Abstract
Purpose
Prior studies report that weekend admission to an intensive care unit is associated with increased mortality, potentially attributed to the organizational structure of the unit. This study aims to determine whether treatment of hypotension, a risk factor for mortality, differs according to level of staffing.
Methods
Using the Multiparameter Intelligent Monitoring in Intensive Care database, we conducted a retrospective study of patients admitted to an intensive care unit at Beth Israel Deaconess Medical Center who experienced one or more episodes of hypotension. Episode(s) were categorized according to the staffing level, defined as high during weekday daytime (7am–7pm) and low during weekends or nighttime (7pm–7am).
Results
Patients with a hypotensive event on a weekend were less likely to be treated compared to those that occurred during the weekday daytime (p=0.02). No association between weekday daytime versus weekday nighttime staffing levels and treatment of hypotension was found (RR 1.02; 95% CI 0.98–1.07).
Conclusion
Patients with a hypotensive event on a weekend were less likely to be treated than patients with an event during high-staffing periods. No association between weekday nighttime staffing and hypotension treatment was observed. We conclude that treatment of a hypotensive episode relies on more than solely staffing levels.
Keywords: critical care, hospital medical staff, hypotension, intensive care unit, resuscitation
Introduction
In the last decade, there has been emerging interest in the efficient allocation of healthcare resources to critically ill patients. One area of research has focused on the organizational structure of intensive care units (ICUs) and whether having more or less staff on duty affects patient outcomes. A recent meta-analysis demonstrated an increased risk of death for patients admitted to an ICU over the weekend.[1] They attributed this finding to the organizational structure and staffing differences on the weekend as compared to the weekday. Another study that examined intensivist coverage reported a higher mortality rate for those patients admitted to an ICU with low-intensity staffing, defined as either no intensivist coverage or elective intensivist consultation.[2] However, other studies have recently questioned the benefit of increased off-hour intensivist coverage.[3] Wallace, et al. examined the organizational structure of 49 ICUs and found a mortality benefit associated with nighttime intensivist coverage for ICUs with low-intensity daytime coverage but not for ICUs with high-intensity daytime staffing.[4] This finding was corroborated by a single-center, prospective trial in the medical ICU of an academic medical center that demonstrated no mortality benefit from overnight intensivist coverage.[5] An emerging body of literature suggests that the intensity of ICU staffing may reduce the risk of mortality, though the physiological evidence for this association remains unclear. In addition, the association between hypotension and mortality, presumed to be secondary to organ dysfunction, is well established in the trauma literature.[6, 7] We are unaware of published literature evaluating whether one possible cause of mortality, hypotension, is associated with staffing levels.
We aimed to further explore the association between staffing and patient care by investigating whether the management of sustained hypotension is associated with the level of ICU staffing. If a physiologic intervention were associated with staffing levels, it could have far-reaching implications for clinical management. We hypothesized that hypotension occurring during low-staffing periods would be associated with a reduced likelihood of hypotension treatment.
Methods
Patient cohort
This was a retrospective cohort study of patients admitted to ICUs at Beth Israel Deaconess Medical Center (BIDMC) in Boston, Massachusetts, USA from 2001 through 2008. Patient data were extracted from the Multiparameter Intelligent Monitoring in Intensive Care (MIMIC-II) database[8] (version 2.6), which is a publicly available, de-identified ICU database developed jointly by the Massachusetts Institute of Technology, BIDMC and Philips Healthcare. The Institutional Review Board at BIDMC approved the study protocol with a waiver of informed consent.
Eligibility criteria included age greater than 15 years; admission to the medical ICU, surgical ICU, coronary care unit, or cardiac surgery recovery unit; at least one hypotensive episode (HE) during the ICU admission; and complete data for potential confounders. We excluded patients with a do not resuscitate (DNR) or do not intubate (DNI) order in effect at any time during their ICU admission. A hypotensive episode was identified using mean arterial pressure (MAP) measurements recorded using invasive arterial catheters or non-invasive sphygmomanometers. If both measurement techniques were available for the same time point, invasive measurements were analyzed. In general, both types of MAP measurements were recorded every 10–15 minutes. The beginning of an HE was defined as the time of the first of two consecutive MAP measurements less than 60 mmHg, preceded by two consecutive MAP values greater than or equal to 60 mmHg. The end of the HE was defined as the time of the first of two consecutive MAP measurements greater than or equal to 60 mmHg, following the beginning of the HE.
Study variables and outcomes
The primary exposure was staffing level at the onset of the HE. Weekday daytime (7 am to 7 pm) was considered a high-staffing period, while weekday nighttime (7 pm to 7 am), weekend daytime and weekend nighttime were considered as three distinct periods of low-staffing.
Throughout the study period, core staffing at BIDMC typically consisted of 5 nurses for 8 patients, allowing for 2 of those patients to have a 1:1 patient to nurse ratio, while less acute patients had a 2:1 ratio. This core nursing staff structure was the same for all four exposure periods.
During weekday daytime, the high-staffing period, each ICU was staffed with a resource nurse and unit-based educator, as well as one attending, three residents, and often a fellow. Weekend daytime staffing consisted of the primary attending and fellow for each unit present for morning rounds and then available by telephone, and one in-house resident per unit. During both weekday nighttime and weekend nighttime, the primary attending was available by telephone, there was one in-house resident for each unit, and there was one overnight in-house attending to cover all units. Weekends (both daytime and nighttime) are staffed with the same core nursing staff that staffs the units during the week. The primary outcome of interest was any HE treatment; secondary outcomes included treatment with fluid resuscitation, or vasoactive therapy only. Fluid resuscitation was defined as one or more infusions of either a bolus of isotonic crystalloid of at least 250 ml or any non-zero volume of colloids. Vasoactive therapy was defined as the initiation of or increase in dosage of any vasoactive agent during the HE. The following vasoactive agents were considered: dobutamine, dopamine, epinephrine, norepinephrine, phenylephrine and vasopressin.
The following variables were considered potential confounders and assessed for inclusion in the models: age, sex, Elixhauser Comorbidity Index for in-hospital death, [9,10] Simplified Acute Physiologic Score (SAPS) I (a predictor of mortality for critically ill patients), MAP in the three hour period immediately prior to HE onset, total volume of urine output in the three hour period immediately prior to HE onset, last serum creatinine level prior to and within 24 hours of the HE onset, the total volume of fluids (normal saline or lactated ringer) given to the patient between ICU admission and HE onset, and service type on admission.
Statistical analysis
We used modified Poisson regression with robust error variance, which accounts for the repeated HE episodes in the same individual, to estimate the risk ratio (RR) and 95% confidence interval (CI) for the association between staffing intensity and each of the primary outcomes: fluid resuscitation, vasoactive therapy and any HE treatment. [11] We then used multivariable models to assess the influence of all potential confounders listed above, and retained those variables that had an appreciable effect on the association. Consequently, the final models were adjusted for age, SAPS I, number of blood pressure measurements per hour, minimum blood pressure during the HE, hours since ICU admission and mean blood pressure 3 hours before the HE.[12] For all regression models, p-values <0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC).
Results
Figure 1 depicts how we applied our exclusion criteria to the MIMIC-II patient population of 32,426 to arrive at 6,446 eligible patients. The study population had a slightly larger proportion of men (54.3%), a mean age of 66.7 ± 15.9 years, and a mean Elixhauser Comorbidity Index of 2.6 ± 5.5 (Table 1). There were 21,003 HEs, with a mean of 2.6 ± 3.4 HEs per patient during the ICU stay. The mean MAP during HEs was 58.8 ± 3.9 mmHg, while the mean minimum MAP during HEs was 51.9 ± 5.6 mmHg.
Figure 1.
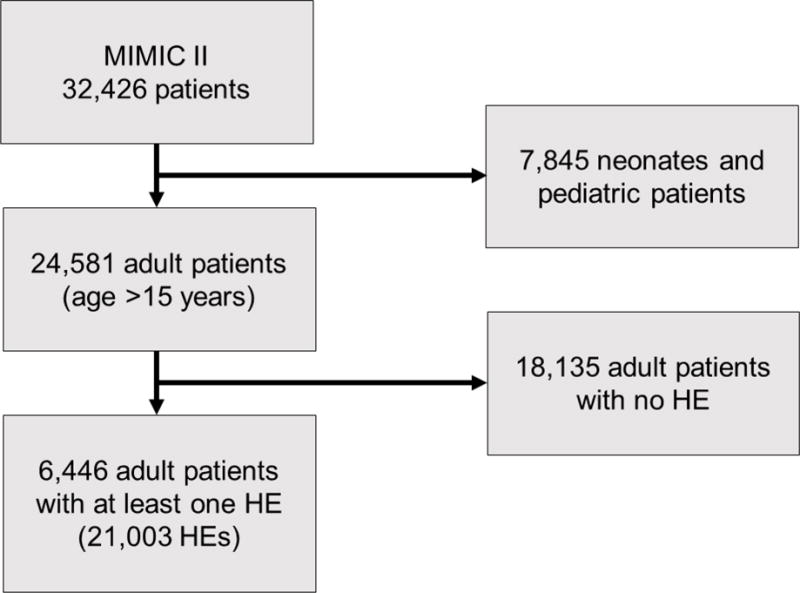
Exclusion criteria applied to the Multiparameter Intelligent Monitoring in Intensive Care patient database
Table 1.
Characteristics of patient cohort
| Entire Cohort (n=6,446) |
|
|---|---|
| Male | 3500 (54.3) |
| Age (years) | 66.7 ± 15.9 |
| SAPS I | 14.8 ± 5.3 |
| Number of hypotensive episodes per patient | 2.6 ± 3.4 |
| Creatinine before hypotensive episode (mg/dl) | 1.4 ± 1.4 |
| Creatinine after hypotensive episode (mg/dl) | 1.5 ± 1.5 |
| Service on admission | |
| Cardiac Care | 1091 (16.9) |
| Cardiac Surgery | 1925 (29.9) |
| Medical | 1977 (30.7) |
| Surgical | 1376 (21.4) |
| Mixed Medical-Surgical | 77 (1.3) |
| Elixhauser Comorbidity Index | 2.6 ± 5.5 |
| 28-day Elixhauser Comorbidity Index | 3.8 ± 5.8 |
Values are presented as n (%) or mean ± standard deviation
Table 2 stratifies the study population by the four distinct staffing periods at the time of HE onset. Patients who experienced a HE during low-staffing periods as compared to high-staffing periods were more likely to have a longer duration of HE, fewer blood pressure measurements per hour and less urine output in the three hours before the HE. Among all HEs during this study period, 65.4% were never treated. Table 3 demonstrates that treatment was more likely to occur during the high-staffing period than during the three low-staffing periods and that the likelihood of treatment during the weekday nighttime was most similar to that of the weekday daytime, which was the period of high-staffing. In addition, Table 3 shows that, overall, treatment was more common in the surgical ICUs than in the medical ICUs.
Table 2.
Characteristics of patients according to staffing period at the time of the hypotensive episode
| Characteristics | Entire Cohort (n=21,003) |
Weekday Daytime (n=7,402) |
Weekday Nighttime (n=7,967) |
Weekend Daytime (n=2,778) |
Weekday Nighttime (n=2,856) |
|---|---|---|---|---|---|
| Time since ICU admission (hours) | 169.2 ± 282.8 | 174.7 ± 289.5 | 162.7 ± 279.1 | 180.1 ± 295.1 | 162.7 ± 261.7 |
| HE duration (minutes) | 174.1 ± 209.8 | 162.6 ± 190.3 | 178.8 ± 193.4 | 177.0 ± 272.8 | 188.1± 228.9 |
| Number of BP measurements per hour | 3.6 ± 4.6 | 4.1 ± 5.2 | 3.4 ± 4.2 | 3.5± 4.4 | 3.2 ± 3.8 |
| Mean MAP before HE (mmHg) | 69.7± 9.3 | 70.0 ± 9.3 | 69.4 ± 8.9 | 69.7 ± 9.0 | 69.6 ± 10.8 |
| Total urine output 3 hours before HE (mL) | 334.3 ± 406.7 | 347.7 ± 400.1 | 335.5 ± 464.2 | 301.2 ± 298.3 | 328.4 ± 332.6 |
| Total volume of fluids given before HE (L) | 4.2 ± 6.7 | 4.3 ± 6.8 | 4.1 ± 6.9 | 4.3 ± 6.6 | 4.2 ± 5.8 |
| Mean MAP during HE (mmHg) | 58.8 ± 3.9 | 58.8 ± 4.1 | 58.8 ± 3.9 | 58.7 ± 3.8 | 58.8 ± 3.7 |
| Minimum MAP during HE (mmHg) | 51.9 ± 5.6 | 51.7 ± 5.7 | 52.0 ± 5.5 | 51.9 ± 5.8 | 52.0 ± 5.5 |
ICU: intensive care unit; HE: hypotensive episode; BP: blood pressure; MAP: mean arterial pressure Values are presented as n (%) or mean ± standard deviation
Table 3.
Treatment of patients according to staffing period at the time of the hypotensive episode
| Treated | Vasoactive Therapy | Fluid Resuscitation | |
|---|---|---|---|
| Entire Cohort | 7276 (34.6) | 5188 (24.7) | 3195 (15.2) |
|
| |||
| Weekday Daytime | 2663 (36.0) | 1903 (25.7) | 1192 (16.1) |
| Weekday Nighttime | 2790 (35.0) | 1955 (24.5) | 1260 (15.8) |
| Weekday Daytime | 905 (32.6) | 660 (23.8) | 360 (13.0) |
| Weekday Nighttime | 918 (32.1) | 670 (23.5) | 383 (13.4) |
|
| |||
| Surgical Intensive Care Units | 4040 (38.3) | 3007 (28.5) | 1720 (16.3) |
|
| |||
| Weekday Daytime | 1552 (39.9) | 1153 (29.6) | 697 (17.9) |
| Weekday Nighttime | 1559 (39.6) | 1160 (29.5) | 657 (16.7) |
| Weekday Daytime | 462 (34.0) | 341 (25.1) | 177 (13.0) |
| Weekday Nighttime | 467 (34.2) | 353 (25.9) | 189 (13.9) |
|
| |||
| Medical Intensive Care Units | 3236 (31.0) | 2181 (20.9) | 1475 (14.1) |
|
| |||
| Weekday Daytime | 1111 (31.6) | 750 (21.4) | 495 (14.1) |
| Weekday Nighttime | 1231 (30.5) | 795 (19.7) | 603 (15.0) |
| Weekday Daytime | 443 (31.2) | 319 (22.5) | 183 (12.9) |
| Weekday Nighttime | 451 (30.3) | 317 (21.3) | 194 (13.0) |
Values are presented as n (%). The Surgical Intensive Care Units (ICUs) include the Cardiac Surgery and Surgical ICUs. The Medical ICUs include the Cardiac Care, Medical and Mixed Medical-Surgical ICUs.
Patients with an HE during the weekend daytime were significantly less likely to receive any hypotensive treatment compared with those who experienced a hypotensive episode during the weekday daytime (adjusted RR 0.93; 95% CI: 0.87–0.99). This association appeared to be driven by the decreased likelihood of fluid resuscitation during the weekend daytime compared with weekday daytime (RR 0.81, 95% CI: 0.72–0.92). Similar associations were observed when comparing weekday nighttime to the high-staffing period. When comparing weekday daytime and weekday nighttime, we did not find an association with the likelihood of any hypotensive treatment (RR=1.02, CI: 0.98–1.07), vasoactive therapy or fluid resuscitation (Table 4).
Table 4.
Risk of hypotension treatment among patients according to staffing period
| Treated, RR (95% CI) | P | Vasoactive Therapy, RR (95% CI) | P | Fluid Resuscitation, RR (95% CI) | P | |
|---|---|---|---|---|---|---|
| Unadjusted | ||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — |
| Weekday Nighttime | 0.97 (0.93–1.02) | 0.21 | 0.95 (0.90–1.01) | 0.09 | 0.98 (0.91–1.06) | 0.64 |
| Weekend Daytime | 0.91 (0.85–0.97) | 0.003 | 0.92 (0.85–1.00) | 0.06 | 0.80 (0.72–0.90) | 0.0003 |
| Weekend Nighttime | 0.89 (0.84–0.95) | 0.001 | 0.91 (0.84–0.99) | 0.03 | 0.83 (0.75–0.93) | 0.001 |
| Adjusted* | ||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — |
| Weekday Nighttime | 1.02 (0.98–1.07) | 0.35 | 1.02 (0.96–1.08) | 0.57 | 1.00 (0.92–1.08) | 0.98 |
| Weekend Daytime | 0.93 (0.87–0.99) | 0.04 | 0.97 (0.89–1.05) | 0.42 | 0.81 (0.72–0.92) | 0.001 |
| Weekend Nighttime | 0.93 (0.87–0.99) | 0.03 | 0.99 (0.91–1.07) | 0.80 | 0.81 (0.72–0.91) | 0.0003 |
Adjusted for age, Simplified Acute Physiologic Score, number of blood pressure measurements per hour, minimum blood pressure during the hypotensive episode (HE), hours since ICU admission and mean blood pressure 3 hours prior to the HE
In our subgroup analysis, we did not observe significant differences in treatment of hypotension during weekday daytime compared with weekday nighttime in either the medical or surgical ICUs, consistent with what we observed in the full cohort (Table 5). When restricting to surgical ICUs, we observed the same decreased risk of any hypotension treatment and fluid resuscitation when comparing both weekend daytime and weekend nighttime with the high-staffing period in multivariable analyses. In contrast, in the medical ICUs there was no association between staffing level and treatment of HE.
Table 5.
Risk of hypotension treatment among patients according to staffing period, as presented by ICU type
| Treated, RR (95% CI) | P | Vasoactive Therapy, RR (95% CI) | P | Fluid Resuscitation, RR (95% CI) | P | |||
|---|---|---|---|---|---|---|---|---|
| Surgical Intensive Care Units | ||||||||
|
| ||||||||
| Unadjusted | ||||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — | ||
| Weekday Nighttime | 0.99 (0.94–1.05) | 0.82 | 1.00 (0.93–1.06) | 0.89 | 0.93 (0.84–1.03) | 0.17 | ||
| Weekend Daytime | 0.85 (0.78–0.93) | 0.0002 | 0.85 (0.76–0.94) | 0.002 | 0.73 (0.62–0.86) | 0.0001 | ||
| Weekend Nighttime | 0.86 (0.79–0.93) | 0.0004 | 0.87 (0.79–0.97) | 0.01 | 0.77 (0.66–0.90) | 0.001 | ||
| Adjusted* | ||||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — | ||
| Weekday Nighttime | 1.03 (0.98–1.09) | 0.27 | 1.04 (0.97–1.12) | 0.22 | 0.95 (0.86–1.05) | 0.29 | ||
| Weekend Daytime | 0.90 (0.83–0.98) | 0.02 | 0.92 (0.83–1.02) | 0.10 | 0.75 (0.63–0.88) | 0.001 | ||
| Weekend Nighttime | 0.90 (0.83–0.98) | 0.02 | 0.94 (0.85–1.05) | 0.27 | 0.79 (0.68–0.92) | 0.003 | ||
|
| ||||||||
| Medical Intensive Care Units | ||||||||
|
| ||||||||
| Unadjusted | ||||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — | ||
| Weekday Nighttime | 0.96 (0.90–1.03) | 0.30 | 0.92 (0.84–1.01) | 0.08 | 1.06 (0.95–1.19) | 0.32 | ||
| Weekend Daytime | 0.99 (0.89–1.09) | 0.81 | 1.05 (0.92–1.20) | 0.44 | 0.92 (0.77–1.08) | 0.30 | ||
| Weekend Nighttime | 0.96 (0.87–1.05) | 0.37 | 1.00 (0.88–1.13) | 0.94 | 0.92 (0.78–1.09) | 0.34 | ||
| Adjusted* | ||||||||
| Weekday Daytime | 1.00 (Reference) | — | 1.00 (Reference) | — | 1.00 (Reference) | — | ||
| Weekday Nighttime | 1.01 (0.94–1.09) | 0.76 | 0.98 (0.89–1.08) | 0.68 | 1.08 (0.96–1.22) | 0.21 | ||
| Weekend Daytime | 0.98 (0.89–1.09) | 0.77 | 1.05 (0.91–1.21) | 0.53 | 0.93 (0.78–1.12) | 0.45 | ||
| Weekend Nighttime | 0.97 (0.88–1.08) | 0.59 | 1.07 (0.94–1.22) | 0.31 | 0.85 (0.71–1.01) | 0.07 | ||
Patients included in the Surgical Intensive Care Units (ICUs) subgroup analysis include the Cardiac Surgery and Surgical ICUs. Patients in the Medical ICUs include those in the Cardiac Care, Medical and Mixed Medical-Surgical ICUs.
Adjusted for age, Simplified Acute Physiologic Score, number of blood pressure measurements per hour, minimum blood pressure during the hypotensive episode (HE), hours since ICU admission and mean blood pressure 3 hours prior to the HE
Discussion
In this large, retrospective study of patients admitted to the ICU, we found that patients who were hypotensive during the weekend daytime and weekend nighttime, periods with low-staffing, were less likely to receive treatment compared to the weekday daytime high-staffing period. This association was driven by fluid resuscitation; no association was observed for vasoactive therapy. However, we did not find an association between likelihood of treatment of HEs during the weekday nighttime, another low-staffing period, compared to weekday daytime.
To our knowledge, this is the first paper that examines how the delivery of care in an ICU may depend on the time an event occurs. While several studies have examined the association between low versus high-staffing during admission to an ICU and mortality, our results may provide physiologic evidence for these studies. Further studies are required in order to elucidate the relationship between staffing levels, hypotension treatment, and mortality.
Our results show that the likelihood of HE treatment was similar for weekday daytime and weekday nighttime, which is contrary to our hypothesis. If our observations regarding HE treatment were due strictly to staffing levels at the time of an HE, we would expect the incidence of treatment to be similarly low during the weekday nighttime and weekend nighttime, when staffing levels are comparable. This is an interesting result, which may indicate that ICU intensivist and nurse staffing levels are not the only factor contributing to increased ICU mortality on weekends. A possible explanation is that a given ICU attending and/or nurse manager spends a full shift in the ICU on a weekday, allowing them to observe a patient for a longer period of time and to create a more thorough plan of care for the nighttime resident and nurses, as compared to the weekend when the attending is only in the ICU for morning rounds and there is no nurse manager. In addition, differences in the treatment of HEs were more prominent in surgical patients as compared to medical patients. This too may point to differences in the culture of the ICU. Variations in the treatment of hypotension may exist across clinical specialties or populations of patients, which are not due directly to the staffing structure.
Although significant heterogeneity exists in the way ICUs are staffed, the weekend is almost uniformly a time with the least resources. While the ideal level of staffing would approximate that found during the weekday, this may not be practical for several reasons. The additional cost of maintaining weekday staffing levels on the weekend has been cited as a barrier to implementation.[13] Despite evidence that 24-hour intensivist coverage leads to improved outcomes and lower overall cost,[14] administrative buy-in may be difficult. In addition, the relative shortage of intensivists may make full-time ICU coverage challenging. Whether overnight coverage by non-intensivist physicians or mid-level providers would reduce morbidity and mortality is unknown. Smaller community-based hospitals with limited overnight resources may be stretched in attempting to provide this intensity of critical care service.
While it is possible that a more stringent definition of an HE would result in a greater frequency of treatment, our definition of 60 mmHg represents a common threshold that should prompt treatment. [16] If a patient’s MAP consistently falls below the goal MAP, even if by a small margin, nurses will typically act on it, taking into consideration the overall clinical context (i.e. mental status, urine output and other vital signs). It is possible that for an asymptomatic patient, a value slightly below the threshold would go untreated.
We were interested to find that 65% of HEs as defined in the study were not treated. This was a rather striking finding and may be explained by the fact that we included all HEs, including those that occurred when the patient was no longer acutely sick. Blood pressure is but a surrogate of tissue perfusion, which is critical to organ function. Clinicians consider markers of tissue perfusion other than blood pressure in isolation, which may include urine output, mental status, and serum lactate, when deciding whether to treat a HE. Treatment of hypotension in the setting of adequate tissue perfusion has been demonstrated to be potentially harmful.[15, 16] It is possible that the HEs identified in the study were accompanied by evidence of adequate tissue perfusion.
Our study is limited by its retrospective nature. This study is also limited by the data being obtained from a single center; thus, our results may not generalize to other ICUs. As is noted in several studies however, significant heterogeneity exists in the organizational structure of an ICU.[17–19] In our study, one overnight in-house attending covered all of the ICUs and was available for consultation. While the weekend is usually associated with the least amount of staffing, other ICUs may maintain close to weekday levels on the weekend. The generalizability of our findings may also be limited due to the exclusion of patients identified as having a DNR/DNI status at any time during their admission to the ICU.
In addition, while it is possible that our results are confounded by time at which the patient was admitted, we adjusted for the patient’s baseline comorbidities (Elixhauser Comorbidity Index) and severity of illness (SAPS I). However, this may not entirely capture subtle differences associated with timing of patient admission. Despite these limitations, our study begins to identify that treatment of an important physiologic parameter relies on more than staffing levels alone.
Conclusion
In conclusion, our study indicates that HEs occurring during the weekend daytime and weekend nighttime, low-staffing periods, are less likely to be treated than those with onset during the weekday daytime, a period of high-staffing. If this finding were strictly related to the level of ICU staffing, we would expect that HEs occurring during the weekday nighttime, also considered a low-staffing period, would have a similarly lower likelihood of treatment. In contrast, we found that the likelihood of treatment was similar during the weekday nighttime and weekday daytime. This indicates that staffing structure alone does not affect whether patients who experience a HE receive treatment. Furthermore, although only postulated, this study suggests that there may be a hypotension-related mortality benefit to increasing allocation of intensivist coverage to weekends and not to weekday nights. Additional studies are needed to investigate possible physiological intermediates that could explain the increased risk in mortality during weekends in ICUs and to elucidate why the same pattern is not seen during the weekday nighttime.
Acknowledgments
M. Dustin Boone received statistical support from the Center for Anesthesia Research Excellence (CARE) at Beth Israel Deaconess Medical Center.
MDB and AM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. MDB, JM, AM, SJ, JL, RK, DJS, JC, LAC, and MRH contributed substantially to the study design, data analysis, and interpretation, and to the writing of the manuscript.
Funding
Leo Anthony Celi is funded by the National Institute of Health through the NIBIB grant R01 EB017205-01A1.
Michele R. Hacker receives support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers.
No funding source had involvement in study design, collection, analysis, and interpretation of data, writing of this manuscript, or the decision to submit for purposes of publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: none
References
- 1.Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE. Association between time of admission to the icu and mortality: A systematic review and metaanalysis. Chest. 2010;138(1):68–75. doi: 10.1378/chest.09-3018. [DOI] [PubMed] [Google Scholar]
- 2.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288(17):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 3.Luyt C-E, Combes A, Aegerter P, Guidet B, Trouillet J-L, Gibert C, Chastre J. Mortality among patients admitted to intensive care units during weekday day shifts compared with “off” hours*. Crit Care Med. 2007;35(1):3–11. doi: 10.1097/01.CCM.0000249832.36518.11. [DOI] [PubMed] [Google Scholar]
- 4.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366(22):2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kerlin MP, Small DS, Cooney E, Fuchs BD, Bellini LM, Mikkelsen ME, Schweickert WD, Bakhru RN, Gabler NB, Harhay MO. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209. doi: 10.1056/NEJMoa1302854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel JH, Rivkind AI, Dalal S, Goodarzi S. Early physiologic predictors of injury severity and death in blunt multiple trauma. Arch Surg. 1990;125(4):498–508. doi: 10.1001/archsurg.1990.01410160084019. [DOI] [PubMed] [Google Scholar]
- 7.Zenati MS, Billiar TR, Townsend RN, Peitzman AB, Harbrecht BG. A brief episode of hypotension increases mortality in critically ill trauma patients. Journal of Trauma and Acute Care Surgery. 2002;53(2):232–237. doi: 10.1097/00005373-200208000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Saeed M, Villarroel M, Reisner AT, Clifford G, Lehman L-W, Moody G, Heldt T, Kyaw TH, Moody B, Mark RG. Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC-II): a public-access intensive care unit database. Crit Care Med. 2011;39(5):952. doi: 10.1097/CCM.0b013e31820a92c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 10.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009:626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 11.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 12.Hosmer DW, Lemeshow S. Applied Logistic Regression. Second. Danvers, MA: John Wiley & Sons; 2000. [Google Scholar]
- 13.Vincent J-L. Need for intensivists in intensive-care units. The Lancet. 2000;356(9231):695–696. doi: 10.1016/S0140-6736(00)02622-2. [DOI] [PubMed] [Google Scholar]
- 14.Hanson CW, Deutschman CS, Anderson HL, Reilly PM, Behringer EC, Schwab CW, Price J. Effects of an organized critical care service on outcomes and resource utilization: a cohort study. Crit Care Med. 1999;27(2):270–274. doi: 10.1097/00003246-199902000-00030. [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Louw E, Niemi M, Nelson R, Mark R, Celi L, Mukamal K, Danziger J. Association between fluid balance and survival in critically ill patients. J Intern Med. 2015;277(4):468–477. doi: 10.1111/joim.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee J, Kothari R, Ladapo JA, Scott DJ, Celi LA. Interrogating a clinical database to study treatment of hypotension in the critically ill. BMJ open. 2012;2(3):e000916. doi: 10.1136/bmjopen-2012-000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, Fan E. Do Intensivist Staffing Patterns Influence Hospital Mortality Following ICU Admission? A Systematic Review and Meta-Analyses*. Crit Care Med. 2013;41(10):2253–2274. doi: 10.1097/CCM.0b013e318292313a. [DOI] [PubMed] [Google Scholar]
- 18.Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA. Critical care delivery in the United States: Distribution of services and compliance with Leapfrog recommendations*. Crit Care Med. 2006;34(4):1016–1024. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 19.Lilly CM, Zuckerman IH, Badawi O, Riker RR. Benchmark data from more than 240,000 adults that reflect the current practice of critical care in the United States. CHEST Journal. 2011;140(5):1232–1242. doi: 10.1378/chest.11-0718. [DOI] [PubMed] [Google Scholar]


