Abstract
[Purpose] The aim of this study was to investigate the efficiency of Nintendo® Wii games in addition to neurodevelopmental treatment in patients with cerebral palsy. [Subjects and Methods] Thirty hemiparetic cerebral palsy patients (16 females, 14 males; mean age, 6–15 years) were included in the study and divided into two groups: a neurodevelopmental treatment+Nintendo Wii group (group 1, n=15) and a neurodevelopmental treatment group (group 2, n=15). Both groups received treatment in 45-minute sessions 2 days/week for six weeks. Use of the upper extremities, speed, disability and functional independence were evaluated using the Quality of Upper Extremity Skills Test, Jebsen Taylor Hand Function Test, ABILHAND-Kids test, and Pediatric Functional Independence Measure (self-care) before and after treatment. [Results] There were statistically significant improvements in all parameters for group 1 and group 2 (except quality of function) after six weeks of treatment. Intergroup analysis showed that group 1 was superior to group 2 in mean change differences in the Jebsen Taylor Hand Function Test. [Conclusion] Our results showed that neurodevelopmental treatment is effective for improving hand functions in hemiplegic cerebral palsy. To provide a enjoyable, motivational, safe, and effective rehabilitation program, the Nintendo® Wii may be used in addition to neurodevelopmental treatment.
Key words: Cerebral palsy, Virtual reality, Nintendo® Wii
INTRODUCTION
Cerebral palsy (CP) is the most common cause of neurological disability in children1), affecting approximately 1 in 1,300 live births2). At an early age, the most affected parts of upper extremity involvement are the wrist and hands. Abnormal hand postures such as thumb adduction and/or flexion with limited wrist extension are the primary manifestations of hand involvement. Daily living activities and functional independence are affected by increased tonus of the upper limb, impaired posture and function3, 4).
In children with CP, neurodevelopmental treatment (NDT) is the most widely used treatment approach, which aims to maximize the child’s potential to improve motor functions while preventing musculoskeletal complications5, 6). In the literature, it has been reported that intensive neurodevelopmental treatment is effective for improvement of gross motor function, hand functions, and the quality of upper-extremity movement7, 8). Virtual rehabilitation is a relatively new method that has been adopted by physical therapists who specialize in CP treatment. In recent years, there has been growing interest in therapeutic use of the Nintendo Wii and Wii Fit (Wii) as virtual rehabilitation tools. Although limited in number, some studies have suggested that use of these devices, could result in significant therapeutic gains in motor function for children with cerebral palsy9, 10).
The theories of motor control and motor learning emphasize the importance of including motivating, repetitive, purposeful exercises with games and fun to support development in the rehabilitation of children with CP11, 12). During standard physiotherapy sessions, it can be difficult to motivate a child and encourage participation in activities. Therefore, physical therapists need various motivational techniques and methods to gain the most benefit from exercises applied to improve limb use13). Virtual reality games can be motivating and entertaining for the paediatric age group, thereby holding the interest of the child during treatment10, 14), whilst also improving upper extremity skills and control4, 10), skills required for daily living activities15), and speed of upper extremity use14). In the literature, there are studies that have evaluated use of theNintendo Wii and similar games consoles for improvement of upper extremity functions in patients with various diagnoses14, 16,17,18), but there are very few that have investigated the effectiveness of use of technological systems to improve upper extremity functions in children with CP. The current study aimed to determine the effects on quality of upper extremity skills, movement speed of the upper extremity, disability, and functional independence as a result of adding virtual reality games to a neurodevelopmental treatment program.
SUBJECTS AND METHODS
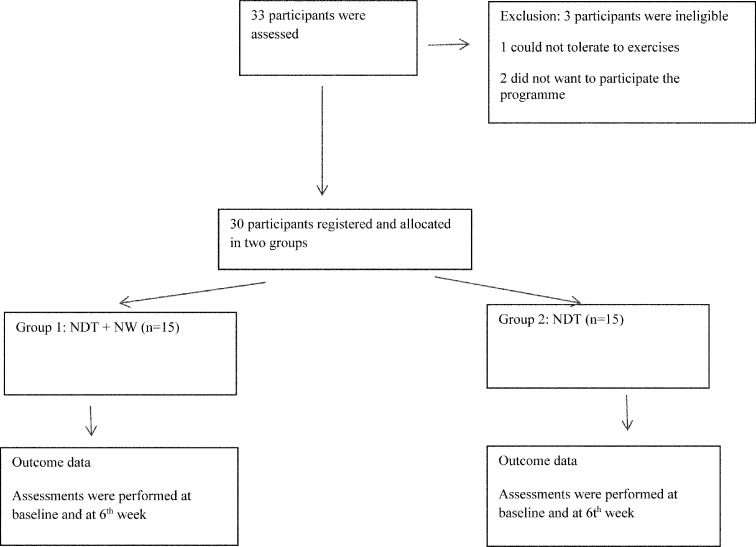
A total of 33 children with spastic hemiparesis were evaluated, and 30 were included in this study between June and September 2014 (Fig. 1). The inclusion criteria were a) aged between 6 and 15 years, b) level 1–3 of the Manual Ability Classification System, c) level 1or 2 of the Gross Motor Function Classification System16, 19, 20), d) ability to grasp and release an object, and e) no history of surgery or botulinum toxin application to the upper extremity in the previous 6 months. Parents or legal guardians read and signed an informed consent form before the study, and the Marmara University Health Sciences Institute Ethics Committee approved the study (02.05.2014-13).
Fig. 1.
Flow chart describing the progression of participants through the trial
The children were divided into two groups on the basis of arrival at the clinic. We used simple randomization with a random number generator (1–15, group 1; 16–30: group 2). The first 15 children were assigned as group 1, and the program applied was NDT+Wii. The second 15 children were assigned as group 2 and received NDT5, 6) only. Treatment in both groups was applied by a physical therapist for 45 minutes per session, twice a week, for 6 weeks. The patients in group 1 played virtual reality games of tennis, baseball, and boxing (each game 5 minutes) for 15 minutes in addition to the standard neurodevelopmental treatment in each treatment session, wich was focus on the hemiplegic hand. Two experienced physical therapists selected the games for moving to the hemiplegic upper extremity. All children were trained by the same therapists during all sessions. The patients who attended school received treatment outside of school hours.
The NDT Program for both groups was applied according to each child’s individual needs and included tonus regulation, support of sensation, perception and motor development, facilitating normal movement for upper extremity activities, upper extremity functional skills training, and daily living activities such as getting dressed and eating.
Before starting the Nintendo Wii games, the patients were informed about the content of each game and had one practice session, during which the children were supported verbally and physically until they achieved the correct movements.
In this study, use of the upper extremity was evaluated using the Quality of Upper Extremity Skills Test (QUEST), which has been tested for validity and reliability in children with neuromotor dysfunction. This test indicates four domains: dissociated movement, grasp, weight-bearing, and protective extension21).
Hand function speed was assessed with the Jebsen Taylor Hand Function Test (JTHFT), which has been shown to be reliable and normative for children22, 23). In this study, the subtests to assess hand function included turning over cards 3 × 5 inches (7.5 cm × 12.5 cm) in size, simulated feeding, picking up small common objects, stacking checkers, picking up large objects, and picking up large heavy objects. The time (in seconds) taken to perform seven fine motor hand tasks was measured.
Hand disability was assessed using the ABILHAND-Kids test, which has been found to be valid and reliable in children with CP. Turkish translation of the ABILHAND-Kids test was performed by the authors. In this test, 21 mainly bimanual, activities are rated by the children’s parents on a 3-point scale (0=impossible, 1=difficult, 2=easy), describing their child’s perceived difficulty in performing each activity. Total maximum score was 42 and show the activities were easy24).
Functional independence was assessed using the WeeFIM. This is a useful tool for assessing functional status in children with neurodevelopmental disabilities; it includes 18 items scored on a 7-level ordinal scale. The reliability and stability of the scale has been proven25, 26). In the current study, the WeeFIM self-care domain was assessed.
All assessments were performed twice: once at the start of the treatment program and again at the end of the 6-week program. In addition, a user satisfaction questionnaire was administered to the patients in group 1. This questionaire assessed parameters related to virtual reality games including the level of difficulty of the game, motivation, cognitive abilities, and physical effort of the player27).
Statistical analyses were performed using SPSS v.18.0 for Windows. A value of p<0.05 was considered statistically significant for all analyses. Baseline characteristics were compared using the independent samples t test and the chi- square test. A comparison of the groups was made using the independent samples t-test for the Jebsen Taylor Hand Function Test and the Mann-Whitney U test for the Quality of Upper Extremity Skills Test, ABILHAND-Kids test, and WeeFIM with an intention-to-treat analysis of the difference between the baseline and final scores with a 95% confidence interval. The paired sample t-test was used to compare JTHFT outcomes before and after treatment. While the Wilcoxon Signed-Rank test was used to compare other outcomes before and after treatment. The Mann-Whitney U test was used to compare improvements and differences between the groups.
RESULTS
From the 33 patients with CP who were referred, 30 were included in the study for evaluation and were divided into 2 groups (Fig. 1). All patients completed the study. There were no significant differences between the groups with respect to demographics, clinical features, or baseline test scores (Tables 1 and2).
Table 1. The demographics and clinical features of the participants.
| NDT+NW (n=15) | NDT (n=15) | ||
|---|---|---|---|
| Age (years) (mean± SD) | 9.53 ± 3.04 | 9.73 ± 2.86 | * |
| Gender (F/M) (n) | 7/8 | 9/6 | ** |
| MACS (medianscore- range) | 2 (range 1–3) | 2 (range 1–3) | * |
| Effected extremity (right/left) | 8/7 | 10/5 | ** |
| GMFCS | 9 cases-2 | 9 cases-2 | * |
| 6 cases-1 | 6 cases-1 |
SD: standard deviation, F: female, M: male, NDT+NW: Neurodevelopment Treatment+Nintendo Wii, NDT: Neurodevelopment Treatment, MACS: Manual Ability Classification System, GMFCS: Gross Motor Function Classification System. *t-test. **χ2 test
Table 2. Results of outcomes for two groups before and after the treatment.
| NDT+NW group | Before Mean (SD) | After Mean (SD) | Mean change (SD) |
| QUEST Dissociated movements (score) | 80.1 (7.73) | 85.6 ( 8.54) | 5.5 (4.40)* |
| QUEST Grasps (score) | 42.2 (18.76) | 47.1 (16.64) | 4.9 (3.61)* |
| QUEST Weight bearing (score) | 69.2 (19.46) | 72.7 (19.60) | 3.5 (5.79)* |
| QUEST Protective extension (score) | 72.9 (14.78) | 77 (12.66) | 4.0 (4.56)* |
| JTHFT (s) | 40.4 (16.44) | 32.9 (14.88) | 0.7 (0.99)* |
| ABILHAND-Kids (logits) | 0.56 (2.34) | 1.33 ( 2.04) | 0.73 (1.16)* |
| WeeFIM (score) | 46 (8.23) | 46.7 (7.51) | 7.5 (4.82)* |
| NDT group | |||
| QUEST Dissociated movements (score) | 81.4 (10.70) | 86.4 (8.78) | 5.0 (4.94)* |
| QUEST Grasps (score) | 53 (16.45) | 55.7 (15.30) | 2.7 (4.62) |
| QUEST Weight bearing (score) | 75.4 (17.07) | 77.3 (15.43) | 1.8 (7.15) |
| QUEST Protective extension (score) | 71 (23.52) | 74 (23.36) | 2.9 (6.84) |
| JTHFT (s) | 31.5 (9.57) | 29.9 (8.83) | 0.4 (0.27)* |
| ABILHAND-Kids (logits) | 1.07 (1.90) | 1.51 ( 1.70) | 0.60 (0.63)* |
| WeeFIM (score) | 48.3 (7.27) | 48.9 (7.14) | 1.5 (1.93)* |
NDT+NW: Neurodevelopment Treatment+Nintendo Wii, NDT: Neurodevelopment Treatment, QUEST: Quality of Upper Extremity Skills Test, JTHFT: Jebsen Taylor Hand Function Test. *Significantly different from pre-treatment p<0.05
Following the 6-week treatment program, statistically significant improvement was seen in the NDT+Wii group in the scores for all domains of QUEST (p=0.002, p=0.003, p=0.017, 0.005), JTHFT (p=0.001), ABILHAND-Kids (p=0.001), and WeeFIM self-care (p=0.026) scores. Statistically significant improvement was determined in the dissociated movements domain of the QUEST (p=0.007), JTHFT (p=0.001), ABILHAND-Kids (p=0.002), and WeeFIM-self-care (p=0.007) scores in the NDT group (Table 2).
The within-group analysis showed that the JTHFT score of the NDT+Wii group was superior to that of the group receiving neurodevelopmental treatment only (p=0.000). There were no significant differences between groups with respect to the other test scores. The results of the User Satisfaction Questionnaire completed by the NDT+Wii group are shown in Table 3. Five children found boxing and playing tennis and baseball too easy, and seven children found the games easy. Fourteen children found the moving objects in the games interesting. Eleven children found all games attractive. All children experienced more fun playing the games compared with their regular therapy. All children were motivated to play the boxing and tennis and baseball games.
Table 3. User satisfaction questionnary: answers in frequencies (n=15).
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| Wii: presentation | |||||
| I could see all things in the game very well | - | - | - | 7 | 8 |
| I found the moving things/objects in the game very interesting | - | 1 | - | 9 | 5 |
| The things I saw in the game were very attractive | - | - | - | 2 | 13 |
| The game reacted good on my movements | - | 2 | 2 | 5 | 6 |
| I could hear all sounds very well | - | 1 | - | 4 | 10 |
| The sounds I heard out of the game were very attractive | - | 1 | - | 4 | 10 |
| I could not hear where all sounds out of the game did come from | 6 | 3 | 3 | 3 | - |
| Wii : level of difficulty | |||||
| The game was too hard | 3 | 5 | - | 7 | - |
| I still must learn a lot, before I can play this game | - | 7 | 1 | 5 | 2 |
| I had the feeling I could win | - | - | - | 6 | 9 |
| The game was too easy | - | 8 | 2 | 5 | - |
| Player: motivation | |||||
| I would find it nice if I could play the game together with more children at the same time | - | - | - | - | 15 |
| I liked it that the game was getting more difficult | - | 2 | 2 | 6 | 5 |
| The game was so attractive that I lost all count of time | - | - | - | 4 | 11 |
| I would not like to play this game more often | 10 | 1 | 2 | - | 2 |
| Wii training is less fun than regular physiotherapy | - | - | - | - | 15 |
| Player: cognitive capability | |||||
| This game was easy to understand | - | 1 | - | 6 | 8 |
| This game was easy to play | 1 | 1 | - | 8 | 5 |
| It was very logical playing the game by moving my arm/hand | 1 | - | 2 | 7 | 5 |
| My experience with playing the game looks like real life playing | 1 | 3 | - | 5 | 6 |
| Player: physical effort | |||||
| I found it hard to play the game by moving my hands | 3 | 9 | - | 3 | - |
| I became more tired from this game than from the regular physiotherapy | 2 | 6 | - | 5 | 2 |
| By playing the game, I learned new movements | - | 1 | - | 3 | 11 |
| I think I could learn new movements by playing the game more often | - | 1 | - | 3 | 11 |
1-completely disagree, 2-slightly disagree, 3-neutral, 4-slightly agree, 5-completely agree
DISCUSSION
In this study, the effects of NDT and NDT+NW on upper extremity functions, speed, manual ability, and level of independence in activities of daily living were comparatively investigated in the children with hemiparetic CP. In the study, improvements were achieved in functional ability, speed, manual ability, and the dissociated movements subgroup of the QUEST results in the group in which NDT (45 min) was applied for 6 weeks. On the other hand, improvements were observed in the results of all hand functions, speed and manual ability, and all subgroup scores of the QUEST scale in the group in which NDT+NW (30 min+15 min) was applied. The satisfaction questionnaire applied to the NDT+NW group showed that the children were extremely satisfied with the practice. Higher success rates were achieved in terms of speed in the group in which Nintendo Wii was added to NDT when compared with the NDT only group.
NDT is a global therapeutic approach that addresses all requirements of a child and aims to increase the child’s functionality and participation in daily life. Although this approach is not a therapeutic modality only for hand functions, it does include some activities in the session that address daily use of the hand5, 7, 8). In the literature, there are few studies that contain sufficient evidence and show the healing effect of the NDT approach on upper extremity functions of children28). For this reason, our study is important. However, the absence of a comparable “no treatment” control group is a limitation decreasing the power of our results. Data from the literature suggest that the use virtual reality positively affects participation of children in treatment and provides motivation and adaptation27, 29). In previous studies focusing on the upper extremity in CP, the study periods were 430), 625, 31, 32) and 8 weeks12, 33). Therefore, as in the literature, we preferred a study period of 6 weeks to compare Nintendo Wii and NDT practices. On the other hand, time spent on virtual reality generally varied between 20 minutes and 3, 5 hours, 3–5 days per week in the studies conducted using virtual reality13, 30, 33,34,35). As it has also been suggested in the literature, we thought that the Nintendo Wii, as a game-based approach, might be a useful part of rehabilitation for children with CP. Therefore, in our study, we evaluated the contribution of the Nintendo Wii to the upper extremity when used for a period of time period (15 min) during a routine NDT treatment session14).
Similar to our study, Shin et al. applied 15 minutes of Nintendo Wii game play in addition to 30 minutes of conventional neurologic treatment twice a week in children with cerebral palsy and obtained significant differences in eye-hand coordination and visual motor speed in comparison of a virtual reality training group with a conventional neurological physical therapy group36).
The children in our study also regarded the virtual reality games as a reward given at the end of NDT practices, but not as a treatment, which may be accepted as a condition that may increase motivation and cooperation. It was also clinically observed that the subjects in our study were more motivated to participate in the activities during the NDT session. This was also observed in the satisfaction questionnaires completed by the NDT+NW group at the end of the study. Since computer games have recently become an important from of entertainment, which may be addictive, in the lives of children lives, this interest and positive motivation in the children were expected.
In addition, the effort of the children to move quickly during Nintendo Wii practice to score in the game and play better versus the computer might be the reason for the higher scores in the NDT+NW group when compared with the NDT only group. It might be accepted as a limitation that we obtained no records of the scores obtained by the children in the games at the beginning and end of the study. Comparison of the scores between the beginning and end of treatment might objectively show the development of the child’s ability to play the game. On the other hand, a powerful aspect of our study is that all cases had homogeneously hemiplegic type cerebral palsy.
The QUEST has been used to measure the results in studies on virtual reality35, 37). In our study, the posttreatment QUEST scores of all participants in the NDT+NW group were better compared with those of the NDT group (p<0.05). We think that achieving a statistically significant increase in NDT+NW group with regard to weight bearing and protective extension scores at the end of 6 weeks might be related to the effort of the children to move their arms to better grasp and use the Nintendo Wii game console. During the practice, it was also clinically observed that some children were unable to firmly grasp Nintendo Wii game console at the beginning of treatment, but were better able to grasp and control the Wii Nunchuk at the end of 6-week treatment period. The posttreatment increase in QUEST grasps scores especially supports this clinical observation.
In our study, JTHFT scores improved in both groups when compared with those for the to pretreatment period. Although there was no statistically significant difference between the two groups in terms of JTHFT results, it was observed that the NDT+NW group completed the test 6 seconds earlier, on average, at the end of the 6-week treatment period. This outcome indicates that the use Nintendo Wii games was more effective than NDT in increasing the speed of movement. In general, an important question about virtual reality practices is about whether achieved gains “contribute to real life activities.” In our study, among the cases tested by a method that includes measurements obtained using functional real life activities, such as the JTHFT, the better results in the Nintendo Wii group represent evidence showing that gained obtained by virtual environment therapies might be transmitted to real life. There are also some other studies presented in the literature demonstrating that similar successful results have been achieved regarding the transmission of through virtual reality therapy skills gained here to real life15, 33).
In our study, independence of the children was evaluated with the WeeFIM, which revealed similar developments in both groups in terms of eating, care, bathing, and the upper and lower trunk dressing fields. There is one study in the literature that included a case with hemiplegic CP and showed results similar to our findings in terms of improvement in daily self-care activities15). Furthermore, a posttreatment improvement was observed in both groups in terms of the scores of the ABILHAND-Kids which was previously used in studies in which virtual reality was applied to measure specific daily life skills of the hand31, 35), while no significant difference was present between the groups. We could measure these functional gains in our study only at the questionnaire level. We suggest that magnetic resonance imaging of this kind of gain might increase the objectivity and power of further studies.
The part of the user satisfaction questionnaire concerning the difficulty of the Nintendo Wii games, all children in the NDT+NW group in our study stated that they could “win the games” in spite of their physical limitations. This situation may indicate that the games strongly motivated the children who tried the virtual reality games, in spite of their physical limitations. Some children stated that the games were more tiring than the other methods applied in NDT. Although they were very tired, all children stated that playing with the Nintendo Wii was much more fun when compared to conventional therapy. In addition, all cases specified that the games were attractive and that they lost track of time during therapy. We interpreted this situation as indicating that supporting traditional therapies, which become boring and monotone for children during long rehabilitation periods in children with CP, with virtual reality games might increase the motivation of children in therapy. Virtual reality games, which have become a part of daily life, make children perform desired activities voluntarily and in a more motivated way. These results suggest that the children were very pleased with the virtual reality games added to therapy.
The game console used in this study relies mostly on use a controller, it was observed that the children with CP sometimes lost control of the controller due to excitement-related increased spasticity and that the device failed to sense their movements. We think that further studies are required that, include a higher number of participants and use more current systems with sensors sensitive to not only movements of a controller but also all body movements.
In conclusion, application of Nintendo Wii virtual reality games combined with NDT had benefical effects on upper extremity functions, upper extremity speed, and independence level in daily life activities in the children with hemiplegic CP. The increase in speed was more prominent in the NDT+NW group than in the NDT group. Since the Nintendo Wii increases motivation and provides on opportunity for enjoyable therapy, we think that it increases adaptation of children to rehabilitation programs and that it may be added to conventional treatment programs. Use of virtual reality as a treatment modality for improving functionality in children is considered a rich study field in which further results may be obtained from randomized studies with larger sample sizes and control groups.
REFERENCES
- 1.Himmelmann K: Epidemilogy of cerebral palsy. In: Handbook of Clinical Neurology Volume 111, Pediatric Neurology Part I, 3rd ed. Amsterdam: Elsevier, 2013, pp 163–169. [DOI] [PubMed] [Google Scholar]
- 2.Surveillance of Cerebral Palsy in Europe: Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol, 2000, 42: 816–824. [DOI] [PubMed] [Google Scholar]
- 3.Basu AP, Pearse J, Kelly S, et al. : Early intervention to improve hand function in hemiplegic cerebral palsy. Front Neurol, 2014, 5: 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arner M, Eliasson AC, Nicklasson S, et al. : Hand function in cerebral palsy. Report of 367 children in a population-based longitudinal health care program. J Hand Surg Am, 2008, 33: 1337–1347. [DOI] [PubMed] [Google Scholar]
- 5.Bobath B, Bobath K: The Neuro-Developmental Treatment, Management of the Motor Disorders of Children with Cerebral Palsy. Clinics in Developmental Medicine 90. Oxford: Spastics International Medical Publications, 1984, pp 6–18. [Google Scholar]
- 6.Mayston MJ: The Bobath Concept—evolution and application. Movement disorders in children. International Sven Jerring Symposium, Stockholm, August 1991: Proceedings. Med Sport Sci, Basel, Karger, 1992, 36, 1–6. [Google Scholar]
- 7.Law M, Russell D, Pollock N, et al. : A comparison of intensive neurodevelopmental therapy plus casting and a regular occupational therapy program for children with cerebral palsy. Dev Med Child Neurol, 1997, 39: 664–670. [DOI] [PubMed] [Google Scholar]
- 8.Tsorlakis N, Evaggelinou C, Grouios G, et al. : Effect of intensive neurodevelopmental treatment in gross motor function of children with cerebral palsy. Dev Med Child Neurol, 2004, 46: 740–745. [DOI] [PubMed] [Google Scholar]
- 9.Farr W, Male I: British Association for Community Child Health/Child Protection Special Interest Group G216 a meta-analysis of “Wii Therapy” in children with cerebral palsy. Arch Dis Child, 2013, 98: A97. [Google Scholar]
- 10.AlSaif AA, Alsenany S: Effects of interactive games on motor performance in children with spastic cerebral palsy. J Phys Ther Sci, 2015, 27: 2001–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shumway-Cook A, Woollacott MH: Motor control theory and practical applications. Maryland: Lippincott Williams and Wilkins, 2001. [Google Scholar]
- 12.Lotze M, Braun C, Birbaumer N, et al. : Motor learning elicited by voluntary drive. Brain, 2003, 126: 866–872. [DOI] [PubMed] [Google Scholar]
- 13.Exner CE: Intervention for children with hand skill problems. Hand Function in the Child: Foundations for Remediation. Missouri: Mosby Elsevier, 2006, pp 239–266. [Google Scholar]
- 14.Reid DT: The use of virtual reality to improve upper-extremity efficiency skills in children with cerebral palsy: a pilot study. Technol Disabil, 2002, 14: 53–61. [Google Scholar]
- 15.You SH, Jang SH, Kim YH, et al. : Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev Med Child Neurol, 2005, 47: 628–635. [PubMed] [Google Scholar]
- 16.Luna-Oliva L, Ortiz-Gutiérrez RM, Cano-de la Cuerda R, et al. : Kinect Xbox 360 as a therapeutic modality for children with cerebral palsy in a school environment: a preliminary study. NeuroRehabilitation, 2013, 33: 513–521. [DOI] [PubMed] [Google Scholar]
- 17.Lee KH: Effects of a virtual reality-based exercise program on functional recovery in stroke patients: part 1. J Phys Ther Sci, 2015, 27: 1637–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tarakci D, Ozdincler AR, Tarakci E, et al. : Wii-based balance therapy to improve balance function of children with cerebral palsy: a pilot study. J Phys Ther Sci, 2013, 25: 1123–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eliasson AC, Krumlinde-Sundholm L, Rösblad B, et al. : The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol, 2006, 48: 549–554. [DOI] [PubMed] [Google Scholar]
- 20.Can Child Centre for Childhood Disability Research: http://motorgrowth.canchild.ca/en/GMFCS/originalversion.asp (Accessed Apr. 11, 2015)
- 21.DeMatteo C, Law M, Russell D, et al. : The reliability and validity of Quality of Upper Extremity Skills Test. Phys Occup Ther Pediatr, 1993, 13: 1–18. [Google Scholar]
- 22.Jebsen RH, Taylor N, Trieschmann RB, et al. : An objective and standardized test of hand function. Arch Phys Med Rehabil, 1969, 50: 311–319. [PubMed] [Google Scholar]
- 23.Taylor N, Sand PL, Jebsen RH: Evaluation of hand function in children. Arch Phys Med Rehabil, 1973, 54: 129–135. [PubMed] [Google Scholar]
- 24.Arnould C, Penta M, Renders A, et al. : ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology, 2004, 63: 1045–1052. [DOI] [PubMed] [Google Scholar]
- 25.Ottenbacher KJ, Taylor ET, Msall ME, et al. : The stability and equivalence reliability of the functional independence measure for children (WeeFIM). Dev Med Child Neurol, 1996, 38: 907–916. [DOI] [PubMed] [Google Scholar]
- 26.Msall ME, DiGaudio K, Rogers BT, et al. : The Functional Independence Measure for Children (WeeFIM). Conceptual basis and pilot use in children with developmental disabilities. Clin Pediatr (Phila), 1994, 33: 421–430. [DOI] [PubMed] [Google Scholar]
- 27.Jannink MJ, van der Wilden GJ, Navis DW, et al. : A low-cost video game applied for training of upper extremity function in children with cerebral palsy: a pilot study. Cyberpsychol Behav, 2008, 11: 27–32. [DOI] [PubMed] [Google Scholar]
- 28.Kerem Gunel M, Kaya Kara O, Ozal C, et al. : Virtual Reality in Rehabilitation of Children with Cerebral Palsy, Cerebral Palsy − Challenges for the Future. http://www.intechopen.com/books/cerebral-palsy-challenges-for-the-future/virtual-reality-in-rehabilitation-of-children-with-cerebral-palsy (Accessed May 1, 2015)
- 29.Deutsch JE, Borbely M, Filler J, et al. : Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther, 2008, 88: 1196–1207. [DOI] [PubMed] [Google Scholar]
- 30.Chen YP, Kang LJ, Chuang TY, et al. : Use of virtual reality to improve upper-extremity control in children with cerebral palsy: a single-subject design. Phys Ther, 2007, 87: 1441–1457. [DOI] [PubMed] [Google Scholar]
- 31.Winkels DG, Kottink AI, Temmink RA, et al. : Wii™-habilitation of upper extremity function in children with cerebral palsy. An explorative study. Dev Neurorehabil, 2013, 16: 44–51. [DOI] [PubMed] [Google Scholar]
- 32.Chiu HC, Ada L, Lee HM: Upper limb training using Wii Sports Resort for children with hemiplegic cerebral palsy: a randomized, single-blind trial. Clin Rehabil, 2014, 28: 1015–1024. [DOI] [PubMed] [Google Scholar]
- 33.Burdea GC, Jain A, Rabin B, et al. : Long-term hand tele-rehabilitation on the PlayStation 3: benefits and challenges. Conf Proc IEEE Eng Med Biol Soc, 2011, 2011: 1835–1838. [DOI] [PubMed] [Google Scholar]
- 34.Rahman SA, Shaheen AA: Virtual reality use in motor rehabilitation of neurological disorders: a systematic review. Middle East J Sci Res, 2011, 7: 63–70. [Google Scholar]
- 35.Zoccolillo L, Morelli D, Cincotti F, et al. : Video-game based therapy performed by children with cerebral palsy: a cross-over randomized controlled trial and a cross-sectional quantitative measure of physical activity. Eur J Phys Rehabil Med, 2015, [Epub ahead of print]. [PubMed] [Google Scholar]
- 36.Shin JW, Song GB, Hwangbo G: Effects of conventional neurological treatment and a virtual reality training program on eye-hand coordination in children with cerebral palsy. J Phys Ther Sci, 2015, 27: 2151–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reid D, Campbell K: The use of virtual reality with children with cerebral palsy: a pilot randomized trial. Ther Recreation J, 2006, 40: 255–268. [Google Scholar]