Abstract
BACKGROUND
A report from a high-volume single center indicated a survival benefit of receiving a kidney transplant from an HLA-incompatible live donor as compared with remaining on the waiting list, whether or not a kidney from a deceased donor was received. The generalizability of that finding is unclear.
METHODS
In a 22-center study, we estimated the survival benefit for 1025 recipients of kidney transplants from HLA-incompatible live donors who were matched with controls who remained on the waiting list or received a transplant from a deceased donor (waiting-list-or-transplant control group) and controls who remained on the waiting list but did not receive a transplant (waiting-list-only control group). We analyzed the data with and without patients from the highest-volume center in the study.
RESULTS
Recipients of kidney transplants from incompatible live donors had a higher survival rate than either control group at 1 year (95.0%, vs. 94.0% for the waiting-list-or-transplant control group and 89.6% for the waiting-list-only control group), 3 years (91.7% vs. 83.6% and 72.7%, respectively), 5 years (86.0% vs. 74.4% and 59.2%), and 8 years (76.5% vs. 62.9% and 43.9%) (P<0.001 for all comparisons with the two control groups). The survival benefit was significant at 8 years across all levels of donor-specific antibody: 89.2% for recipients of kidney transplants from incompatible live donors who had a positive Luminex assay for anti-HLA antibody but a negative flow-cytometric cross-match versus 65.0% for the waiting-list-or-transplant control group and 47.1% for the waiting-list-only control group; 76.3% for recipients with a positive flow-cytometric cross-match but a negative cytotoxic cross-match versus 63.3% and 43.0% in the two control groups, respectively; and 71.0% for recipients with a positive cytotoxic cross-match versus 61.5% and 43.7%, respectively. The findings did not change when patients from the highest-volume center were excluded.
CONCLUSIONS
This multicenter study validated single-center evidence that patients who received kidney transplants from HLA-incompatible live donors had a substantial survival benefit as compared with patients who did not undergo transplantation and those who waited for transplants from deceased donors. (Funded by the National Institute of Diabetes and Digestive and Kidney Diseases.)
More than 32,000 patients awaiting kidney transplantation in the United States have anti-HLA antibodies.1 The presence of anti-HLA antibodies makes it very difficult to find a match with a compatible donor, and these “sensitized” patients can remain on the waiting list for a kidney transplant for years without a suitable donor ever being identified.2,3 Those fortunate enough to have a willing but incompatible live donor can either participate in paired kidney donation, for which the chance of a compatible match is also limited,4–9 or undergo desensitization and subsequent transplantation with a kidney from an incompatible live donor.10–22
Several centers have reported that outcomes after transplantation with a kidney from an incompatible live donor were inferior to outcomes after transplantation with a kidney from a compatible live donor,11,23,24 and we recently confirmed those findings in a 22-center cohort study.25 Since HLA incompatibilities are not accounted for in case-mix–adjusted benchmarks, centers performing transplantations with kidneys from incompatible donors may be subjected to regulatory scrutiny and loss of Centers for Medicare and Medicaid Services certification. Given such pressures, many centers have avoided transplanting kidneys from incompatible live donors. However, for most sensitized patients, receiving a compatible kidney is not an option: their choice is to undergo desensitization or remain on the waiting list, which is associated with a high mortality rate. In other words, it may be in the best interest of the individual patient to receive a transplant from an incompatible donor, even though the success rate is lower for such transplants than for those from compatible donors.
Thus, it is critical to determine whether there is a survival benefit from undergoing desensitization and transplantation with a kidney from an incompatible live donor. Three of us previously reported a survival benefit for desensitization at a single large center (Johns Hopkins University).19 However, at this center, a very high volume of transplantations with kidneys from incompatible live donors are performed, and it was unclear whether our results were generalizable. To quantify the effect of transplantation with kidneys from incompatible live donors on survival among patients at transplantation centers across the United States, we compared recipients of such transplants in a multicenter cohort with carefully matched controls who remained on the waiting list for a kidney transplant.
METHODS
STUDY DESIGN AND OVERSIGHT
The study was designed by the first author and the last two authors. All the study investigators gathered the data, which were analyzed by the first three authors and the last author. The first and last authors wrote the manuscript and vouch for the accuracy and completeness of the data and analysis and the fidelity of the study to the protocol, which is available with the full text of this article at NEJM.org. All the authors made the decision to submit the manuscript for publication. The sponsors did not place confidentiality restrictions on any of the authors or institutions involved in this study.
STUDY POPULATION AND DEFINITIONS
The study population consisted of adults (≥18 years of age) who underwent kidney-only transplantation with transplants from HLA-incompatible live donors performed at 22 transplantation centers in the United States between 1997 and 2011 (for the list of centers, see Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org), as well as matched controls drawn from the Scientific Registry of Transplant Recipients (SRTR). The SRTR data system includes data on all donors, wait-listed candidates for transplants, and transplant recipients in the United States, submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration, Department of Health and Human Services, provides oversight of the activities of the OPTN and SRTR contractors. Some of the data reported here have been supplied by the Minneapolis Medical Research Foundation (MMRF) as the contractor for the SRTR.
Recipients of kidney transplants from HLA-incompatible live donors were defined as those undergoing perioperative desensitization therapy for donor-specific antibodies detected before transplantation, as previously defined.25 Briefly, each participating transplantation center classified the donor-specific antibody level as low, moderate, or high before administering the desensitization protocol of the center’s own choosing. A positive Luminex assay (a sensitive assay for donor-specific anti-HLA antibody) with a negative flow-cytometric cross-match indicated a low donor-specific antibody level, a positive flow-cytometric assay with a negative cytotoxic cross-match indicated a moderate antibody level, and a positive cytotoxic cross-match indicated a high antibody level (Table 1). Patients with anti-HLA donor-specific antibodies who were also ABO-incompatible (5.8% of the cohort) were included and categorized on the basis of their anti-HLA donor-specific antibody level, in light of the minimal risk associated with crossing ABO barriers.26,27
Table 1.
Antibody-Detection Methods and Sensitivity.*
| Assay | Method |
|---|---|
| Cytotoxic cross-match | Donor lymphocytes, recipient serum, and complement are added together. If serum from the recipient contains donor-specific anti-HLA antibody at a level sufficient to kill recipient cells, it is called a positive cross-match. This requires a high level of antibody. |
| Flow-cytometric cross-match | Donor lymphocytes, recipient serum, and fluorescein-labeled antibodies against human IgG are mixed together. If recipient serum contains moderate levels of donor-specific anti-HLA antibody, it will be detected by flow cytometer and is called a positive flow-cytometric cross-match. Flow cytometry detects a moderate level of antibody. |
| Luminex antibody testing | Recipient serum is run through a column of beads coated with a wide range of polymorphic HLA molecules tagged with unique, identifying immunofluorescence. If recipient serum contains donor-specific anti-HLA antibody, even at a very low level, it can be detected by the Luminex assay. |
The assays are listed in order from least sensitive (requires high levels of antibody for a positive result) to most sensitive (can detect low levels of antibody).
DATA LINKAGE
Data provided by the participating transplantation centers were linked to the SRTR for ascertainment of additional patient and donor characteristics and for reliable ascertainment of deaths. The SRTR supplements death ascertainment through linkage to Medicare data and the Social Security Death Master File.
WAIT-LISTED MATCHED CONTROLS
Two sets of matched controls were drawn from the SRTR waiting list. The first group consisted of wait-listed patients, some of whom subsequently received a transplant from a deceased donor (waiting-list-or-transplant control group). The second group consisted of wait-listed patients who never underwent kidney transplantation (waiting-list-only control group). Controls in the waiting-list-or-transplant group were drawn from a pool of 349,844 unique patients, and controls in the waiting-list-only group were drawn from a pool of 200,769 unique patients. The waiting-list-or-transplant group was selected to compare transplantation with a kidney from an incompatible live donor with the next best real-world treatment option (i.e., continuing to be wait-listed for a transplant). The waiting-list-only group was selected to quantify the possible survival benefit associated with transplantation of a kidney from an incompatible live donor.
For each recipient of a kidney from an incompatible live donor, five matched controls were drawn from the waiting-list-or-transplant group, and five were drawn from the waiting-list-only group. Matching was performed with the use of an iterative, expanding-radius matching algorithm, as previously described19,28–32 (for details, see the Methods section in the Supplementary Appendix). For panel-reactive antibody matching, peak values were determined, with the use of calculated panel-reactive antibody when available. Among recipients of kidneys from incompatible live donors, those with a panel-reactive antibody level of 100% were matched only to controls with an antibody level of 100%, and those with an antibody level of 98 to 99% or 95 to 97% were matched to controls with antibody levels in the same range. Recipients with a panel-reactive antibody level of 85 to 94% were matched to controls with a panel-reactive antibody level in the same range plus or minus 2 percentage points, those with an antibody level of 65 to 84% were matched to controls with a level in the same range plus or minus 5 percentage points, and those with an antibody level of 1 to 64% were matched to controls with a level in the same range plus or minus 10 percentage points but higher than 0%. Recipients with a panel-reactive antibody level of 0% were matched to controls with a level of exactly 0%.
Patients who had not received renal-replacement therapy before undergoing transplantation with a kidney from an incompatible live donor were matched to eligible controls who had received renal-replacement therapy for 3 months or less. Patients who had received renal-replacement therapy for any length of time before undergoing transplantation with a kidney from an incompatible live donor were matched to controls receiving renal-replacement therapy within a radius of 1 year but were not matched to controls who had not received any renal-replacement therapy. Recipients of kidneys from incompatible live donors were matched exactly to controls for age, blood group, number of previous kidney transplantations, race, sex, and diabetes status; they were also matched for the percentage of time with a functioning kidney transplant during renal-replacement therapy (plus or minus 10 percentage points) and for the transplantation date, which was matched to the date of placement on the waiting list (within 30 days).
In the event that a sufficient number of controls could not be found for a given transplant recipient with the use of the strict criteria described above, we relaxed the criteria as follows, and in the following order, until five matches were found: by expanding the allowable age difference 1 year at a time for up to 5 years; ignoring blood-group differences; expanding the allowable difference in the number of previous kidney transplantations one at a time until it was necessary to ignore any differences; further expanding the allowable age difference 1 year at a time up to 10 years; expanding the allowable difference in the percentage of time receiving renal-replacement therapy with a functioning kidney transplant 5% at a time up to 60%; further expanding the allowable age difference 1 year at a time for up to 15 years; expanding the allowable difference in the duration of renal-replacement therapy 1 year at a time for up to 4 years; further expanding the allowable age difference 1 year at a time for up to 35 years; further expanding the duration of renal-replacement therapy 1 year at a time for up to 10 years; ignoring differences in race, sex, and then diabetes status; and expanding the allowable difference between the transplantation date and the date of placement on the waiting list for controls 1 month at a time for up to 60 months. Every time the secular-difference radius was expanded, all other radii were reset to their initial (restrictive) settings, and matches were sought with the new secular-difference radius.
MISSING DATA
In the case of missing data on panel-reactive antibody levels for recipients of transplants from incompatible live donors (accounting for 6.7% of all such recipients), we used the mean panel-reactive antibody level for each level of donor-specific antibody among recipients for whom such data were available. All other variables were missing in less than 1% of the recipients of transplants from incompatible live donors. Controls with missing data on any matching variables were excluded.
STATISTICAL ANALYSIS
We used Pearson’s chi-square test to compare categorical variables between groups, and we used the Somers D rank statistic test for comparisons of continuous variables to account for clustering.33–35 Mortality was estimated with the use of the Kaplan–Meier method and was compared between groups by means of Cox modeling with shared frailty, a modeling method that accounted for the clustering of the matched controls to the recipients of transplants from incompatible live donors.36 Comparisons with the matched controls were performed separately for each control group. A two-tailed P value of less than 0.05 was considered to indicate statistical significance. Administrative censoring of data was performed for patients who were alive at the end of the study (March 2014). Given that patients at the highest-volume center (Johns Hopkins University) accounted for 25.8% of the cohort, a sensitivity analysis was performed in which data from this center were excluded. Statistical analysis was performed with the use of Stata software, version 13.0 (StataCorp).
RESULTS
RECIPIENTS OF TRANSPLANTS FROM INCOMPATIBLE LIVE DONORS
We enrolled 1025 patients at 22 centers who received kidney transplants from incompatible live donors: 185 with a positive Luminex assay but a negative flow-cytometric cross-match, 536 with a positive flow-cytometric cross-match but a negative cytotoxic cross-match, and 304 with a positive cytotoxic cross-match (Table 2). The mean age was 45.4, 45.5, and 43.8 years among recipients with a positive Luminex assay, those with a positive flow-cytometric cross-match, and those with a positive cytotoxic cross-match, respectively. The majority of patients were women (125 [67.6%], 365 [68.1%], and 197 [64.8%] in the three subgroups, respectively), 413 (40.3%) had previously received a kidney transplant (60 [32.4%], 204 [38.1%], and 149 [49.0%] in the three subgroups), and 168 (16.4%) were black (32 [17.3%], 100 [18.7%], and 36 [11.8%] in the three subgroups). The median percentage of panel-reactive antibody was 51.0% among recipients with a positive Luminex assay, 57.5% among those with a positive flow-cytometric cross-match, and 85.0% among those with a positive cytotoxic cross-match, and the mean duration of renal-replacement therapy was 5.6, 6.9, and 9.0 years, respectively.
Table 2.
Characteristics of Recipients of Kidney Transplants from HLA-Incompatible Live Donors, According to the Donor-Specific Antibody Level.*
| Characteristic | Recipients of Transplants from Incompatible Live Donors | |||
|---|---|---|---|---|
| Total (N = 1025) | Positive Luminex Assay but Negative Flow-Cytometric Cross-Match (N = 185) | Positive Flow-Cytometric Cross-Match but Negative Cytotoxic Cross-Match (N = 536) | Positive Cytotoxic Cross-Match (N = 304) | |
| Age at transplantation — yr | 45.0±12.8 | 45.4±12.7 | 45.5±12.6 | 43.8±13.2 |
| Female sex — no. (%) | 687 (67.0) | 125 (67.6) | 365 (68.1) | 197 (64.8) |
| Black race — no. (%)† | 168 (16.4) | 32 (17.3) | 100 (18.7) | 36 (11.8) |
| Previous kidney transplant — no. (%) | 413 (40.3) | 60 (32.4) | 204 (38.1) | 149 (49.0) |
| Panel-reactive antibody | ||||
| Median (IQR) — % | 66 (22–94) | 51 (18–82) | 57.5 (14–93) | 85 (50–98) |
| 0–20% — no. (%) | 254 (24.8) | 49 (26.5) | 169 (31.5) | 36 (11.8) |
| 21–50% — no. (%) | 160 (15.6) | 41 (22.2) | 78 (14.6) | 41 (13.5) |
| 51–80% — no. (%) | 198 (19.3) | 48 (25.9) | 90 (16.8) | 60 (19.7) |
| >80% — no. (%) | 413 (40.3) | 47 (25.4) | 199 (37.1) | 167 (54.9) |
| Diabetes mellitus — no. (%) | 210 (20.5) | 47 (25.4) | 119 (22.2) | 44 (14.5) |
| Duration of renal-replacement therapy — yr | 7.3±7.6 | 5.6±6.9 | 6.9±7.7 | 9.0±7.5 |
| Donor age — yr | 40.7±11.6 | 41.6±11.3 | 40.5±11.7 | 40.5±11.8 |
Plus–minus values are means ±SD. IQR denotes interquartile range.
Race was determined by staff at the transplant centers.
MATCHED CONTROLS
The mean age of the overall group of patients who received kidney transplants from incompatible live donors was 45.0 years, as compared with 45.9 years in the group of matched controls who remained on the waiting list or received a transplant from a deceased donor (P = 0.07) and 46.6 years in the group of matched controls who remained on the waiting list and never underwent kidney transplantation; the difference in mean age between the recipients of transplants from incompatible live donors and the waiting-list-only control group, although clinically negligible, was significant (P=0.001) (Table 3). Recipients of transplants from incompatible live donors had a history of slightly more kidney transplants than the waiting-list-or-transplant control group (P = 0.004) or the waiting-list-only control group (P = 0.02). There were no significant between-group differences in sex, black race, percentage of panel-reactive antibody, diabetes status, or mean number of years of renal-replacement therapy. In the waiting-list-or-transplant control group, 2326 controls (45.4%) ultimately received a kidney transplant from a deceased donor. The mean (±SD) follow-up time for these patients was 7.3±2.8 years from the time of matching and 5.0±3.0 years from the time of transplantation. Among patients in the waiting-list-or-transplant control group who did not receive a transplant, the follow-up time was 4.8±3.0 years from the time of matching.
Table 3.
Characteristics of Recipients of Transplants from HLA-Incompatible Live Donors as Compared with Matched Controls.*
| Characteristic | Recipients of Transplants from Incompatible Live Donors (N = 1025) | Waiting-List-or-Transplant Control Group (N = 5125) | Waiting-List-Only Control Group (N = 5125) |
|---|---|---|---|
| Age at transplantation — yr† | 45.0±12.8 | 45.9±12.1 | 46.6±12.0 |
| Female sex — no. (%) | 687 (67.0) | 3444 (67.2) | 3452 (67.4) |
| Black race — no. (%)‡ | 168 (16.4) | 844 (16.5) | 840 (16.4) |
| No. of previous kidney transplants — no. of patients (%)§ | |||
| 0 | 612 (59.7) | 3323 (64.8) | 3321 (64.8) |
| 1 | 350 (34.1) | 1584 (30.9) | 1552 (30.3) |
| 2 | 57 (5.6) | 202 (3.9) | 231 (4.5) |
| ≥3 | 6 (0.6) | 16 (0.3) | 21 (0.4) |
| Median panel-reactive antibody (IQR) — % | 66 (22–94) | 68 (20–95) | 68 (21–95) |
| Diabetes mellitus — no. (%) | 210 (20.5) | 1047 (20.4) | 1047 (20.4) |
| Duration of renal-replacement therapy — yr | 7.3±7.6 | 7.3±7.4 | 7.4±7.4 |
Plus–minus values are means ±SD. There were no significant between-group differences in baseline characteristics except as noted.
P = 0.02 for the comparison between patients who received transplants from incompatible live donors and patients in the waiting-list-only control group.
Race was determined by staff at the transplant centers.
P = 0.004 for the comparison between patients who received transplants from incompatible live donors and patients in the waiting-list-or-transplant control group.
SURVIVAL
Recipients of kidney transplants from incompatible live donors had a significant survival benefit as compared with the waiting-list-or-transplant control group and the waiting-list-only control group (P<0.001 for both comparisons) (Fig. 1). The survival rate was higher for recipients of transplants from incompatible live donors at 1 year (95.0%, vs. 94.0% for the waiting-list-or-transplant control group and 89.6% for the waiting-list-only control group), 3 years (91.7% vs. 83.6% and 72.7%, respectively), 5 years (86.0% vs. 74.4% and 59.2%), and 8 years (76.5% vs. 62.9% and 43.9%) (Table 4). In other words, receiving a kidney from an incompatible live donor was associated with an absolute increase of 13.6 percentage points in the survival rate at 8 years, as compared with remaining on the waiting list or receiving a transplant from a deceased donor (risk of death reduced by a factor of 1.83; 95% confidence interval [CI], 1.58 to 2.12; P<0.001) and an absolute increase of 32.6 percentage points, as compared with remaining on the waiting list and not receiving a transplant from a deceased donor (risk reduced by a factor of 3.37; 95% CI, 2.92 to 3.90; P<0.001).
Figure 1. Overall Comparison of Survival between the Group That Received Kidney Transplants from HLA-Incompatible Live Donors and Each Group of Matched Controls.
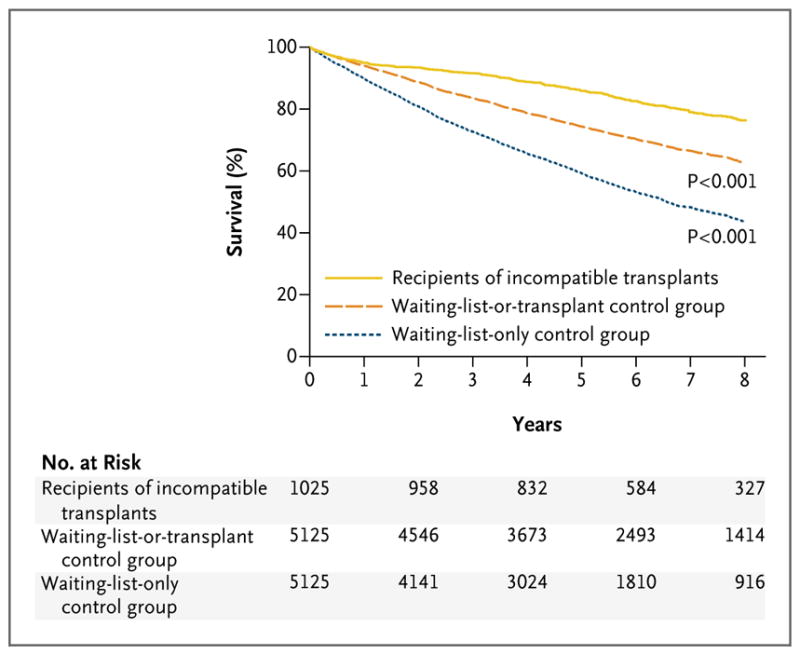
In one control group, the controls remained on the waiting list or received a transplant from a deceased donor. In the other control group, controls remained on the waiting list and did not receive a transplant from a deceased donor.
Table 4.
Kaplan–Meier Survival Estimates for Recipients of Kidney Transplants from Incompatible Live Donors and Matched Controls.*
| Year | Patients Who Survived
|
||
|---|---|---|---|
| Recipients of Transplants from Incompatible Live Donors (N = 1025) | Waiting-List-or-Transplant Control Group (N = 5125) | Waiting-List-Only Control Group (N = 5125) | |
| percent (95% confidence interval) | |||
| 1 | 95.0 (93.5–96.2) | 94.0 (93.3–94.6) | 89.6 (88.8–90.4) |
|
| |||
| 2 | 93.5 (91.8–94.8) | 88.7 (87.8–89.5) | 80.8 (79.7–81.8) |
|
| |||
| 3 | 91.7 (89.8–93.2) | 83.6 (82.5–84.6) | 72.7 (71.5–73.9) |
|
| |||
| 4 | 88.8 (86.7–90.6) | 78.6 (77.4–79.7) | 65.5 (64.2–66.8) |
|
| |||
| 5 | 86.0 (83.6–88.0) | 74.4 (73.1–75.6) | 59.2 (57.8–60.6) |
|
| |||
| 6 | 82.6 (80.0–85.0) | 70.3 (69.0–71.6) | 53.2 (51.7–54.6) |
|
| |||
| 7 | 79.1 (76.1–81.7) | 66.6 (65.1–67.9) | 48.3 (46.8–49.8) |
|
| |||
| 8 | 76.5 (73.3–79.3) | 62.9 (61.4–64.4) | 43.9 (42.3–45.4) |
P<0.001 for the overall comparison of survival among recipients of transplants from incompatible live donors with survival in each of the control groups, on the basis of a Cox shared-frailty model.
SURVIVAL BENEFIT AND CROSS-MATCH STRENGTH
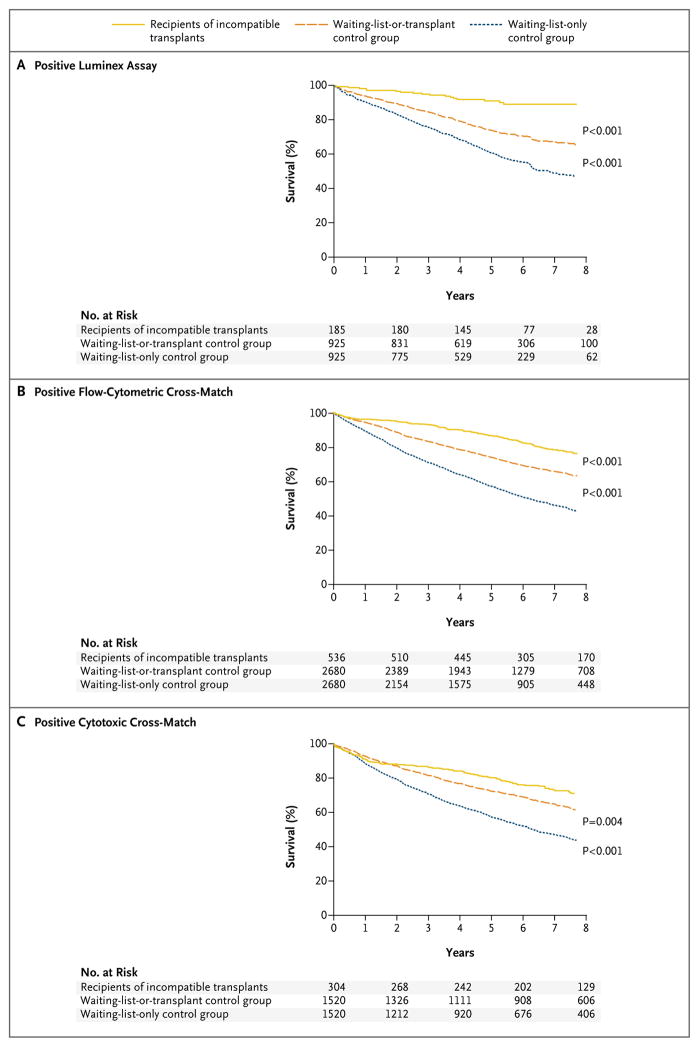
Receipt of a kidney transplant from an incompatible live donor was associated with a survival benefit at all donor-specific antibody levels. Recipients with a positive Luminex assay but a negative flow-cytometric cross-match (185 recipients, or 18.0% of the cohort) had higher survival rates than either group of controls at 1 year (98.4%, vs. 94.0% for the waiting-list-or-transplant group and 90.6% for the waiting-list-only group), 3 years (95.1% vs. 85.2% and 76.3%, respectively), 5 years (91.2% vs. 74.6% and 61.9%), and 8 years (89.2% vs. 65.0% and 47.1%) (P<0.001 for the overall comparison of survival between the group that received transplants from incompatible live donors and each of the control groups) (Fig. 2A). The survival rate for the transplant recipients with a positive Luminex assay exceeded the rate for the waiting-list-or-transplant control group beginning at 1 month, and the survival curves never crossed for the comparison between the transplants recipients with a positive Luminex assay and the waiting-list-only control group. At 8 years, the survival rate for transplant recipients with a positive Luminex assay but a negative flow-cytometric cross-match was increased by 24.2 percentage points as compared with the rate for the waiting-list-or-transplant control group (risk of death reduced by a factor of 3.49; 95% CI, 2.13 to 5.70; P<0.001) and was increased by 42.1 percentage points as compared with the rate in the waiting-list-only control group (risk reduced by a factor of 6.48; 95% CI, 3.98 to 10.56; P<0.001).
Figure 2. Survival Benefit for Recipients of Kidney Transplants from HLA-Incompatible Live Donors as Compared with the Two Groups of Matched Controls, According to Donor-Specific Antibody Level.
The survival benefit is shown for transplant recipients who had a positive Luminex assay but a negative flow-cytometric cross-match (Panel A), those who had a positive flow-cytometric cross-match but a negative cytotoxic cross-match (Panel B), and those who had a positive cytotoxic cross-match (Panel C).
Transplant recipients with a positive flow-cytometric cross-match but a negative cytotoxic cross-match (536 recipients, or 52.3% of the cohort) had higher survival rates at 1 year (96.1%, vs. 94.5% for the waiting-list-or-transplant control group and 89.7% for the waiting-list-only control group), 3 years (93.3% vs. 83.8% and 72.1%, respectively), 5 years (87.1% vs. 74.9% and 58.4%), and 8 years (76.3% vs. 63.3% and 43.0%) (P<0.001 for the overall comparison of survival between the group that received transplants from incompatible live donors and each of the control groups) (Fig. 2B). The survival rate for this group of transplant recipients exceeded the rates in the waiting-list-or-transplant control group and the waiting-list-only control group beginning at 2.2 months and 0.02 months, respectively. At 8 years, the survival rate among transplant recipients with a positive flow-cytometric cross-match but a negative cytotoxic cross-match was increased by 13.0 percentage points as compared with the rate in the waiting-list-or-transplant control group (risk of death reduced by a factor of 1.89; 95% CI, 1.54 to 2.33; P<0.001) and was increased by 33.3 percentage points as compared with the rate in the waiting-list-only control group (risk reduced by a factor of 3.56; 95% CI, 2.90 to 4.36; P<0.001).
Transplant recipients with a positive cytotoxic cross-match (304 recipients, or 29.7% of the cohort) had a survival rate at 1 year that was similar to the rates in the waiting-list-or-transplant and waiting-list-only control groups (91.1%, 93.0%, and 88.9% in the three groups, respectively) but had higher survival rates at 3 years (86.8%, vs. 82.2% and 71.8% in the two control groups, respectively), 5 years (80.9% vs. 73.2% and 58.8%), and 8 years (71.0% vs. 61.5% and 43.7%) (P<0.001 for the overall comparison of survival between the group that received transplants from incompatible live donors and each of the control groups) (Fig. 2C). The survival rate for transplant recipients with a positive cytotoxic cross-match exceeded the rates for the waiting-list-or-transplant and waiting-list-only control groups beginning at 21.7 months and 4.8 months, respectively. At 8 years, the survival rate for transplant recipients with a positive cytotoxic cross-match was increased by 9.5 percentage points as compared with the rate for the waiting-list-or-transplant control group (risk of death reduced by a factor of 1.41; 95% CI, 1.12 to 1.79; P = 0.004) and was increased by 27.3 percentage points as compared with the rate for the waiting-list-only control group (risk reduced by a factor of 2.50; 95% CI, 1.99 to 3.15; P<0.001).
SENSITIVITY ANALYSIS
The results were similar in an analysis that excluded patients from the highest-volume center. The survival rate after receipt of a kidney transplant from an incompatible live donor was similar to the rate in the primary analysis (P = 0.57), as were the rates for the matched controls (P = 0.98 for the waiting-list-or-transplant control group and P = 0.38 for the waiting-list-only control group) (Table S2 in the Supplementary Appendix). Similarly, receipt of a transplant from an incompatible live donor was associated with reductions in the risk of death that were similar to the reductions in the primary analysis for the comparisons with the waiting-list-or-transplant control group (risk reduced by a factor of 1.95; 95% CI, 1.64 to 2.32; P<0.001) and the waiting-list-only control group (risk reduced by a factor of 3.71; 95% CI, 3.13 to 4.40; P<0.001) (Fig. S2 in the Supplementary Appendix).
DISCUSSION
In the present study, receipt of a kidney transplant from an incompatible live donor was associated with a significant survival benefit as compared with the other options available to sensitized patients, with absolute increases in the 8-year survival rate of 13.6 and 32.6 percentage points as compared with the respective rates among controls who remained on the waiting list or received a transplant from a deceased donor (risk of death reduced by a factor of 1.83) and controls who remained on the waiting list and did not receive a transplant from a deceased donor (risk of death reduced by a factor of 3.37). This survival benefit was seen across all donor-specific antibody levels. Survival rates were increased by 24.2 and 42.1 percentage points as compared with the respective rates in the waiting-list-or-transplant and waiting-list-alone control groups (risk of death reduced by a factor of 3.49 and by a factor of 6.48, respectively) for transplant recipients with a positive Luminex assay but a negative flow-cytometric cross-match, by 13.0 and 33.3 percentage points (risk reduced by a factor of 1.89 and by a factor of 3.56) for those with a positive flow-cytometric cross-match but a negative cytotoxic cross-match, and by 9.5 and 27.3 percentage points (risk reduced by a factor of 1.41 and by a factor of 2.50) for those with a positive cytotoxic cross-match. The results of an analysis that excluded patients from the highest-volume center were consistent with these findings.
Previously reported outcomes for patients receiving a kidney transplant from an incompatible live donor at one center, Johns Hopkins University,19 included a survival rate of 80.6% at 8 years as compared with 76.5% in the present multi-center study. The single-center results were similar to the results of this multicenter study when stratified according to the donor-specific antibody level, with a 4-year survival rate of 90.8% in the single-center study and an 8-year survival rate of 89.2% in the multicenter study for transplant recipients with a positive Luminex assay; 8-year survival rates of 79.7% and 76.3% in the single-center and multicenter studies, respectively, for recipients with a positive flow-cytometric cross-match; and 8-year survival rates of 78.0% and 71.0%, respectively, for recipients with a positive cytotoxic cross-match. These findings suggest that the outcomes of transplantation with kidneys from incompatible live donors are generalizable from a single center that provides specialized care for sensitized patients to multiple centers performing such transplantations.
The strengths of the current study include its multicenter design (22 centers), large sample (1025 recipients of kidneys from incompatible live donors), and robust matching of the transplant recipients with controls. One limitation of the study is the heterogeneity in antibody testing and in the interpretation of test results among the centers.37–40 We accounted for these differences by including only transplant recipients who underwent perioperative desensitization — that is, only patients considered by the centers to have a large enough donor-specific antibody burden to warrant desensitization — and by asking the centers to classify the donor-specific antibody level on the basis of the decreasing relative sensitivities of the Luminex assay, flow-cytometric cross-match testing, and cytotoxic cross-match testing. A second limitation is the change in the measure of sensitization in 2009, when the calculated panel-reactive antibody supplanted the traditional panel-reactive antibody system. However, since we matched controls according to the transplantation date for the transplant recipients, equivalent systems of measuring panel-reactive antibody were used for recipients of kidneys from incompatible live donors and their matched controls. Finally, desensitization protocols and their success rates, induction and maintenance immunosuppressive regimens, and treatment of antibody-mediated rejection vary across centers, and our study was not designed to assess those differences. The likelihood of substantial heterogeneity in these practices among the centers enhances the external validity of the survival benefit with transplantation of kidneys from incompatible live donors in clinical settings other than that of a single, specialized, high-volume center.19
Supplementary Material
Acknowledgments
Supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK098431 and K24DK10182801, to Dr. Segev; F32DK093218, to Dr. Orandi; and RC1DK086731, to Dr. Montgomery).
APPENDIX
The authors’ full names and academic degrees are as follows: Babak J. Orandi, M.D., Ph.D., Xun Luo, M.D., M.P.H., Allan B. Massie, Ph.D., Jacqueline M. Garonzik-Wang, M.D., Ph.D., Bonne E. Lonze, M.D., Ph.D., Rizwan Ahmed, M.D., Kyle J. Van Arendonk, M.D., Ph.D., Mark D. Stegall, M.D., Stanley C. Jordan, M.D., Jose Oberholzer, M.D., Ty B. Dunn, M.D., Lloyd E. Ratner, M.D., M.P.H., Sandip Kapur, M.D., Ronald P. Pelletier, M.D., John P. Roberts, M.D., Marc L. Melcher, M.D., Ph.D., Pooja Singh, M.D., Debra L. Sudan, M.D., Marc P. Posner, M.D., Jose M. El-Amm, M.D., Ron Shapiro, M.D., Matthew Cooper, M.D., George S. Lipkowitz, M.D., Michael A. Rees, M.D., Ph.D., Christopher L. Marsh, M.D., Bashir R. Sankari, M.D., David A. Gerber, M.D., Paul W. Nelson, M.D., Jason Wellen, M.D., Adel Bozorgzadeh, M.D., A. Osama Gaber, M.D., Robert A. Montgomery, M.D., D.Phil., and Dorry L. Segev, M.D., Ph.D.
The authors’ affiliations are as follows: the Department of Surgery, Johns Hopkins University School of Medicine, Baltimore (B.J.O., X.L., A.B.M., B.E.L., R.A., K.J.V.A., R.A.M., D.L. Segev); the Department of Surgery, Barnes–Jewish Hospital, St. Louis (J.M.G.-W., J.W.); the Department of Surgery, Mayo Clinic, Rochester (M.D.S.), and the Department of Surgery, University of Minnesota, Minneapolis (T.B.D.) — both in Minnesota; the Department of Medicine, Cedars–Sinai Comprehensive Transplant Center, Los Angeles (S.C.J.), the Department of Surgery, University of California, San Francisco, San Francisco (J.P.R.), the Department of Surgery, Stanford University, Palo Alto (M.L.M.), and the Department of Surgery, Scripps Clinic and Green Hospital, La Jolla (C.L.M.) — all in California; the Department of Surgery, University of Illinois–Chicago, Chicago (J.O.); the Department of Surgery, Columbia University Medical Center (L.E.R.), and the Department of Surgery, New York Presbyterian–Weill Cornell Medical Center (S.K.) — both in New York; the Department of Surgery, Ohio State University, Columbus (R.P.P.), the Department of Urology, University of Toledo Medical Center, Toledo (M.A.R.), and the Department of Urology, Cleveland Clinic, Cleveland (B.R.S.) — all in Ohio; the Department of Medicine, Thomas Jefferson University Hospital, Philadelphia (P.S.); the Department of Surgery, University of Pittsburgh Medical Center, Pittsburgh (R.S.); the Department of Surgery, Duke University Medical Center, Durham (D.L. Sudan), and the Department of Surgery, University of North Carolina School of Medicine, Chapel Hill (D.A.G.) — both in North Carolina; the Department of Surgery, Virginia Commonwealth University, Richmond (M.P.P.); Integris Baptist Medical Center, Transplant Division, Oklahoma City (J.M.E.-A.); Medstar Georgetown Transplant Institute, Washington, DC (M.C.); the Department of Surgery, Baystate Medical Center, Springfield (G.S.L.), and the Department of Surgery, University of Massachusetts Memorial Medical Center, Worcester (A.B.) — both in Massachusetts; the Department of Surgery, St. Vincent Hospital, Indianapolis (P.W.N.); and the Department of Surgery, Houston Methodist Hospital, Houston (A.O.G.).
Footnotes
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Scientific Registry of Transplant Recipients.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Scientific Registry of Transplant Recipients. home page ( http://www.srtr.org/)
- 2.Annual report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: transplant data 1999–2008. ( http://www.srtr.org/annual_reports/archives/2009/2009_Annual_Report/)
- 3.Fuggle SV, Martin S. Tools for human leukocyte antigen antibody detection and their application to transplanting sensitized patients. Transplantation. 2008;86:384–90. doi: 10.1097/TP.0b013e31817c90f5. [DOI] [PubMed] [Google Scholar]
- 4.Segev DL, Gentry SE, Warren DS, Reeb B, Montgomery RA. Kidney paired donation and optimizing the use of live donor organs. JAMA. 2005;293:1883–90. doi: 10.1001/jama.293.15.1883. [DOI] [PubMed] [Google Scholar]
- 5.Blumberg JM, Gritsch HA, Reed EF, et al. Kidney paired donation in the presence of donor-specific antibodies. Kidney Int. 2013;84:1009–16. doi: 10.1038/ki.2013.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gentry SE, Segev DL, Simmerling M, Montgomery RA. Expanding kidney paired donation through participation by compatible pairs. Am J Transplant. 2007;7:2361–70. doi: 10.1111/j.1600-6143.2007.01935.x. [DOI] [PubMed] [Google Scholar]
- 7.Massie AB, Gentry SE, Montgomery RA, Bingaman AA, Segev DL. Center-level utilization of kidney paired donation. Am J Transplant. 2013;13:1317–22. doi: 10.1111/ajt.12189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montgomery RA, Simpkins CE, Segev DL. New options for patients with donor incompatibilities. Transplantation. 2006;82:164–5. doi: 10.1097/01.tp.0000226105.42713.37. [DOI] [PubMed] [Google Scholar]
- 9.Montgomery RA, Zachary AA, Ratner LE, et al. Clinical results from transplanting incompatible live kidney donor/recipient pairs using kidney paired donation. JAMA. 2005;294:1655–63. doi: 10.1001/jama.294.13.1655. [DOI] [PubMed] [Google Scholar]
- 10.Glotz D, Antoine C, Julia P, et al. Desensitization and subsequent kidney transplantation of patients using intravenous immunoglobulins (IVIg) Am J Transplant. 2002;2:758–60. doi: 10.1034/j.1600-6143.2002.20809.x. [DOI] [PubMed] [Google Scholar]
- 11.Haririan A, Nogueira J, Kukuruga D, et al. Positive cross-match living donor kidney transplantation: longer-term outcomes. Am J Transplant. 2009;9:536–42. doi: 10.1111/j.1600-6143.2008.02524.x. [DOI] [PubMed] [Google Scholar]
- 12.Gloor JM, DeGoey SR, Pineda AA, et al. Overcoming a positive crossmatch in living-donor kidney transplantation. Am J Transplant. 2003;3:1017–23. doi: 10.1034/j.1600-6143.2003.00180.x. [DOI] [PubMed] [Google Scholar]
- 13.Higgins R, Lowe D, Hathaway M, et al. Human leukocyte antigen antibody-incompatible renal transplantation: excellent medium-term outcomes with negative cytotoxic crossmatch. Transplantation. 2011;92:900–6. doi: 10.1097/TP.0b013e31822dc38d. [DOI] [PubMed] [Google Scholar]
- 14.Jordan SC, Tyan D, Stablein D, et al. Evaluation of intravenous immunoglobulin as an agent to lower allosensitization and improve transplantation in highly sensitized adult patients with end-stage renal disease: report of the NIH IG02 trial. J Am Soc Nephrol. 2004;15:3256–62. doi: 10.1097/01.ASN.0000145878.92906.9F. [DOI] [PubMed] [Google Scholar]
- 15.Ejaz NS, Shields AR, Alloway RR, et al. Randomized controlled pilot study of B cell-targeted induction therapy in HLA sensitized kidney transplant recipients. Am J Transplant. 2013;13:3142–54. doi: 10.1111/ajt.12493. [DOI] [PubMed] [Google Scholar]
- 16.Magee CC, Felgueiras J, Tinckam K, Malek S, Mah H, Tullius S. Renal transplantation in patients with positive lymphocytotoxicity crossmatches: one center’s experience. Transplantation. 2008;86:96–103. doi: 10.1097/TP.0b013e318176ae2c. [DOI] [PubMed] [Google Scholar]
- 17.Montgomery RA. Renal transplantation across HLA and ABO antibody barriers: integrating paired donation into desensitization protocols. Am J Transplant. 2010;10:449–57. doi: 10.1111/j.1600-6143.2009.03001.x. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery RA, Lonze BE, Jackson AM. Using donor exchange paradigms with desensitization to enhance transplant rates among highly sensitized patients. Curr Opin Organ Transplant. 2011;16:439–43. doi: 10.1097/MOT.0b013e32834897c1. [DOI] [PubMed] [Google Scholar]
- 19.Montgomery RA, Lonze BE, King KE, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365:318–26. doi: 10.1056/NEJMoa1012376. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery RA, Zachary AA. Transplanting patients with a positive donor-specific crossmatch: a single center’s perspective. Pediatr Transplant. 2004;8:535–42. doi: 10.1111/j.1399-3046.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 21.Schweitzer EJ, Wilson JS, Fernandez-Vina M, et al. A high panel-reactive antibody rescue protocol for cross-match-positive live donor kidney transplants. Transplantation. 2000;70:1531–6. doi: 10.1097/00007890-200011270-00023. [DOI] [PubMed] [Google Scholar]
- 22.Montgomery RA, Zachary AA, Racusen LC, et al. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000;70:887–95. doi: 10.1097/00007890-200009270-00006. [DOI] [PubMed] [Google Scholar]
- 23.Bentall A, Cornell LD, Gloor JM, et al. Five-year outcomes in living donor kidney transplants with a positive crossmatch. Am J Transplant. 2013;13:76–85. doi: 10.1111/j.1600-6143.2012.04291.x. [DOI] [PubMed] [Google Scholar]
- 24.Gloor JM, Winters JL, Cornell LD, et al. Baseline donor-specific antibody levels and outcomes in positive crossmatch kidney transplantation. Am J Transplant. 2010;10:582–9. doi: 10.1111/j.1600-6143.2009.02985.x. [DOI] [PubMed] [Google Scholar]
- 25.Orandi BJ, Garonzik-Wang JM, Massie AB, et al. Quantifying the risk of incompatible kidney transplantation: a multi-center study. Am J Transplant. 2014;14:1573–80. doi: 10.1111/ajt.12786. [DOI] [PubMed] [Google Scholar]
- 26.Montgomery RA, Locke JE, King KE, et al. ABO incompatible renal transplantation: a paradigm ready for broad implementation. Transplantation. 2009;87:1246–55. doi: 10.1097/TP.0b013e31819f2024. [DOI] [PubMed] [Google Scholar]
- 27.Montgomery JR, Berger JC, Warren DS, James NT, Montgomery RA, Segev DL. Outcomes of ABO-incompatible kidney transplantation in the United States. Transplantation. 2012;93:603–9. doi: 10.1097/TP.0b013e318245b2af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berger JC, Muzaale AD, James N, et al. Living kidney donors ages 70 and older: recipient and donor outcomes. Clin J Am Soc Nephrol. 2011;6:2887–93. doi: 10.2215/CJN.04160511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muzaale AD, Massie AB, Wang MC, et al. Risk of end-stage renal disease following live kidney donation. JAMA. 2014;311:579–86. doi: 10.1001/jama.2013.285141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orandi BJ, Chow EHK, Hsu A, et al. Quantifying renal allograft loss following early antibody-mediated rejection. Am J Transplant. 2015;15:489–98. doi: 10.1111/ajt.12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Segev DL, Muzaale AD, Caffo BS, et al. Perioperative mortality and long-term survival following live kidney donation. JAMA. 2010;303:959–66. doi: 10.1001/jama.2010.237. [DOI] [PubMed] [Google Scholar]
- 32.Van Arendonk KJ, Orandi BJ, James NT, Segev DL, Colombani PM. Living unrelated renal transplantation: a good match for the pediatric candidate? J Pediatr Surg. 2013;48:1277–82. doi: 10.1016/j.jpedsurg.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 33.Rao JNK, Scott AJ. On chi-squared tests for multiway contingency-tables with cell proportions estimated from survey data. Ann Stat. 1984;12:46–60. [Google Scholar]
- 34.Wilcox RR. A note on the Theil-Sen regression estimator when the regressor is random and the error term is hetero-scedastic. Biom J. 1998;40:261–8. [Google Scholar]
- 35.Newson R. Parameters behind “non-parametric” statistics: Kendall’s tau, Somers’ D and median differences. Stata J. 2002;2:45–64. [Google Scholar]
- 36.Therneau TM, Grambsch PM. Modeling survival data: extending the Cox model. New York: Springer Science & Business Media; 2000. [Google Scholar]
- 37.Reed EF, Rao P, Zhang Z, et al. Comprehensive assessment and standardization of solid phase multiplex-bead arrays for the detection of antibodies to HLA. Am J Transplant. 2013;13:1859–70. doi: 10.1111/ajt.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tait BD, Süsal C, Gebel HM, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013;95:19–47. doi: 10.1097/TP.0b013e31827a19cc. [DOI] [PubMed] [Google Scholar]
- 39.Zachary AA, Klingman L, Thorne N, Smerglia AR, Teresi GA. Variations of the lymphocytotoxicity test. An evaluation of sensitivity and specificity. Transplantation. 1995;60:498–503. doi: 10.1097/00007890-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 40.Zachary AA, Lucas DP, Detrick B, Leffell MS. Naturally occurring interference in Luminex assays for HLA-specific antibodies: characteristics and resolution. Hum Immunol. 2009;70:496–501. doi: 10.1016/j.humimm.2009.04.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.