Abstract
To date, substantial evidence has shown a significant association between inflammatory bowel diseases (IBD) and development of colitis-associated cancer (CAC). The incidence/prevalence of IBD is higher in western countries including the US, Australia, and the UK. Although CAC development is generally characterized by stepwise accumulation of genetic as well as epigenetic changes, precise mechanisms of how chronic inflammation leads to the development of CAC are largely unknown. Preceding intestinal inflammation is one of the major influential factors for CAC tumorigenesis. Mucosal immune responses including activation of aberrant signaling pathways both in innate and adaptive immune cells play a pivotal role in CAC. Tumor progression and metastasis are shaped by a tightly controlled tumor microenvironment which is orchestrated by several immune cells and stromal cells including macrophages, neutrophils, dendritic cells, myeloid derived suppressor cells, T cells, and myofibroblasts. In this article, we will discuss the contributing factors of epithelial as well as immune cell signaling in initiation of CAC tumorigenesis and mucosal immune regulatory factors in the colonic tumor microenvironment. In depth understanding of these factors is necessary to develop novel anti-inflammatory and anti-cancer therapies for CAC in the near future.
Keywords: Colitis associated cancer, Sporadic colon cancer, Intestinal epithelial cells, Immune cells, Tumor microenvironment, Signaling molecule
Colorectal cancer is the second leading cause of mortality in the US and the third most common cancer when men and women are considered separately. The American Cancer Society has estimated approximately 93,090 new colon cancer patients in 2015. The association between inflammatory bowel disease (IBD) and colitis-associated cancer (CAC) has been identified about eight decades ago by Drs. Burrill Crohn and Herman Rosenberg (1). IBD is a group of inflammatory disorders and primarily includes ulcerative colitis (UC) and Crohn’s disease. Approximately 1.4 and 2.2 million people are affected with IBD in the US and Europe, respectively (2, 3). CAC contributes to 10–15% of death cases in IBD patients who have long standing (>10 years) and extensive inflammation in the colon. The risk of getting CAC increases by 2%, 8% and 18 % with the duration of UC diagnosis for 10, 20 and 30 years, respectively (4). The effect of pro and anti-inflammatory cytokines on immune and epithelial cells in combination with environmental and genetic factors results in CAC. Our current understanding of the pathogenesis of CAC, molecular signaling, and treatment strategies have improved the survival of CAC patients considerably. However, much more detailed functional studies are necessary to develop precise treatment strategies for CAC. This review will discuss the characteristics of Sporadic Colon Cancer and CAC, effect of inducible molecules on intestinal epithelial cells (IECs), role of tumor associated immune cells in CAC development, tumor microenvironment, and possible future therapeutics.
1. Sporadic Colon Cancer and Colitis Associated Cancer
Sporadic colon cancer and CAC are the two major forms of colon cancer. Tumorigenesis occurs when accumulation of selected genetic mutations leads to clonal expansion of cells by surpassing the balance between cell death and proliferation. Accumulation of mutations in oncogenes and tumor suppressor genes drive the initiation of sporadic colon cancer whereas chronic inflammation and immune dysregulation predispose dysplasia of intestinal epithelial cells and eventually lead to the development of CAC in IBD patients. Various risk factors are involved in the development of sporadic colon cancer and CAC including family history, age, gender, genomic instability, and severity of inflammation. Approximately 5–10% of colon cancers are initiated by heritable mutation. Most common hereditary-related cancer syndromes are hereditary nonpolyposis colorectal cancer (HNPCC), familial adenomatous polyposis (FAP), and MUTYH [mutY homolog (E. coli)]-associated polyposis (MAP). In the case of IBD, only 20% of patients have a family history of the disease. Accumulated evidence has shown that environmental changes play a pivotal role in IBD development, in particular changes in the composition of the intestinal microbiota. Genome-wide association studies (GWAS) have identified more than 180 susceptibility loci in association with Crohn’s disease (CD) and UC. A study by Khalili et al, analyzed the association between risk loci of CD and UC, and CAC using logistic regression modeling (5). They found that rs11676348, a susceptibility gene for UC, is inversely associated with colorectal cancer. This gene is located at chromosome 2 and correlated with the expression level of CXCR2. CXCR2 is strongly associated with CAC. However, direct role of rs11676348 in colorectal cancer is not elucidated yet. Population studies suggest that men are at slightly higher risk than women in developing colorectal cancer. Since mutations in normal IECs or mucosal immune cells occur randomly and at lower rates, development of sporadic colon cancer is slower and occurs at later age between 50 and 80 years old. Growing evidence shows that mean age of sporadic colon cancer development is 62.2 years old. Since the younger generation is highly susceptible to IBD (6), CAC development occurs between 15 and 30 years old. Based on the retrospective cohort study from 1975–2010 by Bailey et al, incidence rates of colon cancer and rectal cancer among the young patients (between 20 to 34 years old) tend to increase by 90% and 124.2%, respectively (7). However, the prognosis of both CAC and sporadic colon cancer is approximately 50% in 5 years period after the initial diagnosis of cancer (8, 9).
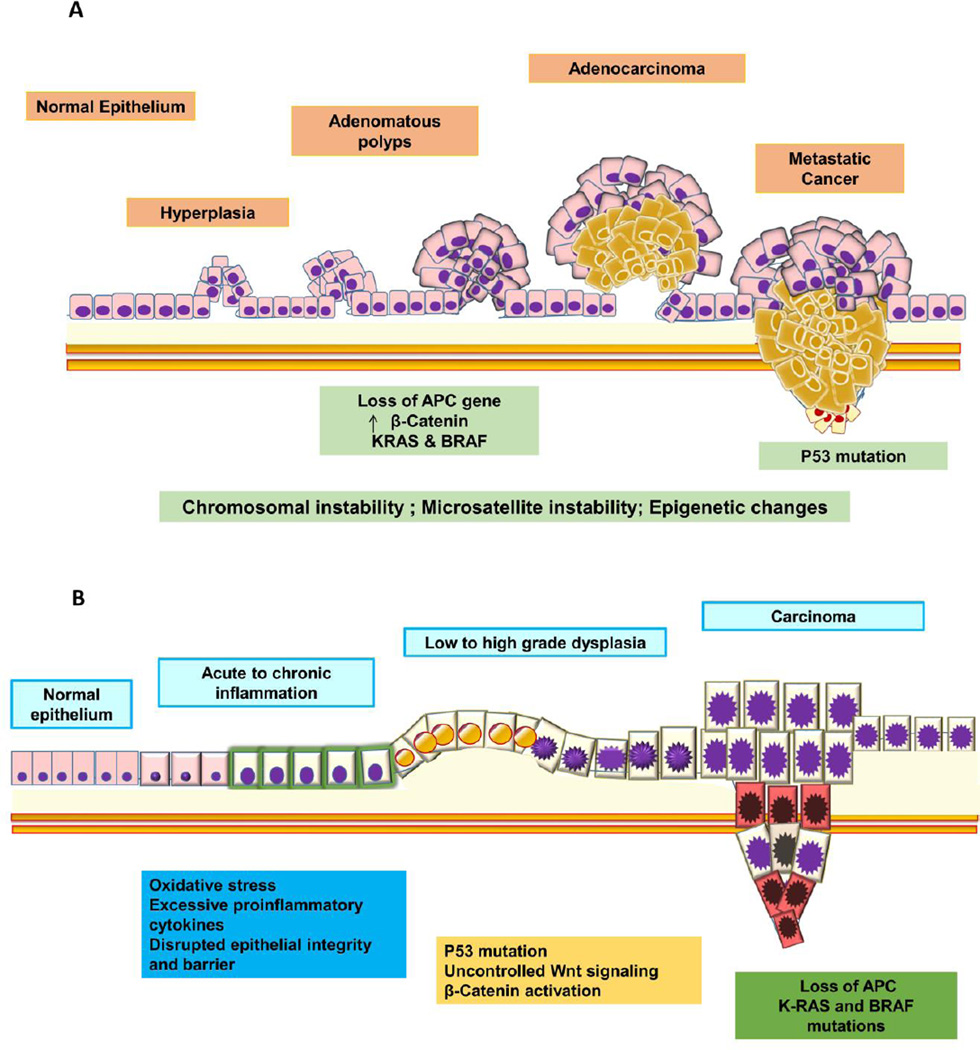
Genomic instability and epigenetic changes significantly contribute to the development of sporadic colon cancer. Chromosomal Instability (CIN) and MicroSatellite Instability (MSI) are the two main types of genomic instability factors which contribute 85% and 15% to the development of sporadic colon cancer, respectively (6, 10). CpG island methylation is one of the major epigenetic modifications, which alters the promoter region of the tumor-related genes and plays an important role in the development of sporadic colon cancer. Histone methylation in APC, INK4a, and MLH has been frequently observed in sporadic colon cancer: APC and INK4a are tumor suppressor genes and MLH controls DNA stability (11–13). Cumulative effects of CIN, MSI and CpG methylation result in continuous activation of Wnt/β-catenin signaling pathway and formation of adenomatous lesions in the colon. CAC pathogenesis is associated with the severity of inflammation. For example, IBD patients who have longer duration of the disease and chronic inflammation are more susceptible to CAC development. In addition, CIN, MSI and CpG methylation contribute to CAC to a certain degree, but the initiation, timing, location, and frequency of alterations in tumor related genes differ from sporadic colon cancer. Some distinct molecular mechanisms are involved in the initiation as well as the promotion of tumor development between CAC and sporadic colon cancer. Loss of adenomatous polyposis coli (APC) which is a tumor suppressor gene occurs due to CIN at the early stage of sporadic colon cancer and it occurs in a much later stage of CAC development with less frequency. APC inhibits β-catenin nuclear localization by sequestering in the cytoplasmic compartment (14, 15). Wnt dependent signaling leads to a proteolytic degradation of APC as well as translocation of β-catenin to the nucleus (16). Furthermore, mutations in p53, K-Ras and BRAF are associated with the neoplastic changes of IECs during the sporadic colon cancer development; BRAF and K-Ras mutations have been considered as prognostic markers for MSI (17). P53 and/or K-Ras mutations occur later in large adenomas of sporadic colon cancer patients. In contrast, cytokine stimulation and/or NF-kB activation drive p53 mutation in some inflamed mucosa and most of the non-dysplastic mucosa at early stages of CAC development (18). During acute and chronic inflammation, Tumor Necrosis Factor α (TNFα), Prostaglandin E2 (PGE2), NF-kB, and Akt signaling pathways lead to β-catenin activation independently from accumulated mutations (19–21). These signaling favor cell proliferation and initiation of tumorigenesis. Initiation of sporadic colon cancer and CAC occurs with adenomatous polyps and early dysplasia of epithelial cells with abnormal proliferation, respectively. In general, carcinogenic change to sporadic colon cancer is a stepwise progressive process from normal epithelium to the “adenoma-to-carcinoma sequence” (Fig.1A). In contrast, CAC follows the sequence of no dysplasia to indefinite dysplasia, low-grade dysplasia, high-grade dysplasia, and eventually to invasive adenocarcinoma, so-called the “inflammation-dysplasia-carcinoma sequence”(22) (Fig.1B). Although, initiation mechanisms of sporadic colon cancer and CAC are distinct from each other, both tumors show similar characteristics at the later stage. For example, K-Ras and BRAF mutations have been associated with some cases of CAC as well. Accumulated evidence has shown that the sporadic colon cancer tumor progression and metastasis are largely influenced by proinflammatory and anti-inflammatory cytokines as well as the other soluble factors, which are secreted by hematopoietic immune cells and non-hematopoietic cells including mainly IECs (23).
Figure 1.
A. Process of sporadic colon cancer development. Cumulative mutations due to chromosomal instability, microsatellite instability, and epigenetic changes result in DNA damage and loss of tumor suppressor genes including APC. These changes lead to clonal expansion of mutated IECs. Sporadic colon cancer development initiates from hyperplasia to adenoma and eventually into adenocarcinoma. B. Process of colitis associated cancer (CAC) development. Epithelial regeneration signaling is activated as a repair mechanism in response to chronic inflammation. Increased oxidative stress, aberrant inflammatory and tissue repair signaling lead to p53 mutation, Wnt signaling and β–catenin activation, which initiate dysplasia in IECs. Dysplasia in IECs progress to low to high grade dysplasia and eventually to carcinoma. Sustaining inflammation is the key for the development of CAC. Genetic and epigenetic changes in DNA further contribute to CAC carcinoma at later stage of carcinoma.
In addition, several studies have also reported the association between dysbiosis of microbiota, and development of sporadic colon cancer and CAC (24). Tjalsma et al proposed a “Driver-Passenger model” for colon cancer (25). Based on their model, bacteria with the pro-carcinogenic potential act as drivers and induce inflammation, which facilitates the growth of pathogenic or pro-biotic passenger bacteria. Most of the studies have characterized the bacterial/viral species/genus associated with tumor tissues (26, 27). In depth analysis of the strains of microbiota and its metabolomics are crucial to identify the involvement of unique microbiota composition in colon cancer. Furthermore, diet also play an important role in microbiota composition (28) However, identifying a specific set of microbiota as an aetiological agent is challenging because of the dynamic changes in the composition of microbiota during the course of disease progression.
2. Role of inducible molecules on intestinal epithelial cells (IECs) during the development of CAC
Numerous factors including tight anatomical barriers between IECs, pattern recognition receptors (PRRs) on IECs, its molecular signaling, cytokines, and growth factors play a significant role in the maintenance of epithelial homeostasis. The intestinal epithelial layer provides a first line of immune defense against luminal exogenous antigens, such as bacterial and food-related antigens. Loss of the epithelial barrier results in penetration of bacteria from lumen to lamina propria (LP) and initiation of the inflammatory cascade. Growth factors and pro-inflammatory cytokines may directly or indirectly stimulate IECs during inflammation and facilitate epithelial cell proliferation and restitution. Toll-like receptors (TLRs) and Nucleotide–binding domain and leucine-rich repeats (NLRs) have recently emerged as critical mediators of gastrointestinal inflammation which contribute to the initiation and progression of CAC. TLR signaling leads to the production of many proinflammatory cytokines including IL6. IL-6 mediated STAT3 activation plays a central role in IEC regeneration and proliferation (29–31). Other proinflammatory cytokines such as IL-17, IL-18, IL-22, and IL23 also contribute to CAC development and progression at different levels.
TLRs
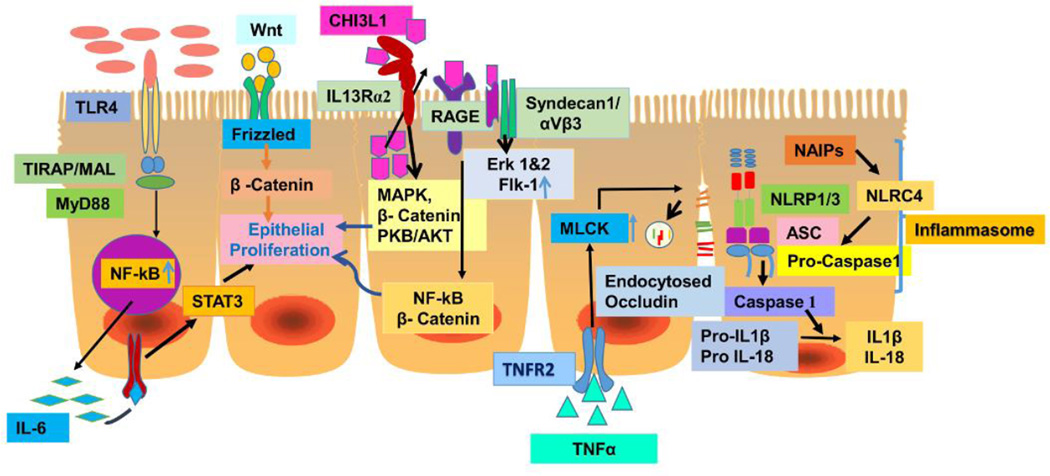
The TLR family consists of 10 and 13 receptors in humans and mice, respectively. TLRs are uniquely distributed in the gastrointestinal tract (GIT), which indicates how well their function is coordinated to maintain intestinal homeostasis. TLR2 and TLR4 are expressed at low levels in IECs and abundantly present in crypts of the colon. In contrast, TLR3 and TLR5 expression are predominantly present in mature enterocytes of small intestine and colon, and IECs of colon, respectively. IECs are continuously exposed to intestinal luminal antigens, microbes or microbial products. Interaction of TLRs with microbe associated molecular patterns (MAMP) initiates NF-kB signaling, which regulates intestinal homeostasis and cell repair through IL6/STAT3-dependent pathway. Uncontrolled NF-kB signaling results in hyper proliferation of IECs. Therefore, in healthy individuals, TLRs are hyporesponsive to prevent aberrant signaling of NF-kB. Negative regulators such as Toll-interacting protein (TOLLIP) and Single immunoglobulin IL-1R related molecule (SIGIRR/TIR8) inhibits aberrant signaling by TLR4 and maintain intestinal homeostasis in healthy individuals (32). TLR4 mediated inflammation is also attenuated by peroxisome proliferator activated receptor-γ (PPARγ). Growing evidence shows the close association between TLRs and CAC development. Increased expression of TLR 4, 5,7 and 8 have been reported in colon cancers and carcinoma cell lines (33). In particular, TLR4 expression has been shown to be upregulated in CAC lesions in humans and mice as well (34, 35). The role of TLRs has been demonstrated in mice which were induced to develop CAC using Azoxymethane (AOM) and dextran sulfate sodium (DSS). A combination of AOM and DSS are widely used to chemically induce tumorigenesis in the colon. AOM activates cyclooxygenase 2 (COX-2) and tyrosine kinase of epidermal growth factor receptor (EGFR), and suppresses TGF-β signaling. DSS is directly toxic to IECs and initiates inflammation (36). TLR4 knockout (KO) mice were resistant to develop CAC when they were induced tumors using AOM and DSS (37). Adoptive transfer of bone marrow (BM) cells from TLR4 KO mice to WT and, WT BM cells to TLR4 KO mice demonstrated that TLR4 expression in IECs is one of the critical factors for epithelial proliferation and CAC tumorigenesis (35). Myeloid differentiation factor 88 (MyD88) is the adaptor protein which mediates the formation of TLR2/4 signalsome and results in the nuclear translocation of NF-kB signaling (38). Studies have reported that MyD88 KO mice protect against CAC progression (39, 40). In contrast, some other studies showed that MyD88 KO mice are highly susceptible to colonic inflammation and CAC (41). It’s plausible that distinct TLR/other receptor-MyD88 signaling drive opposite outcome of the carcinogenic change of IECs. Although MyD88 can bind with TLR directly, TLR2 and 4 also bind with a second adaptor molecules called TIRAP [TIR (Toll-IL-1 receptor) domain-containing adapter protein], also known as Mal (MyD88 adaptor-like protein). A recent study by Aviello et al, demonstrated that Mal expression in IECs plays an important protective role against CAC (42) (Fig.2). The role of TLR2 in CAC has been reported in favor as well against CAC development. The function of TLRs in innate immune cells are like a double edged sword exhibiting anti-tumorigenic response as well as a pro-tumorigenic response as reviewed recently (43).
Figure 2. Colonic epithelial inducible signaling in CAC development.
TLRs and NLRs bind with microbe associated molecular patterns (MAMP) or microbial products. In particular, binding of LPS with TLR4 results in NF-kB signaling and induces IL-6 and other pro-inflammatory cytokine production. IL6-IL-6R interaction exerts uncontrolled STAT3 mediated cell proliferation and tumor. Signaling through different NLRs converts pro IL-1β and IL-18 into biologically active IL-1β and IL-18 either through forming inflammasome complex or independent signaling. NLRs have been shown to suppress CAC development. However, IL-18 has been reported to play a dual role in CAC. CHI3L1, a secretory molecule, binds with multiple receptors including RAGE, IL-13Rα2 and syndecan-1/αVβ3, and induces carcinogenic and angiogenic signals, which promote CAC initiation and progression. Wnt-β-catenin signaling is crucial in cancer initiation, progression and metastasis. In addition, epithelial barrier significantly contributes to the pathogenesis of CAC through facilitating chronic inflammation. TNFR2-TNFα interaction upregulates MLCK which results in internalization of occludins and loss of epithelial barrier. Multiple signaling pathways are simultaneously induced in IECs upon chronic inflammation, which initiate the transition from dysplasia to CAC and favor successful progression.
NLRs
NLRs belong to the PRR family and they significantly modulate IBD and CAC pathogenesis. NLRs include NLRP (pyrin domain-containing family), NLRC4 (CARD containing protein), and NAIP (apoptosis inhibitory protein). Single Nucleotide Polymorphisms (SNPs) in a variety of NLRs including NOD1 and NLRP3 are known to predispose IBD. GWAS studies have identified a link between NLRP1 mutation and CD development (44–46). Growing evidence has shown the association between NLRP1, NLRP3, NLRC4, NLRP6, and CAC. NLR, the adaptor protein ASC and caspase1 compose a macromolecular scaffold complex called an inflammasome. Activation of NLR through microbes or damage-associated molecular patterns (MAMP/DAMP) leads to activation of caspase 1, which converts pro-IL-1β and pro-IL-18 into biologically mature and active IL-1β and IL-18 (Fig.2). ASC KO and Caspase 1 KO mice treated with DSS and DSS/AOM were highly susceptible to UC and CAC, respectively. A study by William et al, analyzed the expression of 25 NLR and NLR-associated genes in human IECs and monocytes and confirmed NLRP1 as the only NLR highly upregulated in IECs (47). They further demonstrated that NLRP1 is a critical modulator which attenuates IBD and CAC using a DSS/AOM model. Adoptive bone marrow transplantation of Nlrp1b KO to WT mice clearly demonstrated that NLRP1 attenuates CAC through non-hematopoietic cells (mainly IECs). Levels of IL-1β and IL-18 were low in these KO mice. Contributions of IL-1β and IL-18 cytokines to CAC pathogenesis remain highly controversial. There is a number of evidence to support that IL-18 is essential to protect from CAC, however there are also reports refuting this that indicate IL-18 promotes CAC: It is likely that higher concentrations of IL-18 promote tumorigenesis and optimum concentration of IL-18 prevents tumorigenesis (48–51). However, the cutoff point remains elusive. Expression analysis of various NLRs in colon cancer tissue from human patients resulted in significant down-regulation of NLRP1, up-regulation of NLRP3 and NLRC4, and unchanged NLRP6 (47). NLRP12 KO mice were highly susceptible to UC and CAC due to increased production of proinflammatory cytokines, tumorigenesis factors, chemokines, and failure to control NF-kB activation in activated macrophages (52).
NLR family apoptosis inhibitor proteins (NAIPs) play a key role in suppressing CAC. NAIPs have four functional copies including 1,2,5,6 and two noncoding copies in mice. NAIPs are highly expressed in colon and innate immune myeloid cells. Since NAIPs have three BIR (Baculovirus Inhibitor of apoptosis protein Repeat) domains, it’s likely that NAIPs can function alone or in combination with NLRC4 in an inflammasome complex. Epithelial specific NAIP1-6 KO mice showed significantly increased tumorigenesis in the colon independently from IL-1β and IL-18, which indicates epithelial NAIPs protect against CAC development (53). In addition, down regulation of NAIPs in colon tumor tissues have also been reported (54).
Chitinase 3-like 1 (CHI3L1/YKL-40)
CHI3L1 is a pseudo-chitinase and a secretory glycoprotein with a chitin-binding motif (55). It is expressed by various cell types including IECs, macrophages, neutrophils, chondrocytes, and vascular smooth muscles. Increased serum levels of CHI3L1 have been shown in several inflammatory conditions in human and animal models. In IBD patients, both message and protein levels of CHI3L1 are significantly upregulated in IECs and macrophages during the development of intestinal inflammation (56–58). In response to an injury due to inflammation, CHI3L1 is secreted in the lung as well as in the colon to maintain mucosal homeostasis by promoting epithelial cell restitution (57). Studies have shown elevated levels of CHI3L1 in IBD and CAC patients although the expression is completely absent in the colon of healthy individuals (57, 59). CHI3L1 has been widely reported as a potential diagnostic and prognostic biomarker for solid tumors (60, 61). Our recent AOM/DSS model studies showed that high endogenous CHI3L1 expression enhances epithelial proliferation, which promotes carcinogenic changes of IECs (61). Interestingly, CHI3L1 synergistically activates IL-6-mediated STAT3 signaling in IECs and results in tissue regeneration and proliferation (62). To examine the distinct functional roles of CHI3L1 in hematopoietic and non-hematopoietic lineages, we generated bone marrow chimeras in CHI3L1 KO and WT mice in an AOM/DSS-induced CAC model (63). We found that non-hematopoietic lineage, including IECs, is indeed the major source of CHI3L1, which promotes CAC tumorigenesis and epithelial proliferation. CHI3L1 level proportionately increases with severity of inflammation. In chronic inflammatory conditions, it competes with S100A9, one of the DAMP molecules, in a concentration dependent manner and binds with cell surface molecule RAGE (Receptor for Advance Glycation End Product) which results in tumorigenesis via enhanced activation of NF-kB, β-catenin, and MAPK signaling pathways (63). RAGE is a multi-ligand pattern recognition receptor which initiates cellular activation of multiple pathways and is involved in carcinogenesis of various solid tumors. Its ligands are AGE (advanced glycation end products), amyloid β-peptide, HMGB1 (DNA binding protein high mobility group box-1, S100/calgranulins and CHI3L1 (63, 64). RAGE is expressed in IECs and primarily concentrated at lateral membranes of IECs close to the apical cell junction complexes (65). Similarly, CHI3L1 has the ability to bind with multiple receptors (Fig.2) and elicit a variety of cellular responses: Recently, the Elias group elegantly proved that the catalytic domain of CHI3L1 can specifically bind with the extracellular domain of IL13Rα2, which binding is independent from IL13 and induces MAPK p42/p44 (Erk 1/2), AKT, and Wnt/β-catenin signaling (66). Heparan sulfate chains of Syndecan-1 also interact with CHI3L1 and coordinate Syndecan-1/αVβ3 signaling. This interaction has been shown to induce Erk1/2 in macrophages and promote angiogenesis in the tumor microenvironment by increasing Flk-1 expression and sensitizing the angiogenic responses to VEGF (67, 68). Overall, CHI3L1 regulates multiple cellular responses including apoptosis, pyroptosis, inflammasome activation, wound healing, tumorigenesis, and angiogenesis due to its ability to bind with different receptors.
Myosin light chain kinase (MLCK)
The epithelial barrier is important to maintain mucosal homeostasis between intestinal micobiota and interstitium. In vitro studies have demonstrated various cytokine dependent mechanisms of epithelial barrier disruption. The barrier loss occurs either due to downregulation of tight junction protein expression, decreased Na+K+ATPase production, cytoskeletal contraction, or increased apoptosis/cell death of IECs. Phosphorylation of mysoin II regulatory light chain by MLCK leads to cytoskeletal contraction, which in turn results in disruption of the epithelial barrier. In fact, increased MLCK expression has been reported in IECs during the development of IBD and CAC (69). Persistent MLCK over-expression in IECs promotes MLCK-mediated occludin internalization, which results in disruption of tight junctions. Consequently increased permeability of IECs and paracellular influx of luminal contents lead to immune activation with uncontrolled cytokine production in intestinal LP cells. Studies have shown that TNFR2 signaling in IECs up regulates MLCK and epithelial barrier loss. Blockade of either TNFR2 or MLCK protein expression restored tight junction integrity and attenuated IBD as well as CAC development (70–72).
3. Role of tumor-associated cells in intestinal inflammation
Innate and adaptive immune cells play a pivotal role in the development of CAC. Selected signaling pathways in IECs and myeloid immune cells show opposite function in CAC initiation and progression. For example, IKKβ/NF-kB signaling in IECs plays a pivotal role in CAC tumorigenesis. IEC specific of IKKβ KO increased apoptosis of tumor cells and decreased colonic tumor incidence, but did not affect inflammation. In contrast, depletion of IKKβ in immune cells reduced the colonic tumorigenesis and inflammation but not affected the rate of apoptosis of tumor cells (73).
Macrophages
Tissue-resident macrophages are abundant in the colon and are recruited to the LP by endogenous chemoattractants in non-inflamed mucosa, while circulatory macrophages migrate to LP in response to proinflammatory chemokines during intestinal inflammation. Tissue-resident macrophages exhibit functions of proinflammatory modulation and phagocytic/bactericidal activities (74). During the course of intestinal inflammation, circulatory macrophages mount a typical proinflammatory phenotype and play an indispensable role in IBD and CAC pathogenesis. Polarized macrophages are classified into two types: 1. Classically activated macrophages (M1 phenotype), which secrete proinflammatory cytokines including TNFα, IL1-β, IL-6 and IL-12 and produce reactive oxygen (ROS) and nitrogen species (RON). 2. Alternatively activated macrophages (M2 phenotype) which promote production of anti-inflammatory cytokines including IL-10 and TGFβ, and enhanced tissue repair by favoring cell proliferation. Inflammation-dependent oxidative stress induces mutations in IECs and lead to their carcinogenic changes, as seen in UC patients who have highly activated leukocytes which generate excessive ROS and RON productions (75). A study by Wang et al, characterized M1/M2 macrophages to be involved in CAC initiation, promotion and metastasis. They found that M2 macrophages play a significant role in development of CAC and functional changes occur in M1 macrophages which promote CAC without alteration in polarization (76). Several studies have reported different markers for M1, M2, M1-like-M2 and M2 subtypes, however the phenotypic and functional classifications are ambiguous. Of note, mouse M2 macrophages generally express mammalian chitinases including CHI3L1, CHI3L3 (YM1) and CHI3L4 (YM2). P38/MK2 [mitogen-activated protein kinases (MAPK)-activated protein kinase 2 (MK2)] pathway activation in macrophages has also been shown to partly contribute to the development of CAC (77). TAMs (tumor-associated macrophages), mostly M2 macrophages, play an important role in tumorigenesis, metastasis, immune suppression and angiogenesis by producing various cytokines and growth factors (78, 79). Growth factors and cytokines secreted by tumor cells and other infiltrating cells change the phenotype of recruited circulatory macrophages. There is evidence that peritumoral TAMs exhibit antitumor property and improve survival of cancer patients (80). Based on several studies, it seems that TAMs function and prognosis of cancer patients differ with their localization in tumors (81, 82).
Neutrophils
Neutrophils are the most abundant leukocytes in the blood and play an important role in first line defense. These cells respond to chemokine signals and migrate to the site of infection and/or inflammation efficiently. Neutrophils are critical to control infection and inflammation, however if inflammation is uncontrolled, it can lead to severe tissue injury and promote tumorigenesis. Neutrophils secrete both pro- and anti-inflammatory cytokines, and contribute to angiogenesis and immune surveillance. Recent studies indicated that neutrophils also assume pro-tumorigenic phenotype (N2) and promote neoplastic changes of IECs. Based on the inflammatory milieu, they could differentiate either N2 or anti-tumorigenic phenotype (N1), which are similar to macrophage phenotypes (83, 84). Studies have suggested that peripheral neutrophil to lymphocyte ratio can be potentially used as one of the predictive and prognostic factors for CAC (85, 86).
Neutrophils secrete cytokines and chemokines including TNFα, IL1-β, IL-8, as well as other chemokines including CCs and CXCs. CXCR2 on the surface of neutrophils binds with CXCL1, 2, 3 and 5 and recruits neutrophils to the site of inflammation. In addition, myeloperoxidase (MPO) is considered as a commonly used marker for neutrophil infiltration in inflammation and tumors. Methylation status of RUNX3 (Runt-related transcripton factor 3), which is a putative tumor suppressor gene, as well as TNFα polymorphism, and MPO in UC-associated cancer tissues showed a positive correlation with the severity of the tumor development (87). Mice treated with AOM/DSS showed significant increase in CXCR2 expression in neutrophils. Serine proteases including elastase, cathepsin G, proteinase 3, and matrix metalloproteinase (MMP)-8 and −9 are present in the secondary granules of neutrophils and promote tumorigenesis. Depletion of neutrophils with Ly6G antibodies ameliorated CAC development in terms of tumor number and size (88). It is likely that blocking CXCL2-CXCR2 will also reduce the risk of CAC by controlling neutrophil infiltration in chronic colitis.
Dendritic cells (DCs)
Several studies have reported an infiltration of DCs in inflamed tissues of CAC patients. DCs act as sentinel cells and directly capture luminal antigens by using their long processes which travel in between epithelial cells to maintain intestinal homeostasis (74). T-bet, a transcription factor which is required for the priming of Th1 cells, is highly expressed in DCs but not in macrophages. Depletion of T-bet exclusively in innate immune cells [T-bet × Rag double KO (DKO), so called TRUC] in mice resulted in uncontrolled chronic inflammation and subsequent CAC development, suggesting the immunoregulatory and anti-tumorigenic roles of T-bet expression in DCs (89). Since T-bet is a TNFα repressor in DCs, over-expression of T-bet selectively in DCs also markedly reduced the severity of chronic colitis and the incidence of CAC development.
T cells
In contrast to innate immune cells, which act as a first line of defense, acquired immune cells aggravates the inflammation and tissue injury in IBD by activating inflammatory signaling pathways in mucosal tissues. These cells may also lead to CAC initiation if the inflammation is chronically perpetuated. Different subsets of T cells play distinct roles in inflammation, tumor initiation, progression and anti-tumor immunity. When CD4+ T cells get activated, they differentiate into distinct T helper (Th) subsets including Th1, Th2, Th17 and Tfh (follicular helper CD4 T cells) based on their ability to produce cytokines and transcription factors. For example, cytokines such as TGFβ, IL-6, IL-21 and IL-23 and transcription factors including STAT3, ROR γ (retinoic acid receptor- related orphan receptor γ), RORα, IRF4 (interferon regulatory factors), AhR (aryl hydrocarbon receptor) and Batf (Basic Leucine Zipper Transcription Factor, ATF-Like) influence Th17 differentiation. Each of these subsets secretes different types of cytokines and elicits diverse immune responses. Th1 immunity completely arrests the tumor growth via TNFα- and IFNγ-mediated signaling pathways. Th2-deficient mice (IL4 KO) treated with AOM and trinitrobenzene sulfonic acid (TNBS), which induces Th1-type colitis, developed significantly less colonic tumor as compared to Th1-deficient mice (IFNγ KO). This result indicates that Th2 cells specifically promote tumorigenic changes of IECs under inflammatory conditions in the colon (90). Rag1 × CD4 DKO mice developed chronic DSS colitis although tumor formation was markedly reduced in AOM/DSS-induced colitis. Human studies have shown higher infiltration of Th17 cells in UC and CAC colonic tissues. A recent study by Martin et al, demonstrated that absence of ROR γ -dependent Th17 cells induces chronic colitis but fewer macroscopic tumor formation in an AOM/DSS mouse model (91). It suggests that tumor initiation itself was not inhibited but the cell proliferation was not accelerated due to the absence of RORγ- dependent Th17 cells. Furthermore, this study confirmed that tumor cell proliferation is partially regulated by RORγ expressing hematopoietic cells.
Presence of CD3+,CD8+, CD45RO+, and granzyme B+ cells in human colonic tumors is positively associated with disease prognosis (92). CD8+ cytotoxic T cells are known to elicit anti-tumor immune response. Presence of higher number of CD8+ T cells and lower number of FoxP3+ cells in colonic tumors reflect favorable prognosis in CAC patients (93, 94). Successful control of intestinal pathology depends on the balance between Th cells, CD8+ T cells and regulatory T cells (Tregs). Based on cellular phenotype, Tregs can be classified as CD4+CD25+ FoxP3+ cells and CD8+CD25+FoxP3+ cells. The number of CD8+ Tregs is 100 times less than CD4+ Tregs. Adoptive transfer of Foxp3+ Tregs improved the IBD outcome in mice and studies suggested that increasing number of Tregs could replace immunosuppressive drugs. In contrast, increased number of Foxp3+ Tregs in tumors suppresses anti-tumor immunity elicited by Th1 cells and CD8+ cytotoxic T cells, and result in tumor progression. Transient ablation of Tregs in an AOM/DSS mouse model indicates that reduction/absence of Tregs promote effective anti-tumor immune response. Depletion of Tregs resulted in the increase of CD8+ effector Tcells with elevated level of IFNγ and granzyme B productions, and the ultimate death of neoplastic cells in CAC (95).
A unique subset of T cells called invariant natural killer (iNKT) T cells express NK receptor and invariant T cell receptor (TCR) α chain. A few studies have shed some light on the anti-tumor role of iNKT cells by inhibiting IL-13 production in NK1.1+ T effector cells and mononuclear cells in inflamed colon (96).
Myeloid-derived suppressor cells (MDSCs) and innate lymphoid cells (ILCs)
MDSCs are heterogeneous myeloid progenitor cells including immature granulocytes, macrophages and DCs. MDSCs highly contribute to tumor immune evasion by suppressing T cell-mediated anti-tumor effects and other innate immune cell signaling (97). During the course of chronic inflammation, proinflammatory cytokines such as IL-6, IL-1β and PGE2 recruit MDSCs which suppress anti-tumor immunity and immune surveillance (98). MDSCs suppress the activities of T cells and other innate immune cells through distinct mechanisms including production of arginase, ROS and nitration of TCR. Increased level of CCL2 and MDSCs infiltration have been reported in patients with CACs, colonic adenoma and sporadic colon cancer.. Chun et al, showed that CCL2 promotes CAC tumorigenesis by recruiting monocytic MDSCs and polymorpho nuclear (PMN)-MDSCs to suppress effector T cell function via iNOS and STAT3 dependent ROS production, respectively (99). Depletion of CCL2 prevented the progression of CAC and accumulation of MDSCs around the tumor.
ILCs, predominantly found in gut associated lymphoid tissue (GALT), are an emerging new set of innate immune cells which contribute to initiation and regulation of inflammation. ILCs can be classified into three different types, ILC1, 2 and 3, based on the functional criteria. Different studies have shown increased or decreased number of proinflammatory ILC3s in IBD patients as well as in mouse models of colitis. These discrepancies could be due to the differences in characterization of ILCs by different groups and heterogeneity in the unitized mouse models. A study by Kirchberger et al, concluded that ILCs mediate bacteria-induced CAC through IL-22 production using a Helicobacter hepaticus-infected AOM model (100). Depletion of ILCs with anti-Thy1 antibody reduced the severity of colonic inflammation as well as the incidence of CAC development in this model. The role of ILCs at different stages of inflammation in various organs has been extensively reviewed recently (101), which suggest that ILCs also contribute to anti-tumor immunity by limiting inflammation in contrast to their pro-tumorigenic characterisitics.
Myofibroblasts (MFs)
Intestinal MFs in the LP contribute to tissue repair, inflammation, angiogenesis and fibrosis. In particular, MFs play an important role in maintaining IEC homeostasis by providing a niche rich in non-canonical Wnts, extracellular matrix and growth factors. Similarly, MFs also contribute to carcinogenesis and play a pivotal role in tumor microenvironment (TME). A study by Vermeulen et al, demonstrated that stemness of colon cancer cells is maintained by hepatocyte growth factor (HGF)-secreted by MFs in TME (102). Wnt gene expression profiling analysis of MFs of normal and UC patients revealed down regulation of secreted frizzled-related protein (SFRP), a natural Wnt inhibitor, in MFs of UC patients (103), which shows that UC patients with down-regulation of SFRP are at higher risk of CAC development. Tumor progression locus 2 (Tpl2) is a serine-threonine kinase which belongs to the MAPK family and is involved in colonic inflammation and oncogenesis. MF specific ablation of Tpl2 in mice resulted in increased number and size of tumors, increased epithelial proliferation and reduced apoptosis in an AOM/DSS mouse model (104). Furthermore, Tpl2 deficient mice showed increased expression of HGF in colon. Furthermore, Tpl2 suppresses the colonic tumorigenesis by regulating TGFβ and HGF/c-met pathways in IECs. Based on a result of inhibition experiment, CCL3-CCR5 axis seems to be involved in the recruitment and accumulation of fibroblast in TME as well as the CAC development via suppressing the expression of heparin binding epidermal growth factor–like–growth factor (HB-EGF) (105). In human primary MFs, TNFα induces epidermal growth factor receptor (EGFR) expression and binding of EGF-EGFR induces ERK signaling activation, which results in increased Cox2 expression (106, 107). Whole genome profiling has shown that in both CAC patients and a murine AOM/DSS cancer model, there is an increased epiregulin expression which is mainly produced by MFs. A study by Neufert et al, showed that epiregulin producing MFs in TME promotes tumor-growth via ERK-induced IEC proliferation (108). MFs also secrete fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF) which contribute to angiogenesis in TME.
4. Tumor microenvironment (TME)
Successful initiation, progression and metastasis of colorectal cancer depends on the micro environment surrounding the tumor. Inflammation and inflammatory mediators are the major contributors of TME. In general, IBD patients with chronic inflammation tend to have frequent flare up and disease history for more than 10 years. Due to chronic inflammation, loss of epithelial integrity and increased intestinal permeability are observed in these patients over time. Disruption of epithelial barrier allows luminal microbiota to enter freely into the LP and will further activate immune cells which result in secretion of proinflammatory mediators (23). Selected microbes are likely to be involved in tumor initiation in addition to inducing UC. For example, Enterotoxic Bacteroides fragilis is known to cause UC and also promote CAC by cleaving E-cadherin and inducing β-catenin signaling activation (109, 110). Studies have shown the enrichment of microbes in tumor tissues (26) which provoke the question whether these microbes promote tumorigenesis, progression and metastasis.
TME consists of various interplayers including tumor cells, stromal cells, infiltrating immune cells, vasculature, extracellular matrix (ECM) and ECM-associated molecules. A variety of cells infiltrate tumor-environment including TAMs, neutrophils, DCs, CD4+ T cells, CD8+ T cells, MDSCs, NK cells, mast cells, endothelial cells, endothelial progenitor cells (EPCs), platelets, fibroblasts and mesenchymal stem cells (MSCs) (Fig.3). M1 macrophages are part of Th1 response and M2 macrophages are part of Th2 response: M1 contributes to chronic inflammation by producing TNFα, IL-12, IL-23, ROS and RON, while M2 macrophages secrete low levels of IL-12 and high levels of IL-10, decoy R, IL-1RA, CCL17, and CCL22 chemokines. Change in the M1/M2 macrophage phenotype promotes tumor initiation, progression and metastasis. In the study by Wang et al, although M1 phenotype did not change in CAC tissues in an AOM/DSS mouse model, functional changes were similar to M2 phenotype (76). Infiltration of significant M2 polarized TAMs in TME have been reported as a poor prognostic indicator. TNFα, IL-6 and IL-8 secreted by macrophages and neutrophils promote infiltration of T cells and MDSCs. Macrophage and neutrophil products of oxidative stress (e.g., ROS and RON) result in DNA damage and p53 mutation in IECs. Pro-myelopoietic factors such as GM-CSF (granulocyte macrophage colony stimulating factor), IL-6, VEGF and M-CSF (macrophage colony stimulating factor) produced in the TME lead to the expansion of MDSCs. Increased expression of arginase1 and inducible nitroxide synthase by MDSCs deplete anti-tumor effective T cells and promote FoxP3+ Tregs in the environment. MDSCs and Tregs suppress the antitumor immunity and favor tumor progression. The NF-kB and IL-6–STAT3-mediated signaling pathways are critical for cell proliferation and tumor metastasis. IFNγ is responsible for early inflammation and is involved in anti-tumor property at later stage.
Figure 3. Components of tumor microenvironment (TME).
After initiation of tumor, progression and metastasis depend on tightly controlled TME. TME is infiltrated with immune cells including TAMs, TANs, DCs, MDSCs, CD4+ Tcells, CD8+ Tcells, Tregs and CAFs, pro and anti-inflammatory cytokines, and growth factors. New blood vessel networks around the tumor provide nutrients and oxygen for the survival of tumor cells and tumor associated cells. Signaling from stromal cells contribute to the stemness of the cancer cells.
Epithelial mesenchymal transition (EMT) is an important process in inflammation, wound healing and cancer. Epithelial cells obtain the characteristics of fibroblast, and loss of tight junction, desmosomes, and gap junction results in the failure of cell-cell interaction. Expression of fibroblast markers such as fibronectin, α–SMA (α–smooth muscle actin) and matrix metalloproteinases increase during EMT process (111). EMT is largely controlled by cytokines and particularly TGF-β signaling controls the EMT by inducing SMAD (contraction of Sma and Mad)/Snail/EMT pathway (112). TNFα stabilizes Snail, a key transcription factor, involved in the last step of EMT. In addition, NF-kB and STAT3 also play a role in EMT process (113–115). Accumulating evidence suggests that the proinflammatory cytokines such as TNFα, IL6 and IL8 substantiate the EMT process. Since cytokines drive the EMT process, mesenchymal cells differentiate back to epithelial cells in metastasized organ due to low gradient /absence of cytokines in that environment.
The increased distance between the tumor cell and blood vessels reduces the chance of getting oxygen and decreases the survival of tumor cells. Therefore, neoangiogenesis in TME is vital to provide sufficient oxygen and nutrients to tumor cell survival (Fig. 3). VEGF contributes to the new blood vessel network. Inhibition of VEGF dramatically reduced the tumor development, angiogenesis and cell proliferation (116). In addition to angiogenesis, VEGF signaling through VEGF receptor 2 promotes tumor cell proliferation in a STAT3 dependent manner. TAMs over-express VEGF and also other pro-angiogenic factors including MMP7, MMP12, and COX2, which contribute to angiogenesis in TME. Prothrombin, a clotting factor for the normal coagulation of blood, is another factor which contributes to initiation and metastasis of CAC (117), and its deficiency reduces the precancerous aberrant crypt foci.
During tumor initiation, surrounding stromal cells mount suppressive response to tumor development. However, subsequent dynamic interaction between tumor cells and stromal cells changes in favor of tumor progression and metastasis with reversible or irreversible genetic mutations/modifications in stromal cells. Cancer-associated fibroblasts (CAF) promote the tumor growth by producing several growth factors including EGF, hepatocyte HGF and FGF. Increased levels of stromal fibroblast activated protein (FAP) have been correlated with an increased risk of tumor metastasis and progression (118). Aberrant activation of Wnt signaling is considered as one of the major pathways in cancer biology. It is a notion that all IECs have tumorigenic capacity. Regardless of this notion, immunohistochemical studies on colorectalcarcinoma (CRC) cells showed non-homogenous distribution of nucleus β-catenin. This finding has shed some light that only a subset of CRC cells have the stem cell-like property and others loose the tumorigenicity after differentiating into neoplastic cells. A study by Vermuelen et al, demonstrated that CRC stemness is closely regulated by TME and tumor-initiating cells (TIC) (102). Wnt/ β-catenin signaling in TICs is induced by HGF secreted by MFs. TME is distinct from the normal tissue environment and consists of unique phenotype of TAMs, neutrophils, MDSCs, stromal cells, cytokines and secretory molecules. Therefore, targeting TME components for therapeutic purposes will benefit prevention of tumor progression and metastasis.
5. Signaling molecules as therapeutic targets
CAC seems to be preventable if inflammation is controlled effectively and properly. Even after developing CAC, there are several treatment options including surgery, chemotherapy, radiation therapy, cancer-targeted therapy and immunotherapy. The treatment strategy with the greatest chance of cure is surgery, which resects localized cancers, specifically in early-stage tumors. Chemotherapy is controlling cancer by drugs and is often paired with radiation therapy, which uses high energy particles or waves to destroy cancer cells, which result in reduction of tumor size. General drugs used in chemotherapy also cause damage in normal cells to certain extent, to remedy this; cancer-targeted therapy may be used by specifically targeting unique properties of cancer cells, which reduces the risk of destroying normal cells. Another strategy is immunotherapy, which stimulates one’s own immune system to fight against cancer. To effectively treat cancers, a combination of these therapies is often used. Cancer treatment should be targeted against cause, molecules-involved in promoting cancer signaling pathways, and immune/stromal cells involved in tumorigenesis, progression, and metastasis. In addition, accumulated evidence has clearly indicated the importance of targeting tumor microenvironment.
As we discussed above, chronic inflammation is one of the major contributing factors for CAC development in IBD patients. Therefore, anti-inflammatory drugs are given to patients to control inflammation, which reduces the risk of neoplastic changes in IECs. Corticosteroids have been used for a long time to control IBD and effectively reduce the CAC risk but also suppress the general immune system which makes the patients susceptible to infections and other complications (119, 120). CAC has also been associated with primary sclerosing cholangitis in IBD patients (121). Studies have suggested that using Ursodeoxycholic acid (UDCA) reduces bile acids and lowers the risk of CAC in a dose dependent manner (121–123). Studies have shown that excess bile acids particularly secondary bile acids in the colonic lumen increase the risk of IBD as well as CAC development using animal models (124). Also correlated with IBD is folate deficiency, (125–127) and folate supplements will likely reduce the risk of CAC. Statins, a class of drugs that can help lower cholesterol levels in the blood, have also been shown to reduce the risk by 47% in patients who were diagnosed with colorectal tumors (128).
5-amino salicyclic acid (5-ASA) or mesalamine is widely used as maintenance therapy for UC. 5-ASA inhibits the NF-kB pathway, which promotes proliferation of IECs and chronic inflammation. Velayos et al, performed a meta-analysis of 9 studies that included a total of 1932 patients and demonstrated a protective effect of 5-ASA to CAC (129). In contrast, a study by Terdiman et al, concluded that 5-ASA is not effective in patients who was treated with this compound for about 12 months, which indicates that the period of treatment plays a significant role in the outcome (risk/protection) of CAC (130). Other promising chemical compounds like sesquiterpene, lactones-like parthenolide, and micheliolide have been shown to exhibit anti-inflammatory effects by inhibiting the NF-kB signaling pathway which results in the attenuation of IBD and CAC in AOM/DSS mouse model (131).
Histone deacetylase (HDAC) inhibitors are another therapeutic strategy for CAC treatment and have been also utilized in other cancer clinical trials currently. HDAC modulates the acetylation state of different transcription pathways including NF-kB signaling pathway. The pro-apoptotic characteristic of HDACs makes them good candidates for anti-cancer drugs. Glauben et al, reported that HDAC inhibitor ITF2357 attenuates CAC by inhibiting IFNγ production, NF-kB activation, and increasing apoptosis of mononuclear cells in the LP (132, 133). Pro-biotic bacterial metabolites such as butyrate and acetate are considered as a class of HDAC inhibitors. These short chain fatty acids have the anti cancerous, anti inflammatory and anti proliferative properties. Few clinical trials on probiotic effect of Lactobacillus species against colon cancer showed suppression of the diseases (134, 135). However, the sample size of these studies is not sufficient to draw a definitive conclusion.
Modulating inflammation is a prerequisite for CAC prevention. Blocking TLRs and MLCK using antibodies may attenuate the disease development. However, TLRs intervention should be done without altering the beneficial effect of TLR. CHI3L1 is highly involved in promoting inflammation-associated tumorigenesis and angiogenesis, and therefore neutralizing CHI3L1 by anti-CHI3L1 antibodies will potentially reduce the tumor development and progression. Since CHI3L1 binds with multiple receptors (Figure 2), inhibiting one receptor will not completely abrogate CHI3L1-mediated signaling pathways.
Experimental and clinical data have shown that anti-inflammatory cytokines/receptors can be used as therapeutic targets for CAC prevention. Anti-TNFα antibodies are extensively used in IBD patients, in particular CD patients (136). As we discussed above, IL-6–STAT3 signaling plays a central role in CAC pathogenesis. Increased level of IL-6 trans signaling through soluble IL-6 receptor has been reported in IBD and CAC. Glycoprotein 130 (gp130) is a natural inhibitor of IL-6 trans signaling but not membrane bound IL-6R signaling, which is why gp130 fusion antibodies have been proposed for therapeutic use in CAC. IL-6 stimulates the differentiation of Th1 to Th17 cells, which is the major source of IL-17. An increased level of IL17 has been associated in IBD as well as CAC pathogenesis (137). Blocking of IL-17A and/or IL-17F has attenuated the chronic inflammation and CAC tumorigenesis as well (138). IL-22 has been shown to induce CAC and inhibition of IL-22 significantly attenuated CAC development compared to IL-17 inhibition (100). IL-10 is an anti-inflammatory cytokine which suppresses IBD and CAC. In fact, IL-10 KO mice are highly susceptible to UC and CAC due to uncontrolled inflammation in the colon (139, 140). IL-15 suppresses CAC by promoting anti-tumor immunity by CD8+ T cells and NK cells (141). Several studies have shown that either inhibition of a combination of proinflammatory cytokines, cytokine receptors or addition of recombinant anti-inflammatory cytokines will likely reduce the CAC in IBD patients.
VEGF is playing a major role in forming new blood vessel networks around tumors. Targeting VEGF or VEGFR directly inhibits the angiogenesis and survival of tumor cells. Several clinical trials are ongoing, targeting VEGF (by anti-VEGF antibodies) and VEGFR (by adoptive cell therapy).
COX-2 and prostaglandin E2 (PGE2) genes are one of the first responsive genes to be expressed by IECs and inflammatory cells in response to growth factors and proinflammatory cytokines during inflammation (142). Nuclear hormone receptor peroxisome proliferator-activated receptor δ (PPARδ) is a ligand dependent transcription factor which plays an important role in CAC. Downstream signaling of PPARδ-mediated COX-2/PGE2 signaling significantly contributes to chronic inflammation and CAC by maintaining the cross talk between neoplastic IECs and TAMs (143). In contrast, Ishikawa and Herschman reported expression of COX-1 and COX-2 is not necessary for CAC using an AOM/DSS mouse model (144). PGE2 also recruits more MDSCs to the tumor site. Non steroidal anti-inflammatory drugs (NSAIDs), which specifically inhibit the inducible isoform of COX-2, are used as a general therapy to reduce inflammation and cancer. Growing evidence shows that COX-2 selective inhibitors including CG100649 and celecoxib are likely to be used in treatment with other therapies (145–147).
In addition to the above therapies, several clinical trials have been conducted on targeting inhibitory T cell pathways to unleash antitumor immune responses. CTLA-4 (cytotoxic T lymphocyte–associated antigen 4), one of the inhibitory molecules of T cells, binds with B7 on antigen presenting cells (APCs) which inhibits T cell activation and suppresses the antitumor immunity. Anti-CTLA-4 antibodies are extensively studied and approved for the treatment of melanoma. Clinical trials are ongoing to determine the efficacy of anti-CTLA-4 antibodies against colon and other cancers (148, 149). In addition to CTLA4, PD-1 (programmed cell death protein 1) is another T cell inhibitory molecule, which is present in activated T cells. PD-1 ligands (PD-L1 and PD-L2) are present in APCs and tumor cells. Clinical trials on antibodies against PD-1, PD-1 L1, and PD-1 positive T cells to treat various cancers including colon cancer are currently in progress (150).
Conclusion
Accumulated evidence on CAC has clearly shown the close contribution of several factors including diet, microbiota, secretory molecules, pro-/anti-inflammatory cytokines, transcription factors, growth factors, and other components, which are produced during the development of CAC. Since CAC development involves a complex network, different treatment strategies are continuously explored in this field. However, blocking one signaling-associated molecule will only partially ameliorate CAC development. Therefore, effective combined therapies should be tested in clinical trials. Furthermore, in depth studies are necessary to delineate the critical underlying mucosal and immune cell mediated mechanism involved in the transition from IBD to CAC to optimize the current therapeutic regime.
Acknowledgments
The authors are grateful to Dr. Daren Low (A*STAR Graduate Academy, Singapore) for carefully reading this review article with helpful discussions and advices. The authors would also like to thank Arianna DeGruttola for her secretarial assistance.
Sources of support: This work has been supported by National Institute of Health (R01-DK80070, DK91247, AI81807), and grants from the Broad Medical Foundation and American Gastroenterological Association Foundation to EM.
Abbreviations list
- AGE
advanced glycation end products
- AOM
azoxymethane
- BIR
baculovirus inhibitor of apoptosis protein repeat
- BM
bone marrow
- CAC
colitis-associated cancer
- CAF
cancer-associated fibroblasts
- CD
Crohn’s disease
- CHI3L1
chitinase 3-like 1
- CIN
chromosome instability
- COX-2
cyclooxygenase2
- CRC
colorectal cancer
- CTLA-4
cytotoxic T lymphocyte–associated antigen 4
- DC
dendritic cells
- DSS
dextran sulfate sodium
- ECM
extracellular matrix
- EGFR
epidermal growth factor receptor
- EMT
epithelial mesenchymal transition
- FAP
familial adenomatous polyposis
- FGF
fibroblast growth factor
- FAP
fibroblast activation protein
- GALT
gut-associated lymphoid tissue
- GIT
gastrointestinal tract
- GWAS
genome-wide association studies
- HDAC
histone deacetylase
- HGF
hepatocyte growth factor
- HMGB-1
DNA binding protein high mobility group box-1
- HNPCC
hereditary non-polyposis colorectal cancer
- MAP
MUTYH [mutY homolog (E. coli)]-associated polyposis
- IBD
inflammatory bowel diseases
- IRF4
interferon regulatory factors
- IECs
intestinal epithelial cells
- iNKT cells
invariant natural killer T cells
- ILCs
innate lymphoid cells
- MAMP
microbe-associated molecular patterns
- MDSCs
myeloid-derived suppressor cells
- MSI
microsattelite instability
- MSC
mesenchymal stem cells
- MLCK
myosin light chain kinase
- MyD88
myeloid differentiation factor 88
- MFs
myofibroblasts
- NAIP
NLR family apoptosis inhibitor proteins
- NLR
nucleotide–binding domain and leucine-rich repeats
- NSAIDs
nonsteroidal anti-inflammatory drugs
- PD-1
programmed cell death protein-1
- PGE2
prostaglandin E2
- PPARγ
peroxisome proliferator activated receptor-γ
- RAGE
receptor for advance glycation end product
- ROR γ
retinoic acid receptor- related orphan receptor γ
- ROS
reactive oxygen species
- RON
reactive nitrogen species
- SFRP
secreted frizzled-related protein
- SIGRR
single immunoglobulin IL-1R related molecule
- SNP
single nucleotide polymorphisms
- TAM
tumor-associated macrophages
- TME
tumor microenvironment
- TIR
Toll-IL-1 receptor
- TIRRAP
TIR domain containing adaptor
- TLR
toll-like receptors
- TOLLIP
toll-interacting protein
- Tpl2
tumor progression locus 2
- TIL
tumor-initiating cells
- TNBS
trinitrobenzene sulfonic acid
- UC
ulcerative colitis
- VEGF
vascular endothelial growth factor
- UDCA
ursodeoxycholic acid
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
References
- 1.Crohn BRH. The sigmoidoscopic picture of chronic ulcerative colitis (non -specific) Am J Med Sci. 1925:170. [Google Scholar]
- 2.Shanahan F, Bernstein CN. The evolving epidemiology of inflammatory bowel disease. Current opinion in gastroenterology. 2009 Jul;25(4):301–305. doi: 10.1097/MOG.0b013e32832b12ef. [DOI] [PubMed] [Google Scholar]
- 3.Economou M, Pappas G. New global map of Crohn's disease: Genetic, environmental, and socioeconomic correlations. Inflamm Bowel Dis. 2008 May;14(5):709–720. doi: 10.1002/ibd.20352. [DOI] [PubMed] [Google Scholar]
- 4.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001 Apr;48(4):526–535. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalili H, Gong J, Brenner H, Austin TR, Hutter CM, Baba Y, et al. Identification of a common variant with potential pleiotropic effect on risk of inflammatory bowel disease and colorectal cancer. Carcinogenesis. 2015 Sep;36(9):999–1007. doi: 10.1093/carcin/bgv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulmann K, Mori Y, Croog V, Yin J, Olaru A, Sterian A, et al. Molecular phenotype of inflammatory bowel disease-associated neoplasms with microsatellite instability. Gastroenterology. 2005 Jul;129(1):74–85. doi: 10.1053/j.gastro.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 2015 Jan;150(1):17–22. doi: 10.1001/jamasurg.2014.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dyson JK, Rutter MD. Colorectal cancer in inflammatory bowel disease: what is the real magnitude of the risk? World J Gastroenterol. 2012 Aug 7;18(29):3839–3848. doi: 10.3748/wjg.v18.i29.3839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhodes JM, Campbell BJ. Inflammation and colorectal cancer: IBD-associated and sporadic cancer compared. Trends in molecular medicine. 2002 Jan;8(1):10–16. doi: 10.1016/s1471-4914(01)02194-3. [DOI] [PubMed] [Google Scholar]
- 10.Tahara T, Inoue N, Hisamatsu T, Kashiwagi K, Takaishi H, Kanai T, et al. Clinical significance of microsatellite instability in the inflamed mucosa for the prediction of colonic neoplasms in patients with ulcerative colitis. Journal of gastroenterology and hepatology. 2005 May;20(5):710–715. doi: 10.1111/j.1440-1746.2005.03803.x. [DOI] [PubMed] [Google Scholar]
- 11.Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009 Jul;30(7):1073–1081. doi: 10.1093/carcin/bgp127. [DOI] [PubMed] [Google Scholar]
- 12.Grady WM, Carethers JM. Genomic and epigenetic instability in colorectal cancer pathogenesis. Gastroenterology. 2008 Oct;135(4):1079–1099. doi: 10.1053/j.gastro.2008.07.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perucho M. Tumors with microsatellite instability: many mutations, targets and paradoxes. Oncogene. 2003 Apr 17;22(15):2223–2225. doi: 10.1038/sj.onc.1206580. [DOI] [PubMed] [Google Scholar]
- 14.Korinek V, Barker N, Morin PJ, van Wichen D, de Weger R, Kinzler KW, et al. Constitutive transcriptional activation by a beta-catenin-Tcf complex in APC−/− colon carcinoma. Science. 1997 Mar 21;275(5307):1784–1787. doi: 10.1126/science.275.5307.1784. [DOI] [PubMed] [Google Scholar]
- 15.Morin PJ, Sparks AB, Korinek V, Barker N, Clevers H, Vogelstein B, et al. Activation of beta-catenin-Tcf signaling in colon cancer by mutations in beta-catenin or APC. Science. 1997 Mar 21;275(5307):1787–1790. doi: 10.1126/science.275.5307.1787. [DOI] [PubMed] [Google Scholar]
- 16.Bienz M, Clevers H. Linking colorectal cancer to Wnt signaling. Cell. 2000 Oct 13;103(2):311–320. doi: 10.1016/s0092-8674(00)00122-7. [DOI] [PubMed] [Google Scholar]
- 17.de Cuba EM, Snaebjornsson P, Heideman DA, van Grieken NC, Bosch LJ, Fijneman RJ, et al. Prognostic value of BRAF and KRAS mutation status in stage II and III microsatellite instable colon cancers. Int J Cancer. 2015 Sep 16; doi: 10.1002/ijc.29855. [DOI] [PubMed] [Google Scholar]
- 18.Xie J, Itzkowitz SH. Cancer in inflammatory bowel disease. World J Gastroenterol. 2008 Jan 21;14(3):378–389. doi: 10.3748/wjg.14.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castellone MD, Teramoto H, Williams BO, Druey KM, Gutkind JS. Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-beta-catenin signaling axis. Science. 2005 Dec 2;310(5753):1504–1510. doi: 10.1126/science.1116221. [DOI] [PubMed] [Google Scholar]
- 20.Kaler P, Augenlicht L, Klampfer L. Macrophage-derived IL-1beta stimulates Wnt signaling and growth of colon cancer cells: a crosstalk interrupted by vitamin D3. Oncogene. 2009 Nov 5;28(44):3892–3902. doi: 10.1038/onc.2009.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaler P, Godasi BN, Augenlicht L, Klampfer L. The NF-kappaB/AKT-dependent Induction of Wnt Signaling in Colon Cancer Cells by Macrophages and IL-1beta. Cancer Microenviron. 2009 Dec;2(1):69–80. doi: 10.1007/s12307-009-0030-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Low D, Mino-Kenudson M, Mizoguchi E. Recent advancement in understanding colitis-associated tumorigenesis. Inflamm Bowel Dis. 2014 Nov;20(11):2115–2123. doi: 10.1097/MIB.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010 Jun;138(6):2101 e5–2114 e5. doi: 10.1053/j.gastro.2010.01.058. [DOI] [PubMed] [Google Scholar]
- 24.Nistal E, Fernandez-Fernandez N, Vivas S, Olcoz JL. Factors Determining Colorectal Cancer: The Role of the Intestinal Microbiota. Front Oncol. 2015;5:220. doi: 10.3389/fonc.2015.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tjalsma H, Boleij A, Marchesi JR, Dutilh BE. A bacterial driver-passenger model for colorectal cancer: beyond the usual suspects. Nat Rev Microbiol. 2012 Aug;10(8):575–582. doi: 10.1038/nrmicro2819. [DOI] [PubMed] [Google Scholar]
- 26.Kostic AD, Gevers D, Pedamallu CS, Michaud M, Duke F, Earl AM, et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res. 2012 Feb;22(2):292–298. doi: 10.1101/gr.126573.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanapareddy N, Legge RM, Jovov B, McCoy A, Burcal L, Araujo-Perez F, et al. Increased rectal microbial richness is associated with the presence of colorectal adenomas in humans. ISME J. 2012 Oct;6(10):1858–1868. doi: 10.1038/ismej.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duncan SH, Louis P, Flint HJ. Cultivable bacterial diversity from the human colon. Lett Appl Microbiol. 2007 Apr;44(4):343–350. doi: 10.1111/j.1472-765X.2007.02129.x. [DOI] [PubMed] [Google Scholar]
- 29.Neufert C, Pickert G, Zheng Y, Wittkopf N, Warntjen M, Nikolaev A, et al. Activation of epithelial STAT3 regulates intestinal homeostasis. Cell Cycle. 2010 Feb 15;9(4):652–655. doi: 10.4161/cc.9.4.10615. [DOI] [PubMed] [Google Scholar]
- 30.Bromberg J, Wang TC. Inflammation and cancer: IL-6 and STAT3 complete the link. Cancer Cell. 2009 Feb 3;15(2):79–80. doi: 10.1016/j.ccr.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009 Feb 3;15(2):103–113. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abreu MT. Toll-like receptor signalling in the intestinal epithelium: how bacterial recognition shapes intestinal function. Nat Rev Immunol. 2010 Feb;10(2):131–144. doi: 10.1038/nri2707. [DOI] [PubMed] [Google Scholar]
- 33.Basith S, Manavalan B, Yoo TH, Kim SG, Choi S. Roles of toll-like receptors in cancer: a double-edged sword for defense and offense. Arch Pharm Res. 2012 Aug;35(8):1297–1316. doi: 10.1007/s12272-012-0802-7. [DOI] [PubMed] [Google Scholar]
- 34.Huang HY, Zhang ZJ, Cao CB, Wang N, Liu FF, Peng JQ, et al. The TLR4/NF-kappaB signaling pathway mediates the growth of colon cancer. Eur Rev Med Pharmacol Sci. 2014;18(24):3834–3843. [PubMed] [Google Scholar]
- 35.Fukata M, Hernandez Y, Conduah D, Cohen J, Chen A, Breglio K, et al. Innate immune signaling by Toll-like receptor-4 (TLR4) shapes the inflammatory microenvironment in colitis-associated tumors. Inflamm Bowel Dis. 2009 Jul;15(7):997–1006. doi: 10.1002/ibd.20880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanneganti M, Mino-Kenudson M, Mizoguchi E. Animal models of colitis-associated carcinogenesis. Journal of biomedicine & biotechnology. 2011;2011:342637. doi: 10.1155/2011/342637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fukata M, Chen A, Vamadevan AS, Cohen J, Breglio K, Krishnareddy S, et al. Toll-like receptor-4 promotes the development of colitis-associated colorectal tumors. Gastroenterology. 2007 Dec;133(6):1869–1881. doi: 10.1053/j.gastro.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee CC, Avalos AM, Ploegh HL. Accessory molecules for Toll-like receptors and their function. Nat Rev Immunol. 2012 Mar;12(3):168–179. doi: 10.1038/nri3151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rakoff-Nahoum S, Medzhitov R. Regulation of spontaneous intestinal tumorigenesis through the adaptor protein MyD88. Science. 2007 Jul 6;317(5834):124–127. doi: 10.1126/science.1140488. [DOI] [PubMed] [Google Scholar]
- 40.Salcedo R, Cataisson C, Hasan U, Yuspa SH, Trinchieri G. MyD88 and its divergent toll in carcinogenesis. Trends Immunol. 2013 Aug;34(8):379–389. doi: 10.1016/j.it.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Araki A, Kanai T, Ishikura T, Makita S, Uraushihara K, Iiyama R, et al. MyD88-deficient mice develop severe intestinal inflammation in dextran sodium sulfate colitis. J Gastroenterol. 2005 Jan;40(1):16–23. doi: 10.1007/s00535-004-1492-9. [DOI] [PubMed] [Google Scholar]
- 42.Aviello G, Corr SC, Johnston DG, O'Neill LA, Fallon PG. MyD88 adaptor-like (Mal) regulates intestinal homeostasis and colitis-associated colorectal cancer in mice. Am J Physiol Gastrointest Liver Physiol. 2014 May 1;306(9):G769–G778. doi: 10.1152/ajpgi.00399.2013. [DOI] [PubMed] [Google Scholar]
- 43.Sipos F, Furi I, Constantinovits M, Tulassay Z, Muzes G. Contribution of TLR signaling to the pathogenesis of colitis-associated cancer in inflammatory bowel disease. World J Gastroenterol. 2014 Sep 28;20(36):12713–12721. doi: 10.3748/wjg.v20.i36.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Allen IC. Non-Inflammasome Forming NLRs in Inflammation and Tumorigenesis. Front Immunol. 2014;5:169. doi: 10.3389/fimmu.2014.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allen IC, TeKippe EM, Woodford RM, Uronis JM, Holl EK, Rogers AB, et al. The NLRP3 inflammasome functions as a negative regulator of tumorigenesis during colitis-associated cancer. J Exp Med. 2010 May 10;207(5):1045–1056. doi: 10.1084/jem.20100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hu B, Elinav E, Huber S, Booth CJ, Strowig T, Jin C, et al. Inflammation-induced tumorigenesis in the colon is regulated by caspase-1 and NLRC4. Proc Natl Acad Sci U S A. 2010 Dec 14;107(50):21635–21640. doi: 10.1073/pnas.1016814108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Williams TM, Leeth RA, Rothschild DE, Coutermarsh-Ott SL, McDaniel DK, Simmons AE, et al. The NLRP1 inflammasome attenuates colitis and colitis-associated tumorigenesis. J Immunol. 2015 Apr 1;194(7):3369–3380. doi: 10.4049/jimmunol.1402098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Siegmund B. Interleukin-18 in intestinal inflammation: friend and foe? Immunity. 2010 Mar 26;32(3):300–302. doi: 10.1016/j.immuni.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 49.Zaki MH, Boyd KL, Vogel P, Kastan MB, Lamkanfi M, Kanneganti TD. The NLRP3 inflammasome protects against loss of epithelial integrity and mortality during experimental colitis. Immunity. 2010 Mar 26;32(3):379–391. doi: 10.1016/j.immuni.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zaki MH, Vogel P, Body-Malapel M, Lamkanfi M, Kanneganti TD. IL-18 production downstream of the Nlrp3 inflammasome confers protection against colorectal tumor formation. J Immunol. 2010 Oct 15;185(8):4912–4920. doi: 10.4049/jimmunol.1002046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Villani AC, Lemire M, Fortin G, Louis E, Silverberg MS, Collette C, et al. Common variants in the NLRP3 region contribute to Crohn's disease susceptibility. Nat Genet. 2009 Jan;41(1):71–76. doi: 10.1038/ng285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zaki MH, Vogel P, Malireddi RK, Body-Malapel M, Anand PK, Bertin J, et al. The NOD-like receptor NLRP12 attenuates colon inflammation and tumorigenesis. Cancer Cell. 2011 Nov 15;20(5):649–660. doi: 10.1016/j.ccr.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Allam R, Maillard MH, Tardivel A, Chennupati V, Bega H, Yu CW, et al. Epithelial NAIPs protect against colonic tumorigenesis. J Exp Med. 2015 Mar 9;212(3):369–383. doi: 10.1084/jem.20140474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Endo T, Abe S, Seidlar HB, Nagaoka S, Takemura T, Utsuyama M, et al. Expression of IAP family proteins in colon cancers from patients with different age groups. Cancer Immunol Immunother. 2004 Sep;53(9):770–776. doi: 10.1007/s00262-004-0534-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Low D, Tran HT, Lee IA, Dreux N, Kamba A, Reinecker HC, et al. Chitin-binding domains of Escherichia coli ChiA mediate interactions with intestinal epithelial cells in mice with colitis. Gastroenterology. 2013 Sep;145(3):602 e9–612 e9. doi: 10.1053/j.gastro.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen CC, Llado V, Eurich K, Tran HT, Mizoguchi E. Carbohydrate-binding motif in chitinase 3-like 1 (CHI3L1/YKL-40) specifically activates Akt signaling pathway in colonic epithelial cells. Clin Immunol. 2011 Sep;140(3):268–275. doi: 10.1016/j.clim.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mizoguchi E. Chitinase 3-like-1 exacerbates intestinal inflammation by enhancing bacterial adhesion and invasion in colonic epithelial cells. Gastroenterology. 2006 Feb;130(2):398–411. doi: 10.1053/j.gastro.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 58.Kawada M, Seno H, Kanda K, Nakanishi Y, Akitake R, Komekado H, et al. Chitinase 3-like 1 promotes macrophage recruitment and angiogenesis in colorectal cancer. Oncogene. 2012 Jun 28;31(26):3111–3123. doi: 10.1038/onc.2011.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen CC, Pekow J, Llado V, Kanneganti M, Lau CW, Mizoguchi A, et al. Chitinase 3-like-1 expression in colonic epithelial cells as a potentially novel marker for colitis-associated neoplasia. The American journal of pathology. 2011 Sep;179(3):1494–1503. doi: 10.1016/j.ajpath.2011.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eurich K, Segawa M, Toei-Shimizu S, Mizoguchi E. Potential role of chitinase 3-like-1 in inflammation-associated carcinogenic changes of epithelial cells. World J Gastroenterol. 2009 Nov 14;15(42):5249–5259. doi: 10.3748/wjg.15.5249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Low D, DeGruttola AK, Poltrak A, Mizoguchi A, Mino-Kenudson M, Mizoguchi E. High Endogenous Expression of Chitinase 3-Like 1 and Excessive Epithelial Proliferation with Colonic Tumor Formation in MOLF/EiJ Mice. PLoS One. 2015;10(10):e0139149. doi: 10.1371/journal.pone.0139149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tran HT, Lee IA, Low D, Kamba A, Mizoguchi A, Shi HN, et al. Chitinase 3-like 1 synergistically activates IL6-mediated STAT3 phosphorylation in intestinal epithelial cells in murine models of infectious colitis. Inflamm Bowel Dis. 2014 May;20(5):835–846. doi: 10.1097/MIB.0000000000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Low D, Subramaniam R, Lin L, Aomatsu T, Mizoguchi A, Ng A, et al. Chitinase 3-like 1 induces survival and proliferation of intestinal epithelial cells during chronic inflammation and colitis-associated cancer by regulating S100A9. Oncotarget. 2015 Sep 28; doi: 10.18632/oncotarget.5440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chuah YK, Basir R, Talib H, Tie TH, Nordin N. Receptor for advanced glycation end products and its involvement in inflammatory diseases. Int J Inflam. 2013;2013:403460. doi: 10.1155/2013/403460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zen K, Chen CX, Chen YT, Wilton R, Liu Y. Receptor for advanced glycation endproducts mediates neutrophil migration across intestinal epithelium. J Immunol. 2007 Feb 15;178(4):2483–2490. doi: 10.4049/jimmunol.178.4.2483. [DOI] [PubMed] [Google Scholar]
- 66.He CH, Lee CG, Dela Cruz CS, Lee CM, Zhou Y, Ahangari F, et al. Chitinase 3-like 1 regulates cellular and tissue responses via IL-13 receptor alpha2. Cell Rep. 2013 Aug 29;4(4):830–841. doi: 10.1016/j.celrep.2013.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Francescone R, Ngernyuang N, Yan W, Bentley B, Shao R. Tumor-derived mural-like cells coordinate with endothelial cells: role of YKL-40 in mural cell-mediated angiogenesis. Oncogene. 2014 Apr 17;33(16):2110–2122. doi: 10.1038/onc.2013.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shao R, Francescone R, Ngernyuang N, Bentley B, Taylor SL, Moral L, et al. Anti-YKL-40 antibody and ionizing irradiation synergistically inhibit tumor vascularization and malignancy in glioblastoma. Carcinogenesis. 2014 Feb;35(2):373–382. doi: 10.1093/carcin/bgt380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blair SA, Kane SV, Clayburgh DR, Turner JR. Epithelial myosin light chain kinase expression and activity are upregulated in inflammatory bowel disease. Lab Invest. 2006 Feb;86(2):191–201. doi: 10.1038/labinvest.3700373. [DOI] [PubMed] [Google Scholar]
- 70.Suzuki M, Nagaishi T, Yamazaki M, Onizawa M, Watabe T, Sakamaki Y, et al. Myosin light chain kinase expression induced via tumor necrosis factor receptor 2 signaling in the epithelial cells regulates the development of colitis-associated carcinogenesis. PLoS One. 2014;9(2):e88369. doi: 10.1371/journal.pone.0088369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Su L, Nalle SC, Shen L, Turner ES, Singh G, Breskin LA, et al. TNFR2 activates MLCK-dependent tight junction dysregulation to cause apoptosis-mediated barrier loss and experimental colitis. Gastroenterology. 2013 Aug;145(2):407–415. doi: 10.1053/j.gastro.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mizoguchi E, Mizoguchi A, Takedatsu H, Cario E, de Jong YP, Ooi CJ, et al. Role of tumor necrosis factor receptor 2 (TNFR2) in colonic epithelial hyperplasia and chronic intestinal inflammation in mice. Gastroenterology. 2002 Jan;122(1):134–144. doi: 10.1053/gast.2002.30347. [DOI] [PubMed] [Google Scholar]
- 73.Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ, et al. IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004 Aug 6;118(3):285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 74.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007 Jul 26;448(7152):427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 75.Waldner MJ, Neurath MF. Mechanisms of immune signaling in colitis associated cancer. CMGH. 2015;1:6–16. doi: 10.1016/j.jcmgh.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang W, Li X, Zheng D, Zhang D, Peng X, Zhang X, et al. Dynamic changes and functions of macrophages and M1/M2 subpopulations during ulcerative colitis-associated carcinogenesis in an AOM/DSS mouse model. Mol Med Rep. 2015 Apr;11(4):2397–2406. doi: 10.3892/mmr.2014.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ray AL, Castillo EF, Morris KT, Nofchissey RA, Weston LL, Samedi VG, et al. Blockade of MK2 is protective in inflammation-associated colorectal cancer development. Int J Cancer. 2015 Aug 3; doi: 10.1002/ijc.29716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sica A, Schioppa T, Mantovani A, Allavena P. Tumour-associated macrophages are a distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eur J Cancer. 2006 Apr;42(6):717–727. doi: 10.1016/j.ejca.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 79.Condeelis J, Pollard JW. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006 Jan 27;124(2):263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 80.Forssell J, Oberg A, Henriksson ML, Stenling R, Jung A, Palmqvist R. High macrophage infiltration along the tumor front correlates with improved survival in colon cancer. Clin Cancer Res. 2007 Mar 1;13(5):1472–1479. doi: 10.1158/1078-0432.CCR-06-2073. [DOI] [PubMed] [Google Scholar]
- 81.Ohno S, Inagawa H, Dhar DK, Fujii T, Ueda S, Tachibana M, et al. The degree of macrophage infiltration into the cancer cell nest is a significant predictor of survival in gastric cancer patients. Anticancer Res. 2003 Nov-Dec;23(6D):5015–5022. [PubMed] [Google Scholar]
- 82.Erreni M, Mantovani A, Allavena P. Tumor-associated Macrophages (TAM) and Inflammation in Colorectal Cancer. Cancer microenvironment : official journal of the International Cancer Microenvironment Society. 2011 Aug;4(2):141–154. doi: 10.1007/s12307-010-0052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fridlender ZG, Albelda SM. Tumor-associated neutrophils: friend or foe? Carcinogenesis. 2012 May;33(5):949–955. doi: 10.1093/carcin/bgs123. [DOI] [PubMed] [Google Scholar]
- 84.Formica V, Cereda V, Nardecchia A, Tesauro M, Roselli M. Immune reaction and colorectal cancer: friends or foes? World J Gastroenterol. 2014 Sep 21;20(35):12407–12419. doi: 10.3748/wjg.v20.i35.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005 Sep 1;91(3):181–184. doi: 10.1002/jso.20329. [DOI] [PubMed] [Google Scholar]
- 86.Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011 Apr 12;104(8):1288–1295. doi: 10.1038/bjc.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Garrity-Park M, Loftus EV, Jr, Sandborn WJ, Smyrk TC. Myeloperoxidase immunohistochemistry as a measure of disease activity in ulcerative colitis: association with ulcerative colitis-colorectal cancer, tumor necrosis factor polymorphism and RUNX3 methylation. Inflamm Bowel Dis. 2012 Feb;18(2):275–283. doi: 10.1002/ibd.21681. [DOI] [PubMed] [Google Scholar]
- 88.Shang K, Bai YP, Wang C, Wang Z, Gu HY, Du X, et al. Crucial involvement of tumor-associated neutrophils in the regulation of chronic colitis-associated carcinogenesis in mice. PLoS One. 2012;7(12):e51848. doi: 10.1371/journal.pone.0051848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Garrett WS, Punit S, Gallini CA, Michaud M, Zhang D, Sigrist KS, et al. Colitis-associated colorectal cancer driven by T-bet deficiency in dendritic cells. Cancer Cell. 2009 Sep 8;16(3):208–219. doi: 10.1016/j.ccr.2009.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Osawa E, Nakajima A, Fujisawa T, Kawamura YI, Toyama-Sorimachi N, Nakagama H, et al. Predominant T helper type 2-inflammatory responses promote murine colon cancers. Int J Cancer. 2006 May 1;118(9):2232–2236. doi: 10.1002/ijc.21639. [DOI] [PubMed] [Google Scholar]
- 91.Martin M, Kesselring RK, Saidou B, Brunner SM, Schiechl G, Mouris VF, et al. RORgammat(+) hematopoietic cells are necessary for tumor cell proliferation during colitis-associated tumorigenesis in mice. Eur J Immunol. 2015 Jun;45(6):1667–1679. doi: 10.1002/eji.201444915. [DOI] [PubMed] [Google Scholar]
- 92.Pages F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C, Fridman WH. Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene. 2010 Feb 25;29(8):1093–1102. doi: 10.1038/onc.2009.416. [DOI] [PubMed] [Google Scholar]
- 93.Danese S, Malesci A, Vetrano S. Colitis-associated cancer: the dark side of inflammatory bowel disease. Gut. 2011 Dec;60(12):1609–1610. doi: 10.1136/gutjnl-2011-300953. [DOI] [PubMed] [Google Scholar]
- 94.Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004 Aug;21(2):137–148. doi: 10.1016/j.immuni.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 95.Pastille E, Bardini K, Fleissner D, Adamczyk A, Frede A, Wadwa M, et al. Transient ablation of regulatory T cells improves antitumor immunity in colitis-associated colon cancer. Cancer Res. 2014 Aug 15;74(16):4258–4269. doi: 10.1158/0008-5472.CAN-13-3065. [DOI] [PubMed] [Google Scholar]
- 96.Yoshioka K, Ueno Y, Tanaka S, Nagai K, Onitake T, Hanaoka R, et al. Role of natural killer T cells in the mouse colitis-associated colon cancer model. Scandinavian journal of immunology. 2012 Jan;75(1):16–26. doi: 10.1111/j.1365-3083.2011.02607.x. [DOI] [PubMed] [Google Scholar]
- 97.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009 Mar;9(3):162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol. 2009 Apr 15;182(8):4499–4506. doi: 10.4049/jimmunol.0802740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chun E, Lavoie S, Michaud M, Gallini CA, Kim J, Soucy G, et al. CCL2 Promotes Colorectal Carcinogenesis by Enhancing Polymorphonuclear Myeloid-Derived Suppressor Cell Population and Function. Cell Rep. 2015 Jul 14;12(2):244–257. doi: 10.1016/j.celrep.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kirchberger S, Royston DJ, Boulard O, Thornton E, Franchini F, Szabady RL, et al. Innate lymphoid cells sustain colon cancer through production of interleukin-22 in a mouse model. The Journal of experimental medicine. 2013 May 6;210(5):917–931. doi: 10.1084/jem.20122308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sonnenberg GF, Artis D. Innate lymphoid cells in the initiation, regulation and resolution of inflammation. Nature medicine. 2015 Jul;21(7):698–708. doi: 10.1038/nm.3892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vermeulen L, De Sousa EMF, van der Heijden M, Cameron K, de Jong JH, Borovski T, et al. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010 May;12(5):468–476. doi: 10.1038/ncb2048. [DOI] [PubMed] [Google Scholar]
- 103.Hughes KR, Sablitzky F, Mahida YR. Expression profiling of Wnt family of genes in normal and inflammatory bowel disease primary human intestinal myofibroblasts and normal human colonic crypt epithelial cells. Inflamm Bowel Dis. 2011 Jan;17(1):213–220. doi: 10.1002/ibd.21353. [DOI] [PubMed] [Google Scholar]
- 104.Koliaraki V, Roulis M, Kollias G. Tpl2 regulates intestinal myofibroblast HGF release to suppress colitis-associated tumorigenesis. J Clin Invest. 2012 Nov;122(11):4231–4242. doi: 10.1172/JCI63917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sasaki S, Baba T, Shinagawa K, Matsushima K, Mukaida N. Crucial involvement of the CCL3-CCR5 axis-mediated fibroblast accumulation in colitis-associated carcinogenesis in mice. Int J Cancer. 2014 Sep 15;135(6):1297–1306. doi: 10.1002/ijc.28779. [DOI] [PubMed] [Google Scholar]
- 106.Yoo J, Rodriguez Perez CE, Nie W, Edwards RA, Sinnett-Smith J, Rozengurt E. TNF-alpha induces upregulation of EGFR expression and signaling in human colonic myofibroblasts. Am J Physiol Gastrointest Liver Physiol. 2012 Apr 15;302(8):G805–G814. doi: 10.1152/ajpgi.00522.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Yoo J, Rodriguez Perez CE, Nie W, Sinnett-Smith J, Rozengurt E. TNF-alpha and LPA promote synergistic expression of COX-2 in human colonic myofibroblasts: role of LPA-mediated transactivation of upregulated EGFR. BMC Gastroenterol. 2013;13:90. doi: 10.1186/1471-230X-13-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Neufert C, Becker C, Tureci O, Waldner MJ, Backert I, Floh K, et al. Tumor fibroblast-derived epiregulin promotes growth of colitis-associated neoplasms through ERK. J Clin Invest. 2013 Apr;123(4):1428–1443. doi: 10.1172/JCI63748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rabizadeh S, Rhee KJ, Wu S, Huso D, Gan CM, Golub JE, et al. Enterotoxigenic bacteroides fragilis: a potential instigator of colitis. Inflamm Bowel Dis. 2007 Dec;13(12):1475–1483. doi: 10.1002/ibd.20265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wu S, Rhee KJ, Albesiano E, Rabizadeh S, Wu X, Yen HR, et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat Med. 2009 Sep;15(9):1016–1022. doi: 10.1038/nm.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Peddareddigari VG, Wang D, Dubois RN. The tumor microenvironment in colorectal carcinogenesis. Cancer Microenviron. 2010;3(1):149–166. doi: 10.1007/s12307-010-0038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li F, Cao Y, Townsend CM, Jr, Ko TC. TGF-beta signaling in colon cancer cells. World J Surg. 2005 Mar;29(3):306–311. doi: 10.1007/s00268-004-7813-6. [DOI] [PubMed] [Google Scholar]
- 113.Wang S, Liu Z, Wang L, Zhang X. NF-kappaB signaling pathway, inflammation and colorectal cancer. Cell Mol Immunol. 2009 Oct;6(5):327–334. doi: 10.1038/cmi.2009.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Klampfer L. The role of signal transducers and activators of transcription in colon cancer. Front Biosci. 2008;13:2888–2899. doi: 10.2741/2893. [DOI] [PubMed] [Google Scholar]
- 115.Grivennikov SI. Inflammation and colorectal cancer: colitis-associated neoplasia. Semin Immunopathol. 2013 Mar;35(2):229–244. doi: 10.1007/s00281-012-0352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Waldner MJ, Wirtz S, Jefremow A, Warntjen M, Neufert C, Atreya R, et al. VEGF receptor signaling links inflammation and tumorigenesis in colitis-associated cancer. J Exp Med. 2010 Dec 20;207(13):2855–2868. doi: 10.1084/jem.20100438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Turpin B, Miller W, Rosenfeldt L, Kombrinck K, Flick MJ, Steinbrecher KA, et al. Thrombin drives tumorigenesis in colitis-associated colon cancer. Cancer Res. 2014 Jun 1;74(11):3020–3030. doi: 10.1158/0008-5472.CAN-13-3276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Henry LR, Lee HO, Lee JS, Klein-Szanto A, Watts P, Ross EA, et al. Clinical implications of fibroblast activation protein in patients with colon cancer. Clin Cancer Res. 2007 Mar 15;13(6):1736–1741. doi: 10.1158/1078-0432.CCR-06-1746. [DOI] [PubMed] [Google Scholar]
- 119.Eaden J, Abrams K, Ekbom A, Jackson E, Mayberry J. Colorectal cancer prevention in ulcerative colitis: a case-control study. Aliment Pharmacol Ther. 2000 Feb;14(2):145–153. doi: 10.1046/j.1365-2036.2000.00698.x. [DOI] [PubMed] [Google Scholar]
- 120.Velayos FS, Loftus EV, Jr, Jess T, Harmsen WS, Bida J, Zinsmeister AR, et al. Predictive and protective factors associated with colorectal cancer in ulcerative colitis: A case-control study. Gastroenterology. 2006 Jun;130(7):1941–1949. doi: 10.1053/j.gastro.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 121.Tung BY, Emond MJ, Haggitt RC, Bronner MP, Kimmey MB, Kowdley KV, et al. Ursodiol use is associated with lower prevalence of colonic neoplasia in patients with ulcerative colitis and primary sclerosing cholangitis. Ann Intern Med. 2001 Jan 16;134(2):89–95. doi: 10.7326/0003-4819-134-2-200101160-00008. [DOI] [PubMed] [Google Scholar]
- 122.Sjoqvist U, Tribukait B, Ost A, Einarsson C, Oxelmark L, Lofberg R. Ursodeoxycholic acid treatment in IBD-patients with colorectal dysplasia and/or DNA-aneuploidy: a prospective, double-blind, randomized controlled pilot study. Anticancer Res. 2004 Sep-Oct;24(5B):3121–3127. [PubMed] [Google Scholar]
- 123.Hansen JD, Kumar S, Lo WK, Poulsen DM, Halai UA, Tater KC. Ursodiol and colorectal cancer or dysplasia risk in primary sclerosing cholangitis and inflammatory bowel disease: a meta-analysis. Dig Dis Sci. 2013 Nov;58(11):3079–3087. doi: 10.1007/s10620-013-2772-0. [DOI] [PubMed] [Google Scholar]
- 124.Seraj MJ, Umemoto A, Kajikawa A, Mimura S, Kinouchi T, Ohnishi Y, et al. Effects of dietary bile acids on formation of azoxymethane-induced aberrant crypt foci in F344 rats. Cancer Lett. 1997 May 1;115(1):97–103. doi: 10.1016/s0304-3835(97)04719-8. [DOI] [PubMed] [Google Scholar]
- 125.Potack J, Itzkowitz SH. Colorectal cancer in inflammatory bowel disease. Gut and liver. 2008 Sep;2(2):61–73. doi: 10.5009/gnl.2008.2.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lashner BA, Heidenreich PA, Su GL, Kane SV, Hanauer SB. Effect of folate supplementation on the incidence of dysplasia and cancer in chronic ulcerative colitis. A case-control study. Gastroenterology. 1989 Aug;97(2):255–259. doi: 10.1016/0016-5085(89)90058-9. [DOI] [PubMed] [Google Scholar]
- 127.Lashner BA, Provencher KS, Seidner DL, Knesebeck A, Brzezinski A. The effect of folic acid supplementation on the risk for cancer or dysplasia in ulcerative colitis. Gastroenterology. 1997 Jan;112(1):29–32. doi: 10.1016/s0016-5085(97)70215-4. [DOI] [PubMed] [Google Scholar]
- 128.Poynter JN, Gruber SB, Higgins PD, Almog R, Bonner JD, Rennert HS, et al. Statins and the risk of colorectal cancer. The New England journal of medicine. 2005 May 26;352(21):2184–2192. doi: 10.1056/NEJMoa043792. [DOI] [PubMed] [Google Scholar]
- 129.Velayos FS, Terdiman JP, Walsh JM. Effect of 5-aminosalicylate use on colorectal cancer and dysplasia risk: a systematic review and metaanalysis of observational studies. Am J Gastroenterol. 2005 Jun;100(6):1345–1353. doi: 10.1111/j.1572-0241.2005.41442.x. [DOI] [PubMed] [Google Scholar]
- 130.Terdiman JP, Steinbuch M, Blumentals WA, Ullman TA, Rubin DT. 5-Aminosalicylic acid therapy and the risk of colorectal cancer among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2007 Apr;13(4):367–371. doi: 10.1002/ibd.20074. [DOI] [PubMed] [Google Scholar]
- 131.Viennois E, Xiao B, Ayyadurai S, Wang L, Wang PG, Zhang Q, et al. Micheliolide, a new sesquiterpene lactone that inhibits intestinal inflammation and colitis-associated cancer. Lab Invest. 2014 Sep;94(9):950–965. doi: 10.1038/labinvest.2014.89. [DOI] [PubMed] [Google Scholar]
- 132.Glauben R, Batra A, Stroh T, Erben U, Fedke I, Lehr HA, et al. Histone deacetylases: novel targets for prevention of colitis-associated cancer in mice. Gut. 2008 May;57(5):613–622. doi: 10.1136/gut.2007.134650. [DOI] [PubMed] [Google Scholar]
- 133.Glauben R, Sonnenberg E, Zeitz M, Siegmund B. HDAC inhibitors in models of inflammation-related tumorigenesis. Cancer letters. 2009 Aug 8;280(2):154–159. doi: 10.1016/j.canlet.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 134.Gianotti L, Morelli L, Galbiati F, Rocchetti S, Coppola S, Beneduce A, et al. A randomized double-blind trial on perioperative administration of probiotics in colorectal cancer patients. World J Gastroenterol. 2010 Jan 14;16(2):167–175. doi: 10.3748/wjg.v16.i2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ishikawa H, Akedo I, Otani T, Suzuki T, Nakamura T, Takeyama I, et al. Randomized trial of dietary fiber and Lactobacillus casei administration for prevention of colorectal tumors. Int J Cancer. 2005 Sep 20;116(5):762–767. doi: 10.1002/ijc.21115. [DOI] [PubMed] [Google Scholar]
- 136.Popivanova BK, Kitamura K, Wu Y, Kondo T, Kagaya T, Kaneko S, et al. Blocking TNF-alpha in mice reduces colorectal carcinogenesis associated with chronic colitis. J Clin Invest. 2008 Feb;118(2):560–570. doi: 10.1172/JCI32453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wang K, Kim MK, Di Caro G, Wong J, Shalapour S, Wan J, et al. Interleukin-17 receptor a signaling in transformed enterocytes promotes early colorectal tumorigenesis. Immunity. 2014 Dec 18;41(6):1052–1063. doi: 10.1016/j.immuni.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Qi H, Yang H, Xu G, Ren J, Hua W, Shi Y, et al. Therapeutic efficacy of IL-17A antibody injection in preventing the development of colitis associated carcinogenesis in mice. Immunobiology. 2015 Jan;220(1):54–59. doi: 10.1016/j.imbio.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 139.Dennis KL, Saadalla A, Blatner NR, Wang S, Venkateswaran V, Gounari F, et al. T-cell Expression of IL10 Is Essential for Tumor Immune Surveillance in the Small Intestine. Cancer Immunol Res. 2015 Jul;3(7):806–814. doi: 10.1158/2326-6066.CIR-14-0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sturlan S, Oberhuber G, Beinhauer BG, Tichy B, Kappel S, Wang J, et al. Interleukin-10-deficient mice and inflammatory bowel disease associated cancer development. Carcinogenesis. 2001 Apr;22(4):665–671. doi: 10.1093/carcin/22.4.665. [DOI] [PubMed] [Google Scholar]
- 141.Bahri R, Pateras IS, D'Orlando O, Goyeneche-Patino DA, Campbell M, Polansky JK, et al. IL-15 suppresses colitis-associated colon carcinogenesis by inducing antitumor immunity. Oncoimmunology. 2015 Sep;4(9):e1002721. doi: 10.1080/2162402X.2014.1002721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wang D, DuBois RN. PPARdelta and PGE signaling pathways communicate and connect inflammation to colorectal cancer. Inflamm Cell Signal. 2014 Oct 19;1(6) doi: 10.14800/ics.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Wang D, Fu L, Ning W, Guo L, Sun X, Dey SK, et al. Peroxisome proliferator-activated receptor delta promotes colonic inflammation and tumor growth. Proc Natl Acad Sci U S A. 2014 May 13;111(19):7084–7089. doi: 10.1073/pnas.1324233111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ishikawa TO, Herschman HR. Tumor formation in a mouse model of colitis-associated colon cancer does not require COX-1 or COX-2 expression. Carcinogenesis. 2010 Apr;31(4):729–736. doi: 10.1093/carcin/bgq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kim SH, Margalit O, Katoh H, Wang D, Wu H, Xia D, et al. CG100649, a novel COX-2 inhibitor, inhibits colorectal adenoma and carcinoma growth in mouse models. Invest New Drugs. 2014 Dec;32(6):1105–1112. doi: 10.1007/s10637-014-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Setia S, Nehru B, Sanyal SN. The PI3K/Akt pathway in colitis associated colon cancer and its chemoprevention with celecoxib, a Cox-2 selective inhibitor. Biomed Pharmacother. 2014 Jul;68(6):721–727. doi: 10.1016/j.biopha.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 147.Setia S, Nehru B, Sanyal SN. Celecoxib prevents colitis associated colon carcinogenesis: an upregulation of apoptosis. Pharmacol Rep. 2014 Dec;66(6):1083–1091. doi: 10.1016/j.pharep.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 148.Hoos A, Ibrahim R, Korman A, Abdallah K, Berman D, Shahabi V, et al. Development of ipilimumab: contribution to a new paradigm for cancer immunotherapy. Semin Oncol. 2010 Oct;37(5):533–546. doi: 10.1053/j.seminoncol.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 149.Callahan MK, Wolchok JD, Allison JP. Anti-CTLA-4 antibody therapy: immune monitoring during clinical development of a novel immunotherapy. Semin Oncol. 2010 Oct;37(5):473–484. doi: 10.1053/j.seminoncol.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Postow MA, Callahan MK, Wolchok JD. Immune Checkpoint Blockade in Cancer Therapy. J Clin Oncol. 2015 Jun 10;33(17):1974–1982. doi: 10.1200/JCO.2014.59.4358. [DOI] [PMC free article] [PubMed] [Google Scholar]