Abstract
Background: Most American mothers who feed human milk (HM) now use pumps to produce some of the HM they feed. Pumping is nationally recommended, but associations between pumping and HM-feeding durations are unknown.
Objectives: We examined whether and how the pumping frequency and types of reasons for pumping between 1.5 and 4.5 mo postpartum are associated with HM-feeding durations. We classified pumping reasons as nonelective [e.g., because of a difficulty feeding at the breast (FAB)] or elective (e.g., to produce HM to mix with solids). We hypothesized that women who pumped more frequently or nonelectively would have shorter HM-feeding durations.
Design: We used data from 1116 mothers in a longitudinal cohort who fed and pumped HM 1.5–4.5 mo postpartum. We used χ2 and Cox proportional hazards regression models to examine the survival of any HM feeding, exclusive HM feeding, and FAB.
Results: Compared with mothers who pumped for elective reasons, mothers who reported one nonelective reason had greater hazards of stopping feeding any HM (HR: 1.12; 95% CI: 1.05, 1.21) or exclusive HM (HR: 1.14; 95% CI: 1.09, 1.20) and of stopping FAB (HR: 2.07; 95% CI: 1.77, 2.42). Mothers who pumped most frequently had the highest mean hazards of stopping feeding any HM (HR: 1.82; 95% CI: 1.68, 1.93) and feeding exclusive HM (HR: 1.21; 95% CI: 1.14, 1.26). Hazards of stopping FAB varied across the year. Compared with the least-frequent pumpers, the most-frequent pumpers had a 2.6-fold higher hazard of stopping FAB at 3 mo postpartum and a 1.7-fold higher hazard at 6 mo postpartum.
Conclusions: Nonelective pumping reasons and higher pumping frequency were associated with shorter HM-feeding durations. Mothers who report that they use a breast pump for reasons related to either employment or FAB difficulty and their infants may be more vulnerable to risks associated with a shorter HM-feeding duration.
Keywords: human milk, infant feeding, lactation, milk expression, pumping
INTRODUCTION
Most US mothers who produce human milk (HM)2 to feed to their infants now use pumps in place of some or all feeding at the breast (FAB). HM expression, or pumping, has rapidly become a widespread practice (1–4) because of a convergence of work-related constraints to FAB (5–8) and recent technological advancements in commercially available pumps (9, 10). National endorsements (11) have promoted pumping and feeding pumped HM as equivalent to FAB to meet HM-feeding goals and optimal health outcomes for the mother and infant (11, 12). However, little is known about the relation between pumping practices and HM-feeding outcomes.
Two complementary longitudinal studies have provided an understanding of current pumping practices. First, the Infant Feeding Practices Study II (IFPS II) (13) has survey provided quantitative data on pumping from a large, national sample of 3000 mothers. In IFPS II mothers who fed HM between 1.5 and 4.5 mo postpartum, 85% of them had pumped, and many had pumped regularly or exclusively (4). Second, in our recent qualitative study (14), 20 pumping mothers reported their attitudes, perceptions, and determinants of and practices for pumping.
Mothers’ reasons for pumping may influence how they pump and, thus, how they feed their HM. Mothers in our earlier qualitative sample described reasons for pumping that included, expanded on, and provided key insights into reasons for pumping that were reported by IFPS II mothers. Mothers in the qualitative sample reported reasons for pumping that could be described by the degree to which mothers elected to pump. Mothers who pumped for nonelective reasons, such as latch difficulty or work outside the home, pumped more often than did mothers who pumped only for elective reasons such as allowing other caregivers to bond with infants. Mothers who pumped for nonelective reasons also fed formula and stopped feeding HM much earlier than mothers did who pumped only occasionally. These qualitative findings have provided a context to interpret IFPS II data and have suggested the importance of considering elective compared with nonelective reasons for pumping.
A recent review showed inconsistent evidence for the claim that pumping when FAB is unavailable maintains or extends the duration that HM is fed (15). The potential link between pumping and FAB practices is of particular interest because some benefits to infants result from FAB than from feeding HM from a bottle (16–20). Thus, because breastfeeding can be interpreted as both feeding HM from a bottle and at the breast, we use the term FAB to refer unambiguously to HM feeds at the breast.
With the use of data from the IFPS II cohort, we investigated 2 hypotheses. First, we hypothesized that mothers who had more nonelective reasons for pumping between 1.5 and 4.5 mo postpartum would have shorter durations of any and exclusive HM feeding and of FAB than would mothers with fewer or no nonelective reasons for pumping. Second, we hypothesized that mothers who pumped more frequently between 1.5 and 4.5 mo postpartum would have shorter durations of any and exclusive HM feeding and of FAB than would mothers who pumped less often during this interval.
METHODS
IFPS II data
The IFPS II data set was collected by the US Food and Drug Administration and the CDC between 2005 and 2007 (13). Briefly, ∼3000 mothers from a national consumer opinion panel were surveyed once prenatally and 10 times across the first year postpartum. All infants were singletons born at term with birth weights >2500 g. IFPS II mothers reported pumping practices on month 2, 5, and 7 surveys. Because the timing of mothers’ receipt and return of these surveys varied, previous IFPS II investigators (4) regrouped these 3 surveys by infant age at the time of the survey return into 3 mutually exclusive ranges (i.e., 1.5–4.5, >4.5 to 6.5, and >6.5 to 9.5 mo postpartum). Because our qualitative study suggested the importance of early pumping practices in relation to long-term HM-feeding outcomes, the IFPS II analysis was limited to mothers who reported pumping practices between 1.5 and 4.5 mo postpartum. We identified women who fed HM during this interval (n = 1696) and excluded those who did not report pumping practices, which left 1116 women to be considered for the analyses (Figure 1). Inasmuch as preliminary analyses showed that a substantial number of mothers in this group were missing data on pumping frequency (n = 72) or other model covariates (n = 233), we used multiple imputation through chained equations to simulate 10 similar data sets. Statistical analyses were run in each data set, and effect variables were pooled to obtain one overall variable for the exposure of interest for each model. This imputation and all other statistical analyses were conducted with SAS software (version 9.3; SAS Institute Inc.).
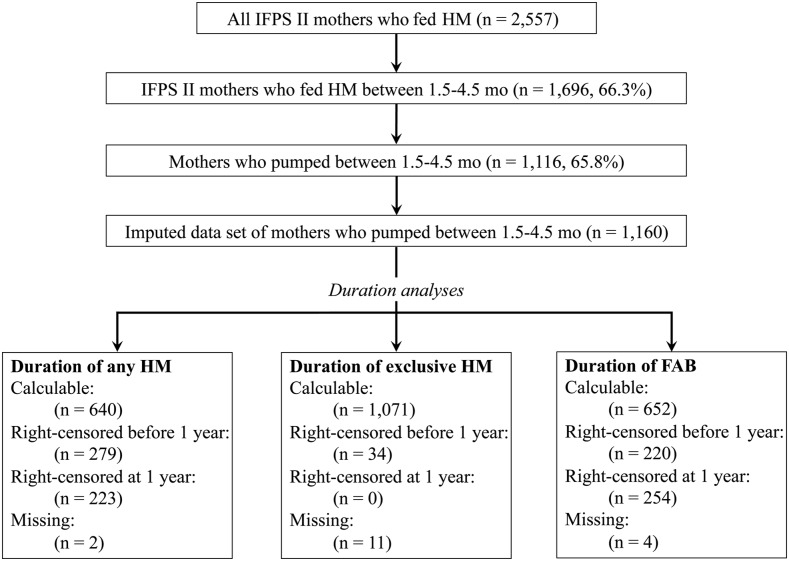
FIGURE 1.
Inclusion of IFPS II mothers into samples for analyses. The figure shows which mothers were considered for inclusion in our final sample and how many mothers were excluded. The bottom 3 boxes in the figure show how many mothers reported enough data to calculate the duration that they fed any or exclusive HM and fed at the breast and how many mothers’ durations were right-censored for analyses. FAB, feeding at the breast; HM, human milk; IFPS II, Infant Feeding Practices Study II.
Statistical analyses
Hypothesis 1
In our exploratory analyses, we observed a substantial overlap in mothers’ indicated reasons for pumping so that it was impossible to ascertain the impact of any single reason on the duration of HM-feeding practices. In addition, some survey questions included answers that grouped multiple reasons for pumping that might have had differing effects on long-term HM feeding (e.g., pumping “to feed to my baby when I do not want to breastfeed or when baby cannot breastfeed”) or were too ambiguous to interpret (e.g., “to get milk for someone else to feed my baby”).
In light of these limitations, we used a score to indicate the number of nonelective reasons reported for pumping. Mothers indicated their reasons from a closed list of 9 options that we classified as elective or nonelective (Table 1). On the basis of previous qualitative research, we classified 5 reasons as nonelective, 3 reasons as elective, and one reason as ambiguous. Mothers were given a score from zero to 5 to indicate the number of possible nonelective reasons for pumping that they had indicated; few mothers reported between 3 and 5 nonelective reasons for pumping, and thus, these mothers were combined.
TABLE 1.
Classification of pumping reasons as elective compared with nonelective1
| Reason for pumping | Classification |
| To relieve engorgement | Nonelective |
| Because my nipples were too sore to nurse | Nonelective |
| To increase my milk supply | Nonelective |
| To get milk for someone else to feed my baby | Ambiguous |
| For me to feed to my baby when I do not want to breastfeed or when baby cannot breastfeed | Nonelective |
| To keep my milk supply up when my baby could not nurse (such as while you were away from your baby or when your baby was too sick to nurse) | Nonelective |
| To mix with cereal or other food | Elective |
| To have an emergency supply of milk | Elective |
| To donate to a baby other than my own | Elective |
See Statistical analyses, Hypothesis 1 for explanation.
To test the first hypothesis, we used survival analyses to model the nonelective pumping score as a predictor of the duration of any HM-feeding, FAB, and exclusive HM-feeding (3 separate models; one model for each outcome). To create variables for the durations of feeding any or exclusive HM and of FAB, we used the methods described in Statistical analyses, Hypothesis 2. Adjusted models included all covariates used in hypothesis 2 models except employment-related variables, which were omitted because of their direct impact on nonelective reasons for pumping.
Hypothesis 2
We examined the effect of pumping practices as both categorical and continuous predictors of the duration of HM-feeding practices. Mothers reported whether they considered themselves to be pumping regularly and how many times they had pumped in the previous 2 wk. To model pumping as a continuous predictor, we calculated HRs for a difference of 10 pumping episodes in the previous 2 wk or one pumping episode per workday for 2 full work weeks. We also used the pumping frequency of mothers as a categorical predictor by dividing mothers at the median pumping frequency and into pumping-frequency quartiles.
The primary study outcomes were the duration of any HM feeding, the duration of exclusive HM feeding, and the duration of FAB. In descriptive analyses, durations were described by the median rather than by the mean because a large proportion of mothers either reported still feeding HM and FAB at the end of data collection (12 mo postpartum) or were right censored before 12 mo postpartum. For survival analysis models, durations were computed on the basis of data on feeding practices from each returned survey. The surveys asked mothers to estimate the number of feedings of HM, formula, and other milks in the previous week, and with the use of these questions, we categorized each dyad at each postpartum month (yes; no; or missing or could not determine) for feeding HM, formula, and solids and for FAB. One question explicitly asked about bottle-feeding HM, but no question explicitly assessed FAB. As such, other survey questions that referenced FAB were used to infer FAB status where possible. To calculate the durations of feeding any HM, feeding exclusive HM, and FAB, we used these monthly categorizations to identify key changes in feeding practices. For example, we assumed that mothers stopped feeding HM between the last survey on which they reported feeding HM and the first survey on which no HM feeding was reported. For a mother who last reported HM feeding on the month 9 survey, the duration of HM feeding was calculated as the infant’s age at the midpoint between the dates she returned month 9 and month 10 surveys. The duration of FAB was calculated in the same way. For the duration of feeding exclusive HM, we identified the survey when mothers first reported feeding formula or solids, and calculated the midpoint between this survey and the last survey on which only HM feeding was reported. For all duration variables, if mothers did not return the necessary adjacent survey, the most proximal adjacent survey was identified and used to estimate durations.
We identified potential survival model covariates with the use of previous IFPS II analyses of pumping practices and their determinants (4), our qualitative work (14), and the scientific literature that has described the predictors of HM-feeding practices (6, 19, 21–23). Sociodemographic variables included mothers’ age, race/ethnicity (white non-Hispanic, black non-Hispanic, Asian or Pacific Islander non-Hispanic, Hispanic, or other), education (less than or equal to high school, some college, or college or greater), income (<185%, 185–350%, or >350% of the poverty-income ratio), marital status (married, widowed, divorced, separated, or never married), BMI category (normal weight, overweight, or obese), postnatal participation in the Special Supplemental Nutrition Program for Women, Infants, and Children, and national region of residence (Northeast, South, Midwest, and West). Employment-related variables included employment status between 1.5 and 4.5 mo postpartum and the intensity of return to work (0, 1–19, 20–34, or ≥35 h/wk). Pumping-related variables included whether mothers used electric compared with nonelectric pumps and new compared with used pumps, and mothers’ reported satisfaction with their pumps (high compared with low-to-medium satisfaction). Lactation-, HM-feeding, and FAB-related variables included mothers’ previous experience feeding HM and prenatal reports of discomfort FAB in public; whether mothers had vaginal, medicated, or a cesarean delivery; infant gestational age at birth; the timing of onset of lactogenesis II; how often infants emptied their bottles; and whether mothers reported a perception of a low HM supply. Perceptions of a low HM supply were not directly measured in IFPS II surveys. Thus, we created a dichotomous variable for mothers’ perceived low HM supply with the use of mothers’ reports of the use of pumping to increase their supply or of the introduction of formula because they perceived their supply to be inadequate or their infants to be unsatisfied with HM alone. We did not consider mothers reasons for pumping in our adjusted models because mothers’ reasons for pumping precede pumping practices and, thus, were antecedents to the exposure of interest (pumping practices).
We used survival analyses to model the pumping frequency during 1.5–4.5 mo postpartum as a predictor of the durations of any HM feeding, FAB, and exclusive HM feeding. To build survival models, we first used log-rank tests of equality for each potential categorical covariate and Cox proportional hazards models to narrow the list of potential covariates tested in main effect models. Each tested model contained covariates from each of the 4 groups of variables. Second, we evaluated a potential effect modification by testing 2-way interactions between the pumping frequency and descriptive variables for pumps. A potential effect mediation was evaluated by comparing models with and without each potential mediator for their main effect variables and significance. If a mediating effect was not seen, but covariates were significantly associated with the exposure and outcome, these covariates were tested for their modifying or confounding effects and kept in models as appropriate. We tested potential time-dependent effects between the pumping frequency and HM-feeding durations by including corresponding time-dependent covariates in the model. When time-dependent variables were significant in the model (α = 0.05), they were kept in the final model to account for these nonproportional effects and to obtain HRs at specific time points. This research was declared exempt by the Cornell University Institutional Review Board because all data were deidentified.
RESULTS
Mothers who pumped between 1.5 and 4.5 mo postpartum had a higher income and education, were less likely to have had a previous experience feeding HM, intended to feed HM longer, and returned to work more often, earlier, and at more hours per week than did mothers who fed HM but did not pump in this time period. Comparisons between these 2 groups are summarized in Table 2. Mothers in our imputed data set did not differ from mothers in the sample with missing data for any variables of interest.
TABLE 2.
Sample characteristics in mothers who fed and pumped HM between 1.5 and 4.5 mo postpartum1
| Characteristics and potential model covariates | Mothers who fed HM between 1.5 and 4.5 mo postpartum but did not pump (n = 493)2 | Mothers who fed and pumped HM between 1.5 and 4.5 mo postpartum (n = 1116) | P | Data set with imputation of missing covariates (n = 1116) |
| Sociodemographic characteristics | ||||
| Race/ethnicity, % | 0.20 | |||
| White | 83.6 | 85.4 | 85.4 | |
| Black | 5.0 | 3.1 | 3.1 | |
| Hispanic | 5.7 | 6.5 | 6.5 | |
| Asian/Pacific Islander | 4.1 | 3.1 | 3.1 | |
| Other | 1.6 | 1.9 | 1.9 | |
| Age, y | 29.6 ± 5.23 | 29.6 ± 5.1 | 0.69 | 29.6 ± 5.1 |
| Marital status, % | 0.56 | |||
| Married | 84.4 | 85.6 | 85.6 | |
| Widowed | 0.0 | 0.2 | 0.2 | |
| Divorced | 2.8 | 2.4 | 2.4 | |
| Separated | 0.7 | 0.8 | 0.8 | |
| Never married | 12.1 | 11 | 11 | |
| Region, % | 0.0004 | |||
| Northeast | 36.1 | 36.0 | 36 | |
| Midwest | 15.7 | 8.8 | 8.8 | |
| South | 30.7 | 34.6 | 34.6 | |
| West | 17.6 | 20.6 | 20.6 | |
| BMI, % | 0.72 | |||
| Normal | 53.3 | 50.8 | 50.8 | |
| Overweight | 25.5 | 26.6 | 26.6 | |
| Obese or greater | 21.2 | 22.6 | 22.6 | |
| Income (% of the PIR), % | <0.0001 | |||
| <185 | 44.5 | 31.5 | 31.5 | |
| 185–350 | 37.8 | 38.4 | 38.4 | |
| >350 | 17.7 | 30.1 | 30.1 | |
| WIC participation, % | <0.0001 | |||
| Yes | 38.3 | 28.3 | 28.2 | |
| No | 61.7 | 71.8 | 71.8 | |
| Education, % | <0.0001 | |||
| High school or less | 17.4 | 12.1 | 12.1 | |
| Some college | 41.7 | 35.9 | 35.9 | |
| College or greater | 40.9 | 52.0 | 52 | |
| Any work 1.5–4.5 mo postpartum, % | <0.0001 | |||
| Yes | 33.6 | 53.0 | 53 | |
| No | 66.5 | 47.0 | 47 | |
| Return to work timing, wk | 15.1 ± 13.3 | 12.4 ± 9.8 | 0.03 | 12.4 ± 9.8 |
| Return to work intensity, h/wk, % | <0.0001 | |||
| 0 | 73.6 | 54.5 | 54.5 | |
| 1–19 | 13.6 | 16 | 16.0 | |
| 20–34 | 5.6 | 10.3 | 10.3 | |
| ≥35 | 7.2 | 19.3 | 19.3 | |
| Lactation- and delivery-related variables, % | ||||
| HM-feeding experience | <0.0001 | |||
| Yes | 79.6 | 64.3 | 64.3 | |
| No | 20.4 | 35.7 | 35.7 | |
| Intended HM-feeding duration, mo | 0.0004 | |||
| <12 | 40.0 | 50.7 | 50.7 | |
| ≥12 | 60.0 | 49.3 | 49.3 | |
| Intended exclusive HM-feeding duration, mo | 0.53 | |||
| <5 | 37.1 | 35.9 | 35.9 | |
| ≥5 | 62.9 | 64.1 | 64.1 | |
| Perception of low milk supply | <0.0001 | |||
| No | 81.7 | 58.3 | 58.3 | |
| Yes | 18.3 | 41.8 | 41.8 | |
| Embarrassment of FAB in public | 0.45 | |||
| No | 58.1 | 56.2 | 57.1 | |
| Yes | 41.9 | 43.8 | 42.9 | |
| Lactogenesis II onset, d | 0.0004 | |||
| ≤3 | 83.1 | 75.3 | 75.3 | |
| >3 | 16.9 | 24.7 | 24.7 | |
| Bottle-emptying 1.5–4.5 mo postpartum | 0.03 | |||
| Most of the time or always | 62.7 | 69.9 | 69.9 | |
| Never to sometimes | 37.3 | 30.1 | 30.1 | |
| Delivery type | <0.0001 | |||
| Vaginal, unmedicated | 23.5 | 15.2 | 15.2 | |
| Vaginal, medicated | 53.7 | 57.4 | 57.4 | |
| Cesarean delivery | 22.7 | 27.4 | 27.4 | |
| Gestational age at birth, wk | 0.10 | |||
| 35–37 | 2.5 | 4.1 | 4.1 | |
| ≥ 37 | 97.5 | 95.9 | 95.9 | |
| Pumps and pumping practices | ||||
| Pump type, % | NA | |||
| Electric or combination electric/battery powered | NA | 68.1 | 68.1 | |
| Battery powered or manual | NA | 31.9 | 31.2 | |
| Age of most-used pump at purchase, % | NA | |||
| New | NA | 73.9 | 73.9 | |
| Used | NA | 26.2 | 26.2 | |
| Satisfaction with most-used pump, % | NA | |||
| High | NA | 82 | 81.9 | |
| Low | NA | 18 | 18.2 | |
| Timing of first pumping episode, wk | NA | 2.2 ± 2.2 | NA | 2.1 ± 2.2 |
| Reported nonelective reasons for pumping, n, % | NA | |||
| 0 | NA | 21.0 | 24.3 | |
| 1 | NA | 39.9 | 38.9 | |
| 2 | NA | 24.7 | 23.3 | |
| 3–5 | NA | 14.6 | 13.5 |
P values are for comparisons between mothers who both fed and pumped HM between 1.5 and 4.5 mo postpartum and mothers who fed HM but did not pump during this interval. Thus, P < 0.05 indicates a significant difference between mothers who pumped during this interval and those who did not use pumps to provide HM to their infants. FAB, feeding at the breast; HM, human milk; NA, not applicable; PIR, poverty-income ratio; WIC, the Special Supplemental Nutrition Program for Women, Infants, and Children.
Number of mothers in this column includes only mothers who indicated that they fed HM between 1.5 and 4.5 mo postpartum and also reported that they did not pump during this interval. Thus, 90 women for whom a pumping status between 1.5 and 4.5 mo postpartum could not be ascertained were excluded from these comparisons.
Mean ± SD (all such values).
Reasons for pumping and associated HM-feeding practices
In unadjusted analyses, mothers who pumped for a greater number of nonelective reasons had shorter durations of feeding any HM (P < 0.0001), of FAB (P < 0.0001), and of feeding exclusive HM (P < 0.0001) than mothers did who pumped for fewer or no nonelective reasons (Table 3). In adjusted models, an increasing number of nonelective reasons for pumping was generally associated with decreasing durations of feeding any or exclusive HM and of FAB (Table 4).
TABLE 3.
Outcomes for feeding HM associated with varying nonelective uses of pumping between 1.5 and 4.5 mo postpartum for mothers in the imputed data set1
| Feeding any HM, mo |
FAB, mo |
Feeding exclusive HM, mo |
|||||||||||
| ≥6 | ≥9 | ≥12 | ≥6 | ≥9 | ≥12 | ≥2 | ≥4 | ≥6 | |||||
| Group | n2 | Median | % | % | % | Median | % | % | % | Median | % | % | % |
| All | 1116 | 8.4 | 64.6 | 46.7 | 23.9 | 7.9 | 59.9 | 42.9 | 21.1 | 0.8 | 40.2 | 23.5 | 3.2 |
| Nonelective reasons for pumping, n | |||||||||||||
| 0 | 271 | 9.4 | 65.7 | 51.7 | 30.3 | 8.9 | 64.2 | 49.4 | 28.4 | 1.9 | 49.4 | 28.8 | 4.8 |
| 1 | 434 | 8.63,4 | 66.1 | 47.7 | 22.8 | 7.93,4> | 60.1 | 43.5 | 19.8 | 0.93,4 | 40.8 | 23.3 | 3.0 |
| 2 | 260 | 8.04,5 | 65.0 | 43.8 | 22.3 | 7.85 | 60.8 | 40.4 | 18.8 | 0.65 | 38.5 | 23.8 | 2.3 |
| 3–5 | 115 | 7.54,6 | 55.0 | 39.7 | 18.5 | 6.04,6 | 44.4 | 28.5 | 15.9 | 0.54,6 | 25.2 | 13.9 | 2.6 |
Medians are reported in each group because of the large number of mothers who were right censored at or before 1 y postpartum. Percentages represent proportions of mothers who were still feeding any HM, FAB, and feeding exclusive HM at each time point. Only mothers for whom the relevant feeding duration could be calculated or given a right-censored value were included in these calculations. Mothers who were right-censored at the study end for feeding HM and FAB were considered to have been feeding HM and FAB at each time point. FAB, feeding at the breast; HM, human milk.
Values represent numbers of mothers who were still feeding any HM, FAB, and feeding exclusive HM at each time point.
Duration for mothers who reported pumping for one nonelective reason between 1.5 and 4.5 mo postpartum was tested for a significant difference from the median feeding duration for mothers who did not report nonelective reasons for pumping.
Duration for mothers significantly differed from the median duration for mothers in the comparison group (i.e., the group of mothers with the next-lowest number of reported nonelective reasons for pumping) (P < 0.0001).
Duration for mothers who reported pumping for 2 nonelective reasons between 1.5 and 4.5 mo postpartum was tested for a significant difference from the median feeding duration for mothers who reported one nonelective reason for pumping.
Duration for mothers who reported pumping for 3–5 nonelective reasons between 1.5 and 4.5 mo postpartum was tested for a significant difference from the median feeding duration for mothers who reported 2 nonelective reasons for pumping.
TABLE 4.
Numbers of nonelective reasons for pumping and survival of HM-feeding durations for mothers in the imputed data set1
| Comparison, nonelective reasons for pumping compared with 0,2 n | Adjustment | HR (95% CI) | P |
| 1 | |||
| Feeding any HM | Adjusted3 | 1.12 (1.05, 1.21) | 0.001 |
| FAB | Adjusted4 | 2.07 (1.77, 2.42) | <0.0001 |
| Feeding exclusive HM | Adjusted5 | 1.14 (1.09, 1.20) | <0.0001 |
| 2 | |||
| Feeding any HM | Adjusted3 | 1.18 (1.01, 1.27) | <0.0001 |
| FAB | Adjusted4 | 2.13 (1.80, 2.52) | <0.0001 |
| Feeding exclusive HM | Adjusted5 | 1.23 (1.16, 1.30) | <0.0001 |
| 3–5 | |||
| Feeding any HM | Adjusted3 | 1.36 (1.25, 1.49) | <0.0001 |
| FAB | Adjusted4 | 3.34 (2.86, 4.04) | <0.0001 |
| Feeding exclusive HM | Adjusted5 | 1.55 (1.45, 1.65) | <0.0001 |
FAB, feeding at the breast; HM, human milk.
In all models, survival analyses were used to compare the survival HM feeding, FAB, and feeding HM exclusively between the frequency group of interest and the comparison group.
Full models were adjusted for mothers’ age, marital status (married, widowed, divorced, separated, or never married), the level of education achieved (high school or less, some college, or college or greater), and the level of satisfaction with their most-used pump (high compared with low-to-medium).
Full models were adjusted for mothers’ age, the level of education achieved (high school or less, some college, or college or greater), the level of satisfaction with their most-used pump (high compared with low-to-medium), and whether their most-used pump was used or new when they obtained it.
Full models were adjusted for mothers race/ethnicity (white, black, Asian/Pacific Islander, Hispanic, or other), BMI category (normal weight, overweight, or obese), hours worked per week on return to work (0, 1–19, 20–34, or ≥35), timing of first pumping episode, whether mothers’ most-used pumps were new or used, and mothers’ level of satisfaction with their most-used pump (high compared with low-to-medium).
Pumping practices and HM-feeding outcomes
Any pumping compared with no pumping and feeding durations
Mothers who pumped at all between 1.5 and 4.5 mo postpartum stopped feeding HM ∼6 wk before mothers did who did not pump (Table 5). Similarly, mothers who pumped also stopped FAB ∼7 wk earlier than mothers did who did not pump. Mothers who pumped at all between 1.5 and 4.5 mo postpartum were also less likely to be feeding HM or FAB at 6, 9, and 12 mo postpartum than were mothers who did not pump, and this difference widened with an increasing pumping frequency.
TABLE 5.
Reported pumping frequency between 1.5 and 4.5 mo postpartum and duration of HM-feeding practices in mothers in the imputed data set1
| Feeding any HM, mo |
FAB, mo |
Feeding exclusive HM, mo |
|||||||||||
| ≥6 | ≥9 | ≥12 | ≥6 | ≥9 | ≥12 | ≥2 | ≥4 | ≥6 | |||||
| Pumping episodes in the previous 2 wk, n | n2 | Median | % | % | % | Median | % | % | % | Median | % | % | % |
| 0 | 493 | 9.8 | 66.1 | 51.9 | 34.7 | 9.7 | 64.5 | 50.5 | 32.0 | 0.9 | 41.0 | 28.8 | 4.3 |
| Any | 1116 | 8.4 | 64.6 | 46.7 | 23.9 | 7.9 | 59.9 | 42.9 | 21.1 | 0.8 | 40.2 | 23.5 | 3.2 |
| ≤6 (less than or equal to the median) | 541 | 9.83 | 73.4 | 54.7 | 31.2 | 8.73,4 | 71.2 | 52.3 | 28.1 | 1.23,5 | 44.9 | 29.0 | 5.4 |
| 7–14 (third quartile) | 255 | 8.06 | 65.5 | 42.7 | 18.4 | 6.44,6 | 62.4 | 40.0 | 16.9 | 0.86,7 | 38.4 | 21.6 | 1.6 |
| 15–115 (fourth quartile) | 248 | 6.14,8 | 56.0 | 40.7 | 18.1 | 4.24,8 | 42.3 | 31.9 | 14.1 | 0.64,8 | 37.9 | 16.9 | 1.2 |
Median durations are reported in each group because of the large number of mothers who were right censored at or before 1 y postpartum. Percentages represent the proportion of mothers who were still feeding any HM, FAB, and feeding exclusive HM at each time point. Only mothers for whom the relevant feeding duration could be calculated or given a right-censored value were included in these calculations. Mothers who were right-censored at the study’s end for feeding HM and FAB were considered to have been feeding HM and FAB at each time point. FAB, feeding at the breast; HM, human milk.
Values represent numbers of mothers known to be in each group. Mothers were included in the group with zero pumping episodes only if they indicated that they did not pump (n = 493), and mothers for whom pumping status could not be ascertained were excluded from this group. Mothers who did not report a pumping frequency were excluded from the descriptive statistics for each pumping-frequency group.
Duration for mothers who pumped at or below the median frequency was tested for a significant difference from the median feeding duration for mothers who fed HM but did not pump between 1.5 and 4.5 mo postpartum.
Duration for mothers in this group significantly differed from the median duration for mothers in the comparison group (i.e., the group of mothers with the next-lowest number of reported nonelective reasons for pumping) (P < 0.0001).
Duration for mothers in this group significantly differed from the median duration for mothers in the comparison group (i.e., the group of mothers with the next-lowest number of reported nonelective reasons for pumping) (P < 0.01).
Duration in mothers who pumped in the third quartile of pumping frequency was tested for a significant difference from the median feeding duration in mothers who pumped at or below the median frequency.
Duration for mothers in this group significantly differed from the median duration for mothers in the comparison group (i.e., the group of mothers with the next-lowest number of reported nonelective reasons for pumping) (P = 0.02).
Duration for mothers who pumped in the fourth quartile of pumping frequency was tested for a significant difference from the median feeding duration in mothers who pumped in the third quartile of the median frequency.
Pumping frequency and feeding durations
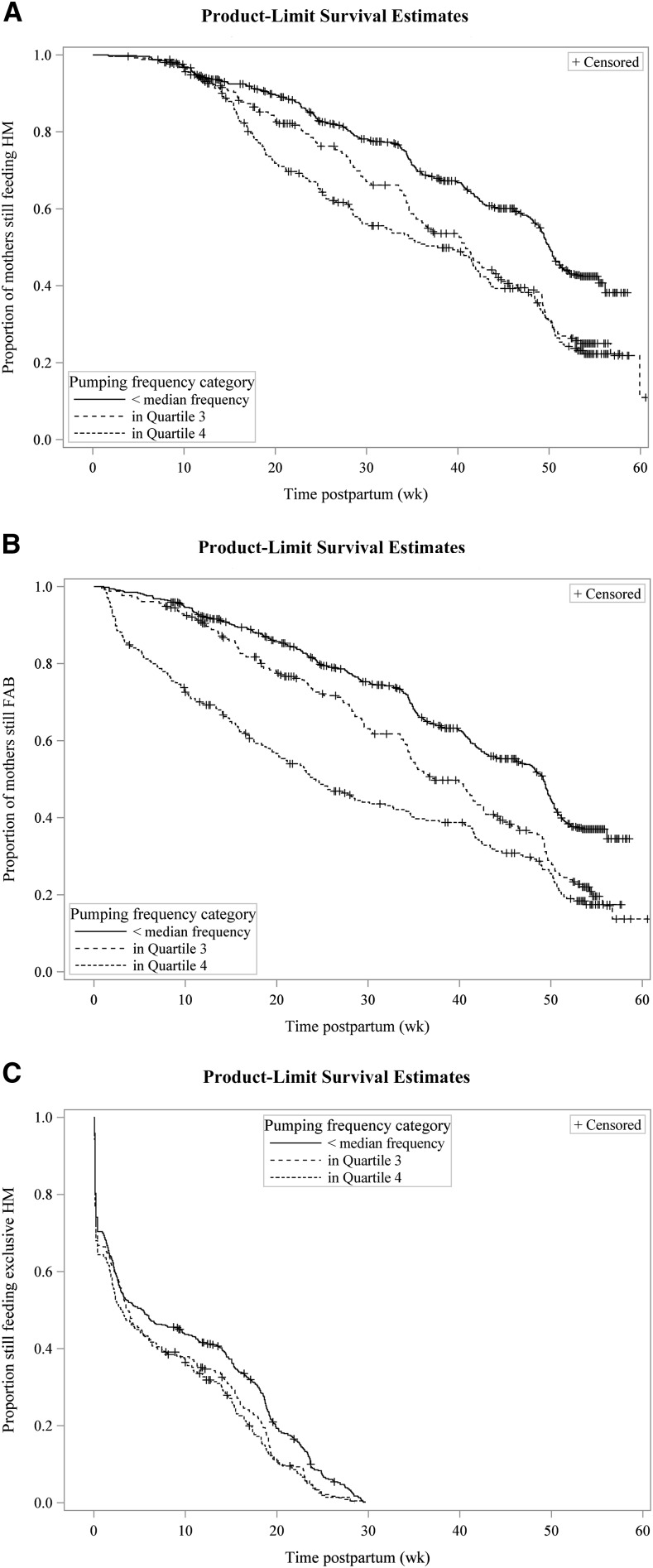
In mothers who pumped, those women who pumped at or below the median pumping frequency (6 times in the previous 2 wk) fed their HM for about as long as mothers did who did not pump but stopped FAB ∼1 mo earlier. When mothers were divided into 3 groups (i.e., women who pumped less often than the group median, women in the third quartile, and women in the top quartile), shorter HM-feeding durations were observed with an increasing pumping frequency (Figure 2). Differences between these 3 groups were more pronounced for the duration of feeding any HM (Figure 2A) and the duration of FAB (Figure 2B); these groups differed less for the duration of feeding exclusive HM (Figure 2C). Mothers in the third quartile (7–14 times in the previous 2 wk) stopped feeding their HM ∼1.8 mo earlier than mothers did who did not pump, and mothers in the fourth quartile (>14 times in the previous 2 wk) stopped feeding HM ∼3.5 mo earlier than mothers did who did not pump (Table 5). Differences between these groups were largest for FAB outcomes. Mothers in the fourth quartile stopped FAB ∼5.5 mo before mothers did who did not pump and ∼2.2 mo earlier than mothers did in the third quartile. Differences in exclusive HM-feeding outcomes were either absent or comparatively smaller.
FIGURE 2.
Pumping frequency categories between 1.5 and 4.5 mo postpartum and survival of HM-feeding practices. Unadjusted survival curves for feeding any HM (A), FAB (B), and feeding HM exclusively (C) are illustrated. Shown are mothers who pumped at a frequency below the median (≤6 times in the previous 2 wk) (solid lines), in the third quartile of pumping frequency (7–14 times in the previous 2 wk) (short-dashed lines), and in the fourth quartile of pumping frequency (15–115 times in the previous 2 wk) (long-dashed lines). FAB, feeding at the breast; HM, human milk.
Pumping frequency and duration of HM feeding
Persistence of HM feeding
In fully adjusted models that considered the pumping frequency as a categorical variable, mothers who pumped more frequently than the group median had a higher average hazard of stopping HM feeding across the year (Table 6). Mothers who pumped with the greatest frequency had the highest hazard of stopping feeding HM. In fully adjusted models in which the pumping frequency was a continuous variable, an increase of 10 pumping episodes over the previous 2 wk was associated with a greater average hazard of stopping feeding exclusive HM.
TABLE 6.
Associations between pumping practices between 1.5 and 4.5 mo postpartum and duration of any HM feeding in mothers in the imputed data set1
| Predictor | Adjustment | HR (95% CI) | P |
| Pumping frequency as a categorical exposure2 | |||
| Third quartile compared with less than or equal to the median | Unadjusted | 1.49 (1.39, 1.56) | 0.0001 |
| Fourth quartile compared with less than or equal to the median | Unadjusted | 1.74 (1.58, 1.86) | <0.0001 |
| Third quartile compared with less than or equal to the median | Adjusted3 | 1.44 (1.37, 1.52) | 0.0007 |
| Fourth quartile compared with less than or equal to the median | Adjusted3 | 1.82 (1.68, 1.93) | <0.0001 |
| Pumping frequency as a continuous exposure4 | |||
| Pumping episodes in previous 2 wk, n | Unadjusted | 1.14 (1.10, 1.18) | <0.0001 |
| Pumping episodes in previous 2 wk, n | Adjusted5 | 1.148 (1.147, 1.149) | <0.0001 |
HM, human milk.
In all models, survival analyses were used to compare the survival of HM feeding between the frequency group of interest and the comparison group.
Full models were adjusted for mothers’ age, marital status (married, widowed, divorced, separated, or never married), the level of education achieved (high school or less, some college, or college or greater), whether they worked at all between 1.5 and 4.5 mo postpartum, and the level of satisfaction with their most-used pump (high compared with low-to-medium).
HRs are presented for an increase of 10 pumping episodes in the previous 2 wk. This number of pumping episodes was chosen to reflect one additional pumping episode per workday for 2 full work weeks.
Full models were adjusted for mothers’ age, marital status (married, widowed, divorced, separated, or never married), the level of education achieved (high school or less, some college, or college or greater), and the level of satisfaction with their most-used pump (high compared with low-to-medium).
Persistence of FAB
In fully adjusted models that considered the pumping frequency as a categorical variable, the pumping frequency was associated with a shorter duration of FAB. We showed a time-dependent effect of the pumping frequency between 1.5 and 4.5 mo postpartum and the duration of FAB, which indicated that, for frequent pumpers, the hazard of stopping FAB relative to less-frequent pumpers changed across the year. Specifically, the greatest HRs were seen in the earliest months (Table 7) although the difference between groups decreased and was no longer significant by 9 mo postpartum. For example, at 3 mo postpartum, mothers who pumped most frequently had a 2.6-fold higher hazard of stopping FAB than did mothers who pumped less often than the median. However, these most-frequent pumpers did not differ from the least-frequent pumpers at 9 mo postpartum. In fully adjusted models that considered the pumping frequency as a continuous variable, an increase of 10 pumping episodes over the previous 2 wk was associated with a greater average hazard of cessation of FAB. This effect was also dependent on whether mothers reported indicators that suggested a perception of a low HM supply. Specifically, the association between an increase of 10 pumping episodes and a shorter duration of FAB was more pronounced in mothers without a perception of a low HM supply than in mothers with a perception of an adequate HM supply.
TABLE 7.
Associations between pumping practices between 1.5 and 4.5 mo postpartum and duration of FAB in mothers in imputed data set1
| Predictor2 | Adjustment | HR (95% CI) | P |
| Pumping frequency as a categorical exposure | |||
| Third quartile compared with less than or equal to the median | Unadjusted | 1.49 (1.37, 1.51) | 0.0001 |
| Fourth quartile compared with less than or equal to the median | Unadjusted | 2.03 (1.90, 2.10) | <0.0001 |
| Third quartile compared with less than or equal to the median | Adjusted3 | 1.39 (1.33, 1.45 | 0.0013 |
| Fourth quartile compared with less than or equal to the median | <0.0001 | ||
| At 3 mo postpartum | Adjusted3 | 2.60 (1.89, 3.36) | |
| At 6 mo postpartum | Adjusted3 | 1.74 (1.19, 2.47) | |
| At the median FAB duration of 7.9 mo | Adjusted3 | 1.34 (0.75, 1.82) | |
| At 9 mo postpartum | Adjusted3 | 1.16 (0.75, 2.47) | |
| Pumping frequency as a continuous exposure | |||
| Pumping episodes in previous 2 wk,4 n | Unadjusted | 1.29 (1.24, 1.34) | <0.0001 |
| Pumping episodes in previous 2 wk,4 n | <0.0001 | ||
| With low–HM-supply perception | Adjusted5,6 | 0.78 (0.77, 0.85) | |
| No low–HM-supply perception | Adjusted5,6 | 1.296 (1.293, 1.299) |
FAB, feeding at the breast; HM, human milk.
In all models, survival analyses were used to compare the survival of FAB between the frequency group of interest and the comparison group.
Full models were adjusted for mothers’ age, the level of education achieved (high school or less, some college, or college or greater), whether they worked at all between 1.5 and 4.5 mo postpartum, the level of satisfaction with their most-used pump (high compared with low-to-medium), whether their most-used pump was used or new when they obtained it, and whether they reported indicators of a perceived low HM supply.
HRs are presented for an increase of 10 pumping episodes in the previous 2 wk. This number of pumping episodes was chosen to reflect one additional pumping episode per workday for 2 full work weeks.
Full models were adjusted for whether mothers worked at all between 1.5 and 4.5 mo postpartum, the level of satisfaction with their most-used pump (high compared with low-to-medium), the level of education achieved (high school or less, some college, or college or greater), and whether they reported indicators of a perceived low HM supply.
Model also included a time-dependent effect of mothers’ continuous pumping frequency on the duration of FAB. However, the inclusion or exclusion of a covariate that represented this time-dependent effect did not substantially affect either the main effect variable or its significance. Thus, the covariate was excluded from the model for simplicity.
Persistence of exclusive HM feeding
In fully adjusted models that considered the pumping frequency as a categorical variable, mothers who pumped more frequently than the median had a greater average hazard of the cessation of exclusive HM feeding than did mothers who pumped less often (Table 8). Mothers in the fourth quartile had the highest hazard in the 3 groups of mothers but were not markedly different from mothers in third quartile. In fully adjusted models that considered the pumping frequency as a continuous variable, an increase of 10 pumping episodes in the previous 2 wk was associated with a greater average hazard of cessation of exclusive HM feeding. Again, mothers who pumped most frequently had the highest hazard of stopping HM feeding.
TABLE 8.
Associations between pumping practices between 1.5 and 4.5 mo postpartum and duration of exclusive HM feeding in mothers in the imputed data set1
| Predictor2 | Adjustment | HR (95% CI) | P |
| Pumping frequency as categorical exposure | |||
| Third quartile compared with less than or equal to the median | Unadjusted | 1.22 (1.18, 1.26) | 0.01 |
| Fourth quartile compared with less than or equal to the median | Unadjusted | 1.31 (1.24, 1.37) | 0.001 |
| Third quartile compared with less than or equal to the median | Adjusted3 | 1.17 (1.13, 1.21) | 0.06 |
| Fourth quartile compared with less than or equal to the median | Adjusted3 | 1.21 (1.14, 1.26) | 0.05 |
| Pumping frequency as continuous exposure | |||
| Pumping episodes in previous 2 wk,4 n | Unadjusted | 1.10 (1.06, 1.14) | <0.0001 |
| Pumping episodes in previous 2 wk,4 n | Adjusted5 | 1.082 (1.078, 1.084) | <0.0001 |
HM, human milk.
In all models, survival analyses were used to compare the survival of exclusive HM feeding between the frequency group of interest and the comparison group.
Full models were adjusted for mothers' race/ethnicity (white, black, Asian/Pacific Islander, Hispanic, or other), BMI category (normal weight, overweight, or obese), hours worked per week on return to work (0, 1–19, 20–34, or ≥35), timing of their pumping episode, whether mothers' most-used pumps were new or used, and mothers’ level of satisfaction with their most-used pump (high compared with low-to-medium).
HRs are presented for an increase of 10 pumping episodes in the previous 2 wk. This number of pumping episodes was chosen to reflect one additional pumping episode per workday for 2 full work weeks.
Full models were adjusted for mothers' race/ethnicity (white, black, Asian/Pacific Islander, Hispanic, or other), BMI category (normal weight, overweight, or obese), hours worked per week on return to work (0, 1–19, 20–34, or ≥35), timing of the first pumping episode, whether mothers' most-used pumps were new or used, and mothers’ level of satisfaction with their most-used pump (high compared with low-to-medium).
DISCUSSION
National recommendations, policies, and legislation have supported and promoted pumping as an equivalent means of supporting long-term HM-feeding goals when FAB is unavailable (24). However, in this epidemiologic investigation, our findings suggest that the substitution of pumping for FAB may adversely affect the duration of feeding any HM, feeding exclusive HM, and of FAB. In addition, our findings suggest that mothers who must rely on pumping nonelectively to a high degree may be particularly at risk of falling short of public health targets for HM feeding.
Our findings suggest the possibility that mothers’ reasons for pumping may drive the relation observed between the pumping frequency and the duration of HM-feeding practices. In this sample, mothers who pumped nonelectively (i.e., for reasons related to the difficulty or unavailability of FAB) stopped feeding HM exclusively and FAB earlier than did mothers who only pumped for elective reasons. The dose-response relation that we observed suggested that, as the number of nonelective reasons for pumping increased, mothers’ HM-feeding behaviors were further from public health goals. This finding lends quantitative support to our qualitative work that has been reported elsewhere (14) in which mothers who pumped out of necessity early in infancy fed HM at all and at the breast for shorter durations than did mothers who pumped only as desired. Thus, it is possible that the association between the pumping frequency and HM-feeding practices may actually have resulted from an association between pumping reasons and feeding durations. This prospect highlights the need for data that clearly distinguish between mothers’ potential reasons for pumping such that their individual effects on feeding outcomes may be assessed.
This possibility may be clearest in light of our observation that the strongest association with a higher pumping frequency was the hazard of stopping FAB. This finding was expected on the basis of our previous qualitative work. More importantly, this finding suggests the possibility that our observed links between more pumping and shorter durations of HM feeding may also reflect consequences of less FAB in early postpartum weeks. Specifically, mothers who do not successfully establish regular FAB in the early postpartum period may have more difficulty sustaining HM production for an extended period.
The shorter durations of FAB in mothers with high-frequency pumping practices in our sample raise concerns because some benefits of HM feeding are specifically linked with FAB rather than feeding HM by any method. For example, compared with bottle-feeding infant formula, mothers are more responsive to infant cues while FAB (20). Our qualitative data (14) suggest that this phenomenon is similar when bottle feeding HM is compared to FAB. Moreover, FAB is important for the optimal development of craniofacial muscles (25) and breathing patterns (26). In addition, compared with FAB, bottle-feeding pumped HM may incur independent risks to infants. Infants in the IFPS II who were bottle-fed HM were less able to regulate their intake from bottles (18), gained weight more rapidly (17), and had more episodes of coughing and wheezing (16) in their first year of life than did infants who were fed at the breast.
Taken together, these findings underscore the importance of supporting mothers in their efforts to successfully establish and maintain FAB as a means of feeding HM. For mothers who cannot or do not wish to feed at the breast, pumps are an important means of reducing risks to their own health or the health of their infants that are associated with the alternative of only feeding infant formula. However, many American mothers must maintain HM feeding while working outside the home, and most American mothers do not have the ability to have their infants with them while they work (27). Our findings suggest that these mothers who must substitute FAB with pumping episodes at a high frequency may be less likely to meet public health targets for feeding HM.
The finding that a higher pumping frequency was associated with a shorter duration of feeding HM raises concerns about infant health outcomes that drive national recommendations. Infants who are introduced to formula earlier have more gastrointestinal tract infections (28–30) and respiratory infections (31), hospitalizations for respiratory infections (32), otitis media (33), and sudden infant death syndrome (34). Limited evidence also suggests that they may be at greater risk of obesity (35–37), type II diabetes (38), cardiovascular outcomes (39, 40), and certain pediatric cancers (33). Additional research is needed to provide direct data to examine associations between mothers’ pumping practices, methods of feeding HM, and infant health.
In our analyses, we showed an association between the pumping frequency and duration of exclusive HM feeding. However, the typically short durations of exclusive HM feeding in this sample, which were observed in all pumping-frequency groups, limited the conclusions that could be drawn from these findings. For example, mothers who pumped less often than the median fed their HM exclusively only ∼2 wk longer than did mothers in the highest quartile. Thus, the between-group differences we observed may not be clinically meaningful. However, they do highlight that, even in a nonrepresentative sample with generally better HM-feeding practices than the national average, exclusive HM-feeding practices fall far short of public health targets.
The analyses reported here have 2 key limitations. First, the durations of HM feeding and FAB were estimated for some mothers across intervals that ranged from 2 to 8 mo because of missing data from unreturned surveys. This estimation introduced noise into our outcome data. However, we have no reason to believe that the actual endpoints of HM feeding and FAB in these intervals were not randomly distributed. Thus, we do not expect that the calculation of the feeding duration with the use of the midpoint of these intervals introduced bias into the duration calculations. Second, this sample was not representative of the US population. However, the IFPS II is a diverse, national sample, which permits inferences about the potential relations between pumping and HM feeding in the general population.
This analysis also had 3 key strengths. First, the longitudinal nature of the IFPS II permitted us to distinguish the impact of pumping early in infancy and measure the progression of feeding behaviors over time. Second, the use of multiple imputation to create a complete data set made our findings more robust by reducing the potential bias that could have resulted from missing data. Third, we used previous ethnographic findings (14) to inform these analyses in key ways, namely in choosing potential model covariates, testing potential mediation and moderation in survival models, and creating and examining a variable that represented mothers’ nonelective reliance on pumping. This mixed-method design lent credence to the validity of our models, findings, and conclusions.
In conclusion, taken together, our findings signal the urgency of additional investigation into the links in the determinants of pumping, pumping practices, and long-term feeding practices and health, growth, and development outcomes for infants. This signal is critical because risks to HM-feeding practices and health outcomes that may be incurred by pumping might be disproportionately borne by infants of working mothers who must rely heavily on pumps. In addition, these quantitative findings support a conclusion from our ethnographic work, namely that it is not pumping or pumps themselves that may hinder individual and national HM-feeding goals, but when mothers must pump for nonelective reasons (i.e., when FAB might be preferred but is unavailable or inadequate). Thus, our findings underscore the importance of promoting FAB nationally and supporting mothers’ efforts to feed at the breast.
Acknowledgments
We thank Francoise Vermeylen and Jason Barry of the Cornell Statistical Consulting Unit for their assistance in conceiving and executing the statistical analyses and Melissa Smith of the Department of Statistical Science at Cornell University for her help with the interpretation of the survival analyses.
The authors’ responsibilities were as follows—JPF: analyzed the data, wrote the manuscript, and had primary responsibility for the final content of the manuscript; PAC and KMR: provided regular input on conceptualization of design and statistical analyses, interpretation of results, and manuscript writing; and all authors: designed the research and read and approved the final manuscript. None of the authors reported a conflict of interest related to the study.
Footnotes
Abbreviations used: FAB, feeding at the breast; HM, human milk; IFPS II, Infant Feeding Practices Study II.
REFERENCES
- 1.Geraghty SR, Sucharew H, Rasmussen KM. Trends in breastfeeding: it is not only at the breast anymore. Matern Child Nutr 2013;9:180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rasmussen KM, Geraghty SR. The quiet revolution: breastfeeding transformed with the use of breast pumps. Am J Public Health 2011;101:1356–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geraghty SR, Rasmussen KM. Redefining “breastfeeding” initiation and duration in the age of breastmilk pumping. Breastfeed Med 2010;5:135–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Labiner-Wolfe J, Fein SB, Shealy KR, Wang C. Prevalence of breast milk expression and associated factors. Pediatrics 2008;122(Suppl 2):S63–8. [DOI] [PubMed] [Google Scholar]
- 5.Rojjanasrirat W, Sousa VD. Perceptions of breastfeeding and planned return to work or school among low-income pregnant women in the USA. J Clin Nurs 2010;19:2014–22. [DOI] [PubMed] [Google Scholar]
- 6.Thulier D, Mercer J. Variables associated with breastfeeding duration. J Obstet Gynecol Neonatal Nurs 2009;38:259–68. [DOI] [PubMed] [Google Scholar]
- 7.Kimbro RT. On-the-job moms: work and breastfeeding initiation and duration for a sample of low-income women. Matern Child Health J 2006;10:19–26. [DOI] [PubMed] [Google Scholar]
- 8.Ryan AS, Zhou W, Arensberg MB. The effect of employment status on breastfeeding in the United States. Womens Health Issues 2006;16:243–51. [DOI] [PubMed] [Google Scholar]
- 9.Lepore J. Baby food: if breast is best, why are women bottling their milk? New Yorker 2009;34–9. [PubMed] [Google Scholar]
- 10.Walker M, Auerbach K. Breast pumps and other technologies 2nd ed. Riordan J, Auerbach KG, editors. Boston: Jones and Barlett Publishers; 1998. [Google Scholar]
- 11.Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–41. [DOI] [PubMed] [Google Scholar]
- 12.US Department of Labor. Wage and Hour Division [Internet]. Fact sheet #73: Break time for nursing mothers under the FLSA. 2013. Available from: http://www.dol.gov/whd/regs/compliance/whdfs73.pdf.
- 13.Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant Feeding Practices Study II: study methods. Pediatrics. 2008;122(Suppl 2):S28–35. [DOI] [PubMed] [Google Scholar]
- 14.Felice J. A mixed methods investigation of pumping human milk and feeding pumped milk to infants [dissertation]. Ithaca (NY): Cornell University; 2015.
- 15.Johns HM, Forster DA, Amir LH, McLachlan HL. Prevalence and outcomes of breast milk expressing in women with healthy term infants: a systematic review. BMC Pregnancy Childbirth 2013;13:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soto-Ramírez N, Karmaus W, Zhang H, Davis S, Agarwal S, Albergottie A. Modes of infant feeding and the occurrence of coughing/wheezing in the first year of life. J Hum Lact 2013;29:71–80. [DOI] [PubMed] [Google Scholar]
- 17.Li R, Magadia J, Fein S, Grummer-Strawn L. Risk of bottle-feeding for rapid weight gain during the first year of life. Arch Pediatr Adolesc Med 2012;166:431–6. [DOI] [PubMed] [Google Scholar]
- 18.Li R, Fein SB, Grummer-Strawn LM. Do infants fed from bottles lack self-regulation of milk intake compared with directly breastfed infants? Pediatrics 2010;125:e1386–93. [DOI] [PubMed] [Google Scholar]
- 19.Li R, Fein SB, Grummer-Strawn LM. Association of breastfeeding intensity and bottle-emptying behaviors at early infancy with infants’ risk for excess weight at late infancy. Pediatrics 2008;122(Suppl 2):S77–84. [DOI] [PubMed] [Google Scholar]
- 20.Wright P, Fawcett J, Crow R. The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behav Processes 1980;5:1–20. [DOI] [PubMed] [Google Scholar]
- 21.Odom EC, Li R, Scanlon KS, Perrine CG, Grummer-Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baxter J, Cooklin AR, Smith J. Which mothers wean their babies prematurely from full breastfeeding? An Australian cohort study. Acta Paediatr 2009;98:1274–7. [DOI] [PubMed] [Google Scholar]
- 23.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: evidence from a cohort study. Pediatrics 2006;117:e646–55. [DOI] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau. Employees’ guide to breastfeeding and working. Every Mother, Inc. and Rich Winter Design and Multimedia; 2008. Available from: http://www.womenshealth.gov/breastfeeding/government-in-action/business-case-for-breastfeeding/employee%27s-guide-to-breastfeeding-and-working.pdf. [Google Scholar]
- 25.Narbutytė I, Narbutytė A, Linkevičienė L. Relationship between breastfeeding, bottle-feeding and development of malocclusion. Stomatologija 2013;15:67–72. [PubMed] [Google Scholar]
- 26.Limeira AB, Aguiar C, de Lima Bezerra N, Câmara A. Association between breastfeeding and the development of breathing patterns in children. Eur J Pediatr 2013;172:519–24. [DOI] [PubMed] [Google Scholar]
- 27.Fein SB, Mandal B, Roe BE. Success of strategies for combining employment and breastfeeding. Pediatrics 2008;122(Suppl 2):S56–62. [DOI] [PubMed] [Google Scholar]
- 28.Kramer MS, Guo T, Platt RW, Sevkovskaya Z, Dzikovich I, Collet J-P, Shapiro S, Chalmers B, Hodnett E, Vanilovich I, et al. Infant growth and health outcomes associated with 3 compared with 6 mo of exclusive breastfeeding. Am J Clin Nutr 2003;78:291–5. [DOI] [PubMed] [Google Scholar]
- 29.Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, Collet J-P, Vanilovich V, Mknuik D, Gluchanina E, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 2001;285:413–20. [DOI] [PubMed] [Google Scholar]
- 30.Chien PF, Howie P. Breast milk and the risk of opportunistic infection in infancy in industrialized and non-industrialized settings. Adv Nutr Res 2001;10:69–104. [DOI] [PubMed] [Google Scholar]
- 31.Duijts L, Jaddoe V, Hofman A, Moll H. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics 2010;126:e18–25. [DOI] [PubMed] [Google Scholar]
- 32.Bachrach VR, Schwarz E, Bachrach L. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: a meta-analysis. Arch Pediatr Adolesc Med 2003;157:237–43. [DOI] [PubMed] [Google Scholar]
- 33.Ip S, Chung M, Raman G, Trikalinos T, Lau J. A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeed Med 2009;4(Suppl 1):S17–30. [DOI] [PubMed] [Google Scholar]
- 34.Hauck FR, Thompson JMD, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics 2011;128:103–10. [DOI] [PubMed] [Google Scholar]
- 35.Arenz S, von Kries R. Protective effect of breastfeeding against obesity in childhood Koletzko B, Dodds P, Akerblom H, Ashwell M, editors. Early nutrition and its later consequences: new opportunities Dordrecht (Netherlands): Springer Netherlands; 2005. p. 40–8. [Google Scholar]
- 36.Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol 2005;162:397–403. [DOI] [PubMed] [Google Scholar]
- 37.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics 2005;115:1367–77. [DOI] [PubMed] [Google Scholar]
- 38.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Does breastfeeding influence risk of type 2 diabetes in later life? A quantitative analysis of published evidence. Am J Clin Nutr 2006;84:1043–54. [DOI] [PubMed] [Google Scholar]
- 39.Owen CG, Whincup PH, Cook DG. Breast-feeding and cardiovascular risk factors and outcomes in later life: evidence from epidemiological studies. Proc Nutr Soc 2011;70:478–84. [DOI] [PubMed] [Google Scholar]
- 40.Owen CG, Whincup PH, Odoki K, Gilg JA, Cook DG. Infant feeding and blood cholesterol: a study in adolescents and a systematic review. Pediatrics 2002;110:597–608. [DOI] [PubMed] [Google Scholar]