (82.3) | 1298 (17.7) | 7313 (65.5) | < 0.001 |
| Yes | 3524 (91.6) | 323 (8.4) | 3847 (34.5) | |
Significance (P) is the probability associated with the χ2 testing whether the likelihood of survival to discharge is independent of the different patient characteristics.
IHCA indicates in-hospital cardiac arrest.
Table 3 shows the results of fitting bivariate models, which estimate the effects of the different nursing factors and the other hospital and patient characteristics (one at a time) on the likelihood of surviving to discharge, and a multivariate model which estimates all effects simultaneously. In the multivariate models for which results are displayed in the table, some of the hospital characteristics were dropped when their effects were insignificant or did not significantly alter the effects of the nursing characteristics (Supplementary Digital Content 2, http://links.lww.com/MLR/B77 shows similar results for the full model). In both the bivariate and multivariate models, the effects of the different patient and event characteristics—the characteristics we thought might be potential confounds to estimating the effects of the nursing characteristics—are sizable and, in most cases, significant. Notably, patients with shockable rhythms were over 3 times as likely as patients without shockable rhythms to survive, even when other factors were taken into account, and patients who were being monitored were nearly twice as likely to survive. Patients who were mechanically ventilated were only half as likely to survive, and the odds on survival were also significantly diminished for patients with the other characteristics we considered, including septicemia, hepatic insufficiency, hypotension, and malignancies. What is most noteworthy for present purposes, however, is that in the final model, in which we estimate the effects of the nursing factors after taking account of these potential confounds, as well as other hospital characteristics, the effects of 2 of the 3 nursing characteristics remained sizable and significant. Although ICU staffing had no discernable effect on survival, either before or after adjustment, each additional patient per nurse on medical-surgical units was associated with a 5% (OR = 0.95; 95% confidence interval, 0.91–0.99) lower odds of survival to discharge in the adjusted model. Furthermore, there was a decreased likelihood of survival, by 16%, in hospitals with poor work environments (OR = 0.84; 95% confidence interval, 0.71–0.95). We also evaluated models (Supplementary Digital Content 2, http://links.lww.com/MLR/B77) focusing on ICU and medical-surgical patients separately. The results were qualitatively similar.
TABLE 3.
Unadjusted (Bivariate) and Adjusted (Multivariate) Odds Ratios Indicating the Effects of Nurse Staffing, the Nurse Work Environment, and Other Hospital and Patient Characteristics on Survival to Discharge (N = 11,160)
| Predictors | Odds Ratios
|
|
|---|---|---|
| Unadjusted (Bivariate) | Adjusted (Multivariate) | |
| Nursing characteristics | ||
| Intensive care unit staffing | 1.02 (0.86–1.21) | 1.02 (0.90–1.15) |
| Medical-surgical staffing | 0.94*** (0.92–0.97) | 0.95* (0.91–0.99) |
| Work environment | 0.70* (0.53–0.92) | 0.84* (0.71–0.99) |
| Other hospital characteristics | ||
| Beds | ||
| 251–500 | 1.19 (0.91–1.55) | 0.95 (0.79–1.15) |
| ≥501 | 1.08 (0.83–1.42) | 0.97 (0.83–1.12) |
| Teaching status | ||
| Minor | 0.87 (0.71–1.07) | 0.94 (0.79–1.14) |
| Major | 1.13 (0.70–1.82) | 0.92 (0.72–1.19) |
| Technology status | 1.32* (1.05–1.66) | 1.24** (1.06–1.43) |
| Urban | 1.22 (0.78–1.89) | 1.44** (1.12–1.85) |
| State | ||
| Pennsylvania | 0.86 (0.68–1.07) | 1.08 (0.84–1.39) |
| Florida | 1.15 (0.71–1.88) | 1.09 (0.87–1.36) |
| New Jersey | 0.92 (0.67–1.25) | 1.31* (1.05–1.64) |
| Patient and event characteristics | ||
| Age | 0.99* (0.99–1.00) | 0.99*** (0.98–0.99) |
| Arrest location in ICU | 0.67*** (0.55–0.81) | 0.86 (0.73–1.01) |
| Monitored | 1.31* (1.00–1.71) | 1.84*** (1.40–2.41) |
| Witnessed | 1.14 (0.99–1.32) | 1.38** (1.13–1.67) |
| Initial shockable rhythm | 3.43*** (2.68–4.39) | 3.21*** (2.57–4.02) |
| Mechanical ventilation | 0.39*** (0.34–0.45) | 0.48*** (0.41–0.57) |
| Septicemia | 0.43*** (0.35–0.53) | 0.59*** (0.49–0.72) |
| Hepatic insufficiency | 0.49*** (0.37–0.65) | 0.60*** (0.45–0.80) |
| Hypotension | 0.44*** (0.36–0.53) | 0.66*** (0.55–0.79) |
| Metastatic/hematologic malignancy | 0.50*** (0.40–0.62) | 0.51*** (0.41–0.64) |
| Intravenous vasopressor | 0.42*** (0.32–0.56) | 0.59*** (0.49–0.71) |
ICU staffing and medical-surgical staffing are measured by the ratios of patients to nurses; the work environment measure contrasts hospitals with poor environments with hospitals with mixed or good environments; the referent categories for beds, teaching status, technology status, and urban are <200 beds, nonteaching, nonhigh technology, and rural, respectively. Our models include dummy variables for state leaving one state as the reference category; age is coded in years; arrest location is coded as occurring on an ICU unit (1) versus medical-surgical unit (0); all other patient characteristics are coded as present (1) versus absent (0).
P < 0.05.
P < 0.01.
P < 0.001.
ICU indicates intensive care unit.
DISCUSSION
The study reported here is the first to describe the relationship between nursing factors and patient outcomes following in-hospital resuscitation, after taking into account other explanations, including patient severity of illness and clinical interventions. Our findings have implications for workforce interventions to improve patient outcomes.
Better work environments and lower patient to nurse ratios on medical-surgical units were associated with increased odds of survival after IHCA, even after taking into account other likely explanations. The likelihood of survival was 16% lower for patients cared for in hospitals with poor nursing work environments. In addition, the odds of survival were 5% lower for each additional patient per nurse on medical-surgical units. In contrast, there was no association between nurse staffing in ICUs and survival, most likely due to the national standardization of ICU nurse staffing at 2 patients per nurse, whereas nurse staffing in medical-surgical units varies substantially across hospitals. Thus, the interpretation is not that nurse staffing is any less important in the ICU than on medical-surgical units, but that detecting the impact of very small variations in ICU staffing in large, multihospital studies is difficult.
Prior research points to the importance of early detection of IHCA and rapid treatment. In our study, non-witnessed and nonmonitored arrests, in which response time to treatment is greater, occurred most frequently on medical-surgical units where there is most variability in nurse staffing. Considering our findings that survival is much better when patients are monitored, better targeted and increased use of cardiac monitoring would be a worthwhile consideration. Only 12% of patients, however, were not monitored. An advantage of focusing on nursing is that the benefits not only accrue to those at risk for IHCA as we show in this study, but, as the large body of literature has now shown, many populations at risk for multiple poor outcomes benefit (eg, mortality, FTR, and readmissions for general surgery patients, mortality and readmissions for medical patients, adverse events, infant outcomes). Ultimately, more monitors still require sufficient numbers of nurses to watch, interpret, and respond to them. In addition, poor work environments, which we found to be significantly associated with lower likelihood of survival independent of staffing levels, may have their effect because they are associated with in-efficiencies and interruptions that undermine nurses’ surveillance and mobilization of rapid treatment. Poor nurse and physician relationships for example, a component of our measure of work environments, may also add to delays in comprehensive treatment.35,36
Our results add to a growing body of research literature suggesting that improving hospital work environments may hold promise for reducing preventable deaths, and specifically for improving survival following IHCA. Our findings also supply additional evidence that adequate hospital nurse staffing may be an important strategy in efforts aimed at achieving excellent patient outcomes. Improving nurse staffing, however, may be difficult for some hospitals because of costs; nurse staffing accounts for over 40% of direct inpatient care costs.37 Improvement of work environments, in contrast, requires a change of interprofessional culture and extended delegation of care management to those care providers who are closest to patients. We have found in prior research that the relationship between staffing and outcomes can depend on having a good work environment.23 This suggests that adding more nurses without considering the work environment may be a poor investment. One potential pathway for dealing with the obstacles of culture change and achieving improved nurse work environments is the American Nurses Credentialing Center’s Magnet Recognition Program.38 Research suggests that Magnet programs tend have better work environments as measured empirically using the PES-NWI as in this paper.39
This study should be interpreted in the context of the following limitations. Foremost, because this study used a cross-sectional design, we cannot establish causality. Establishing causality would require, at a minimum, an alternative design with different data, and repeated measures over time. In addition, although GWTG-R allowed us to adjust for key variables that have been linked to survival, there may be other confounding variables not accounted for that might otherwise have influenced our findings. Participation in GWTG-R is voluntary, and as we have shown, hospitals that participate are larger and more likely to be high-technology hospitals compared with the full population of hospitals. Thus, care should be taken in generalizing our research findings from the GWTG-R hospitals to others, although there is evidence to suggest that nurse staffing and better work environments are associated with improved patient outcomes in representative groups of hospitals.23,40 Likewise, we expect that the GWTG-R hospitals have less variation than the general hospital population in terms of both staffing and work environment, which likely leads us to understate the relationship between these nursing factors and outcomes.
Adequate nurse staffing and good nurse work environments are associated with survival following an IHCA and are important to consider as factors to be modified in efforts to improve the survival of patients who experience a cardiac arrest in the hospital. Nearly half of IHCAs occur on medical-surgical units, which also have the most variable staffing levels and the most problematic work environments. Higher patient-to-nurse ratios on these units are associated with lower odds of survival after IHCAs. This study adds to the evidence that investment in nursing resources, particularly nurse staffing and work environments in medical-surgical units, should be considered as potentially important factors in efforts to improve patient survival following IHCA.
Supplementary Material
Acknowledgments
Supported by the National Institute of Nursing Research (R01NR04513 and T32NR0714, L.H.A.: PI), the National Institute on Aging (R01AG041099, M.D.M.: PI), and the American Association of Critical Care Nurses (M.F.R.: PI).
The authors would like to acknowledge the American Heart Association for providing access to the Get With The Guidelines-Resuscitation (GWTG-R) and to the hospitals that participated in the GWTG-R. The authors would like to thank Tim Cheney, Jesse Chittams, and Amy Praestgaard for their analytic support.
Footnotes
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Website, www.lww-medicalcare.com.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e1–e240. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merchant RM, Berg RA, Yang L, et al. Hospital variation in survival after in-hospital cardiac arrest. J Am Heart Assoc. 2014;3:e000400. doi: 10.1161/JAHA.113.000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan PS, Nichol G, Krumholz HM, et al. American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Hospital variation in time to defibrillation after in-hospital cardiac arrest. Arch Intern Med. 2009;169:1265–1273. doi: 10.1001/archinternmed.2009.196. [DOI] [PubMed] [Google Scholar]
- 4.Spearpoint KG, McLean CP, Zideman DA. Early defibrillation and the chain of survival in ‘in-hospital’ adult cardiac arrest; minutes count. Resuscitation. 2000;44:165–169. doi: 10.1016/s0300-9572(00)00158-1. [DOI] [PubMed] [Google Scholar]
- 5.Merchant RM, Yang LMS, Becker LB, et al. Variability in case-mix adjusted in-hospital cardiac arrest rates. Med Care. 2012;50:124–130. doi: 10.1097/MLR.0b013e31822d5d17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinha SS, Chen LM, Nallamothu BK. Survival by the fittest: hospital-level variation in quality of resuscitation care. J Am Heart Assoc. 2014;3:e000768. doi: 10.1161/JAHA.113.000768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Heart Association. [Accessed November 4, 2014];Chain of Survival. 2014 Available at: http://www.heart.org/HEARTORG/CPRAndECC/WhatisCPR/AboutEmergencyCardiovascularCareECC/Chain-of-Survival_UCM_307516_Article.jsp.
- 8.Cummins RO. The “chain of survival” concept: how it can save lives. Heart Dis Stroke. 1991;1:43–45. [PubMed] [Google Scholar]
- 9.Cummins RO, Ornato JP, Thies WH, et al. Improving survival from sudden cardiac arrest: the “chain of survival” concept. A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation. 1991;83:1832–1847. doi: 10.1161/01.cir.83.5.1832. [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine. Keeping Patients Safe: Transforming the Work Environment of Nurses. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 11.Fagin CM. When Care Becomes a Burden: Diminishing Access to Adequate Nursing. New York, NY: Milbank Memorial Fund; 2001. [Google Scholar]
- 12.Kutney-Lee A, Lake ET, Aiken LH. Development of the hospital nurse surveillance capacity profile. Res Nurs Health. 2009;32:217–228. doi: 10.1002/nur.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shever LL. The impact of nursing surveillance on failure to rescue. Res Theory Nurs Pract. 2011;25:107–126. doi: 10.1891/1541-6577.25.2.107. [DOI] [PubMed] [Google Scholar]
- 14.National Quality Forum. National Voluntary Consensus Standards for Nursing-Sensitive Care: An Initial Performance Measure Set. Washington, DC: National Quality Forum; 2004. NQFCR-08-04. [Google Scholar]
- 15.Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45:918–925. doi: 10.1097/MLR.0b013e31812e01cc. [DOI] [PubMed] [Google Scholar]
- 16.Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 17.Brooks-Carthon JM, Kutney-Lee A, Jarrin O, et al. Nurse staffing and postsurgical outcomes in black adults. J Am Geriatr Soc. 2012;60:1078–1084. doi: 10.1111/j.1532-5415.2012.03990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aiken LH, Clarke SP, Sloane DM, et al. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38:223–229. doi: 10.1097/01.NNA.0000312773.42352.d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friese CR, Lake ET, Aiken LH, et al. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv Res. 2008;43:1145–1163. doi: 10.1111/j.1475-6773.2007.00825.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boyle SM. Nursing unit characteristics and patient outcomes. Nurs Econ. 2004;22:111–123. [PubMed] [Google Scholar]
- 21.Chen LM, Nallamothu BK, Spertus JA, et al. Association between a hospital’s rate of cardiac arrest incidence and cardiac arrest survival. JAMA Intern Med. 2013;173:1186–1195. doi: 10.1001/jamainternmed.2013.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spetz J, Donaldson N, Aydin C, et al. How many nurses per patient? measurements of nurse staffing in health services research. Health Serv Res. 2008;43:1674–1692. doi: 10.1111/j.1475-6773.2008.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aiken LH, Cimiotti JP, Sloane DM, et al. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49:1047–1053. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on inhospital resuscitation: the in-hospital “Utstein style”. Ann Emerg Med. 1997;29:650–679. doi: 10.1016/s0196-0644(97)70256-7. [DOI] [PubMed] [Google Scholar]
- 25.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries.: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Southern Africa) Resuscitation. 2004;63:233–249. doi: 10.1016/j.resuscitation.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 26.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 27.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14 720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 28.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 29.Lake ET. Development of the Practice Environment Scale of the Nursing Work Index. Res Nurs Health. 2002;25:176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- 30.Lake ET. The nursing practice environment: measurement and evidence. Med Care Res Rev. 2007;64(suppl):104S–122S. doi: 10.1177/1077558707299253. [DOI] [PubMed] [Google Scholar]
- 31.Warshawsky NE, Havens DS. Global use of the Practice Environment Scale of the Nursing Work Index. Nurs Res. 2011;60:17–31. doi: 10.1097/NNR.0b013e3181ffa79c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carr BG, Goyal M, Band RA, et al. A national analysis of the relationship between hospital factors and post-cardiac arrest mortality. Intensive Care Med. 2009;35:505–511. doi: 10.1007/s00134-008-1335-x. [DOI] [PubMed] [Google Scholar]
- 33.Chan PS, Berg RA, Spertus JA, et al. Risk-standardizing survival for inhospital cardiac arrest to facilitate hospital comparisons. J Am Coll Cardiol. 2013;62:601–609. doi: 10.1016/j.jacc.2013.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rogers W. Regression standard errors in clustered samples. Stata Technical Bulletin. 1994;3:19–23. [Google Scholar]
- 35.Baggs J, Schmitt M, Mushlin A, et al. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit Care Med. 1999;27:1991–1998. doi: 10.1097/00003246-199909000-00045. [DOI] [PubMed] [Google Scholar]
- 36.Tschannen D, Kalisch BJ. The impact of nurse/physician collaboration on patient length of stay. J Nurs Manag. 2009;17:796–803. doi: 10.1111/j.1365-2834.2008.00926.x. [DOI] [PubMed] [Google Scholar]
- 37.Kane NM, Siegrist RB. [Accessed December 12, 2014];Understanding rising hospital inpatient costs: key components of cost and the impact of poor quality. 2002 Available at: http://www.selectqualitycare.com/SQC/Understanding%20Rising%20Hospital%20Inpatient%20Costs.pdf.
- 38.American Nurses Credentialing Center. The Magnet Model Components and Sources of Evidence: Magnet Recognition Program. Silver Spring, MD: ANCC; 2008. [Google Scholar]
- 39.Lake ET, Friese CR. Variations in nursing practice environments: relation to staffing and hospital characteristics. Nurs Res. 2006;55:1–9. doi: 10.1097/00006199-200601000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Aiken LH, Sloane DM, Bruyneel L, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383:1824–1830. doi: 10.1016/S0140-6736(13)62631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.