Abstract
Objectives
In this study, we examined whether (1) positive end-expiratory pressure (PEEP) has a protective effect on the risk of major postoperative respiratory complications in a cohort of patients undergoing major abdominal surgeries and craniotomies, and (2) the effect of PEEP is differed by surgery type.
Background
Protective mechanical ventilation with lower tidal volumes and PEEP reduces compounded postoperative complications after abdominal surgery. However, data regarding the use of intraoperative PEEP is conflicting.
Methods
In this observational study, we included 5915 major abdominal surgery patients and 5063 craniotomy patients. Analysis was performed using multivariable logistic regression. The primary outcome was a composite of major postoperative respiratory complications (respiratory failure, reintubation, pulmonary edema, and pneumonia) within 3 days of surgery.
Results
Within the entire study population (major abdominal surgeries and craniotomies), we found an association between application of PEEP ≥5cmH2O and a decreased risk of postoperative respiratory complications compared with PEEP <5cmH2O. Application of PEEP >5cmH2O was associated with a significant lower odds of respiratory complications in patients undergoing major abdominal surgery (odds ratio 0.53, 95% confidence interval 0.39 – 0.72), effects that translated to deceased hospital length of stay [median hospital length of stay : 6 days (4–9 days), incidence rate ratios for each additional day: 0.91 (0.84 - 0.98)], whereas PEEP >5cmH2O was not significantly associated with reduced odds of respiratory complications or hospital length of stay in patients undergoing craniotomy.
Conclusions
The protective effects of PEEP are procedure specific with meaningful effects observed in patients undergoing major abdominal surgery. Our data suggest that default mechanical ventilator settings should include PEEP of 5–10cmH2O during major abdominal surgery.
Worldwide, more than 234 million patients per year undergo a surgical procedure.1 General anesthesia including mechanical ventilation is a necessity for the majority of these procedures. Postoperative respiratory complications are common with reported incidences of 5%-10% in the general surgical population, depending on their definition.2–4 These complications represent a leading cause of increased morbidity and mortality5,6 and are associated with prolonged hospital stay and increases in healthcare utilization and costs.7,8
Different intraoperative ventilation strategies including the use of positive end-expiratory pressure (PEEP) have been proposed to reduce the incidence of postoperative respiratory complications. The use of PEEP may prevent repeated opening and closing of alveoli (atelectrauma) and development of atelectasis, thereby reducing the risk of postoperative adverse outcomes.9,10 However, PEEP also has the potential to result in cyclic overstretching and inflammation of aerated lung areas.11–13 Recent studies have reported contradictory results regarding the association between PEEP and the risk of postoperative respiratory complications.14–17
An explanation for these conflicting results could be the fact that optimal PEEP levels may vary with the respiratory functional burden produced by different types of surgery. Although supine position and muscle relaxation, present in most surgeries, produce lung derecruitment,18 substantially different additional factors are present in distinct types of operations. Indeed, during abdominal surgery the diaphragm can be shifted in a cephalad direction or have its movement restricted because of retractors, pneumoperitoneum, Trendelenburg position, and other surgical maneuvers. These factors reduce chest-wall elasticity and functional residual capacity, and favor the development of atelectasis.19,20 Application of high PEEP would oppose those mechanisms. In contrast, patients undergoing craniotomy usually do not present additional factors contributing to lung derecruitment, and might consequently require a lower PEEP for mechanical ventilation. We, therefore, examined whether (1) PEEP has a beneficial effect on the risk of major postoperative respiratory complications in a study population including major abdominal surgeries and craniotomies and (2) the effect of PEEP differs in patients undergoing major abdominal surgery compared with those undergoing craniotomies.
METHODS
Study Design
The project received approval from the Partners Institutional Review Board, protocol number: 2014P002718. Data were retrieved from the Anesthesia Information Management System (AIMS) and the Research Patient Data Registry and combined to provide pre-, intra-, and postoperative information. The AIMS records ventilator parameters every minute, provides intraoperative data regarding drug and fluid therapy, transfusions and anesthesia techniques, and equipment during the procedure. The Research Patient Data Registry is a centralized registry that compiles data from various institutional systems for research objectives and provides pre- and postoperative information about demographics, medical history, laboratory results, postoperative outcome, and survival.
Subject Selection
We included all patients over the age of 18 years who underwent major abdominal surgery or craniotomy with general anesthesia at the Massachusetts General Hospital, Boston, MA, between January 2007 and August 2014. We used Current Procedural Terminology codes to identify the surgical procedures. Craniotomies include all procedures performed by a neurosurgeon, except for spine surgery. Major abdominal surgery was defined using a previously developed classification described in the prior literature.21 Only patients who were intubated with an endotracheal tube at the start and extubated at the end of the procedure were included. Exclusion criteria were missing data regarding exposure, outcome variables, or covariates and patients with a billing code for any of the outcome variables within 4 weeks before their procedure. Further, patients were excluded if they had subsequent surgical procedures that were separated by less than 10 days.
Outcome
The outcome was a composite of major postoperative respiratory complications within 3 days of the index procedure. This outcome definition has been used in previous studies17,22 and includes respiratory failure, reintubation, pneumonia, and pulmonary edema. The outcome variable was treated as a binary variable in our model. Billing codes from the International Statistical Classification of Diseases, ninth revision (ICD-9) and Current Procedural Terminology definitions were used to define the outcome variables. The codes used to generate the outcome measure can be found in the appendix (table S1, http://links.lww.com/SLA/A866).
Exposure
The median PEEP value applied during the surgical procedure was obtained for every patient from the AIMS. The median PEEP level was specified as a categorical variable with 3 categories, based on prior studies in perioperative medicine.15,17,23 The 3 categories were PEEP <5 cmH2O, PEEP = 5 cmH2O, and PEEP >5 cmH2O.
Covariate Data
Baseline characteristics including sex, age, body mass index, emergent or nonemergent surgery, and American Society of Anesthesiologists physical status classification were obtained. The Charlson Comorbidity Index Score24 was calculated using billing codes defined by the ICD-9 and used to adjust for comorbidities including existing or previous pulmonary diseases. We adjusted for the risk of postoperative respiratory complications using the previously validated SPORC score.25 We collected the Work Relative Value Units for all procedures to adjust for surgical complexity. Further, we controlled for intraoperative factors including fluid therapy, transfusion of fresh frozen plasma, packed red blood cells and platelets, duration of intraoperative ventilation, and plateau pressure.
Statistical Analysis
Primary Analysis
In the primary analysis, multivariable logistic regression was performed to assess the effect of intraoperative application of PEEP on the risk of postoperative respiratory complications, in a cohort including both major abdominal and craniotomy procedures. We tested for collinearity between PEEP and plateau pressure by linear regression, which showed a variance inflation factor of 1 (not collinear). We adjusted for the covariates listed above, based on previously identified risk factors for postoperative respiratory complications and physiological plausibility without further selection. Continuous variables were categorized into quintiles and then included in the model. We tested for interactions between PEEP and fluids, duration of ventilation, age, and emergent/urgent surgery, and found that none of these interaction terms were significant (smallest P value of 0.13). Therefore, these interaction terms were not included in any of the analytic models.
Secondary Analysis
We then tested the hypothesis that the preventive effect of PEEP on the risk of postoperative respiratory complications is stronger in patients undergoing abdominal surgery compared with those undergoing craniotomies. This was done by including an interaction term of PEEP multiplied by surgery type (major abdominal vs craniotomy) in our multivariable logistic regression model. We used the Wald P value of the interaction term to assess whether there was an interaction between PEEP and surgery type. Given that the interaction term was significant, we stratified the cohort into 2 subsets based on surgery type: major abdominal surgery and craniotomy. We examined the association of intraoperative application of PEEP and risk of postoperative respiratory complications separately in both subgroups, using the same logistic regression model as in the primary analysis. We also examined the association between PEEP and hospital length of stay in days, separately in both surgical subgroups, using zero-truncated Poisson regression. This analysis was adjusted for all covariates used in the primary analysis.17
Sensitivity Analyses
To eliminate possible collinearity, we excluded plateau pressure from the logistic regression model to see if the effect estimates remained the same. To ensure that the benefits of PEEP in major abdominal surgery were not caused by other parameters, we repeated the subgroup analysis by adjusting for driving pressure (instead of plateau pressure), tidal volume, intraoperative median oxygen saturation to median fraction of inspired oxygen concentration ratio, dose of nondepolarizing neuromuscular blocking agents, and dose of neostigmine.17
We explored whether the differences among surgery types were simply because of differences in patient characteristics in the 2 cohorts by creating a propensity score to determine the type of surgery a patient would receive. This was created using type of surgery—that is, abdominal versus craniotomy as the dependent variables and then all the covariates used in the primary analysis as independent predictors. Patients were then matched in a 1:1 fashion using a greedy matching algorithm without replacement with a maximum distance of 0.1. We then repeated the procedure specific analysis in this matched cohort of patients.
To further characterize the dose-response function, we included PEEP as a continuous variable rather than categories. Nonlinear associations between PEEP and the log odds of complications were assessed by the inclusion of quadratic term and assessing the P value of this variable. Additionally we explored spline terms with cut-offs of 5.6 cmH2O and 8 cmH2O.
All statistical analyses were performed using IBM SPSS Statistics (version 19.0. Armonk, NY) and SAS (version 9.3; SAS, Carey, NC). Continuous and ordinal variables were expressed as mean (± standard deviation), categorical variables as n (%). All tests were two-tailed with significance defined as a P value of ≤ 0.05.
RESULTS
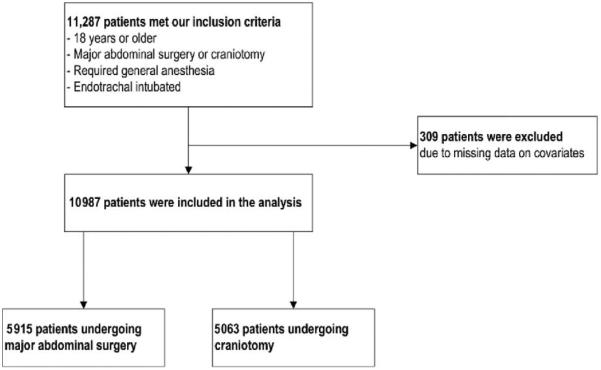
A total of 11,287 patients met our eligibility criteria. Less than 0.03% of the patients were excluded because of missing data, leading to a final set of 10,978 patients; among which 5915 patients undergoing major abdominal surgery and 5063 patients undergoing craniotomy (Fig. 1). The majority of patients were ventilated using volume control (87%). The median PEEP values in our cohort had a range from 0 cmH2O to 17 cmH2O. Patients undergoing major abdominal surgery were more likely to have comorbidities, preexisting pulmonary disease, emergency procedures, and transfusion of blood products compared with patients undergoing craniotomy (Table 1). The most common type of surgery in the abdominal group was gastrointestinal surgery (52.7%) and the most frequent indication for craniotomies was tumor resection (45.1%).
FIGURE 1.
Flow diagram of study population.
TABLE 1.
Baseline Characteristics in the Entire Unmatched Cohort
| Total Cohort (n=10,978) |
Major Abdominal Surgery (n=5915) |
Craniotomy (n=5063) |
|
|---|---|---|---|
| Demographic characteristics | |||
| Sex, male, n (%) | 5755 (52.4) | 2944 (49.8) | 2811 (55.5) |
| Age (years), mean ± SD | 55.6±16.3 | 58.8±16.0 | 51.9±15.9 |
| Category of body mass index (kg/m2), n (%) | |||
| 1 | 204 (1.9) | 140 (2.4) | 64 (1.3) |
| 2 | 3949 (36.0) | 2300 (38.9) | 1649 (32.6) |
| 3 | 3769 (34.3) | 1976 (33.4) | 1793 (35.4) |
| 4 | 1855 (16.9) | 941 (15.9) | 914 (18.1) |
| 5 | 1201 (10.9) | 558 (9.4) | 643 (12.7) |
| Comorbidities | |||
| Charlson Comorbidity Index, mean±SD | 3.4±3.5 | 4.3±3.7 | 2.3±2.9 |
| Existing chronic pulmonary disease, n (%) | 1413 (12.9) | 833 (14.1) | 580 (11.5) |
| Score for prediction of postoperative respiratory complications, mean±SD |
2.7±2.1 | 2.0±2.1 | 3.5±1.9 |
| Emergency/urgent, n (%) | 1075 (9.8) | 677 (11.4) | 398 (7.9) |
| Work relative value units, mean±SD | 30.8±14.7 | 30.7±13.9 | 30.9±15.6 |
| Intraoperative factors | |||
| Median PEEP (cmH2O), n (%) | |||
| <5 | 4078 (36.1) | 1997 (33.8) | 1963 (38.8) |
| 5 | 5719 (50.7) | 3140 (53.1) | 2427 (47,9) |
| >5 | 1490 (13.2) | 778 (13.2) | 673 (13.3) |
| Median plateau pressure (cmH2O), mean ± SD | 17.9 ±3.9 | 17.7 ±3.9 | 18.2±3.9 |
| Total resuscitation volume (mL), mean±SD | 3398±7,505 | 3698±6749 | 3046±8290 |
| Platelets transfused (units), mean±SD | 0.1±1.1 | 0.1±1.2 | 0.1±1.0 |
| Fresh frozen plasma transfused (units), mean±SD | 0.08±0.7 | 0.1±0.9 | 0.02±0.2 |
| Packed red blood cells transfused (units), mean±SD | 0.1±0.7 | 0.2±0.8 | 0.04±0.3 |
| Duration of intraoperative ventilation (hours), mean ± SD | 4.2±3.1 | 4.0±3.0 | 4.4±3.2 |
Postoperative respiratory complications were present in 8% of the patients in the total cohort and were more frequent in patients undergoing major abdominal procedures (11.2%) than in those undergoing craniotomies (4.3%) (Table 2). The incidence of postoperative respiratory complications in patients undergoing major abdominal surgery was lower when a PEEP of ≥5 cmH2O was applied than when PEEP <5 cmH2O was used (10.9% vs 12.4%) (Table 2). In contrast, we did not observe a decrease in incidence of postoperative respiratory complications when a PEEP of ≥5 cmH2O was applied in patients undergoing craniotomies (Table 2).
TABLE 2.
Incidences of Outcomes for Every PEEP Exposure Group in the Total Cohort Including Major Abdominal Surgeries and Craniotomies
| Total Cohort (n=10,978) |
Major Abdominal Surgery (n=5915) |
Craniotomy (n=5063) |
||||
|---|---|---|---|---|---|---|
| Number of Patients |
Outcome Events, n (%) |
Number of Patients |
Outcome Events, n (%) |
Number of Patients |
Outcome Events, n (%) |
|
| Exposure | ||||||
| PEEP <5cmH2O | 3960 | 331 (8.4) | 1997 | 247 (12.4) | 1963 | 84 (4.3) |
| PEEP=5 cmH2O | 5567 | 425 (7.6) | 3140 | 328 (10.4) | 2427 | 97 (4.0) |
| PEEP >5cmH2O | 1451 | 120 (8.3) | 778 | 85 (10.9) | 673 | 35 (5.2) |
Patients who developed complications were more likely to be admitted to the intensive care unit (ICU) within 7 days after the procedure [unadjusted risk ratio: 5.3, 95% confidence interval (CI) 4.8–5.9] and had a higher risk of 30-day mortality (unadjusted risk ratio: 5.0, 95% CI 3.37.6).
Primary Analysis
For the entire cohort of patients undergoing either major abdominal surgery or craniotomies, there was a significant protective effect of PEEP = 5 cmH2O [odds ratio (OR) 0.72, 95% CI 0.61–0.85] and PEEP >5 cmH2O (OR 0.60, 95% CI 0.47–0.79) (Fig. 2) in reducing postoperative respiratory outcomes (Fig. 2).
FIGURE 2.
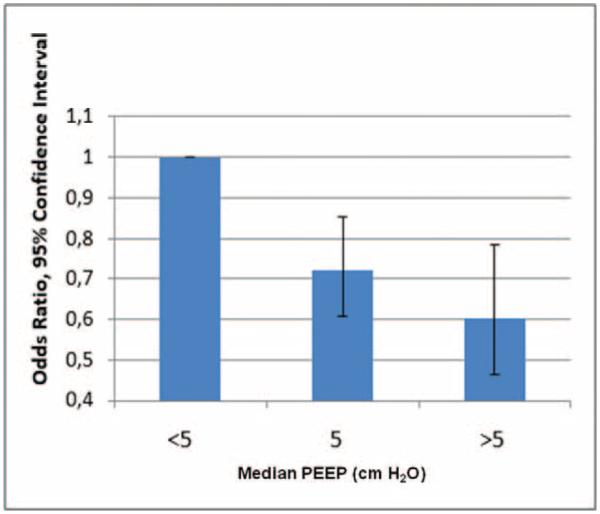
Effect of median intraoperative PEEP on the risk of postoperative respiratory complications in the entire cohort of patients undergoing major abdominal surgery or craniotomy. Multivariable logistic regression analysis, adjusted for: age, sex, body mass index, American Society of Anesthesiologists classification, score for prediction of postoperative respiratory complications, Charlson Comorbidity index, work relative value units, preexisting pulmonary disease, duration of ventilation, units of packed red blood cells, fresh frozen plasma and platelets transfused, urgent/emergent surgery, total fluids administered, type of surgery, and plateau pressure. A PEEP of ≥5 cmH2O is associated with a lower odds of respiratory complications compared with PEEP <5 cmH2O, across surgical services.
Secondary Analysis
There was a significant interaction between PEEP and surgery type (Wald P <0.01), indicating that the beneficial effect of PEEP (5 cmH2O or >5 cmH2O) differed by type of surgery. Accordingly, we examined the effect of PEEP in the separately in each group of surgical procedures. The adjusted analysis of the effect of PEEP in patients undergoing major abdominal surgery revealed a significant protective effect of PEEP = 5cmH2O (OR 0.69, 95% CI 0.56–0.84) and PEEP >5 cmH2O (OR 0.53, 95% CI 0.39–0.72) in reducing postoperative respiratory complications (Fig. 3). These effects of PEEP during major abdominal surgery translated into a decreased hospital length of stay. Median hospital length of stay (IQR) was 6 days (IQR 4–9). Application of PEEP = 5 cmH2O and PEEP >5 cmH2O was associated with a decreased hospital length of stay; incidence rate ratios (IRR) for each hospital day of 0.92 (0.88–0.97) and 0.91 (0.84–0.98), respectively. In contrast, the same adjusted analysis applied to patients undergoing craniotomy did not show a significant effect of PEEP = 5 cmH2O (OR 0.80, 95% CI 0.57–1.13) and no significant effect of PEEP >5 cmH2O (OR 0.89, 95% CI 0.54–1.46) on the risk of postoperative respiratory complications (Fig. 3), and did not affect hospital length of stay.
FIGURE 3.
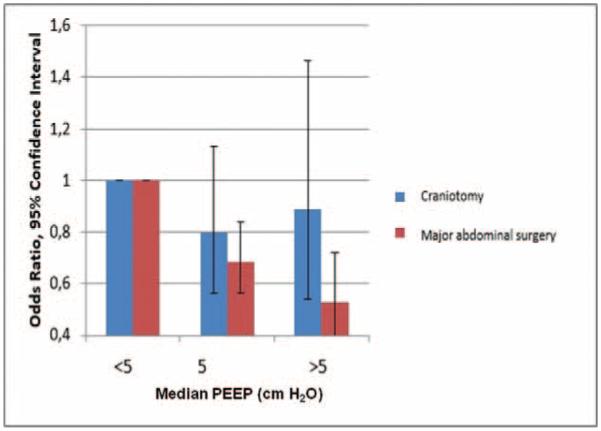
Respiratory complications as a function of median intraoperative PEEP. Data are shown separated by abdominal surgery and craniotomy. Multivariable logistic regression analysis, adjusted for: age, sex, body mass index, American Society of Anesthesiologists classification, score for prediction of postoperative respiratory complications, Charlson Comorbidity index, work relative value units, preexisting pulmonary disease, duration of ventilation, units of packed red blood cells, fresh frozen plasma and platelets transfused, urgent/emergent surgery, total fluids administered, and plateau pressure. There is a significant reduction in the odds ratio for postoperative respiratory complications for PEEP ≥5 in major abdominal surgery compared with PEEP 5 and PEEP 0, whereas no significant beneficial effect of high PEEP is observed in patients undergoing a craniotomy.
Sensitivity Analysis
As PEEP might influence the plateau pressure,26 we excluded plateau pressure as a covariate from our primary logistic regression model to eliminate collinearity. We found that the association between application of high PEEP and a decreased risk of post-operative respiratory complications remained significant (Table 3). To determine whether the impact of PEEP was attributed exclusively to its effects on driving pressure or tidal volumes, we performed additional analysis adjusting for driving pressure (defined as plateau pressure minus PEEP) and tidal volume in patients undergoing major abdominal surgery. The significant beneficial effect of PEEP in reducing postoperative respiratory complications remained in these sensitivity analyses (Table 4; Table 5). We also performed an additional analysis adjusting for intraoperative median oxygen saturation to median fraction of inspired oxygen concentration ratio, dose of nondepolarizing neuromuscular blocking agents, and dose of neostigmine. This analysis shows a significant protective effect of PEEP = 5 cmH2O (OR 0.66, 95% CI 0.51–0.86) and PEEP >5 cmH2O (OR 0.51, 95% CI 0.33–0.78) in patients undergoing major abdominal surgery compared with PEEP <5 cmH2O.
TABLE 3.
Effect of PEEP on the Risk of Postoperative Respiratory Complications in Patients Undergoing Major Abdominal Surgery, Plateau Pressure Excluded as Covariate
| Major Abdominal Surgery (N=5915) |
|||
|---|---|---|---|
| Exposure | Patients With Outcome Events, n (%) | OR | 95% CI |
| PEEP <5cmH2O (n=1997) | 247 (12.4) | 1.00 | – |
| PEEP=5cmH2O (n=3140) | 328 (10.4) | 0.72 | 0.59–0.87 |
| PEEP>5cmH2O (n=778) | 85 (10.9) | 0.62 | 0.46–0.84 |
Multivariable logistic regression analysis, adjusted for: age, sex, body mass index, American Society of Anesthesiologists classification, score for prediction of postoperative respiratory complications, Charlson Comorbidity Index, work relative value units, preexisting pulmonary disease, duration of ventilation, units of packed red blood cells, fresh frozen plasma and platelets transfused, urgent/emergent surgery, and total fluids administered. CI indicates confidence interval; OR, odds ratio.
TABLE 4.
Effect of PEEP on the Risk of Postoperative Respiratory Complications in Patients Undergoing Major Abdominal Surgery, Driving Pressure Included as an Additional Covariate
| Major Abdominal Surgery (N=5915) |
|||
|---|---|---|---|
| Exposure | Patients With Outcome Events, n (%) | OR | 95% CI |
| PEEP <5cmH2O (n=1997) | 247 (12.4) | 1.00 | – |
| PEEP=5cmH2O (n=3140) | 328 (10.4) | 0.78 | 0.64–0.95 |
| PEEP>5cmH2O (n=778) | 85 (10.9) | 0.68 | 0.50–0.92 |
Multivariable logistic regression analysis, adjusted for: age, sex, body mass index, American Society of Anesthesiologists classification, score for prediction of postoperative respiratory complications, Charlson Comorbidity Index, work relative value units, preexisting pulmonary disease, duration of ventilation, units of packed red blood cells, fresh frozen plasma and platelets transfused, urgent/emergent surgery, total fluids administered, and driving pressure. CI indicates confidence interval; OR, odds ratio.
TABLE 5.
Effect of PEEP on the Risk of Postoperative Respiratory Complications in Patients Undergoing Major Abdominal Surgery, Tidal Volume Included as an Additional Covariate
| Major Abdominal Surgery (N=5915) |
|||
|---|---|---|---|
| Exposure | Patients With Outcome Events, n (%) | OR | 95% Ci |
| PEEP <5cmH2O (n=1997) | 247 (12.4) | 1.00 | – |
| PEEP=5cmH2O (n=3140) | 328 (10.4) | 0.67 | 0.55–0.82 |
| PEEP>5cmH2O (n=778) | 85 (10.9) | 0.49 | 0.36–0.67 |
Multivariable logistic regression analysis, adjusted for: age, sex, body mass index, American Society of Anesthesiologists classification, score for prediction of postoperative respiratory complications, Charlson Comorbidity index, work relative value units, preexisting pulmonary disease, duration of ventilation, units of packed red blood cells, fresh frozen plasma and platelets transfused, urgent/emergent surgery, total fluids administered, plateau pressure, and tidal volume. CI indicates confidence interval; OR, odds ratio.
When propensity score matching was used, there were 5948 patients who could be matched. Baseline characteristics of the propensity score matched cohort are described in Table 6. Logistic regression analysis in the propensity-score matched cohort shows a significant protective effect of PEEP = 5 cmH2O (OR 0.73, 95% CI 0.54–0.99) and PEEP >5 cmH2O (OR 0.42, 95% CI 0.25–0.68) in patients undergoing abdominal surgery. The analysis in the propensity-score matched patients undergoing craniotomy did not show a significant effect of PEEP = 5 cmH2O (OR 0.77, 95% CI 0.50–1.17) and PEEP >5 cmH2O (OR 1.05, 95% CI 0.56–1.96) in reducing postoperative respiratory complications.
TABLE 6.
Baseline Characteristics in the Propensity Matched Cohort
| Major Abdominal Surgery (N=2974) | Craniotomy (N=2974) | |
|---|---|---|
| Demographic characteristics | ||
| Sex, male, n (%) | 1385 (46.5%) | 1382 (46.5%) |
| Age (years), mean±SD | 54.7±16.1 | 54.9±15.6 |
| Category of body mass index (kg/m2), n (%) | ||
| 1 | 68 (2.3) | 16 (1.4) |
| 2 | 1149 (38.6) | 333 (29.9) |
| 3 | 979 (32.9) | 404 (36.3) |
| 4 | 487 (16.4) | 199 (17.9) |
| 5 | 291 (9.8) | 160 (14.4) |
| Comorbidities | ||
| Charlson Comorbidity Index, mean ± SD | 3.0±3.2 | 3.0±3.2 |
| Existing chronic pulmonary disease, n (%) | 367 (12.3) | 368 (12.4) |
| Score for prediction of postoperative respiratory complications, mean ± SD | 1.6±1.9 | 3.6±1.9 |
| Emergency/urgent, n (%) | 233 (7.8) | 227 (7.6) |
| Intraoperative factors | ||
| Median PEEP (cmH2O), n (%) | ||
| <5 | 1108 (37.3) | 1111 (37.4) |
| 5 | 1484 (49.9) | 1476 (49.6) |
| >5 | 382 (12.8) | 387 (13.0) |
| Median plateau pressure (cmH2O), mean±SD | 17.8±4.0 | 18.2±3.8 |
| Total resuscitation volume (mL), mean ± SD | 3104±2,118 | 2794±5,515 |
| Platelets transfused (units), mean±SD | 0.04±0.5 | 0.05±0.6 |
| Fresh frozen plasma transfused (units), mean ± SD | 0.03±0.4 | 0.02±0.3 |
| Packed red blood cells transfused (units), mean ± SD | 0.08±0.5 | 0.07±0.4 |
| Duration of intraoperative ventilation (hours), mean ± SD | 4.9±1.9 | 4.7±2.4 |
To further characterize the dose-response relationship of PEEP, we repeated the analysis in major abdominal surgery patients and included PEEP as a continuous variable. This analysis showed a significant preventive effect of PEEP (OR 0.89, 95% CI 0.85–0.93) on respiratory complications. When examining a possible nonlinear relationship between PEEP and the risk of suffering a pulmonary complication through the use of a quadratic term, this variable was not significant. Additionally we explored splines with cut-offs of 5, 6, and 8. The OR between the terms were similar, suggesting that there is no clear cut-off.
The unadjusted comparison of outcomes in the 3 PEEP groups in major abdominal surgeries and craniotomies did not show significant differences for most outcome variables. We showed a significant increase of pneumonia when a PEEP of ≥ 5 cmH2O was applied in patients undergoing craniotomy (tables S2 and S3 in the appendix, http://links.lww.com/SLA/A866).
DISCUSSION
Our data show that application of PEEP during intraoperative mechanical ventilation is associated with a significantly lower risk of major postoperative respiratory complications in a large cohort including both patients undergoing major abdominal surgery and craniotomy. The preventive effect of PEEP for postoperative respiratory complications is dose-dependent, and procedure specific, and translates into a decreased length of stay of 3 days in patients who receive PEEP during abdominal surgery compared with those who do not receive PEEP.
There is significant heterogeneity in the definition of post-operative pulmonary complications. Our composite outcome represents a collection of serious pulmonary conditions. Accordingly, in the present set of patients, we showed a 5.3 times increase in the risk of ICU admission after the procedure and a 5.0 times increase in 30-day mortality in patients with a postoperative respiratory complication. Such findings document the clinical relevance of the utilized outcome measure. The used definition contrasts with others that included milder findings, such as atelectasis, with less influence on the long-term outcome.14
The effect of intraoperative ventilator settings on the risk of postoperative respiratory complications has been investigated in several studies. Our study supports the view that application of PEEP during intraoperative mechanical ventilation is associated with a significantly lower risk of major postoperative respiratory complications.23
Two randomized controlled trials compared the effects of protective mechanical ventilation (application of PEEP of 6–10 cmH2O, lower tidal volumes, and recruitment maneuvers) to a ‘standard’ care arm (low PEEP and high tidal volumes) in patients undergoing abdominal surgery. Both studies demonstrated a beneficial effect of intraoperative protective ventilation on post-operative respiratory complications.15,23 However, these trials do not enable us to determine whether the benefit of protective ventilation was because of the application of PEEP or lower tidal volume, as those variable were not independently assessed. The PROVE Network Investigators conducted then a randomized trial comparing the effects of high (12 cmH2O with recruitment maneuvers) versus low (≥2 cmH2O without recruitment maneuvers) PEEP on the risk of postoperative pulmonary complications among 900 patients undergoing open abdominal surgery. The authors found no difference in pulmonary complications by postoperative day 5 between the 2 groups.14 A possible explanation for the absence of significant effects might be that a PEEP of 12 cmH2O is too high for some patients with healthy lungs, leading to more hemodynamic deterioration than lung protection.27 This is supported by the reported hemodynamic compromise in that trial. These deleterious cardiovascular effects could have been compounded by the effects of recruitment maneuvers.14 A review including 10 randomized controlled trials with a limited number of patients concluded that evidence for the effect of intra-operative PEEP on postoperative mortality and respiratory complications is insufficient, and suggested differential effects of PEEP depending on the type of surgery.28
Our main findings were supported by the sensitivity analysis performed to explore the intervening role of additional variables implied in the studied outcomes. A recent study from our lab shows that nondepolarizing neuromuscular blocking agents and neostigmine are associated in a dose-dependent manner with the risk of postoperative respiratory complications.22 Moreover, inspired oxygen could play a role in facilitating oxygen absorption atelectasis and promoting oxidative stress. Our sensitivity analyses supported the independent beneficial effects of PEEP for respiratory outcomes in patients undergoing major abdominal surgery, as the results remained significant when controlled for plateau pressure, driving pressure, tidal volume, doses of neuromuscular blocking agents and neostigmine,22 and intraoperative median oxygen saturation to median fraction of inspired oxygen concentration ratio. Thus, the preventive effects of PEEP appear not to be merely epiphenomena of those other effects, but to have a value in itself to improve patient outcome. These results also support the view that protective intraoperative ventilation cannot be defined simply by low tidal volume. Our data imply that a combination of low tidal volume and optimal PEEP decreases the risk of postoperative respiratory complications.
Biological Plausibility of Our Findings
Reduction of functional residual capacity leading to atelectasis is a well described major pathophysiological derangement during general anesthesia and muscle paralysis.18,29 The associated mechanical ventilation cyclically deforms the lung parenchyma, and produces regional stress and strain on lung structures conductive to volutrauma, atelectrauma, and biotrauma.30 Such mechanical forces can have deleterious effects particularly in the presence of additional injurious stimuli, when a ‘‘two-hit’’ mechanism, frequent in the studied clinical setting, amplifies the resulting lung injury.31 PEEP homogenizes lung inflation and ventilation up to small peripheral regions in mechanically ventilated sheep lungs with aeration heterogeneities comparable with those of humans.32 This redistribution of lung inflation and ventilation not only improves oxygenation, but also reduces the magnitude of dynamic lung strain32 and inflammation,33 and homogenizes the distribution of lung inflammation in two-hit lung injury conditions consistent with a reduction in mechanical injury.33 Such beneficial effects of PEEP could be offset if too high levels of PEEP were used, producing lung overexpansion and cardiovascular compromise. Our finding of reduced OR for post-operative respiratory complications with PEEP in the global cohort indicates that the favorable PEEP effects predominate in the intra-operative period in the studied clinical conditions.
In addition, our results demonstrate that benefits of PEEP are higher in major abdominal surgery than in craniotomies. Major abdominal surgery is associated with high risk for postoperative respiratory complications with incidences reported up to 40%.34 The presence of numerous factors producing lung derecruitment and inflammation during abdominal surgery, such as muscle paralysis, direct and indirect diaphragmatic compression, surgical retraction, manipulation of abdominal contents, endotoxemia,35 bacteremia,36 supine position, and diaphragmatic dysfunction37 compound to produce a multihit injury.38 This contrasts to neurological surgery with lower incidences of postoperative respiratory complications reported up to 24%39 and less intraoperative factors for lung derecruitment. Our results of larger benefit of PEEP in major abdominal surgery are consistent with such differential mechanisms of pulmonary burden in the different surgery types, and indicate that individualization of PEEP to type of surgery is important to optimize outcomes.
Our data show that the application of PEEP is not the typical practice, as a significant number of patients in our cohort did not receive PEEP. It is not possible to provide a clear cut-point to delineate the optimal PEEP level that fits all patients undergoing major abdominal surgery, but a PEEP level between 5 –10 cmH2O seems to be a reasonable starting point to be selected after induction of anesthesia based on our data. The authors believe that ultimately individualized patient care through PEEP titration should be provided. Different methods have been proposed with this goal, for instance, maximization of dynamic compliance that aims to optimize aeration and avoid intermittent alveolar collapse.40 Future studies should test the feasibility of brief intraoperative ‘‘best PEEP trials’’ to analyze the effects of PEEP on compliance and select a preventive PEEP level during surgery for the individual patient.
Strengths and Limitations of the Study
The data used in this study have an observational nature; this could have led to errors and bias in documentation. However, we have no reason to suspect that documentation of postoperative respiratory complications was performed different depending on the level of PEEP that was applied during the procedure. The AIMS did not register use of recruitment maneuvers and we were not able to adjust for this. Patients undergoing major abdominal surgery or craniotomy already have a higher risk on development of post-operative respiratory complications regardless of the application of PEEP. Despite our confounder control, residual confounding is possible because of the observational nature. From our data, we can only conclude on associations between PEEP and postoperative respiratory complications. Randomized controlled trials are needed to write conclusions about a causal relationship.
We excluded patients with respiratory complications (the patients with a lower lung compliance) before the surgical procedure. Furthermore, our dataset contained the median value of PEEP during the procedure. This means that we do not know whether PEEP was applied from the start of the procedure or started later on during the procedure because of hypoxemia. This might be an explanation for the fact that we did not find a beneficial effect of PEEP in patients undergoing craniotomy: physicians might be less likely to apply PEEP to craniotomy patients because of concerns regarding increase of intracranial pressure, and only start with PEEP in high risk patients as a response to adverse events during the procedure.
Upper body position should influence the relationship between PEEP-level and aeration. In our study, the body position differed between surgical procedures and often changed several times during the case, to optimize the surgeon’s view of the surgical field. We are unable to identify which specific aspect of the surgical procedure explains the reported differential effects of PEEP, and differences in body position, retractors, and effects of the surgical procedure itself (diaphragmatic and abdominal wall compression, respiratory muscle trauma, and inflammation) may be contributing.
In summary, our data show that the application of PEEP during intraoperative mechanical ventilation is associated with a significantly lower risk of major postoperative respiratory complications in a large cohort of patients undergoing major abdominal surgery. The preventive effects of PEEP for postoperative respiratory complications are dose-dependent, procedure specific, and translated into decreased hospital length of stay in patients undergoing major abdominal surgeries. Type of surgery should be taken into account when selecting the optimal PEEP value to protect the lungs during intraoperative mechanical ventilation. A PEEP level between 5–10 cmH2O seems to be a reasonable default setting during abdominal surgery.
Supplementary Material
What Is Already Known About This Topic?
Protective mechanical ventilation with lower tidal volumes and PEEP reduces compounded postoperative complications after abdominal surgery. However, a strategy with high intraoperative PEEP (12 cmH2O) with recruitment maneuvers did not differ from a low PEEP (2 cmH2O) strategy in reducing postoperative respiratory complications.
What This Study Tells Us That Is New.
Independent of the effects of plateau pressure, driving pressure, and tidal volume intraoperative application of PEEP ≥5 cmH2O is associated with a lower risk of major postoperative respiratory complications within 3 days after surgery compared with use of PEEP <5 cmH2O. The preventive effect of PEEP for postoperative respiratory complications is dose-dependent, and procedure specific, and translates to decreased hospital length of stay.
ACKNOWLEDGMENTS
We are grateful to Judy and Jeff Buzen for supporting this study.
Disclosure: This study was funded by a grant of Judy and Jeff Buzen to Matthias Eikermann and by NIH grant R01 HL 121228 to Marcos Vidal Melo. This project received approval from the Partners Institutional Review Board, protocol number: 2014P002718. The authors declare no conflict of interest.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372:139–144. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 2.Thompson JS, Baxter BT, Allison JG, et al. Temporal patterns of postoperative complications. Arch Surg. 2003;138:596–602. doi: 10.1001/archsurg.138.6.596. discussion 601–603. [DOI] [PubMed] [Google Scholar]
- 3.Fleischer LA, Linde-Zwirble WT. Incidence, outcome, and attributable resource use associated with pulmonary and cardiac complications after major, small, and large bowel procedures. Periop Med (Lond) 2014;3:7. doi: 10.1186/2047-0525-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawrence VA, Hilsenbeck SG, Mulrow CD, et al. Incidence and hospital stay for cardiac and pulmonary complications after abdominal surgery. J Gen Intern Med. 1995:671–678. doi: 10.1007/BF02602761. [DOI] [PubMed] [Google Scholar]
- 5.Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–341. doi: 10.1097/01.sla.0000179621.33268.83. discussion 341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qaseem A, Snow V, Fitterman N, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients\undergoing non-cardiothoracic surgery: a guideline from the American College of Physicians. Ann Intern Med. 2006:575–580. doi: 10.7326/0003-4819-144-8-200604180-00008. [DOI] [PubMed] [Google Scholar]
- 7.McAlister FA, Bertsch K, Man J. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med. 2005;171:514–517. doi: 10.1164/rccm.200408-1069OC. [DOI] [PubMed] [Google Scholar]
- 8.A Shander, LA Fleisher, PS Barie, et al. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Crit Care Med. 2011;39:2163–2172. doi: 10.1097/CCM.0b013e31821f0522. [DOI] [PubMed] [Google Scholar]
- 9.JM Halter, JM Steinberg, HJ Schiller, et al. Positive end expiratory pressure after a recruitment maneuver prevents both alveolar collapse and recruitment/derecruitment. Am J Respir Crit Care Med. 2003;167:1620–1626. doi: 10.1164/rccm.200205-435OC. [DOI] [PubMed] [Google Scholar]
- 10.AR Carvalho, SA Pacheco, de Souza Rocha PV, et al. Detection of tidal recruitment/overdistension in lung-healthy mechanically ventilated patients under general anesthesia. Anesth Analg. 2013:677–684. doi: 10.1213/ANE.0b013e318254230b. [DOI] [PubMed] [Google Scholar]
- 11.JD Ricard, D Dreyfuss, Saumon G. Production of inflammatory cytokines in ventilator induced lung injury: a reappraisal. Am J Respir Crit Care Med. 2001;163:1176–1180. doi: 10.1164/ajrccm.163.5.2006053. [DOI] [PubMed] [Google Scholar]
- 12.S Uhlig, M Ranieri, Slutsky AS. Biotrauma hypothesis of ventilator-induced lung injury. Am J Respir Crit Care Med. 2004;169:314–315. doi: 10.1164/ajrccm.169.2.950. author reply 315. [DOI] [PubMed] [Google Scholar]
- 13.Y Imai, T Kawano, S Iwamoto, et al. Intratracheal antitumor necrosis factor- a antibody attenuates ventilator-induced lung injury in rabbits. J Appl Physiol. 1999;87:510–515. doi: 10.1152/jappl.1999.87.2.510. [DOI] [PubMed] [Google Scholar]
- 14.PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology. Hemmes SNT, Gama de Abreu M, Pelosi P, et al. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384:495–503. doi: 10.1016/S0140-6736(14)60416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.E Futier, J-M Constantin, C Paugam-Burtz, et al. A trial of intraoperative low-tidal volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–437. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 16.EK Wolthuis, G Choi, MC Dessing, et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology. 2008;108:46–54. doi: 10.1097/01.anes.0000296068.80921.10. [DOI] [PubMed] [Google Scholar]
- 17.K Ladha, Melo MF Vidal, DJ McLean, et al. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ. 2015;351:h3646. doi: 10.1136/bmj.h3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.G Hedenstierna, A Strandberg, B Brismar, et al. Functional residual capacity, thoracoabdominal dimensions, and central blood volume during general anesthesia with muscle paralysis and mechanical ventilation. Anesthesiology. 1985;3:247–254. doi: 10.1097/00000542-198503000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Drummond GB. The abdominal muscles in anaesthesia and after surgery. Br J Anaesth. 2003;91:73–80. doi: 10.1093/bja/aeg145. [DOI] [PubMed] [Google Scholar]
- 20.Wyche MP, Jr, Teichner RL, Kallos T, et al. Effects of continuous positive-pressure breathing on functional residual capacity and arterial oxygenation during intra-abdominal operations: studies in man during nitrous oxide and d-tubocurarine anesthesia. Anesthesiology. 1973:68–74. doi: 10.1097/00000542-197301000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Bensley RP, Schermerhorn ML, Hurks R, et al. Risk of late-onset adhesions and incisional hernia repairs after surgery. J Am Coll Surg. 2013;216:1159–1167. doi: 10.1016/j.jamcollsurg.2013.01.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLean DJ, Diaz-Gil D, Farhan HN, et al. Dose-dependent association between intermediate-acting neuromuscular-blocking agents and postoperative respiratory complications. Anesthesiology. 2015;122:1201–1213. doi: 10.1097/ALN.0000000000000674. [DOI] [PubMed] [Google Scholar]
- 23.Severgnini P, Selmo G, Lanza C, et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–1321. doi: 10.1097/ALN.0b013e31829102de. [DOI] [PubMed] [Google Scholar]
- 24.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 25.Brueckman B, Villa-Uribe JL, Bateman BT, et al. Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology. 2013;118:1276–1285. doi: 10.1097/ALN.0b013e318293065c. [DOI] [PubMed] [Google Scholar]
- 26.Torquato JA, Lucato JJJ, Antunes T, et al. Interaction between intra-abdominal pressure and positive-end expiratory pressure. Clinics. 2009;64:105–112. doi: 10.1590/S1807-59322009000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Futier E. Positive end-expiratory pressure in surgery: good or bad? Lancet. 2014;384:472–474. doi: 10.1016/S0140-6736(14)60894-1. [DOI] [PubMed] [Google Scholar]
- 28.Barbosa FT, Castro AA, de Sousa-Rodrigues CF. Positive end-expiratory pressure (PEEP) during anaesthesia for prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst Rev. 2014;6:CD007922. doi: 10.1002/14651858.CD007922.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brismar B, Hedenstierna G, Lundquist H, et al. Pulmonary densities during anesthesia with muscular relaxation–a proposal of atelectasis. Anesthesiology. 1985:422–428. doi: 10.1097/00000542-198504000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Dos Santos CC, Slutsky AS. The contribution of biophysical lung injury to the development of biotrauma. Annu Rev Physiol. 2006:585–618. doi: 10.1146/annurev.physiol.68.072304.113443. [DOI] [PubMed] [Google Scholar]
- 31.Sinclair SE, Chi E, Lin HI, et al. Positive end-expiratory pressure alters the severity and spatial heterogeneity of ventilator-induced lung injury: an argument for cyclical airway collapse. J Crit Care. 2009;24:206–211. doi: 10.1016/j.jcrc.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wellman TJ, Winkler T, Costa EL, et al. Effect of regional lung inflation on ventilation heterogeneity at different length scales during mechanical ventilation of normal sheep lungs. J Appl Physiol. 2012;113:947–957. doi: 10.1152/japplphysiol.01631.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wellman TJ, Winkler T. Costa EL Effect of local tidal lung strain on inflammation in normal and lipopolysaccharide-exposed sheep*. Crit Care Med. 2014;42:491–500. doi: 10.1097/CCM.0000000000000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arozullah AM, Daley J, Henderson WG, et al. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The national veterans administration surgical Quality improvement program. Ann Surg. 2000;232:242–253. doi: 10.1097/00000658-200008000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bregeon F, Delpierre S, Chetaille B, et al. Mechanical ventilation affects lung function and cytokine production in an experimental model of endotoxemia. Anesthesiology. 2005;102:331–339. doi: 10.1097/00000542-200502000-00015. [DOI] [PubMed] [Google Scholar]
- 36.Verbrugge SJ, Sorm V, van’t Veen A, et al. Lung overinflation without positive end-expiratory pressure promotes bacteremia after experimental Klebsiella pneumoniae inoculation. Intensive Care Med. 1998;24:172–177. doi: 10.1007/s001340050541. [DOI] [PubMed] [Google Scholar]
- 37.Ladha K, Eikermann M. Protective mechanical ventilation during anaesthesia: perioperative implications. J Perioper Med. 2014;1:1–7. [Google Scholar]
- 38.García-Martín C, Villagrá A, Saenz-Valiente A, et al. Effects of vascular flow and PEEP in a multiple hit model of lung injury in isolated perfused rabbit lungs. J Trauma. 2008:147–153. doi: 10.1097/TA.0b013e31813e0904. [DOI] [PubMed] [Google Scholar]
- 39.Sogame LCM, Vidotto MC, Jardim JR, et al. Incidence and risk factors for postoperative pulmonary complications in elective intracranial surgery. J of Neurosurgery. 2008;109:222–227. doi: 10.3171/JNS/2008/109/8/0222. [DOI] [PubMed] [Google Scholar]
- 40.Eikermann M, Kurth T. Apply protective mechanical ventilation in the operating room in an individualized approach to perioperative respiratory care. Anesthesiology. 2015 doi: 10.1097/ALN.0000000000000707. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.