Abstract
Objective
Develop and internally validate a triage score that can identify trauma patients at the scene who would potentially benefit from helicopter emergency medical services (HEMS).
Summary Background Data
Although survival benefits have been shown at the population level, identification of patients most likely to benefit from HEMS transport is imperative to justify the risks and cost of this intervention.
Methods
Retrospective cohort study of subjects undergoing scene HEMS or ground emergency medical services (GEMS) in the National Trauma Databank (2007–2012). Data were split into training and validation sets. Subjects were grouped by triage criteria in the training set and regression used to determine which criteria had a survival benefit associated with HEMS. Points were assigned to these criteria to develop the Air Medical Prehospital Triage (AMPT) score. The score was applied in the validation set to determine if subjects triaged to HEMS had a survival benefit when actually transported by helicopter.
Results
There were 2,086,137 subjects included. Criteria identified for inclusion in the AMPT score included GCS<14, respiratory rate<10 or >29, flail chest, hemo/pneumothorax, paralysis, and multisystem trauma. The optimal cut-off for triage to HEMS was ≥2 points. In subjects triaged to HEMS, actual transport by HEMS was associated with an increased odds of survival (AOR 1.28; 95%CI 1.21–1.36, p<0.01). In subjects triaged to GEMS, actual transport mode was not associated with survival (AOR 1.04; 95%CI 0.97–1.11, p=0.20).
Conclusions
The AMPT score identifies patients with improved survival following HEMS transport and should be considered in air medical triage protocols.
INTRODUCTION
Rapid transport of the patient with severe injury to the highest level of care is a cornerstone of modern trauma care. Delay of trauma care is a well-documented cause of mortality.1 Helicopter emergency medical services (HEMS) have become an important component of trauma care and systems. Although survival benefits have been shown at the population level, selection of patients most likely to benefit from HEMS transport is imperative to justify the risks and cost of this resource intensive intervention.2–6
Prospectively identifying patients that would benefit from HEMS at the scene of injury remains a significant challenge. Many prior investigations evaluating HEMS outcomes exclude patients from study using severity indices not available in the field. Thus, a segment of patients who undergo HEMS transport are systematically excluded and this offers little guidance in selecting appropriate patients for HEMS transport after trauma. Overall, there is inadequate evidence to guide development of standardized HEMS triage criteria, leading to a lack in national HEMS triage guidelines and wide variation among regional criteria and compliance.7, 8
The Centers for Disease Control (CDC) developed the most recent version of the national field triage guidelines (NFTG) to identify patients who should be transported to a trauma center.9 It is not clear, however, that the same criteria used for trauma triage are equally effective in identifying patients that should be flown to a trauma center. Adopting this approach leads to high overtriage and costs, limiting the benefits. Our group previously has demonstrated only a subset of NFTG criteria may be useful for HEMS triage based on improved outcomes; however these were not further validated.10
The American College of Surgeons Committee on Trauma (ACS-COT) also recently authored guidelines that have made research to optimize the use of HEMS a national priority.11 These guidelines cite a lack evidence to guide development of standardized HEMS triage criteria, highlighting the need for work to help policy makers develop specific guidelines for triage criteria and appropriate use of HEMS in trauma.
The objective of this study was to develop and internally validate a simple triage score that can prospectively identify trauma patients at the scene of injury who would potentially benefit from HEMS transport compared to ground emergency medical services (GEMS) transport. The study hypothesis was that a subset of existing trauma triage criteria would predict improved survival associated with HEMS transport and therefore would be useful to incorporate into an air medical triage score for injured patients.
METHODS
Study Population
Subjects aged ≥ 16 years undergoing either HEMS or GEMS transport from the scene of injury in the National Trauma Databank (NTDB) between 2007 and 2012 were eligible for inclusion. The NTDB represents a national database containing over 3 million injured patients from more than 900 hospitals in the US.12 Subjects transferred from another hospital or with isolated burn injury were excluded. Demographics, hospital characteristics, injury severity, vital signs, International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes, intensive care unit (ICU) admission, mechanical ventilation, emergency department (ED) disposition, and hospital disposition were collected for each subject. The study sample was divided by year of admission into a training set (2007–2009) and a validation set (2010–2012).
Missing Data
To address missing data, multiple imputation was performed for analysis variables missing between 5% and 30% of observations. Imputed variables included prehospital systolic blood pressure (SBP), prehospital respiratory rate (RRR, prehospital Glasgow Coma Scale (GCS), prehospital heart rate (HR), and insurance status. Multiple imputation using chained equations with a fully conditional specification model based on available demographics, vital signs, and injury characteristics was performed using five imputation steps to develop five imputed datasets. Outcome models were performed using multiple imputation estimation techniques that combine model coefficients and standard errors from each imputed dataset while adjusting for the variability between imputed datasets.13 Missing data for imputed variables ranged from 12% (insurance status) to 27% (prehospital RR). Imputation procedures were performed separately for the training and validation sets. Sensitivity analyses with complete cases not missing any of the five imputed variables were performed to assess the multiple imputation procedures.
Development of the Air Medical Prehospital Triage (AMPT) score
Available triage criteria from the NFTG and National Association of Emergency Medical Service Physicians air medical dispatch criteria were evaluated for inclusion in the Air Medical Prehospital Triage (AMPT) score.9, 14 Criteria included physiologic parameters (SBP<90mmHg, GCS<14, RR<10 or >29bpm), anatomic injuries (penetrating injury, unstable chest wall, open skull fracture, ≥ 2 proximal long bone fractures, pelvic fracture, crush injury, amputation, paralysis, hemo/pneumothorax, acute cardiac injury, multisystem trauma [>2 body regions injured]), and special considerations (age>55). Combinations of criteria were also considered. Criteria not feasible for field use or that resulted in impractically large proportions of subjects triaged to HEMS transport were omitted from the final AMPT score. Final criteria for potential inclusion in the AMPT score were also presented to prehospital providers for input on feasibility and ease of use for providers in the field.
To be included in the AMPT score, criteria were assessed for improved survival associated with HEMS transport compared to GEMS transport when present. To determine this, subjects were stratified by the presence or absence of each of the individual triage criteria described above. Subjects were then separately analyzed in these strata of individual triage criterion groups. A hierarchical mixed-effects logistic regression model was constructed to determine the independent association of HEMS compared to GEMS transport with in-hospital survival within each individual triage criterion group. Each model included a random effect for centers to account for clustering at the center level and allowed for the possibility that the effect of transport mode on survival may differ between centers. Covariates in the models included gender, race, prehospital heart rate (HR), injury severity score (ISS), Trauma Mortality Prediction Model (TMPM) predicted mortality,15 and trauma center level in addition to controlling for the presence of the remaining triage criteria not defining the individual triage criterion group under analysis. To account for multiple model comparisons for each individual triage criterion group, false discovery rate correction was used. False discovery rate correction is a powerful method to ensure the probability of a type I error remains at the pre-specified level across all hypotheses tested and reports q-values which are false discovery rate adjusted p values.16 These q-values can be interpreted similarly to standard p values, and for this study a q-value ≤ 0.05 was considered statistically significant.
Triage criteria identified from the procedures above in the training set with improved survival for subjects undergoing HEMS transport were included in the AMPT score. Each criterion was assigned a point total based of the relative effect estimate from the adjusted odds ratios (AOR). Each criterion’s AOR was divided by the smallest AOR of the included AMPT criteria to obtain a standardized AOR. This standardized AOR was then rounded to the nearest integer to obtain the point assignment for the AMPT score. Combinations of criteria that potentially contained other AMPT criteria were assigned double points.
Internal validation of the AMPT score
To evaluate the potential utility of AMPT criteria and whether a simple score could be used to predict patients most likely to benefit from HEMS transport, internal validation was performed using the validation set. As predictions made by regression models from the dataset in which they were applied are biased and overly optimistic, internal validation with a separate sample allows evaluation of model performance in patients other than those used for model development within the same underlying population.17 Further, overfitting of regression models may occur, particularly in large samples such as the NTDB, and lead to a poor prognostic model in other populations. Internal validation was used to ensure adequate performance of the AMPT score prior to undertaking a more complex and costly external validation of the score. Point totals for the AMPT score were calculated for each subject in the validation set. All subjects were then triaged to either HEMS or GEMS transport based on AMPT score total points. Various AMPT score point cutoffs were assessed for triage of a subject to HEMS transport, beginning with a cutoff of ≥ 1 points for triage to HEMS.
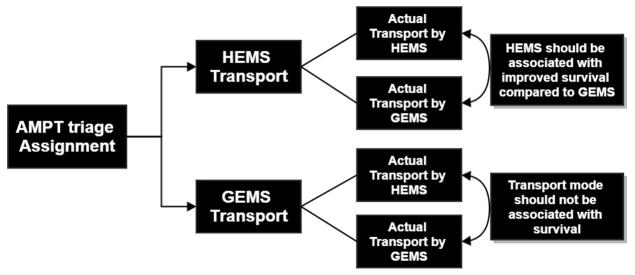
Within each AMPT score triage assignment group (HEMS or GEMS), there were some subjects that actually underwent HEMS transport and some that actually underwent GEMS transport. Validation of the AMPT score was considered successful if both of the following two criteria were met: (1) in the group of subjects triaged to HEMS transport by the AMPT score, actual HEMS transport was independently associated with increased odds of survival, and (2) in the group of subjects triaged to GEMS transport by the AMPT score, actual transport mode was not associated with survival (Fig 1).
Figure 1.
Validation scheme for the Air Medical Prehospital Triage (AMPT) score. For each subject in the validation set, the AMPT score assigned them to either helicopter emergency medical services (HEMS) or ground emergency medical services (GEMS) transport; however within each of these groups, there were some subjects that actually were transported by HEMS and some that were actually transported by GEMS. Successful validation of the score occurred if subjects assigned to HEMS transport by the AMPT score had a significant survival benefit when actually transported by HEMS, while in subjects assigned to GEMS transport by the AMPT score, actual transport mode was not associated with survival.
To evaluate this, similar hierarchical mixed-effect regression models described above were used to determine the association of actual transport mode with in-hospital survival, controlling for age, gender, race, insurance status, prehospital SBP, prehospital HR, prehospital RR, prehospital GCS, ISS, prehospital time, TMPM predicted mortality, and trauma center level across both AMPT score triage assignment groups (HEMS or GEMS). The optimal AMPT point cutoff for determining triage to HEMS transport was considered the lowest single AMPT score point total that resulted in significantly increased odds of survival associated with actual HEMS transport for those triaged to HEMS transport, while actual transport mode remained unassociated with survival for those triaged to GEMS transport.
Subgroup Analysis
There is population of trauma patients injured so close to a trauma center that it would be impractical to transport these patients by HEMS. This group of patients would not have the potential to undergo HEMS transport and it may be less useful to evaluate a triage scoring system for HEMS in these patients. Thus, to capture subjects with the potential to undergo HEMS transport, a subgroup analysis was performed on subjects with a transport time >15 minutes. This transport time cut off was selected as it represents the 25th percentile of HEMS transport time in the validation set. To evaluate the AMPT score in these subjects, the same hierarchical mixed-effects models used in the primary internal validation analysis above were performed.
Statistical Analysis
For univariate comparisons of baseline subject-level characteristics, Chi-square tests were used to compare categorical variables and Wilcoxon rank-sum tests were used to compare continuous variables. A p value ≤ 0.05 was considered significant with 2-sided tests. This study was determined exempt by the Institutional Review Board at the University of Pittsburgh. Data analysis was conducted using STATA version 13 (College Station, TX).
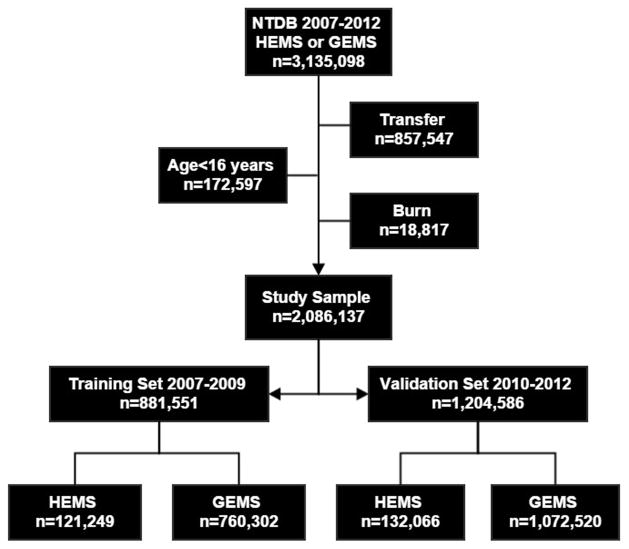
RESULTS
Overall, there were 2,086,137 subjects were included in the study sample, with 12% undergoing HEMS transport (Fig 2). In the training set, HEMS subjects were younger, less likely to have penetrating injury, had higher ISS, and lower unadjusted survival (Table 1). When evaluating complete cases only in the training (N=457,560) and validation (N=792,862) datasets, no differences were seen in criteria included or performance of the AMPT score compared with the imputed datasets. Thus, imputed results are presented below.
Figure 2.
Study participant selection for the training set and validation set of helicopter emergency medical service (HEMS) and ground emergency medical service (GEMS) subjects from the National Trauma Databank 2007–2012.
Table 1.
Characteristics of subjects transported by HEMS and GEMS in the training set (2007–2009)
| HEMS n = 121,424 | GEMS n = 760,302 | p value | |
|---|---|---|---|
| Age [years; med (IQR)] | 38 (24, 52) | 45 (27, 66) | <0.01 |
| Sex [n (%) male] | 86097 (71.1) | 477568 62.9 | <0.01 |
| Insurance Status | <0.01 | ||
| Commercial [n (%)] | 60,532 (49.9) | 308,268 (40.5) | |
| Subsidized/None [n (%)] | 60,892 (50.1) | 452,034 (59.5) | |
| Race [n (%)] | <0.01 | ||
| Caucasian | 100,496 (81.6) | 536,079 (68.3) | |
| Non-Caucasian | 20,928 (18.4) | 224223 (31.7) | |
| Prehospital time [mins; med (IQR)] | 58 (47, 73) | 40 (31, 52) | <0.01 |
| ISS [med (IQR)] | 13 (6, 22) | 9 (4, 13) | <0.01 |
| Age >55 [n (%)] | 24,879 (20.5) | 266,595 (35.1) | <0.01 |
| Prehospital SBP<90mmHg [n (%)] | 6,787 (5.6) | 35,340 (4.6) | <0.01 |
| Prehospital RR<10 or >29bpm [n (%)] | 9,759 (8.0) | 33,901 (4.5) | <0.01 |
| Prehospital GCS≤13 [n (%)] | 32,788 (27.0) | 113,974 (15.0) | <0.01 |
| Penetrating injury [n (%)] | 9,235 (7.6) | 90,486 (11.9) | <0.01 |
| Unstable chest wall fractures [n (%)] | 8,006 (6.9) | 20,171 (2.7) | <0.01 |
| Open skull fracture [n (%)] | 2,376 (2.0) | 7,578 (1.0) | <0.01 |
| ≥2 proximal long bone fractures [n (%)] | 3,297 (2.7) | 11,186 (1.5) | <0.01 |
| Pelvic fracture [n (%)] | 14,716 (12.1) | 51,408 (6.8) | <0.01 |
| Crush injury [n (%)] | 860 (0.7) | 2,932 (0.1) | <0.01 |
| Amputation [n (%)] | 815 (0.7) | 1,116 (0.1) | <0.01 |
| Paralysis [n (%)] | 1,121 (0.9) | 2,198 (0.3) | <0.01 |
| Hemothorax or Pneumothorax [n (%)] | 21,692 (17.9) | 59,605 (7.8) | <0.01 |
| Cardiac injury [n (%)] | 1,270 (1.0) | 5,484 (0.7) | <0.01 |
| Multisystem injury [n (%)] | 1,761 (1.5) | 2,915 (0.4) | <0.01 |
| PHY + ANA injury [n (%)] | 11,598 (9.6) | 40,218 (5.3) | <0.01 |
| Survival [n (%)] | 111,778 (92) | 723,734 (95) | <0.01 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; SBP, systolic blood pressure; RR, respiratory rate; GCS, Glasgow Coma Scale; PHY + ANA, any one physiologic criterion plus any one anatomic criterion
Triage criteria evaluated for inclusion in the AMPT score are listed in Table 2 with the AOR of survival for HEMS compared to GEMS. Of these, eight criteria were identified for which subjects had increased odds of survival if transported by HEMS compared to GEMS (Table 3). The final AMPT score is shown in Table 4 and includes seven of these criteria with operationalized definitions for field use.
Table 2.
Triage criteria evaluated for inclusion in the AMPT score
| Criterion | AOR for Survival HEMS vs GEMS | 95% CI | q-value* |
|---|---|---|---|
| Age >55 | 1.17 | 1.09 – 1.26 | 0.019 |
| GCS <14 | 1.13 | 1.07 – 1.20 | 0.016 |
| SBP <90 | 0.91 | 0.81 – 1.02 | 0.159 |
| RR <10 or >29 | 1.23 | 1.11 – 1.35 | 0.013 |
| Penetrating injury | 1.12 | 0.97 – 1.29 | 0.159 |
| Unstable chest | 1.22 | 1.08 – 1.38 | 0.022 |
| Open skull fracture | 1.17 | 0.99 – 1.38 | 0.112 |
| ≥ 2 proximal long bone fracture | 0.99 | 0.81 – 1.21 | 0.917 |
| Pelvic fracture | 1.04 | 0.95 – 1.14 | 0.535 |
| Crush injury | 1.22 | 0.70 – 2.16 | 0.544 |
| Amputation | 1.07 | 0.73 – 1.57 | 0.764 |
| Paralysis | 1.48 | 1.11 – 1.97 | 0.025 |
| Hemo/pneumothorax | 1.16 | 1.07 – 1.25 | 0.009 |
| Cardiac injury | 0.97 | 0.76 – 1.22 | 0.835 |
| Multisystem trauma† | 1.31 | 1.07 – 1.60 | 0.028 |
| PHY + ANA‡ | 1.27 | 1.18 – 1.36 | 0.003 |
the q-value is the false discovery rate corrected p value for multiple comparisons; q-value ≤ 0.05 considered statistically significant
3 or more anatomic body regions injured
any 1 physiologic criterion plus any 1 anatomic criterion present from American College of Surgeons Committee on Trauma national field triage guidelines
AMPT, air medical prehospital triage; AOR, adjusted odds ratio; HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; 95%CI, 95% confidence interval; GCS, Glasgow Coma Scale; SBP, systolic blood pressure; RR, respiratory rate
Table 3.
Criteria for which patients had improved survival associated with HEMS transport
| Criterion | AOR for Survival HEMS vs GEMS | Standardized AOR |
|---|---|---|
| Age >55 | 1.17 | 1.04 |
| GCS <14 | 1.13 | 1.00 |
| RR <10 or >29 | 1.23 | 1.09 |
| Unstable chest wall | 1.22 | 1.08 |
| Hemo/pneumothorax | 1.16 | 1.02 |
| Paralysis | 1.48 | 1.31 |
| Multisystem trauma* | 1.31 | 1.16 |
| PHY+ANA† | 1.27 | 1.12 |
3 or more anatomic body regions injured
any 1 physiologic criterion plus any 1 anatomic criterion present from American College of Surgeons Committee on Trauma national field triage guidelines
AMPT, air medical prehospital triage; AOR, adjusted odds ratio; HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; 95%CI, 95% confidence interval; GCS, Glasgow Coma Scale; RR, respiratory rate
Age >55 was excluded as it alone resulted in a 54% increase in triage to HEMS, with a 38% greater number of subjects triaged to HEMS than actually underwent HEMS in the validation set. Further analysis of age by decade revealed the survival benefit for HEMS transport was concentrated in older patients with age 56–75 years (AOR 1.10; 95%CI 1.01–1.21, p=0.04), while odds of survival are lower among patients >75 years of age transported by HEMS (AOR 0.86; 95%CI 0.76–0.98, p=0.02). Including a criterion of age 56–75 again alone results in a 25% increase in triage to HEMS. Further, analysis of age<55 as a triage criterion also reveals HEMS is associated with an increase in odds of survival (AOR 1.11; 95%CI 1.04–1.19, p<0.01) in this younger age group. Thus, no specific age criterion appears appropriate for inclusion in the AMPT score.
In the validation set, HEMS subjects were again younger, had more blunt injury, higher ISS, and lower unadjusted survival (Table 5). The optimal cutoff for triage to HEMS transport in the validation set was ≥ 2 points. When using a cutoff of ≥ 2 points for triage to HEMS transport, 9.9% of subjects in the validation set were triaged to HEMS transport by the AMPT score. Of subjects triaged to HEMS transport by the AMPT score, 23.8% actually underwent HEMS transport, while 9.6% of subjects triaged to GEMS by the AMPT score actually underwent HEMS transport.
Table 5.
Characteristics of subjects transported by HEMS and GEMS in the validation set (2010–2012)
| HEMS n = 136,066 | GEMS n = 1,072,520 | p value | |
|---|---|---|---|
| Age [years; med (IQR)] | 40 (25, 55) | 49 (29, 71) | <0.01 |
| Sex [n (%) male] | 93,630 (70.9) | 648,702 (60.5) | <0.01 |
| Insurance Status | <0.01 | ||
| Commercial [n (%)] | 67,666 (51.2) | 422,553 (39.4) | |
| Subsidized/None [n (%)] | 68,400 (48.8) | 649,967(60.6) | |
| Race [n (%)] | <0.01 | ||
| Caucasian | 114,350 (82.9) | 771,087 (70.6) | |
| Non-Caucasian | 21,716 (17.1) | 301,433 (29.4) | |
| Prehospital time [mins; med (IQR)] | 64 (50, 57) | 43 (33, 63) | <0.01 |
| ISS [med (IQR)] | 13 (6, 22) | 9 (4, 11) | <0.01 |
| Age >55 [n (%)] | 31,301 (23.7) | 438,494 (40.9) | <0.01 |
| Prehospital SBP<90mmHg [n (%)] | 7,299 (5.5) | 46,146 (4.3) | <0.01 |
| Prehospital RR<10 or >29bpm [n (%)] | 10,470 (7.9) | 45,888 (4.3) | <0.01 |
| Prehospital GCS≤13 [n (%)] | 35,615 (27.0) | 150,615 (14.0) | <0.01 |
| Penetrating injury [n (%)] | 10,919 (8.3) | 112,413 (10.5) | <0.01 |
| Unstable chest wall fractures [n (%)] | 11,250 (8.5) | 33,178 (3.1) | <0.01 |
| Open skull fracture [n (%)] | 2,959 (2.2) | 10,418 (1.0) | <0.01 |
| ≥ 2 proximal long bone fractures [n (%)] | 3,767 (2.9) | 16,937 (1.6) | <0.01 |
| Pelvic fracture [n (%)] | 15,744 (11.9) | 73,942 (6.9) | <0.01 |
| Crush injury [n (%)] | 816 (0.6) | 3,727 (0.3) | <0.01 |
| Amputation [n (%)] | 884 (0.7) | 1,446 (0.1) | <0.01 |
| Paralysis [n (%)] | 1,279 (1.0) | 2,847 (0.3) | <0.01 |
| Hemothorax or Pneumothorax [n (%)] | 26,099 (19.8) | 86,310 (8.0) | <0.01 |
| Cardiac injury [n (%)] | 1,210 (0.9) | 6,574 (0.6) | <0.01 |
| Multisystem injury [n (%)] | 3,449 (2.6) | 6,881 (0.6) | <0.01 |
| PHY + ANA injury [n (%)] | 12,920 (9.8) | 50,643 (4.7) | <0.01 |
| AMPT triage to HEMS [n (%)] | 28,259 (21.4) | 90,668 (8.5) | <0.01 |
| Survival [n (%)] | 121,494 (92) | 1,023,511 (95) | <0.01 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; SBP, systolic blood pressure; RR, respiratory rate; GCS, Glasgow Coma Scale; PHY + ANA, any one physiologic criterion plus any one anatomic criterion; AMPT, air medical prehospital triage
In subjects triaged to GEMS by the AMPT score (0 or 1 point), actual transport mode was not associated with survival (AOR 1.04; 95%CI 0.97–1.11, p=0.20). In subjects triaged to HEMS by the AMPT score (≥ 2 points), actual transport by HEMS was independently associated with an increased odds of survival (AOR 1.28; 95%CI 1.21–1.36, p<0.01). When evaluating subjects with only 2 points, HEMS transport remained associated with improved survival (AOR 1.34, 95%CI 1.22–1.47, p<0.01).
Evaluation of alternate cutoffs (≥ 1 point, ≥3 points) for triage to HEMS transport demonstrated these cutoffs did not meet criteria for successful validation and confirmed a cutoff of ≥ 2 points as the optimal cutoff. When evaluating a cutoff of ≥ 1 point, subjects triaged to HEMS transport by the AMPT score with only 1 point had no association between actual transport mode and survival (AOR 1.04; 95%CI 0.97–1.12, p=0.26). When evaluating a cutoff of ≥ 3 points, subjects triaged to GEMS transport by the AMPT score had an increase in the odds of survival when actually transported by HEMS (AOR 1.15; 95%CI 1.08–1.22, p<0.01).
In subgroup analysis of subjects with a transport time >15 minutes, using a cutoff of ≥ 2 points to triage subjects to HEMS transport resulted in 8.9% of subjects in the validation set triaged to HEMS transport by the AMPT score. Of subjects triaged to HEMS transport by the AMPT score, 30.0% actually underwent HEMS transport, while 11.3% of subjects triaged to GEMS by the AMPT score actually underwent HEMS transport.
Within the subgroup, subjects triaged to GEMS transport by the AMPT score had no association between transport mode and survival (AOR 1.05; 95%CI 0.98–1.13, p=0.14), while subjects triaged to HEMS by the AMPT score had an increased odds of survival if actual transport was by HEMS (AOR 1.30; 95%CI 1.22–1.40, p<0.01). In subjects from the subgroup analysis triaged to HEMS with only 2 points, actual HEMS transport was also associated with an increased odds of survival (AOR 1.30; 95%CI 1.17–1.45, p<0.01). Alternate cuts of ≥ 1 point and ≥ 3 points again did not meet criteria for successful validation, confirming an optimal cutoff of ≥ 2 points in the subgroup analysis.
DISCUSSION
The current results demonstrate successful development and internal validation of the AMPT score with the ability to discriminate which patients have a survival benefit if transported by HEMS in a large national dataset. Eight triage criteria were found to identify patients with improved survival when undergoing HEMS compared to GEMS transport. Out of these eight criteria, one was not included in the final AMPT score. Age >55 years was omitted as its inclusion resulted in an over 50% increase in triage to HEMS transport, with more patients being triaged to HEMS than were actually transported by HEMS in the study population. This is not feasible from a resource allocation standpoint and defeats the purpose of developing a triage tool to selectively identify patients most likely to benefit from HEMS transport. Further analyses of age groups reveal survival benefits for HEMS transport in patients ≤ 75 years, while survival appears lower in those older than 75 years, similar to findings from other groups.18 Thus, rather than including a specific age criterion, it may be more appropriate to consider applying the AMPT score only in patients ≤ 75 years, while those >75 years undergo ground transport. However, these age analyses are exploratory and require further directed study to establish what, if any, age range restriction may be appropriate for HEMS transport after trauma.
The seven criteria included in the AMPT score are feasible for field use by prehospital personnel. A primary goal for the AMPT score was to develop a tool that is simple and can be rapidly deployed by minimally trained first responders. These criteria are identifiable in the field given the limited resources in the prehospital environment, and prehospital personnel are familiar with them as they represent a subset existing trauma triage criteria. Patients with an AMPT score of ≥ 2 had improved survival if transported by HEMS, whereas in those with a score of 0 or 1 transport mode did not impact survival. The survival benefit of HEMS transport in those triaged to HEMS by the AMPT score persisted even when evaluating only subjects with only 2 points in the AMPT score. The AMPT score also performed similarly well when restricting the analysis to subjects with longer transport times who would have the potential to undergo HEMS transport. This score may prospectively identify patients most likely to benefit from HEMS transport following injury.
Recent evidence has demonstrated significant survival benefits for patients with trauma transported by helicopter at the population level. Our group demonstrated a significant survival benefit at the national level, finding HEMS patients transported from the scene of injury had a 22% increase in the odds of in-hospital survival compared to GEMS patients.4 Our findings were confirmed by Sullivent et al, finding a 39% reduction in the odds of in-hospital mortality among HEMS patients transported to a level I or II trauma center in the National Sample Program from the NTDB.6 Stewart et al also found a 33% reduction in the odds of in-hospital mortality in a state database after controlling for the likelihood of helicopter transport.19 More recently Galvagno and colleagues used propensity score matching in patients with an ISS>15, demonstrating a 16% increase in the odds of survival nationally among HEMS patients transported to a level I or II trauma center.5
Despite this, the risks and resources associated with HEMS transport make patient selection paramount. Concerns about aviation safety, cost, and over-triage have led to questions about the role of HEMS in trauma.2, 3, 20 Some have documented between 50% and 60% of HEMS transports are for patients ultimately determined to have minor injuries and may be unnecessary at a cost of $4,000–$5,000 per transport.3, 21, 22 Operating costs for HEMS programs may be as high as $1,500 per hour. Further, although both ground and helicopter providers are at increased risk of injury from crashes, HEMS accidents have a substantially higher risk of death with a rate of 0.86 fatalities per accident.2, 23
Several studies have failed to demonstrate survival benefits associated with HEMS transport of trauma patients.24–28 While these studies have a number of limitations, they highlight the need for HEMS triage and appropriate patient selection. Undoubtedly in the studies reporting a survival benefit for HEMS transport, not every patient is benefiting from this intervention, particularly when looking at large national cohorts. The survival benefit of HEMS transport is likely driven by some combination of speed, advanced crew capabilities and experience, and trauma center access.29 However, prospectively identifying patients that would benefit from these elements of HEMS transport using criteria available at the scene of injury is difficult. As a consequence, there is wide variation among regional criteria, compliance with local guidelines, and significant use of providers’ discretion in utilizing HEMS transport.7, 8, 30
Trauma triage and air medical triage address fundamentally different questions. The former seeks to determine what level of care the injured patient requires and helps to identify those that would benefit from transport to a trauma center. The latter seeks to identify those patients requiring a trauma center that would benefit from HEMS transport. Many patients may benefit from trauma center care without requiring the resources of HEMS. In other words, needing to go to a trauma center is not the same as needing to fly to a trauma center. It is imperative to recognize this distinction to optimize the use of HEMS. Adopting existing triage guidelines for air medical triage without modification, as many trauma systems have, leads to high over-triage and costs, limiting the benefits conferred by HEMS. Studies that demonstrate significant benefits for HEMS transport in trauma also report high rates of over-triage. A recent analysis reported HEMS needs to save between 1–3 lives per 100 transports with current utilization patterns to be a cost effective intervention.21
Thus, identifying patients most likely to benefit becomes paramount. Despite this, few studies have evaluated air medical triage in trauma. A review article in 2009 found only five studies of low to moderate quality specifically addressing this issue and was unable to draw any substantial conclusions, noting only an altered level of consciousness may be valuable in identifying trauma patients for HEMS transport.7 Our group previously evaluated the NFTG using a similar method as the current study, finding 5 criteria that, when present, were associated with a survival benefit for HEMS transport.10 Patients were similarly sub-grouped according to the presence of physiologic and anatomic NFTG criteria and survival was determined within each triage criterion group for HEMS compared to GEMS transport. Criteria that had a survival benefit associated with HEMS transport in that study included age >55 years, GCS<14, RR<10 or >29 breaths per minute, penetrating injury, and the presence of any one of the NFTG physiologic triage criteria plus any one of the NFTG anatomic triage criteria. All criteria but penetrating injury from our prior study were identified in the current data. This study represents a more robust extension of our prior work in an attempt to validate evidence based criteria for air medical triage in trauma.
Recently, multiple stakeholder agencies attempted to develop an evidence based guideline for air medical transport of trauma patients using Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology.31 This effort was hampered by very low quality evidence, but made the recommendation that trauma patients meeting any physiologic or anatomic triage criteria from the NFTG should be considered for HEMS transport. However, our group’s prior work and the current study demonstrate only a subset of the physiologic and anatomic NFTG criteria have improved survival associated with HEMS transport. While the NFTG criteria continue to be important in determining patient destination, a more selective application of evidence-based criteria for determining patient transport method based on improved outcomes appears warranted to reduce unnecessary cost and risk. Thus, efforts such as the current analysis are essential to help identify the optimal population of trauma patients most likely to benefit from HEMS transport and inform future guidelines and policy.
This work does have several limitations. First are those of a retrospective design. Second are those outlined by American College of Surgeons Committee on Trauma for use of the NTDB.12 Although the NTDB data quality has improved substantially, high levels of missing data persist, particularly in prehospital variables. Multiple imputation was used to mitigate this and has been validated in this database previously.32, 33 No significant differences were seen for outcomes in sensitivity analysis using complete cases only, engendering confidence in the imputed results presented here to maintain statistical power. The NTDB is not a population-based dataset and skewed towards large trauma centers.34 There were limited variables for analysis which precluded us from evaluating mechanism of injury criteria as potential triage criteria for inclusion in the score; however previous studies suggest these criteria perform poorly overall for identifying severely injured patients that may benefit from HEMS transport.35, 36 Anatomic criteria were derived from ICD-9 codes and it is unclear how reliable evaluation of these criteria are in the field based on the current data. We have operationalized these criteria for the final AMPT score here; however prospective study is necessary to ensure these criteria are identified in the field reliably and continue to be useful for HEMS triage. There is inevitable selection bias for allocating patients to HEMS or GEMS transport, and it is impossible to fully evaluate all of the factors that resulted in individual transport decisions in a dataset such as this. We did, however, take advantage of this situation to evaluate survival benefits based on actual transport mode compared to the AMPT allocated transport mode. Internal validation was used to evaluate the potential performance of the AMPT score outside the training set from which it was derived; however the same biases and limitations of the training set are present in the validation set. Despite this, we believe internal validation is a necessary first step. First, it demonstrated the AMPT score is potentially useful to predict patients who are most likely to benefit from HEMS in the same underlying population. Although the noted limitations of the dataset exist, the underlying population is a national sample of trauma patients and lends itself to generalizability. Further, since this represents the first attempt to develop a triage tool for HEMS transport in trauma, there is little to compare performance against and can serve as a benchmark for further validation. Thus, the internal validation here is necessary to establish preliminary data and justify the expense and efforts to move forward with a prospective evaluation of the AMPT score to evaluate external validity in different settings and populations.
Other important outcomes such as health related quality of life are not available, but remain important outcomes to evaluate in severely injured trauma patients. Further, we cannot explore the underlying mechanisms that may drive the outcome benefits seen here. Finally, it is important to distinguish that the AMPT score is for use in HEMS transport decisions and not necessarily helicopter dispatch or launch decisions.
Importantly, this score does not take into account logistical factors such as time, distance, and availability of transport resources, which also play a crucial role in the decision to use HEMS.7, 14, 37 These factors may not be amenable to evaluation using traditional outcomes measures such as improved survival. We did, however, find similar performance of the AMPT score in our subgroup of patients with longer transport times. Additionally, both the capabilities of GEMS providers and availability of these resources influence the role of HEMS in individual trauma systems. HEMS crews frequently provide a higher level of care than GEMS crews. HEMS providers may be trained and authorized to perform potentially lifesaving interventions such as rapid sequence intubation, surgical cricothyroidotomy, or blood product administration that GEMS providers cannot. Moreover, greater exposure to severely injured patients among HEMS providers may confer a volume-outcome benefit. All of these factors must be considered in HEMS triage guidelines. Thus the AMPT score does not provide a comprehensive approach to HEMS triage. It does, however, provide the first evidence based set of patient-level criteria that can be utilized as a starting point for developing tailored air medical triage guidelines within individual trauma systems.
CONCLUSION
This study represents a novel approach with the largest and most robust evaluation of air medical triage criteria for trauma. The AMPT score is feasible for field use and can identify patients with improved outcomes following HEMS transport, targeting patients most likely to benefit from this resource following injury. The AMPT score directly addresses the need for developing standardized HEMS triage criteria raised by the ACS-COT and may help focus future study in this area. These findings warrant prospective validation of the AMPT score in further investigation. The AMPT score should be considered in conjunction with logistical and individual system factors when developing protocols for utilization of HEMS in the scene transport of injured patients.
Table 4.
Air Medical Prehospital Triage (AMPT) Score
| Criterion | Points |
|---|---|
| Glasgow Coma Scale <14 | 1 |
| Respiratory Rate <10 or >29 breaths/min | 1 |
| Unstable chest wall fractures* | 1 |
| Suspected hemothorax or pneumothorax† | 1 |
| Paralysis | 1 |
| Multisystem trauma ‡ | 1 |
| PHY+ANA § | 2 |
|
| |
| Consider helicopter transport if AMPT score ≥ 2 points | |
Any chest wall instability or deformity including flail chest or multiple ribs fractures on physical exam
Absence of breath sounds on affected hemithorax PLUS objective signs of respiratory distress (cyanosis, SpO2<92%, signs of tension physiology)
3 or more anatomic body regions injured
any 1 physiologic criterion plus any 1 anatomic criterion present from American College of Surgeons Committee on Trauma national field triage guidelines
Acknowledgments
Funding/Support: No funding or support was directly received to perform the current study. Dr. Brown receives support from an institutional T32 Ruth L. Kischstein National Research Service Award training grant (5T32GM008516-20) and L30GM112034 from the National Institutes of Health. Dr. Sperry receives support from a career development award (K23GM093032) from the National Institute of General Medical Sciences.
Committee on Trauma, American College of Surgeons. NTDB 2007–2012, Chicago, IL. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables, or figures.
Contributor Information
Joshua B. Brown, Email: brownjb@upmc.edu.
Mark L. Gestring, Email: mark_gestring@urmc.rochester.edu.
Francis X. Guyette, Email: guyefx@upmc.edu.
Matthew R. Rosengart, Email: rosengartmr@upmc.edu.
Nicole A. Stassen, Email: nicole_stassen@urmc.rochester.edu.
Raquel M. Forsythe, Email: forsytherm@upmc.edu.
Timothy R. Billiar, Email: billiartr@upmc.edu.
Andrew B. Peitzman, Email: peitzmanab@upmc.edu.
Jason L. Sperry, Email: sperryjl@upmc.edu.
References
- 1.Sampalis JS, Denis R, Lavoie A, et al. Trauma Care Regionalization: A Process-Outcome Evaluation. The Journal of Trauma and Acute Care Surgery. 1999;46:565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bledsoe BE, Smith MG. Medical Helicopter Accidents in the United States: A 10-Year Review. The Journal of Trauma: Injury, Infection, and Critical Care. 2004;56:1325–1329. doi: 10.1097/01.ta.0000109001.35996.af. [DOI] [PubMed] [Google Scholar]
- 3.Bledsoe BE, Wesley AK, Eckstein M, et al. Helicopter scene transport of trauma patients with nonlife-threatening injuries: a meta-analysis. J Trauma. 2006;60:1257–65. doi: 10.1097/01.ta.0000196489.19928.c0. discussion 1265–6. [DOI] [PubMed] [Google Scholar]
- 4.Brown JB, Stassen NA, Bankey PE, et al. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–4. doi: 10.1097/TA.0b013e3181f6f450. discussion 1034–6. [DOI] [PubMed] [Google Scholar]
- 5.Galvagno SM, Jr, Haut ER, Zafar SN, et al. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307:1602–10. doi: 10.1001/jama.2012.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care. 2011;15:295–302. doi: 10.3109/10903127.2011.569849. [DOI] [PubMed] [Google Scholar]
- 7.Ringburg AN, de Ronde G, Thomas SH, et al. Validity of helicopter emergency medical services dispatch criteria for traumatic injuries: a systematic review. Prehosp Emerg Care. 2009;13:28–36. doi: 10.1080/10903120802472012. [DOI] [PubMed] [Google Scholar]
- 8.Tiamfook-Morgan TO, Kociszewski C, Browne C, et al. Helicopter scene response: regional variation in compliance with air medical triage guidelines. Prehosp Emerg Care. 2008;12:443–50. doi: 10.1080/10903120802290794. [DOI] [PubMed] [Google Scholar]
- 9.Sasser SM, Hunt RC, Faul M, et al. Guidelines for Field Triage of Injured Patients. MMWR. 2012;61:1–20. [PubMed] [Google Scholar]
- 10.Brown JB, Forsythe RM, Stassen NA, et al. The National Trauma Triage Protocol: can this tool predict which patients with trauma will benefit from helicopter transport? J Trauma Acute Care Surg. 2012;73:319–25. doi: 10.1097/TA.0b013e3182572bee. [DOI] [PubMed] [Google Scholar]
- 11.Doucet J, Bulger E, Sanddal N, et al. Appropriate use of helicopter emergency medical services for transport of trauma patients: guidelines from the Emergency Medical System Subcommittee, Committee on Trauma, American College of Surgeons. J Trauma Acute Care Surg. 2013;75:734–41. doi: 10.1097/TA.0b013e3182a5389e. [DOI] [PubMed] [Google Scholar]
- 12.American College of Surgeons. National Trauma Databank Research Data Set Admission Year 2012. Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 13.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 1987. [Google Scholar]
- 14.Thomson DP, Thomas SH. Guidelines for air medical dispatch. Prehosp Emerg Care. 2003;7:265–71. doi: 10.1080/10903120390936923. [DOI] [PubMed] [Google Scholar]
- 15.Glance LG, Osler TM, Mukamel DB, et al. TMPM-ICD9: a trauma mortality prediction model based on ICD-9-CM codes. Ann Surg. 2009;249:1032–9. doi: 10.1097/SLA.0b013e3181a38f28. [DOI] [PubMed] [Google Scholar]
- 16.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Statist Soc B. 1995;57:289–300. [Google Scholar]
- 17.Altman DG, Royston P. What do we mean by validating a prognostic model? Statist Med. 2000;19:453–473. doi: 10.1002/(sici)1097-0258(20000229)19:4<453::aid-sim350>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 18.Werman HA, Cudnik MT, Subrahmanyam D, et al. [Accessed July 2, 2015];Do Trauma Pts Age 55 Older Benefit From Air Medical Transport? Available at: http://www.publicsafety.ohio.gov/links/ems_OSU%20Final%20Report_Do%20Trauma%20Pts%20Age%2055%20%20Older%20Benefit%20From%20Air%20Medical%20Transport.pdf.
- 19.Stewart KE, Cowan LD, Thompson DM, et al. Association of direct helicopter versus ground transport and in-hospital mortality in trauma patients: a propensity score analysis. Acad Emerg Med. 2011;18:1208–16. doi: 10.1111/j.1553-2712.2011.01207.x. [DOI] [PubMed] [Google Scholar]
- 20.Habib FA, Shatz D, Habib AI, et al. Probable cause in helicopter emergency medical services crashes: What role does ownership play? J Trauma Acute Care Surg. 2014;77:989–93. doi: 10.1097/TA.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 21.Delgado MK, Staudenmayer KL, Wang NE, et al. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62:351–364. e19. doi: 10.1016/j.annemergmed.2013.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung BH, Delgado MK, Staudenmayer KL. Patient and Trauma Center Characteristics Associated With Helicopter Emergency Medical Services Transport for Patients With Minor Injuries in the United States. Acad Emerg Med. 2014;21:1232–1239. doi: 10.1111/acem.12512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Highway Traffic Safety Administration. [Accessed April 4th, 2015];NHTSA and Ground Ambulance Crashes 2014. Available at: http://www.ems.gov/pdf/GroundAmbulanceCrashesPresentation.pdf.
- 24.Brathwaite CE, Rosko M, McDowell R, et al. A critical analysis of on-scene helicopter transport on survival in a statewide trauma system. J Trauma. 1998;45:140–4. doi: 10.1097/00005373-199807000-00029. discussion 144–6. [DOI] [PubMed] [Google Scholar]
- 25.Bulger EM, Guffey D, Guyette FX, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2012;72:567–73. doi: 10.1097/TA.0b013e31824baddf. discussion 573–5; quiz 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cunningham P, Rutledge R, Baker CC, et al. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma. 1997;43:940–6. doi: 10.1097/00005373-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Schiller WR, Knox R, Zinnecker H, et al. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma. 1988;28:1127–34. doi: 10.1097/00005373-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Shatney CH, Homan SJ, Sherck JP, et al. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma system. J Trauma. 2002;53:817–22. doi: 10.1097/00005373-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Galvagno SM., Jr Comparative effectiveness of helicopter emergency medical services compared to ground emergency medical services. Crit Care. 2013;17:169. doi: 10.1186/cc12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wigman LD, van Lieshout EM, de Ronde G, et al. Trauma-related dispatch criteria for Helicopter Emergency Medical Services in Europe. Injury. 2011;42:525–33. doi: 10.1016/j.injury.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 31.Thomas SH, Brown KM, Oliver ZJ, et al. An Evidence-based Guideline for the air medical transportation of prehospital trauma patients. Prehosp Emerg Care. 2014;18(Suppl 1):35–44. doi: 10.3109/10903127.2013.844872. [DOI] [PubMed] [Google Scholar]
- 32.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Coll Surg. 2012;214:756–68. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore L, Hanley JA, Lavoie A, et al. Evaluating the validity of multiple imputation for missing physiological data in the national trauma data bank. J Emerg Trauma Shock. 2009;2:73–9. doi: 10.4103/0974-2700.44774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore L, Hanley JA, Turgeon AF, et al. A multiple imputation model for imputing missing physiologic data in the national trauma data bank. J Am Coll Surg. 2009;209:572–9. doi: 10.1016/j.jamcollsurg.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 35.Wuerz R, Taylor J, Smith JS. Accuracy of trauma triage in patients transported by helicopter. Air Med J. 1996;15:168–70. doi: 10.1016/s1067-991x(96)90025-5. [DOI] [PubMed] [Google Scholar]
- 36.Coats TJ, Wilson AW, Cross FW. On-scene medical decision making and overtriage. Br J Surg. 1993;80:1291–3. doi: 10.1002/bjs.1800801023. [DOI] [PubMed] [Google Scholar]
- 37.Air Medical Physicians Association. [Accessed Jan 13, 2015];Appropriate and Safe Utilization of Helicopter Emergency Medical Services. 2012 Available at: https://ampa.org/node/64.