Abstract
Purpose
The Oral Health Impact Profile (OHIP) is currently the most widely used oral health-related quality of life (OHRQoL) instrument. The study validated the English-language 5-item OHIP by investigating its psychometric properties of dimensionality, reliability, and validity in the adult general population.
Methods
In 405 subjects (mean age 45+15.7 years, 63% female) from the 2014 Minnesota State Fair, dimensionality was investigated by confirmatory factor analysis. Construct validity was assessed by using a structural equation model correlating OHRQoL and self-reported global oral health status. Reliability was calculated using Cronbach’s alpha for OHIP5 total scores.
Results
In the confirmatory factor analysis, the unidimensional model fit OHIP5 well as indicated by fit indices (RMSEA: 0.07, SRMR: 0.03, comparative fit indices: >0.95.) In the structural equation model, self–reported global oral health status correlated with 0.46 with the latent OHRQoL factor, indicating sufficient construct validity. Cronbach’s alpha, a measure of score reliability, was “satisfactory” with 0.75.
Conclusion
We validated the English-language version of OHIP5 in the adult general population. Ultrashort instruments such as the 5-item OHIP provide a conceptually appealing and technically feasible opportunity to measure the impact of oral disorders and dental interventions in settings such as general dental practice where the burden to collect and interpret OHRQoL information needs to be minimized.
Keywords: Oral health related quality of life, oral health impact profile, validity, reliability, dimensionality
1. Introduction
Oral health-related quality of life (OHRQoL) is an internationally widely used [1–3] and psychometrically sound [4–6] concept to assess how patients are affected by oral disorders and how they experience the effect of oral interventions. The Oral Health Impact Profile, OHIP is the most widely used OHRQoL instrument. Starting with 49 questions[7], soon an abbreviated version with 14 items was developed[8]. Realizing that some settings, e.g., national health surveys and dental practice, may need even shorter instruments, a 5-item version was created as the shortest OHIP[9]. While OHIP5 reduces the number of items to 10% of those of the original instrument, it intends to capture 90% of the instrument’s summary score information [9], making it an attractive tool for efficient OHRQoL measurement.
While OHIP5 was used in international patients and general population subjects, e.g., in Japanese prosthodontic patients[2], Dutch TMD patients[10] or Swedish general population subjects[11], this instrument has not been thoroughly investigated in an English-speaking population. However, it is known that the psychometric properties, e.g., the validity and the reliability, of the scores depend on the population where the instrument is being used. Therefore, an investigation of these psychometric properties in the general population is necessary before a broader use of OHIP5 in English-speaking subjects can be recommended.
Therefore, the aim of the study was to validate the English-language OHIP5 scores in the adult general population by investigating their dimensionality, reliability, and validity.
2. Method of Research
2.1. Study design and subjects
This report stems from a larger study conducted to explore oral health related quality of life, oral health literacy, and acceptance of treatment care by dental therapists in relationship to clinical oral health markers. Data was collected from 405 adult attendees of the 2014 Minnesota State Fair. The University of Minnesota launched a dedicated research facility, called the “Driven to Discover” (D2D) building, on the State Fair ground in 2014. Our study was conducted on 6 days of the 12-day fair. Participants entered the research facility as they would any other state fair building, and self-selected to participate in any of several available studies. The purpose of the research was provided to interested participants verbally, consented to participate orally, and were given a written information sheet reiterating the study purpose along with researcher and Institutional Review Board contact information. Those eligible for the study were adults aged 18 and older who spoke English well enough to correctly read a sample paragraph aloud and were not physically or mentally impaired. The annual Minnesota State Fair is among the largest state fairs in the United States with over 1,824,000 attendees in 2014. Given the number of attendees relative to the size of the state (approximately 5,300,000 in 2010), it is likely that 20% or more of Minnesota residents attend the fair. Based on the MN State Fair Demographic Outline & Visitor Profile information, 48.7% of the attendees were female, 37.7% were college graduates, and most of the attendees were between 45 to 54 years old. Also, of the attendees participating in D2D studies 84.4% were White, 7.09% were Black, 2.7% were Asian, less than 1 % were American Indian/Alaskan Native or Hawaiian/Pacific Islander, and 4.1% reported their race as “other”.[12]
The University of Minnesota Institutional Review Board approved the study.
2.2. Oral health-related quality of life assessment
The OHIP49 contains 49 questions that were designed to capture seven conceptually formulated dimensions which are Functional Limitation, Physical Pain, Psychological Discomfort, Physical Disability, Psychological Disability, Social Disability and Handicap based on Locker’s theoretical model of oral health[13]. These dimensions were later revised in the Dimensions of OHRQoL Project[14]. Here, Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impact were identified as four correlated aspects of patient-perceived OHRQoL by exploratory[15] and confirmatory factor analyses[16]. Several studies have demonstrated that this instrument has good psychometric properties in clinical as well as population-based studies[17–19] with a “reasonable degree of cross-cultural consistency”[20]. Later, OHIP5 was developed as an ultra- short version of the OHIP. The instrument was created with the aim to contain about 90% of the information of the long OHIP summary score [9]. The instrument has excellent content validity because it has at least one indicator for each OHRQoL dimension and therefore it captures the concept well with a minimum burden.[15,16]
OHIP5 instrument
For each OHIP question, subjects were asked how frequently they had experienced the problem in the last month. Responses were made on a scale 0-never, 1-hardly ever, 2-occasionally, 3-fairly often, and 4-very often. The OHIP5 questions were presented in the state fair survey as follows:
Have you had difficulty chewing any foods because of problems with your teeth, mouth, dentures or jaw?
Have you had painful aching in your mouth?
Have you felt uncomfortable about the appearance of your teeth, mouth dentures or jaws?
Have you felt that there has been less flavor in your food because of problems with your teeth, mouth, dentures or jaws?
Have you had difficulty doing your usual jobs because of problems with your teeth, mouth, dentures or jaws?
2.3. Data Analysis
2.3.1. Dimensionality
The four dimensions of patient-perceived OHRQoL identified by the Dimensions of OHRQoL Project (e.g., Oral Function, Orofacial Pain, Orofacial Appearance and Psychosocial Impact) could serve as a framework to understand and measure the impact of oral conditions and the effect of dental interventions. However, because of substantial correlations between these factors and the small number of indicators for some dimensions, one OHIP summary score can also sufficiently characterize OHRQoL. Based on these findings, we expect that OHIP5 scores should be unidimensional.
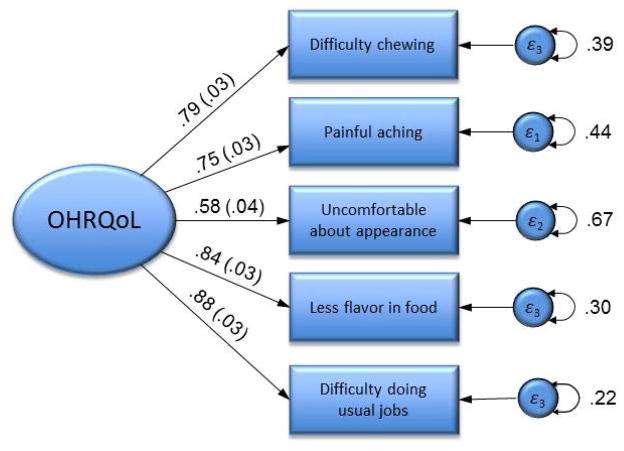
In the unidimensional model, all OHIP items are substantially correlated and “load” on a common (general) factor, representing OHRQoL (Figure 1). To evaluate model fit, we used a set of indices and included the log-likelihood chi-square test, the standardized root mean square residual (SRMR), the root mean square error of approximation (RMSEA), the comparative fit index (CFI) and the Tucker–Lewis index (TLI). Commonly applied guidelines for adequate model fit suggest the following values [21]: SRMR: ≤0.08; RMSEA: ≤0.06; and CFI, TLI: ≥0.95. Responses to the OHIP occur on a 5-point Likert scale and are positively skewed in the data. Thus, the model was estimated using diagonally weighted least squares (DWLS[22]) estimation. This estimation procedure minimizes the squared distance between the observed polychoric correlations and the estimated correlations, weighted by the inverse variances and covariances of the estimated polychoric correlations. As commonly done in CFA, the latent factor was constrained to have a mean of 0 and a variance of 1 for model identification purposes.
Figure 1. Confirmatory factor analysis model of oral health-related quality of life (OHRQoL) measured with five indicators from OHIP5.
The oval represents the latent factor OHRQoL, and the rectangles represent measured indicators for the latent factor with their error variances (circles). The lines connecting the latent factor to indicators are factor loadings (with their standard errors). Numbers provided are standardized values. Analyses were performed with R and used a diagonally weighted least squares estimation, assuming OHIP items were ordered categorically.
2.3.2. Validity
We investigated different aspects of validity. To determine convergent validity, i.e., OHIP5 scores as a measure of OHRQoL should correlate substantially with a similar measure, in our case, a global self-assessment of subject’s oral health. Using a structural equation model (SEM), we determined the correlation between the latent variable OHRQoL measured by the OHIP5 items and the self-reported global oral health status assessed with a five-grade scale (‘poor’, ‘fair’, ‘good’, ‘very good’ and ‘excellent’). Furthermore, we assessed known-groups validity through examining the association between OHIP5 summary scores and groups of patients known to differ in their OHRQoL. Based on clinical expertise and previous studies,[23–25] patients with dentures are expected to have a lower OHRQoL than patients without dentures. Related to denture status is the number of teeth which was also shown to be related to OHRQoL.[26] Subjects with fewer teeth are expected to have lower OHRQoL than subjects with more teeth. According to a systematic review by Gotfredsen et al[27], a dentition consisting of 20 teeth would assure an acceptable level of oral function. Therefore, to assess known-groups validity, we categorized the number of teeth into two groups: equal or more than 20 teeth compared to less than 20 teeth. In addition, we also expected that patients with higher treatment urgency would have poorer OHRQoL, coinciding with higher OHIP scores. Treatment urgency was categorized using the State and Territorial Dental Directors Adult Basic Screening Survey definitions of “no obvious problem”, “early care” and “urgent care”. On the other hand, we did not expect a difference between “early (a preventive) treatment need” and “no obvious problem” because we hypothesized that this differentiation would not matter to patients in term of their perceived oral health. We computed the correlation between OHIP5 summary scores with patients’ global assessment of their oral health using a Spearman rank correlation coefficient. Furthermore, we calculated Cohen’s d, a standardized effect size for the degree of difference between groups, and its 95 % confidence interval (CI) for known-groups validity assessment.
2.3.3. Reliability
We determined internal consistency using Cronbach’s alpha[28] and item-rest correlations.
2.4. Missing data and statistical software
We considered four out of the five items as sufficient to characterize a subject’s OHRQoL level. Therefore, two subjects were excluded from the analysis because the number of missing OHIP items precluded the calculation of an informative summary score. If one item was missing, we imputed it using median imputation. For OHIP5 item no.2 (Painful aching), 2 subjects; item no. 3 (Uncomfortable about appearance), 3 subjects; item no. 4 (Less flavor in your food), 2 subjects; item no. 5 (Difficulty doing your usual jobs), 17 subjects were missing. Overall, 24 subjects were missing OHIP5 items information.
Except for the latent variable analyses, all computations were performed using the statistical software package STATA Release13.1[29], with the probability of a type I error set at the 0.05 level. CFA and SEM analyses were performed in R[30] using the lavaan package[31].
3. Results
3.1. Subject characteristics
The majority of our study participants were female (67%) and college graduates (Table 1). The mean age of participants was 45 years with a greater proportion of White participants (92%) as compared to other races. Approximately 40% of the participants reported their oral health as ‘good’.
Table 1.
Socio-demographic characteristics, self-reported oral health status, and OHIP5 item severity of study subjects.
| Socio-demographic characteristic | All Subjects (N=405) |
|---|---|
| N (%) or mean ± SD | |
| Age (Years)a | 44.9 ± 15.7 |
| Femaleb | 271 (67.1) |
| Racec | |
| Black or African American | 2 (0.5) |
| American Indian | 11 (2.8) |
| Asian | 3 (0.8) |
| White | 367 (92) |
| More than one race | 9 (2.2) |
| Unknown | 7 (1.8) |
| Ethnicityd | |
| Hispanic or Latino | 13 (3.4) |
| Not Hispanic or Latino | 361 (94) |
| Unknown / Not Reported | 10 (2.6) |
| Educatione | |
| Some high school | 9 (2.2) |
| High school graduate or GED | 25 (6.2) |
| Some college credit | 46 (11.4) |
| Trade/vocational/technical training | 33 (8.8) |
| College graduate | 145 (35.9) |
| Some postgraduate work | 32 (7.9) |
| Postgraduate degree | 114 (28.2) |
| Self-reported Global Oral Health Status | |
| Poor | 12 (3.0) |
| Fair | 55 (13.6) |
| Good | 164 (40.5) |
| Very good | 130 (32.1) |
| Excellent | 44 (10.9) |
| OHIP5 items [0 – never,4 – very often] | |
| Difficulty chewing | 0.6 ± 0.8 |
| Painful aching f | 0.7 ± 0.8 |
| Uncomfortable about appearance g | 0.9 ± 1.1 |
| Less flavor in your food h | 0.3 ± 0.6 |
| Difficulty doing your usual jobs i | 0.2 ± 0.5 |
Missing data for
26,
1,
6,
21,
1,
2,
3,
2 and
17 subjects
3.2. Dimensionality
The unidimensional model fit the data well. The chi-square test (χ2(5) = 0.07 p = 0.02) rejected the model, as we expected with our sample size. However, the RMSEA for the unidimensional model was 0.07, the SRMR was 0.03, and both comparative fit indices were greater than 0.95. All these ancillary fit statistics exceeded general recommendations for model fit, suggesting that the OHIP covariance structure can be well-modeled by a latent, one-factor model. Standardized parameter estimates indicated that all items were strong indicators of a general (OHRQoL) factor (median loading of 0.79) with loadings ranging from 0.58 to 0.88. All loadings had small standard errors (0.03 to 0.04), indicating sufficient precision of results. These findings supported the hypothesis that OHIP5 data are well-characterized by a unidimensional model and a summary score describes the construct well.
3.3. Validity
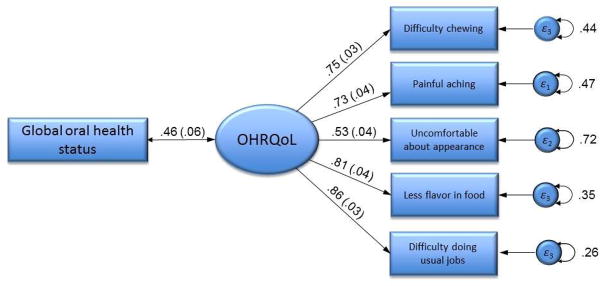
Structural equation modelling combined the OHIP5 items (difficulty chewing, painful aching, uncomfortable about appearance, less flavor in food and difficulty doing usual jobs) into a latent OHRQoL factor. The resulting correlation between global oral health status and this OHRQoL factor was 0.46 with a standard error of 0.06 (Figure 2). In the latent variable’s measurement model, all loadings were very high, precise (i.e., had low standard errors), and statistically significant, supporting the fit of the model. The substantial correlation of 0.46 was considered clinically relevant and was also statistically significant. The lower and the upper limits of the confidence interval indicated a sufficiently precise estimate.
Figure 2. Structural equation model for the association between global oral health status and oral health-related quality of life (OHRQoL).
The oval represents the latent factor OHRQoL, and the rectangles on the right represent measured indicators for the latent factor with their error variances (circles) or the measured exposure variable global oral health status. The lines connecting the latent factor to indicators are factor loadings (with their standard errors), and the line connecting the exposure variable global oral health status to the latent variable OHRQoL is the correlation between the two measures (with its standard error). Numbers provided are standardized values. Analyses were performed with R and used a diagonally weighted least squares estimation, assuming OHIP items were ordered categorical.
Further evidence for the OHIP5 scores’ construct validity came from associations between summary scores and the presence of dentures, number of natural teeth, and treatment urgency, (Table 2 and 3). A dose-response relationship between self-reported oral health status and OHIP5 scores was observed. Subjects with poor self-reported oral health had 5 times the OHIP5 score severity (i.e. worse OHRQOL) compared to subjects with excellent oral health status. The presence of a denture doubled OHRQoL impairment and furthermore, if individuals had less than 20 teeth, OHRQoL was even more impaired. The highest value of impairment was seen in the individual who was deemed to be in need to urgent dental care. Here, OHRQoL suffering was five times that of an average Minnesota State Fair attendee.
Table 2.
Convergent validity: Association between global oral health status and OHIP5 scores in 403 subjects with OHIP5 data.
| Variable | No | OHIP 5 mean ± sd | Correlation coefficient (95% CI) |
|---|---|---|---|
| Self-reported Global Oral Health Status | 403 | 0.30 (0.21 to 0.39) a & 0.46 (0.34 to 0.58)b | |
| Poor | 12 | 8.9 ± 3.9 | |
| Fair | 55 | 4.5 ± 3.2 | |
| Good | 163 | 2.4 ± 2.5 | |
| Very good | 129 | 2.2 ± 2.3 | |
| Excellent | 44 | 1.6 ± 1.8 |
Spearman correlation coefficient
correlation based on SEM model in Figure 2
Table 3.
Known-groups validity:
OHIP5 scores in subjects who differed in their denture status, number of natural teeth present and treatment urgency in 403 subjects with OHIP5 data.
| Variables | No | OHIP 5 mean ± sd | Effect size Cohen’s d (95%CI) |
|---|---|---|---|
| Presence of denture | 396a | 0.91 (0.16 to 1.66) | |
| Yes | 7 | 5.3 ± 4.5 | |
| No | 389 | 2.7 ± 2.8 | |
| Number of natural teeth present | 395b | 1.35 (0.68 to 2.02) | |
| Less than 20 teeth | 9 | 6.4 ± 5.7 | |
| Equal or more than 20 teeth | 386 | 2.6 ± 2.7 | |
| Treatment urgency | 396a | −0.04 (−0.41 to 0.32)* | |
| Urgent care | 1 | 14.0 ± 0.0 | |
| Early care | 31 | 2.8 ± 3.1 | |
| No obvious problem | 364 | 2.7 ± 2.8 |
Excluding ‘Urgent care’ group because of too small number of subjects
Missing data for
7 and
8 subjects
Effect sizes for OHIP5 group differences were large when expected to be large (Cohen’s d 0.91 and 1.35 for denture presence or number of natural teeth) and trivial, i.e., close to zero, when expected not to be present (Cohen’s d −0.04 for the comparison of “early care” versus “no obvious problem”), supporting sufficient known-groups validity of the OHIP5 scores.
3.4. Reliability
Cronbach’s alpha of 0.75 (lower limit of the 95% confidence interval: 0.71) and item-rest correlations ranging from 0.70 to 0.76 indicated satisfactory reliability (Table 4). The Cronbach alphas of 0.68 to 0.70 when each of the five items would be deleted from the scale were homogenous and demonstrated that scale reliability would not change much if a particular OHIP5 item would not be included in the instrument.
Table 4.
Internal consistency measured by Cronbach’s alpha and item-rest correlation in 403 subjects with OHIP5 data.
| OHIP5 items | Cronbach’s alpha when item is deleted | Item-rest correlation |
|---|---|---|
| Difficulty chewing | 0.68 | 0.76 |
| Painful aching | 0.69 | 0.73 |
| Uncomfortable about appearance | 0.70 | 0.71 |
| Less flavor in food | 0.70 | 0.70 |
| Difficulty doing usual jobs | 0.70 | 0.70 |
4. Discussion
The present study is the first providing evidence for score dimensionality, reliability, and validity in the adult general population for an English-language 5-item OHIP. The results were considered sufficient for the instrument’s use to discriminate subjects with different levels of perceived oral health. The use of this validated ultra-short OHIP provides an opportunity to perform OHRQoL assessment in almost any setting because of the minimal burden to subjects and individuals collecting the data such regular dental patients and their dental practitioners.
The Dimensions of Oral Health-Related Quality of Life Project suggested that the construct OHRQoL has four dimensions (Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact), but a total score can sufficiently characterize overall OHRQoL. Our study confirmed this for the ultrashort OHIP version. OHIP5 has at least one indicator for each of the four dimensions, supporting its content validity. A unidimensional model fit OHIP5 data well in our population, a finding similar to OHIP14 scores in another population [32]. This means while perceived oral health is multidimensional from a conceptual perspective, when using OHIP5, a single score can summarize the various aspects of OHRQoL with one total score. This leads to a simple, but nevertheless comprehensive OHRQoL assessment with one informative score.
Validity coefficients for OHIP5 scores in our study were similar compared with the literature. The strongest evidence for the OHIP5 construct validity came from the association between global oral health status and OHIP5 scores. A correlation of both scores resulted in a Pearson correlation coefficient of 0.30. This finding was compared to previous studies using OHIP5 scores using simple summary scores instead of a latent variable. In the general population, OHIP5 scores correlated with a global assessment of self-reported oral health in Germany (r = 0.50)[9] and in Sweden (r=0.46)[11]. In patient populations, coefficients of 0.48, 0.40 and 0.21 were observed in Japanese prosthodontic patients [33], in German TMD patients[9] and in Dutch TMD patients[10], respectively, which is on average (0.36) close to the value of 0.30 we observed.
Latent variable analysis, correlating the oral health global indicator with the construct OHRQoL measured by the individual OHIP5 items, resulted in a correlation of 0.46. This correlation was higher than 0.30 because the latent variable analysis was adjusted for measurement error and therefore the correlation was de-attenuated. This SEM-based correlation could be compared to results from longer items OHIPs, i.e., these instruments characterize the construct OHRQoL with less measurement error because of more items. Our observed correlation of 0.46 was similar to results in Germany (r=0.44)[9], Japan (r=0.53)[2], the Netherlands (r=0.28)[10], Saudi Arabia (r=0.59)[34], Croatia (r=0.40) and Slovenia (r=0.55)[18].
In groups of subjects with different oral status, OHIP5’s construct validity was further supported by effect sizes meeting expectations about their magnitude. Subjects with fewer teeth or subjects who wear removable dentures usually suffer from impaired OHRQoL. The literature provided strong evidence that denture status [23,24,35] as well as the total number of teeth were significantly associated with OHRQoL [25,26,35]. National surveys in the Australia and the UK found that OHIP14 scores were increased (meaning that more problems were reported) for subjects with only 1–8 remaining teeth (10.0 OHIP units in Australia; 6.6 units in the UK) compared to subjects with 25–32 remaining teeth (6.7 units in Australia; 4.9 units in UK).[26] Overall, summarizing the various aspects of the validity assessments conducted in this study, we conclude that the OHIP5 scores demonstrated sufficient validity.
In our study, Cronbach’s alpha for OHIP5 scores in an US adult general population was found to be 0.75. According to guidelines that value indicates “satisfactory” reliability.[36] The magnitude of the reliability coefficients was in line with expectations and the literature. Our population was similar to population-based settings in Germany, Sweden and Hungary where random samples of the general population were studied. German and Swedish results of 0.76[9] and 0.77[11], respectively, were almost identical to our findings. In Hungary, internal consistency was lower with 0.58.[25]
Reliability results in patient populations were more varied than those measured in general populations, but somewhat similar to values observed in our study. In Japanese prosthodontic patients, a high value of 0.81 was observed.[2] In TMD patients, values of 0.65 were seen in Germany[9] and 0.67 in the Netherlands[10]. Summarizing all reliability results, the internal consistency results for OHIP5 appear to be satisfactory for such a short instrument and are relatively similar across populations, given the inherent variability attributed to sampling and study settings. In conclusion, OHIP5 seemed to be sufficiently reliable in general population subjects.
Our study has strengths and limitations. Compared to previous studies, the use of latent variable models to assess the construct validity is a sophisticated method to adjust for the influence of measurement error. However, this analysis was performed only for self-reported global oral health status in order to show the difference between latent variable-based methods and summary scores computations. The Minnesota State Fair attendees were a particular group of general population subjects. We assume that the vast majority of them have a dentist and therefore our subjects also represent typical patients attending a general dentist’s office. Finally, we did not evaluate OHIP5 against OHIP49 as the most comprehensive OHRQoL measure. We did not deem is necessary because OHIP5 scores have consistently performed well in correlation analyses with OHIP49 scores. [2,11]Indeed, when we investigated an English-language population of patients with four orofacial pain conditions in Minnesota, we observed a correlation of 0.90 between OHIP5 and OHIP49.We have no reason to assume that the ultrashort OHIP would not capture the long questionnaire’s information similarly in general population subjects in Minnesota and, for that matter, in other English-language populations likely as well.
5. Conclusion
We validated the English-language version of OHIP5 in the adult general population. We found evidence for score unidimensionality and sufficient reliability as well as validity, making this instrument suitable for cross-sectional studies in this and similar populations.
6. Clinical and public health relevance of the findings
OHRQoL is an informative concept to evaluate the impact of oral disorders and dental interventions in research studies. The benefits of this information are usually weighted against the burden to obtain this information. The psychometrically sound and publically available 5-item OHIP provides a feasible approach to perform OHRQoL assessment in almost any settings because the burden to collect and to interpret the data is low. OHRQoL measurement is therefore now also possible in regular dental practice. Not only can the practitioner compare OHRQoL scores across patients or contrast pre and post-treatment scores to measure and document more systematically his/her patient’s perceived oral health situation, the practitioner can also link his/her own patients to the hundreds of thousands of patients already studied with OHIP in the international literature which allows both the patient and the practitioner to benefit better from clinical research results.
Acknowledgments
Research reported in this publication was supported by the National Institute of Dental and Craniofacial Research of the National Institutes of Health under Award Number R01DE022331.
Footnotes
Conflict of interest
None of the authors reported any conflict of interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Al-Jundi MA, Szentpetery A, John MT. An Arabic version of the Oral Health Impact Profile: translation and psychometric properties. International Dental Journal. 2007;57:84–92. doi: 10.1111/j.1875-595x.2007.tb00443.x. [DOI] [PubMed] [Google Scholar]
- 2.Baba K, Inukai M, John M. Feasibility of oral health-related quality of life assessment in prosthodontic patients using abbreviated Oral Health Impact Profile questionnaires. J Oral Rehabil. 2008;35:224–228. doi: 10.1111/j.1365-2842.2007.01761.x. [DOI] [PubMed] [Google Scholar]
- 3.Sanders AE, Slade GD, John MT, Steele JG, Suominen-Taipale AL, Lahti S, et al. A cross-national comparison of income gradients in oral health quality of life in four welfare states: application of the Korpi and Palme typology. J Epidemiol Community Health. 2009;63:569–574. doi: 10.1136/jech.2008.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reissmann DR, Remmler A, John MT, Schierz O, Hirsch C. Impact of response shift on the assessment of treatment effects using the Oral Health Impact Profile. Eur J Oral Sci. 2012;120:520–525. doi: 10.1111/j.1600-0722.2012.00998.x. [DOI] [PubMed] [Google Scholar]
- 5.Sierwald I, John MT, Durham J, Mirzakhanian C, Reissmann DR. Validation of the response format of the Oral Health Impact Profile. Eur J Oral Sci. 2011;119:489–496. doi: 10.1111/j.1600-0722.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- 6.Reissmann DR, Sierwald I, Heydecke G, John MT. Interpreting one oral health impact profile point. Health Qual Life Outcomes. 2013;11:12. doi: 10.1186/1477-7525-11-12. 7525-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 8.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 9.John MT, Miglioretti DL, LeResche L, Koepsell TD, Hujoel P, Micheelis W. German short forms of the oral health impact profile. Community Dent Oral Epidemiol. 2006;34:277–288. doi: 10.1111/j.1600-0528.2006.00279.x. [DOI] [PubMed] [Google Scholar]
- 10.Van der Meulen M, John M, Naeije M, Lobbezoo F. Developing abbreviated OHIP versions for use with TMD patients. J Oral Rehabil. 2012;39:18–27. doi: 10.1111/j.1365-2842.2011.02242.x. [DOI] [PubMed] [Google Scholar]
- 11.Larsson P, John M, Hakeberg M, Nilner K, List T. General population norms of the Swedish short forms of Oral Health Impact Profile. J Oral Rehabil. 2014;41:275–281. doi: 10.1111/joor.12137. [DOI] [PubMed] [Google Scholar]
- 12.Kabage Amanda. personal communication. Sep 23, 2015.
- 13.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 14.John M, Reißmann D, Feuerstahler L, Waller N, Baba K, Larsson P. Dimensions of Oral Health-Related Quality of Life Project-overview and studied population. J Prosthodont Res. 2014;1:26–34. doi: 10.1016/j.jpor.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John M, Reissmann D, Feuerstahler L, Waller N, Baba K, Larsson P, et al. Exploratory factor analysis of the Oral Health Impact Profile. J Oral Rehabil. 2014;41:635–643. doi: 10.1111/joor.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.John MT, Feuerstahler L, Waller N, Baba K, Larsson P, Celebic A, et al. Confirmatory factor analysis of the Oral Health Impact Profile. J Oral Rehabil. 2014;41:644–652. doi: 10.1111/joor.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van der Meulen MJ, John MT, Naeije M, Lobbezoo F. The Dutch version of the Oral Health Impact Profile (OHIP-NL): Translation, reliability and construct validity. BMC oral health. 2008;8:11. doi: 10.1186/1472-6831-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rener-Sitar K, Petričević N, Čelebić A, Marion L. Psychometric properties of Croatian and Slovenian short form of oral health impact profile questionnaires. Croat Med J. 2008;49:536–544. doi: 10.3325/cmj.2008.4.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong M, Lo E, McMillan AS. Validation of a Chinese version of the oral health impact profile (OHIP) Community Dent Oral Epidemiol. 2002;30:423–430. doi: 10.1034/j.1600-0528.2002.00013.x. [DOI] [PubMed] [Google Scholar]
- 20.Allison P, Locker D, Jokovic A, Slade G. A cross-cultural study of oral health values. J Dent Res. 1999;78:643–649. doi: 10.1177/00220345990780020301. [DOI] [PubMed] [Google Scholar]
- 21.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6:1–55. [Google Scholar]
- 22.Christoffersson A. Two-step weighted least squares factor analysis of dichotomized variables. Psychometrika. 1977;42:433–438. [Google Scholar]
- 23.Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990;54:680–687. [PubMed] [Google Scholar]
- 24.Rener-Sitar K, Čelebić A, Petričević N, Papić M, Sapundzhiev D, Kansky A, et al. The Slovenian version of the Oral Health Impact Profile Questionnaire (OHIP-SVN): translation and psychometric properties. Coll Antropol. 2009;33:1177–1183. [PubMed] [Google Scholar]
- 25.Szabó G, John MT, Szántó I, Marada G, Kende D, Szentpétery A. Impaired oral health-related quality of life in Hungary. Acta Odontol Scand. 2011;69:108–117. doi: 10.3109/00016357.2010.538717. [DOI] [PubMed] [Google Scholar]
- 26.Steele JG, Sanders AE, Slade GD, Allen PF, Lahti S, Nuttall N, et al. How do age and tooth loss affect oral health impacts and quality of life? A study comparing two national samples. Community Dent Oral Epidemiol. 2004;32:107–114. doi: 10.1111/j.0301-5661.2004.00131.x. [DOI] [PubMed] [Google Scholar]
- 27.Gotfredsen K, Walls AW. What dentition assures oral function? Clin Oral Implants Res. 2007;18:34–45. doi: 10.1111/j.1600-0501.2007.01436.x. [DOI] [PubMed] [Google Scholar]
- 28.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 29.L StataCorp. Stata data analysis and statistical Software, Special Edition Release. 2014;10 [Google Scholar]
- 30.R Development Core Team. R:. A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. [Accessed 3 March 2015]. [Google Scholar]
- 31.Rosseel Y. lavaan: An R package for structural equation modeling. Journal of Statistical Software. 2012;48:1–36. [Google Scholar]
- 32.dos Santos CM, de Oliveira BH, Nadanovsky P, Hilgert JB, Celeste RK, Hugo FN. The Oral Health Impact Profile-14: a unidimensional scale? Cad Saude Publica. 2013;29:749–757. doi: 10.1590/s0102-311x2013000800012. [DOI] [PubMed] [Google Scholar]
- 33.Yamazaki M, Inukai M, Baba K, John M. Japanese version of the Oral Health Impact Profile (OHIP-J) J Oral Rehabil. 2007;34:159–168. doi: 10.1111/j.1365-2842.2006.01693.x. [DOI] [PubMed] [Google Scholar]
- 34.Al-Jundi MA, Szentpetery A, John MT. An Arabic version of the Oral Health Impact Profile: translation and psychometric properties. Int Dent J. 2007;57:84–92. doi: 10.1111/j.1875-595x.2007.tb00443.x. [DOI] [PubMed] [Google Scholar]
- 35.Locker D, Slade GD. Association between clinical and subjective indicators of oral health status in an older adult population. Gerodontology. 1994;11:108–114. doi: 10.1111/j.1741-2358.1994.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 36.Bland JM, Altman DG. Statistics notes: Cronbach’s alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]