Abstract
Purpose:
The introduction of a High-Resolution (Hi-Res) scan mode and another associated option that combines Hi-Res mode with the so-called High Definition (HD) reconstruction kernels (referred to as a Hi-Res/HD mode in this paper) in some multi-detector CT (MDCT) systems offers new opportunities to increase spatial resolution for some clinical applications that demand high spatial resolution. The purpose of this work was to quantify the in-plane spatial resolution along both the radial direction and tangential direction for the Hi-Res and Hi-Res/HD scan modes at different off-center positions.
Methods:
A technique was introduced and validated to address the signal saturation problem encountered in the attempt to quantify spatial resolution for the Hi-Res and Hi-Res/HD scan modes. Using the proposed method, the modulation transfer functions (MTFs) of a 64-slice MDCT system (Discovery CT750 HD, GE Healthcare) equipped with both Hi-Res and Hi-Res/HD modes were measured using a metal bead at nine different off-centered positions (0–16 cm with a step size of 2 cm); at each position, both conventional scans and Hi-Res scans were performed. For each type of scan and position, 80 repeated acquisitions were performed to reduce noise induced uncertainties in the MTF measurements. A total of 15 reconstruction kernels, including eight conventional kernels and seven HD kernels, were used to reconstruct CT images of the bead. An ex vivo animal study consisting of a bone fracture model was performed to corroborate the MTF results, as the detection of this high-contrast and high frequency task is predominantly determined by spatial resolution. Images of this animal model generated by different scan modes and reconstruction kernels were qualitatively compared with the MTF results.
Results:
At the centered position, the use of Hi-Res mode resulted in a slight improvement in the MTF; each HD kernel generated higher spatial resolution than its counterpart conventional kernel. However, the MTF along the tangential direction of the scan field of view (SFOV) was significantly degraded at off-centered positions, yet the combined Hi-Res/HD mode reduced this azimuthal MTF degradation. Images of the animal bone fracture model confirmed the improved spatial resolution at the off-centered positions through the use of the Hi-Res mode and HD kernels.
Conclusions:
The Hi-Res/HD scan improve spatial resolution of MDCT systems at both centered and off-centered positions.
Keywords: spatial resolution, MDCT, PSF, MTF, reconstruction kernel, off-center, patient positioning
1. INTRODUCTION
Given the fact that divergent beam acquisition systems are used in modern medical CT scanners, it is difficult to achieve uniform spatial resolution and noise distribution across the entire scan field of view (FOV), although the variation of spatial resolution and noise from iso-center to peripheral locations is mitigated by the introduction of the so-called fan-parallel data rebinning technique before image reconstruction is performed.1 In fact, several previous studies have demonstrated that off-centering of an image object may lead to significant degradation in spatial resolution and elevation in image noise.2–5 Due to the degradation in image quality, off-centering of an image object may generate nondiagnostic images or force the exam to be prescribed with an increased x-ray exposure to compensate for the increase of image noise, which results in an increase of radiation dose to the patients. Therefore, whenever possible, it is recommended that the anatomy of interest should be placed as close to the iso-center of the scan field of view as possible.
However, for some clinical CT exams, patients must be positioned at an off-center position due to certain practical constraints. For example, in elbow CT exams, the presence of the head and shoulder often prevents the elbow to be placed at the iso-center. Another example is the body CT exams for some large patients, where the patient couch needs to be significantly lowered in order to fit the torso into the scanner. For these specific clinical applications, it is desirable to have technical solutions to address the potential loss of spatial resolution at peripheral locations where the target of clinical interest may be forced to locate in the FOV. The introduction of high-resolution (Hi-Res) and Hi-Res/high definition (HD) modes provides a potential solution to compensate for the spatial resolution loss at peripheral regions of the scan FOV in the non-Hi-Res scan modes, particularly for those clinical cases where patient off-centering is inevitable. However, quantitative characterization must be performed to understand how much improvement in spatial resolution can be achieved in the Hi-Res and Hi-Res/HD scan modes.
This paper concerns spatial resolution quantification of a newly introduced high-resolution (Hi-Res) CT scan mode (Hi-Res, GE Healthcare, Waukesha, WI), which was claimed to improve spatial resolution and reduce view angle aliasing artifacts. Higher in-plane resolution can be obtained by doubling the in-plane spatial sampling. The Discovery CT750 HD system can achieve this by the use of customized hardware (x-ray tube and voltage generator) that allows in-plane focal spot deflection. In order to leverage this increased sampling capability, a customized detector and digital acquisition system is also required in order to provide a proportionally fast electronic sampling rate.6–9 The Hi-Res scan mode was accompanied by a set of High Definition (HD) reconstruction kernels that are specifically designed for this Hi-Res scan mode; meanwhile, all of the conventional reconstruction kernels offered by the previous models of GE CT systems are still compatible with the Hi-Res mode. As a result, the Hi-Res scan mode can be either combined with the conventional reconstruction kernel (it is referred to as Hi-Res modes throughout the remainder part of the paper) or the HD kernel (it is referred to as Hi-Res/HD mode in this paper).
Unlike the quantification of spatial resolution in other conventional scan modes, a straightforward procedure to measure spatial resolution of Hi-Res and Hi-Res/HD modes encounters some technical challenges: both Hi-Res and Hi-Res/HD mode generated images of metallic beads used in high contrast spatial resolution measurements with CT numbers that are beyond the allowed highest threshold of some scanners (+3071 HU). As a result, line profiles through high contrast objects commonly used for spatial resolution measurements are truncated (Fig. 1). Therefore, some new technical innovations are needed to quantitatively measure spatial resolution in Hi-Res and Hi-Res/HD mode. In this paper, such a new technical solution is presented and validated to enable the measurement of spatial resolution for the Hi-Res and Hi-Res/HD scan modes.
FIG. 1.
Two-dimensional profiles of the tungsten carbide bead measured from CT images reconstructed using the HD Edge kernel. (a) When the CT image was reconstructed with a thin (0.625 mm) slice thickness, the signal of the bead was truncated beyond the maximum HU (+3071) allowed in some scanners. (b) When the image was reconstructed with a thicker (2.5 mm) slice thickness, signal truncation was avoided due to the partial volume averaging effect.
Note that a complete characterization of image quality of the Hi-Res and Hi-Res/HD scan mode will need to invoke a comprehensive evaluation of spatial resolution, noise characteristics, and the specific imaging tasks. We plan to fully address the image quality evaluation problem with Hi-Res and Hi-Res/HD modes in two consecutive papers: this first paper focuses on the spatial resolution measurements and quantification due to the needed technical innovations to make the measurements. The planned second paper will focus on the noise power spectral studies and the imaging task based performance quantification.
2. METHODS AND MATERIALS
2.A. Technical challenges encountered in the measurement of Modulation Transfer Function (MTF) for the Hi-Res and Hi-Res/HD scan modes
Compared with the conventional CT scan modes and reconstruction kernels, the Hi-Res scan mode and the HD reconstruction kernels imposed new changes in MTF measurements. First, the potential edge enhancement introduced by this method may boost the signal of a high contrast MTF test object above the maximum Hounsfield unit (HU) supported by the CT system. As a result of this signal truncation, the continuity of the measured object profile is disrupted (Fig. 1), leading to inaccurate MTF measurement results. Although some scanners offer the “extended CT number” (or extended HU) mode to extend the maximum HU (e.g., to 31 743), not all scanner model or scan mode supports this mode. Second, spatial resolution improvement is usually accompanied by a significant increase of image noise which adds statistical uncertainty to the experimental measurements of MTF (Fig. 2). While the x-ray exposure level can be increased to reduce noise, it cannot be arbitrarily increased due to the limited power rating of the x-ray generator-tube assembly. Although a low-pass filter can be applied to reduce noise, it may introduce distortion to the MTF and thus is not an ideal solution.
FIG. 2.
CT images of the bead reconstructed using the HD Bone plus kernel before (a) and after (b) ensemble averaging (80 repetitions). The measured MTF curves based on these two cases are shown in (c).
2.B. Technical solutions proposed in this paper
To address the first challenge (i.e., signal truncation), a small high contrast metal tungsten carbide bead (diameter ⊘ = 0.18 mm) inside a commercially available CT Catphan phantom (Catphan 600, The Phantom Laboratory, Greenwich, NY) was used for the MTF measurement. To avoid signal truncation, CT images of this bead were reconstructed with a relatively thick slice (2.5 mm), which allowed the partial-volume averaging effect to significantly reduce the signal magnitude of the bead (Fig. 1).
To illustrate the proposed two-dimensional (2D) MTF measurement method using images with a thick slice-thickness, a brief review of the canonical method to measure both three-dimensional (3D) point spread function (PSF) and the corresponding 3D MTF is beneficial. Mathematically speaking, the measured 3D profile of the bead, Im(x, y, z), is related to the true profile of the bead, I(x, y, z), and the 3D PSF of the CT system, PSF(x, y, z) as the following:
| (1) |
where *** denotes the 3D convolution operator.
If the bead is made of a uniform material and is sufficiently small compared with the spatial resolving capability (i.e., spatial resolution) of the CT imaging system, I(x, y, z) can be approximated as
| (2) |
where μ is the x-ray attenuation coefficient of the bead, V is the geometrical volume of the bead and (x0, y0, z0) is the position of the center of the bead. With this approximation, the measured signal becomes
| (3) |
This equation lays the foundation for the MTF measurement in CT systems: using high contrast and sufficiently small object as the test object to obtain the image of the bead and approximately used it as the 3D point spread function. A Fourier transform of the obtained 3D PSF can then be taken to extract the needed MTF curves of the MDCT systems.
For MDCT systems, the use of multirow detectors and a row-wise filtration in image reconstruction allow one to decouple the z-dependence, i.e., PSF(z), from the axial dependence, i.e., PSF(x, y), when image data is acquired in axial mode, namely,
| (4) |
When Eq. (3) is combined with Eq. (4), the profile of the bead in a CT image with a slice thickness of Δz is then given by
| (5) |
where we used when Δz is sufficiently large. As a result,
| (6) |
Using the normalization condition of the in-plane point spread function [i.e., 1 = ∫∫dxdyPSF(x, y)] and integrating both sides of Eq. (6), the following condition is obtained:
| (7) |
Assuming that the bead is centered in the reconstruction FOV, i.e. (x0, y0) = (0, 0), and combining Eqs. (6) and (7), the PSF results to be
| (8) |
This equation lays the foundation of method used in this paper to measure 2D point spread function from images of thick slice-thickness.
In summary, as long as (1) the test object is sufficiently small and (2) the axial spatial resolution can be decoupled from the z resolution, thick slice reconstruction can still be used to accurately measure the axial PSF (and thus MTF) despite partial volume averaging.
To address the second challenge in MTF measurements encountered in Hi-Res scans, i.e., noise elevation in Hi-Res and Hi-Res/HD scan modes, multiple CT acquisitions (80 times) were performed at each scan mode and system setting. The resulting ensemble of CT images were averaged to reduce noise in the CT image, which significantly improved the reliability of the MTF measurements (Fig. 2).
2.C. Phantom setup and CT acquisition methods
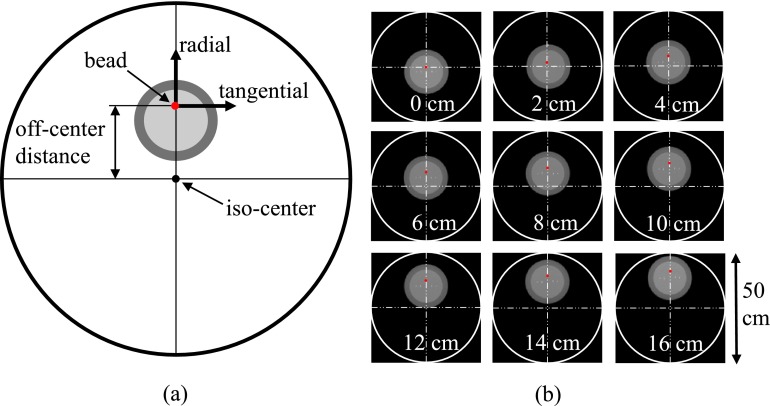
A 64-slice clinical MDCT system (Discovery CT750 HD, GE Healthcare, Waukesha, WI) equipped with the Hi-Res and Hi-Res/HD modes was used in this study. A total of eight reconstruction kernels are available for the conventional scan mode, while seven additional HD kernels are provided for the Hi-Res scan mode (Table I). The bead used in this study was located in Module CTP591 of the Catphan 600 phantom. The material surrounding the bead is similar to water in terms of x-ray attenuation properties. The bead was positioned at nine different locations (0, 2, 4, 6, 8, 10, 12, 14 and 16 cm away from the iso-center of the scanner, as shown in Fig. 3) within the scan field of view (SFOV) to study the impact of off-centering on the MTF. At each position and scan mode, 80 repeated axial scans were performed. Other acquisition parameters are listed as follows: 120 kV, 800 mAs, small focal spot (1.0 × 0.7 mm), large bowtie filter, and 20 mm detector collimation width. The acquired data were reconstructed using a slice thickness of 2.5 mm, 50 mm display FOV, and 512 × 512 image matrix. After ensemble averaging of the 80 repeated scans, the image was subtracted by the mean CT number of the background material surrounding the bead, then the image was normalized as described in Eq. (8) to obtain the two-dimensional (2D) PSF. The 2D MTF was obtained by taking the 2D digital Fourier transform of the 2D PSF. The discrete sampling interval in the spatial domain and frequency domain is 0.098 mm and 0.020 mm−1, respectively.
TABLE I.
Scan modes and the associated reconstruction kernels provided by the Discovery CT750 HD CT system.
| Conventional mode | Hi-Res mode | ||
|---|---|---|---|
| non-HD kernels | HD kernels | non-HD kernels | HD kernels |
| Soft | Soft | HD Standard | |
| Standard | Standard | HD Detail | |
| Detail | Detail | HD Lung | |
| Lung | Lung | HD Bone | |
| Chest | Chest | HD Bone plus | |
| Bone | Bone | HD Ultra | |
| Bone plus | Bone plus | HD Edge | |
| Edge | Edge | ||
FIG. 3.
Setup of the MTF phantom. (a) Definition of the coordinate system. (b) Different off-centered positions studied in this work.
2.D. Ex vivo animal study
A bovine bone with an induced submillimeter fracture was placed in a 16 cm-diameter water cylinder to simulate a high contrast and high frequency CT imaging task; the performance of this kind of task is predominantly determined by the spatial resolution of the CT system. This animal bone fracture model was scanned using both conventional and Hi-Res modes; other scan parameters were kept the same as in the phantom studies. The model was positioned both at the center of the SFOV and at 16 cm off-centered position. Images were reconstructed with 50 mm display FOV, 512 × 512 matrix size, 2.5 mm slice thickness, and all kernels available. The sharpness of the fracture was qualitatively compared with the phantom results.
3. RESULTS
3.A. Validation of the proposed MTF measurement method
We first validated the thick slice-based MTF measurement method proposed in Sec. 2.B for both conventional and Hi-Res scan modes. As shown in Fig. 4, the MTFs of the conventional scan mode with Standard kernel and Hi-Res mode with HD Bone kernel were measured using both 0.625 and 5 mm CT slices after averaging 80 repeated scans. In the case of HD Bone kernel, signal truncation was avoided by the use of extended HU thin-slice images. The MTFs obtained using these two slice thicknesses are matched. Therefore, thick slice can be used to measure the MTF of CT systems despite the presence of partial volume averaging, as long as the test object is small enough compared with the limiting resolution of the system. Nonetheless, extended HU alone cannot achieve accurate results due to high noise levels, as shown in Fig. 4; while extended HU can be considered as an alternative to address signal truncation, repeated scans are still necessary in Hi-Res mode MTF measurements. Note that if the slice thickness is insufficient to contain the spreading of the signal along the z direction, the truncation of the signal (from the bead) along z will impact the MTF. As shown in Fig. 5, the MTF of the Hi-Res mode with the HD Edge kernel varies when the slice thickness is less than 5 mm. Once beyond 5 mm, the MTF becomes stable, indicating that the longitudinal spreading of the signal was completely contained within the 5 mm slice.
FIG. 4.
Comparison of the MTFs measured from thin (0.625 mm) and thick (5 mm) CT slices for the conventional mode with the Standard kernel and the Hi-Res mode with the HD Bone kernel. Thin slice MTF for the HD Bone kernel was obtained from images with extended HU to avoid signal truncation. Thick slice images did not use the extended HU scale. The MTFs were measured at the iso-center.
FIG. 5.
Comparison of MTFs of the Hi-Res mode with the HD Edge kernel measured at different slice thicknesses. The MTFs were measured at the iso-center.
3.B. Dependence of MTF on object positions
Two-dimensional (2D) MTF results acquired at different scan-modes (conventional versus Hi-Res) and off-centered positions are summarized in Fig. 6. To provide an intuitive illustration of the magnitude of spatial blurring at those system settings, the 2D PSF results are also provided in this figure. For a given scan mode, the highest spatial resolution was achieved at the centered position (0 cm); as the position of the MTF test object was moved towards the peripheral region of the SFOV, the PSF became broader and the MTF became narrower, both of which indicated degraded spatial resolution. Figure 7 provides a direct comparison of the MTF plots at different off-centered positions for the conventional mode and the Bone kernel.
FIG. 6.
Comparison of the 2D PSF and MTF results for the “Bone” type of reconstruction kernel (Bone and HD Bone) at different scan modes and off-centered positions. Here, the horizontal and vertical directions correspond to tangential and radial directions, respectively. For the ease of visualization PSF images were selfnormalized.
FIG. 7.
Comparison of the tangential MTFs at different off-centered positions for the conventional scan mode and Bone kernel.
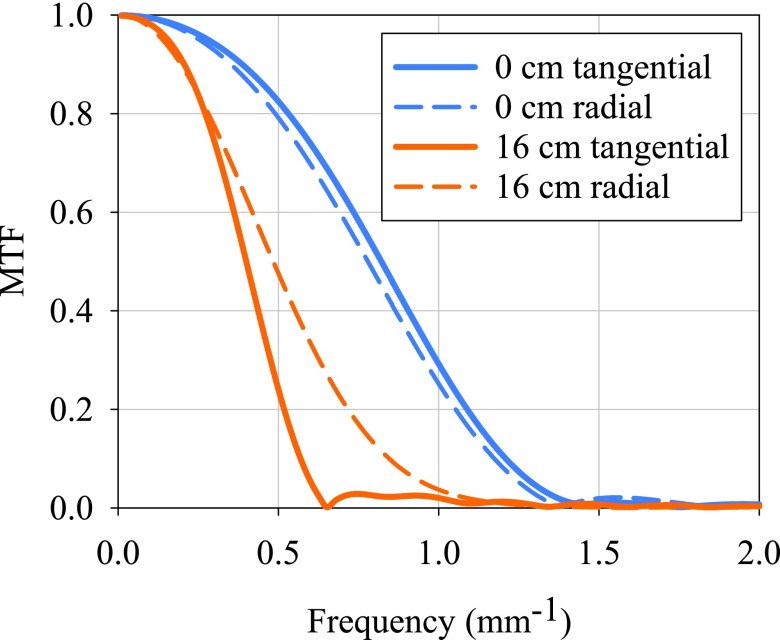
While the PSF and MTF were isotropic at the centered position, they became more and more anisotropic towards the peripheral region. Interestingly, the PSF was elongated more severely along the tangential direction; similarly, the MTF degraded more severely along the same direction (Fig. 8). Along the tangential direction, the frequency corresponding to the 10% level of the MTF curve (i.e., MTF-10) was 1.2 and 0.6 mm−1 for 0 and 16 cm off-centered position, respectively. In comparison, the MTF-10 was 1.2 and 0.9 mm−1 for 0 and 16 cm off-centered position, respectively, along the radial direction. This anisotropic spatial resolution was primarily caused by the finite integration time of the recording process of each projection: during a CT acquisition, the x-ray tube is turned on and continuously rotating around the iso-center; therefore, the recording of each projection within a finite time interval inevitably covers a finite angular interval along the tangential direction. Compared with the centered position, this finite angular interval corresponds to a much longer spatial distance at the peripheral region of the SFOV, leading to increased spatial blurring.1 Therefore, the MTF in the tangential direction is of great interest in our study; throughout the remainder of the paper, reference to one-dimensional MTFs and MTF-10 values is associated with the tangential direction, unless explicitly stated otherwise.
FIG. 8.
Comparison of the tangential MTF with the radial MTF at both centered (0 cm) and off-centered (16 cm) positions for the conventional scan mode and Bone kernel.
3.C. Dependence of MTF on scan mode
The loss in spatial resolution at the off-centered positions was significantly mitigated by the Hi-Res scan mode. As shown in Fig. 6, the spatial span of the PSF is significantly narrower in Hi-Res than in the conventional mode at a given off-centered position; similarly, the frequency span of the MTF is significantly wider in Hi-Res than in the conventional mode at a given off-centered position. MTF-10 of Hi-Res at 6 cm off-centered position matches that of the conventional scan mode at the centered position for the Bone kernel (Fig. 9). At centered position, however, the MTF was not improved by the use of the Hi-Res mode alone: the MTF-10 (Bone kernel) for both the conventional mode and Hi-Res was 1.2 mm−1. Figures 10 and 11 provide a direct comparison of the MTFs of Hi-Res and conventional mode for Bone and Edge kernels. The furthest off-centered distance where Hi-Res mode with HD Edge kernel achieved a similar MTF-10 value to that of conventional mode with Edge kernel at the iso-center was found to be 8 cm (Table II).
FIG. 9.
MTFs of conventional scan mode at centered (0 cm) position and Hi-Res mode at 6 cm off-centered position. Bone reconstruction kernel was used.
FIG. 10.
MTFs of conventional and Hi-Res scan mode (with or without HD kernel) at both centered (0 cm) and off-centered (16 cm) positions. Bone or HD Bone reconstruction kernel was used.
FIG. 11.
MTFs of conventional and Hi-Res scan mode (with or without HD kernel) at both centered (0 cm) and off-centered (16 cm) positions. Edge or HD Edge reconstruction kernel was used.
TABLE II.
MTF-10 along the tangential direction for all scan protocols and off-centered positions included in this study.
| Tangential MTF-10 (mm−1) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Conventional | Hi-Res | |||||||||
| Kernel | 0 cm | 4 cm | 8 cm | 12 cm | 16 cm | 0 cm | 4 cm | 8 cm | 12 cm | 16 cm |
| Soft | 0.62 | 0.62 | 0.60 | 0.55 | 0.48 | 0.62 | 0.63 | 0.62 | 0.61 | 0.58 |
| Standard | 0.71 | 0.70 | 0.66 | 0.59 | 0.50 | 0.71 | 0.71 | 0.70 | 0.68 | 0.63 |
| Detail | 0.84 | 0.83 | 0.75 | 0.63 | 0.52 | 0.86 | 0.86 | 0.82 | 0.75 | 0.67 |
| Lung | 0.90 | 0.89 | 0.85 | 0.78 | 0.59 | 0.89 | 0.91 | 0.88 | 0.85 | 0.77 |
| Chest | 1.08 | 1.06 | 0.91 | 0.75 | 0.56 | 1.42 | 1.39 | 1.23 | 0.95 | 0.78 |
| Bone | 1.21 | 1.17 | 0.99 | 0.78 | 0.57 | 1.23 | 1.23 | 1.14 | 0.94 | 0.78 |
| Bone plus | 1.21 | 1.18 | 1.02 | 0.84 | 0.60 | 1.22 | 1.23 | 1.15 | 0.97 | 0.82 |
| Edge | 1.46 | 1.42 | 1.12 | 0.83 | 0.58 | 1.46 | 1.44 | 1.29 | 0.97 | 0.80 |
| HD Standard | 0.84 | 0.83 | 0.80 | 0.77 | 0.69 | |||||
| HD Detail | 1.05 | 1.05 | 0.97 | 0.85 | 0.71 | |||||
| HD Lung | 1.12 | 1.13 | 1.06 | 0.94 | 0.81 | |||||
| HD Bone | 1.38 | 1.37 | 1.24 | 0.97 | 0.79 | |||||
| HD Bone plus | 1.59 | 1.54 | 1.28 | 0.97 | 0.80 | |||||
| HD Ultra | 1.74 | 1.70 | 1.38 | 1.04 | 1.09 | |||||
| HD Edge | 1.95 | 1.93 | 1.41 | 1.09 | 0.91 | |||||
For completeness, a comparison between results obtained with our method and those obtained from helical scans was also performed. To do so, a limited number of Hi-Res mode helical scans of the Catphan were acquired with the same radiological parameters as the axial scans, and a pitch of 0.5 with the bead at 0 cm off-centered position. Figure 12 shows the results for the Standard kernel and HD Detail kernel; it is observed that both axial and helical MTFs are similar. This result can be explained given the fact that Hi-Res mode only enables relatively small pitches (below 1), so that data interpolation inherent to helical reconstruction does not largely affect the in-plane spatial resolution.
FIG. 12.
Comparison of helical and axial scan MTFs for Hi-Res scan mode with Standard kernel and HD Detail kernel.
3.D. Dependence of MTF on reconstruction kernels
Figure 6 shows that the combined use of the Hi-Res scan mode and the HD reconstruction kernel further improved MTF at all spatial locations. At centered position, the MTF-10 for conventional mode, Hi-Res, and Hi-Res + HD kernel was 1.2, 1.2, 1.3 mm−1, respectively, for the Bone type of reconstruction kernel; when moved to the 8 cm off-centered position, the MTF-10 for conventional mode, Hi-Res, and Hi-Res + HD kernel was 1.0, 1.1, 1.2 mm−1, respectively, along the tangential direction, and 0.8, 1.2, 1.3 mm−1, respectively, along the radial direction.
Figure 13 provides a side-by-side comparison of the MTF curves for several representative reconstruction kernels. A complete list of the measured MTF data in terms of MTF-10 is given in Tables II and III. At a given off-centered position, Hi-Res + HD Edge led to the highest MTF-10, and the MTF-10 of Hi-Res + HD Bone can match that of Hi-Res + Edge. Another interesting finding is that, edge-enhancing kernels (such as the Edge kernel) were more sensitive to off-centering than the relatively smooth kernels (such as the Standard kernel): in the case of conventional scan mode, the MTF-10 of the Edge kernel degraded by 60% by moving from the center to the 16 cm off-centered position, while the degradation was only 30% for the Standard kernel.
FIG. 13.
MTFs of the Hi-Res scan mode generated by different reconstruction kernels at the centered position.
TABLE III.
MTF-10 along the radial direction for all scan protocols and off-centered positions included in this study.
| Radial MTF-10 (mm−1) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Conventional | Hi-Res | |||||||||
| Kernel | 0 cm | 4 cm | 8 cm | 12 cm | 16 cm | 0 cm | 4 cm | 8 cm | 12 cm | 16 cm |
| Soft | 0.60 | 0.63 | 0.59 | 0.61 | 0.54 | 0.61 | 0.64 | 0.63 | 0.63 | 0.57 |
| Standard | 0.68 | 0.69 | 0.64 | 0.66 | 0.61 | 0.68 | 0.71 | 0.71 | 0.70 | 0.65 |
| Detail | 0.78 | 0.82 | 0.69 | 0.71 | 0.66 | 0.79 | 0.86 | 0.83 | 0.81 | 0.73 |
| Lung | 0.89 | 0.87 | 0.78 | 0.79 | 0.81 | 0.91 | 0.89 | 0.89 | 0.87 | 0.83 |
| Chest | 1.07 | 1.05 | 0.76 | 0.80 | 0.81 | 1.39 | 1.37 | 1.35 | 1.18 | 1.05 |
| Bone | 1.17 | 1.17 | 0.77 | 0.84 | 0.85 | 1.21 | 1.21 | 1.19 | 1.10 | 1.00 |
| Bone plus | 1.18 | 1.18 | 0.97 | 1.11 | 0.91 | 1.21 | 1.20 | 1.19 | 1.12 | 1.03 |
| Edge | 1.45 | 1.44 | 1.27 | 0.94 | 0.94 | 1.43 | 1.42 | 1.39 | 1.24 | 1.07 |
| HD Standard | 0.83 | 0.83 | 0.82 | 0.80 | 0.72 | |||||
| HD Detail | 1.02 | 1.04 | 1.01 | 0.95 | 0.85 | |||||
| HD Lung | 1.11 | 1.11 | 1.10 | 1.04 | 0.98 | |||||
| HD Bone | 1.34 | 1.35 | 1.33 | 1.19 | 1.06 | |||||
| HD Bone plus | 1.54 | 1.54 | 1.49 | 1.24 | 1.08 | |||||
| HD Ultra | 1.71 | 1.70 | 1.71 | 1.37 | 1.16 | |||||
| HD Edge | 1.90 | 1.93 | 2.18 | 1.49 | 1.78 | |||||
3.E. Ex vivo bone fracture model
The MTF results were corroborated by the ex vivo bovine bone image results shown in Fig. 14. The loss in sharpness of the fracture when placed at a severely off-centered position can be clearly observed. The use of Hi-Res mode and the HD kernels mitigated such degradation and improved the conspicuity of the fracture. At the centered position, the use of Hi-Res alone did not improve much spatial resolution, but the combined use of Hi-Res and HD kernel improved the ability of the image to convey details about the bony structure. The images also demonstrate that the sharpness of the image strongly depends on the reconstruction kernel; HD Edge led to the sharpest images compared with other HD and non-HD kernels.
FIG. 14.
Images of the ex vivo animal bone fracture model acquired at different scan modes (conventional vs Hi-Res), off-centered positions (0 and 16 cm), and reconstruction kernels. The image display window and level were 2000 and 300, respectively.
4. DISCUSSION
In this work, the spatial resolution performance of the Hi-Res scan mode and the associated high-definition (HD) kernels was experimentally assessed. To address the two major challenges (signal truncation and noise contamination) imposed by the Hi-Res scan modes, an MTF measurement method based on a high contrast metallic bead and thick-slice reconstruction was developed. Results of the validation studies demonstrated that, as long as the dimension of the bead is small enough compared with the spatial resolution of the CT system, CT images with thick slice thickness can still be used to accurately measure the MTF. By combining this method with ensemble averaging, the MTF of the Hi-Res scan mode was systematically studied at different off-centered positions and reconstruction kernels.
The study showed the following major conclusions regarding the measured spatial resolution of the studied MDCT system with Hi-Res scan mode: (1) the spatial resolution of the MDCT system deteriorates toward the peripheral region of the SFOV, and the MTF along the tangential direction of the SFOV suffers more degradation than the MTF along the radial direction; (2) compared with the conventional scan mode, the Hi-Res mode mitigates the loss in spatial resolution at the peripheral region, particularly along the tangential direction; (3) the combined use of the Hi-Res mode and the HD kernels further improved spatial resolution at not only the off-centered position but also at the iso-center; (4) the HD kernels generate better spatial resolution when other system parameters are matched.
However, the studies also demonstrated that the improvement of spatial resolution for the Hi-Res scan mode strongly depends on the object location and the reconstruction kernel. As shown in Fig. 14, the use of Hi-Res alone does not improve spatial resolution at the iso-center. This is due to the fact that the spatial distance covered by each detector element at the center of FOV is independent of the angular sampling rate. The spatial resolution at the iso-center is determined by other factors such as the size of detector elements, size of x-ray focal spot, and the reconstruction kernels. This explains why the HD reconstructions kernel are able to improve spatial resolution even at the iso-center, because they allow more high frequency signal to be transferred from the projection data to the final reconstructed CT images. Compared with the counterpart of the conventional reconstruction kernels, the HD kernels seem to have a wider bandwidth, although the specific shapes of these kernels are the proprietary information of the CT vendor.
While the spatial resolution loss at the off-centered positions can be significantly mitigated, in cases of significantly large off-centering (>8 cm), the loss in spatial resolution is so severe that even the Hi-Res mode and HD kernels cannot completely restore the spatial resolution to the “nominal” level, which is usually characterized at the center of the SFOV. This fact suggests that whenever it is possible, the feature of interest should be placed as close as possible to the iso-center of the SFOV. In case that severe off-centering is inevitable due to some practical constraint, other novel CT technologies may be used as an alternative to perform clinical tasks. For example, a dedicated musculoskeletal cone-beam CT system allows the elbow CT exam to be performed at the centered position without being obstructed by the head and shoulder, and the hardware setup and reconstruction method of this dedicated system can be optimized to further improve spatial resolution.10–13 Model-based iterative reconstruction is another approach to improve spatial resolution for high contrast objects;14,15 however, the current software version of MBIR installed in our scanner is incompatible with Hi-Res mode.
Although the dependence of spatial resolution on off-centered position generally followed a monotonic trend, namely, better resolution with the test object being placed closer to the iso-center, there was one exception: in the conventional mode, the PSF of certain edge enhancing kernel was elongated more along the radial direction at 8 cm than at 10 cm, indicating a poorer spatial resolution along the radial direction at 8 cm than at 10 cm (Fig. 6). This unique point was found only in the conventional mode, and the elongation was increasingly noticeable for kernels with high-frequency coverage, such as the Bone kernel. The exact cause of this unique behavior is yet unknown, but interestingly, the use of Hi-Res mode completely removed it.
When spatial resolution was described by a numerical index in this work, MTF-10 was extensively used (e.g., in Tables II and III), which is a metric commonly used to describe the highest spatial frequency resolvable by an imaging system. Meanwhile, MTF-50 (the frequency corresponding to the 50% level of the MTF curve) is another metric to quantify spatial resolution, particularly at lower or intermediate frequencies. Depending on the application, sometimes it is necessary to use MTF-50 (and even the entire curve of the MTF) to complement MTF-10 when evaluating the spatial resolution performance of the imaging system.
As far as image noise is concerned, for filtered backprojection-based MDCT systems, improved spatial resolution is always associated with an increase in image noise. Figure 14 suggests that the use of the HD kernel and Hi-Res mode amplified noise. Since the conspicuity of a feature in an image is determined by both spatial resolution and noise, better spatial resolution does not necessarily lead to better diagnostic performance, although for some imaging tasks that involve high frequency and high contrast features, the performance is predominantly determined by spatial resolution. In a separate paper, a thorough study to characterize the noise properties of the Hi-Res mode and the HD kernels and the combined effects of spatial resolution and noise on diagnostic performance of some specific imaging tasks will be presented.
Finally, the signal truncation problem encountered in MTF measurements can be addressed by extending the range of CT numbers from the current “normal range” of [ − 1024, 3071] to [ − 31 743, 31 743] by using the extended HU mode offered by some manufacturers. However, not all scanners or scan modes are supported by the extended HU, and the practical value of the extended HU in clinical practice is unknown yet. The method presented in this paper provides a practical means to perform in-plane resolution measurement without invoking of the extended HU. However, if the three-dimensional MTF measurements are required, the “extended range” of CT numbers can be beneficial. Alternative methods to obtain the three-dimensional MTF may not require the extended range of CT numbers, as proposed by Thornton and Flynn.16 Nonetheless, such alternatives need to be explicitly validated for Hi-Res mode and HD kernels.
5. CONCLUSIONS
The Hi-Res scan mode and the associated High-Definition (HD) reconstruction kernels improve spatial resolution of MDCT systems at both centered and off-centered positions. The introduction of Hi-Res and Hi-Res/HD modes provides a solution to compensate for the spatial resolution loss at peripheral regions of the scan FOV, particularly for those clinical cases where patient off-centering is inevitable.
ACKNOWLEDGMENTS
This work is partially supported by an NIH Grant (No. R01CA169331), GE Healthcare, and the National Council for Science and Technology (CONACYT) of Mexico (J.P.C.-B.).
REFERENCES
- 1.Hsieh J., Computed Tomography: Principles, Design, Artifacts, and Recent Advances (SPIE, Bellingham, WA, 2009). [Google Scholar]
- 2.Toth T., Ge Z., and Daly M. P., “The influence of patient centering on CT dose and image noise,” Med. Phys. 34, 3093–3101 (2007). 10.1118/1.2748113 [DOI] [PubMed] [Google Scholar]
- 3.Habibzadeh M., Ay M., Asl A. K., Ghadiri H., and Zaidi H., “Impact of miscentering on patient dose and image noise in x-ray CT imaging: Phantom and clinical studies,” Phys. Med. 28, 191–199 (2012). 10.1016/j.ejmp.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 4.Kam S., Youn H., Kim H. K., and Jeon H., “An experimental study on the shift-variant MTF of CT systems using a simple cylindrical phantom,” Proc. SPIE 8668, 86684Q-1–86684Q-7 (2013). 10.1117/12.2007862 [DOI] [Google Scholar]
- 5.Ranallo F. and Szczykutowicz T., “SU-F-18C-03: Loss of image sharpness in CT bone imaging due to positioning within the scan field of view-possible solutions,” Med. Phys. 41, 403 (2014). 10.1118/1.4889087 [DOI] [Google Scholar]
- 6.Sohval A. R. and Freundlich D., “Plural source computed tomograhy device with improved resolution,” U.S. patent 4637040 A (Jan. 13 1986).
- 7.Lonn A. H., “Computed tomography system with translatable focal spot,” U.S. patent 5173852 A (Dec. 22 1990).
- 8.Hsieh J., Gard M. A., and Gravelle S., “Reconstruction technique for focal spot wobbling,” Proc. SPIE 1652, 175–182 (1992). 10.1117/12.59424 [DOI] [Google Scholar]
- 9.Hsieh J., Saragnese E. L., Stahre J. E., Dorri B., Kaufman J., and Senzig R. F., “Methods and apparatus for x-ray imaging with focal spot deflection,” U.S. patent 7869571 B2 (Jan. 11 2008).
- 10.Zbijewski W., De Jean P., Prakash P., Ding Y., Stayman J. W., Packard N., Senn R., Yang D., Yorkston J., Machado A., Carrino J. A., and Siewerdsen J. H., “Design and optimization of a dedicated cone-beam CT system for musculoskeletal extremities imaging,” Proc. SPIE 7961, 796104-1–796104-8 (2011). 10.1117/12.878077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zbijewski W., De Jean P., Prakash P., Ding Y., Stayman J. W., Packard N., Senn R., Yang D., Yorkston J., Machado A., Carrino J. A., and Siewerdsen J. H., “A dedicated cone-beam CT system for musculoskeletal extremities imaging: Design, optimization, and initial performance characterization,” Med. Phys. 38, 4700–4713 (2011). 10.1118/1.3611039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carrino J. A., Muhit A. A., Zbijewski W., Thawait G. K., Stayman J. W., Packard N., Senn R., Yang D., Foos D. H., Yorkston J., and Siewerdsen J. H., “Dedicated cone-beam CT system for extremity imaging,” Radiology 270, 816–824 (2014). 10.1148/radiol.13130225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thawait G. K., Demehri S., AlMuhit A., Zbijweski W., Yorkston J., Grande F. D., Zikria B., Carrino J. A., and Siewerdsen J. H., “Extremity cone-beam CT for evaluation of medial tibiofemoral osteoarthritis: Initial experience in imaging of the weight-bearing and non-weight-bearing knee,” Eur. J. Radiol. 84, 2564–2570 (2015). 10.1016/j.ejrad.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richard S., Husarik D. B., Yadava G., Murphy S. N., and Samei E., “Towards task-based assessment of CT performance: System and object MTF across different reconstruction algorithms,” Med. Phys. 39, 4115–4122 (2012). 10.1118/1.4725171 [DOI] [PubMed] [Google Scholar]
- 15.Li K., Garrett J., Ge Y., and Chen G.-H., “Statistical model based iterative reconstruction (MBIR) in clinical CT systems. Part II. Experimental assessment of spatial resolution performance,” Med. Phys. 41, 071911 (12pp.) (2014). 10.1118/1.4884038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thornton M. M. and Flynn M. J., “Measurement of the spatial resolution of a clinical volumetric computed tomography scanner using a sphere phantom,” Proc. SPIE 6142, 61421Z-1–61421Z-10 (2006). 10.1117/12.654969 [DOI] [Google Scholar]