Abstract
Herein, we reported a catastrophic condition as the almost complete rupture of trachea associated with esophageal lesion following an urgent surgical tracheostomy performed for unexpected difficult intubation. The extent of lesions required a surgical management. We decided against a resection and an end to end anastomosis but preferred to perform a direct suture of the lesion due to the presence of local and systemic infection. Then, the diagnosis of a tracheal fistula led us to perform a direct suture of the defect that was covered with muscle flaps. Actually the patient is alive without problems. Emergency situations as unexpected airway difficult intubation increase morbidity and mortality rate of tracheostomy also in expert hands. Sometimes these events are unpredictable. Mastery with a number of advanced airway technique should be sought when faced dealing with unexpected difficult intubations and written consent of such a concern should be given to the patient.
Keywords: Catastrophic complication, tracheostomy, tracheal lesion, esophageal lesion
Introduction
Tracheostomy is a routine life-saving operative procedure despite fatal complications may occur when it is performed in emergent situation as difficult air-way.
Herein, we reported a catastrophic condition as the almost complete rupture of trachea associated with esophageal lesion following an urgent surgical tracheostomy performed for unexpected difficult intubation.
Case presentation
A 61-year-old female was scheduled for elective arthroscopic scapular surgery. The unexpected difficult air-way and the cardiac arrest required an urgent surgical tracheostomy performed by the same orthopedic. After cardiopulmonary resuscitation, she was transferred to the intensive care unit and five days later to our institution.
The patient presented clinical and laboratory signs of local and systemic infection. Computed tomography scan of neck and chest showed a cervico-mediastinal collection and an almost complete tracheal wall section (Figure 1). After a multidisciplinary meeting, we decided for surgery.
Figure 1.
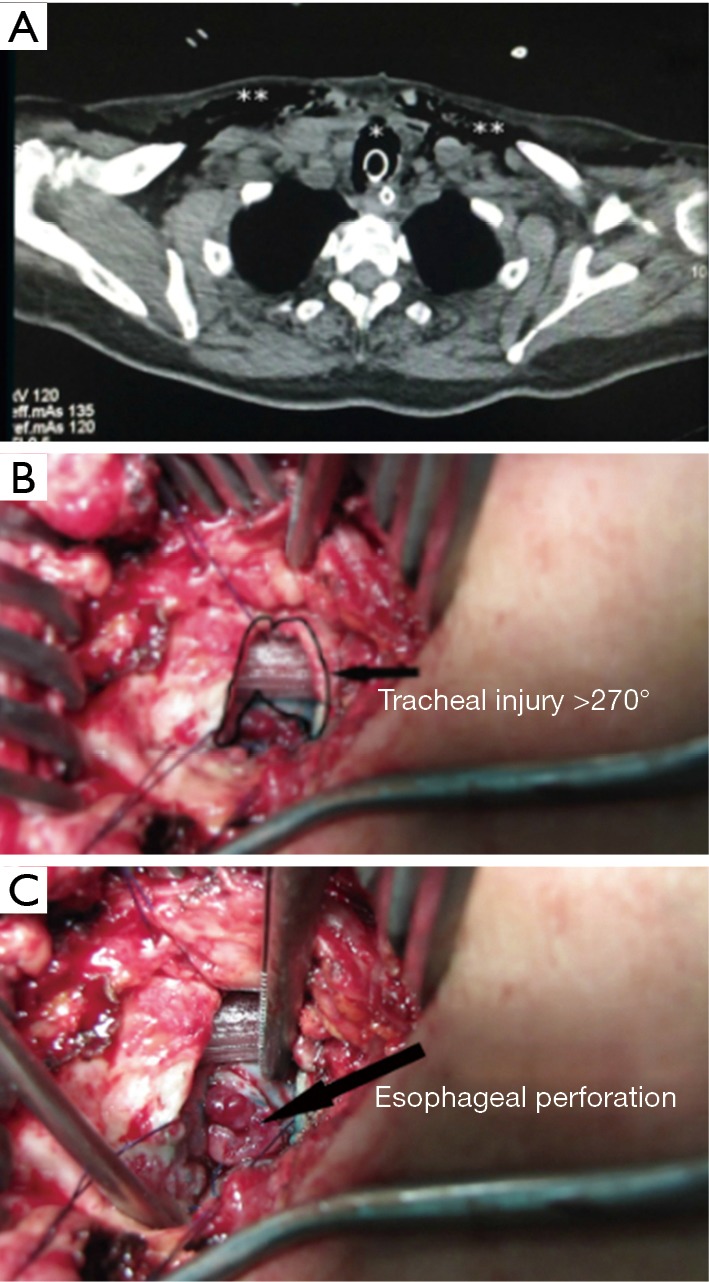
Operative view showed a large defect of trachea associated with esophageal perforation. (A) Computed tomography scan of neck and chest showed a large defect of the trachea* with subcutaneous emphysema**; (B) operative view showed the tracheal; and (C) esophageal lesions.
The operation is summarized in Figure 2. We performed a cervicotomy incision with exposure of tracheal (Figure 1B) and esophageal (Figure 1C) defects that were repaired with interrupted stitches after debridement of necrotic materials (Figure 3A). Three cervical 16 Fr drains on suction were positioned, two in both lateral tracheal side and one in the mediastinum along the pre tracheal plan. Then a right thoracotomy was performed for irrigation of mediastinum and pleural cavity with povidone-iodine solutions. A 24-Fr drain was positioned close to esophageal perforation to avoid spillage in case of post-operative esophageal fistula. Two 28-Fr chest drains were also positioned in the pleural cavity.
Figure 2.

The video edited the main steps of surgical procedure as the surgical repair of the tracheal and esophageal defect due to tracheostomy and the suture of the postoperative tracheal fistula reinforced with muscle flaps. Endoscopic control 24 months later showed normal healing of tracheal lesion (1). Available online: http://www.asvide.com/articles/958
Figure 3.
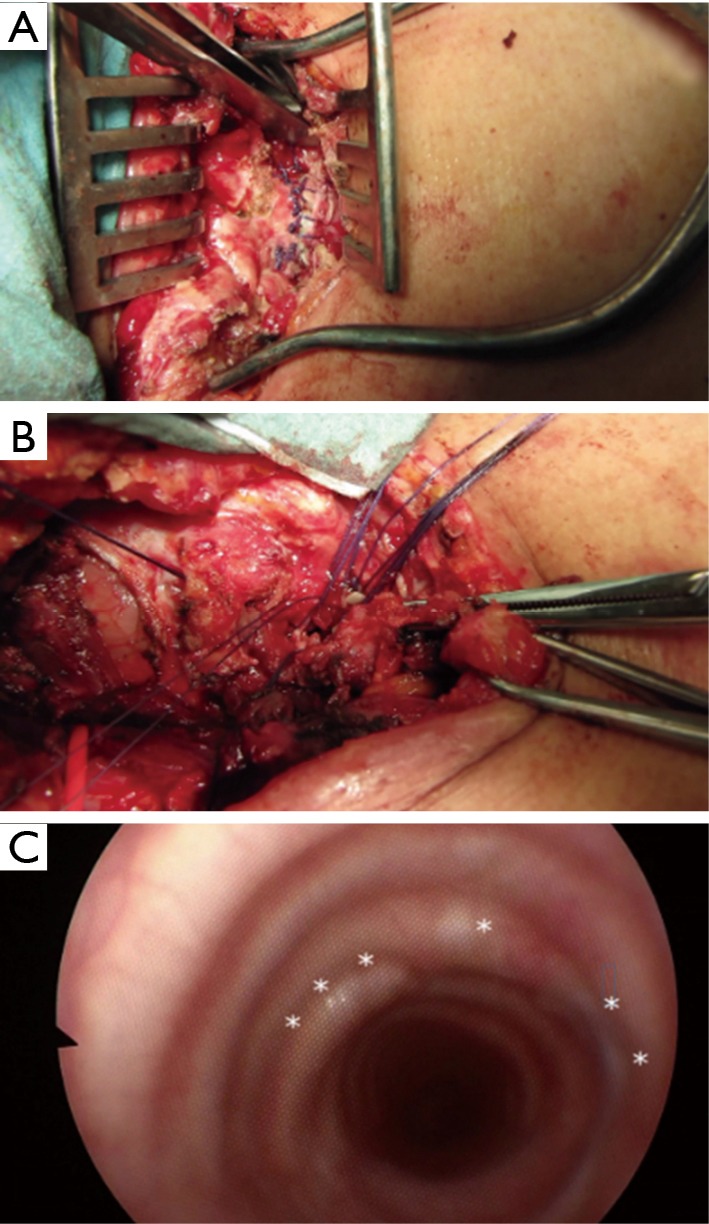
The defect of the trachea was sutured and bronchoscopic check 24 months later showed no defect. (A) The tracheal lesion was repaired with interrupted stitches; (B) on post-operative day 12, a fistula of the right antero-lateral tracheal wall occurred; (C) it was repaired with direct suture and covered with muscle flaps. Endoscopic control 24 months later showed no tracheal defect and normal airway patency.
The patient was transferred to the intensive care unit; she was ventilated with low-tidal volumes and airway pressures to preserve the tracheal closure and was extubated 48 hours later. Antibiotic therapy was given based on airway and blood cultures. Repeated flexible bronchoscopies were performed make air way free from secretions and to exclude any tracheal defects or fistulas. The cervical and chest drains were removed five days later.
Unfortunately, on post-operative day 12 she developed a subcutaneous emphysema due to a fistula of the right antero-lateral tracheal wall (Figure 3B). Thus, she was re-operated and tracheal defect was repaired with separate absorbable stitches and the suture line reinforced with muscle flaps including digastric, sternocleidomastoid, and right sternothyroid muscles. The patient was extubated in the operating room and transferred to the ward. The 24 Fr drain positioned near the repaired esophageal perforation was maintained in place owing to a moderate leak, replaced with a 20 Fr drain in post-operative day number 21, with a 16-Fr drain in post-operative day 40 and removed in post-operative day 67. The patient had a successful surgical outcome and discharge in post-operative day number 75. At the 24-months follow-up, she was in good clinical conditions; bronchoscopy showed a patent tracheal lumen (Figure 3C).
Discussion
Approximately 230 million major surgical procedures are performed annually worldwide (2), 4% of tracheal intubation is unexpectedly difficult and 30% of incidents totally attributable to anesthesia are due to difficult in airway management (3). A recent survey reported that there are approximately 1,000 catastrophic events and approximately 500 tracheotomy-related deaths in the United States annually (4). Of these, tracheoinnominate artery fistula is the catastrophic complication related to tracheostomy mostly reported in literature.
In the present case, we reported an exceptional case as the subtotal lesion of the trachea and esophagus following an urgent tracheostomy. The extent of lesions required a surgical management. We decided against a resection and an end to end anastomosis but preferred to perform a direct suture of the lesion due to the presence of local and systemic infection. Then, the diagnosis of a tracheal fistula led us to perform a direct suture of the defect that was covered with muscle flaps.
In this case, the anesthetist was unable to intubate the patient also with the aid of bronchoscopy for the laryngeal trauma due to the several attempts of intubation and the patient was at high risk for brain damage and death due to severe and prolonged hypoxia. Thus, orthopedic performed a large and deep collar incision without any care for preserving the anatomical integrity of the trachea and of adjacent structures. It is questionable if the poor familiarity of the operator with tracheostomy, being an orthopedic, favored this dramatic complication but certainly the urgent situation situation had an important weight on outcome. In fact, emergency situations also in expert hands increase morbidity and mortality rate of tracheostomy (5).
Conclusions
Our case under lights that catastrophic complications following tracheostomy are always possible and that a multidisciplinary consult, a prompt diagnosis and reconstructive surgery improve prognosis. Although there are different methods to evaluate predictive parameters of difficult intubation in patients without risk factors, sometimes these events are unpredictable.
Mastery with a number of advanced airway technique should be sought when faced dealing with unexpected difficult intubations and written consent of such a concern should be given to the patient (6).
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Caronia FP, Arrigo E, Santini M, et al. The video edited the main steps of surgical procedure as the surgical repair of the tracheal and esophageal defect due to tracheostomy and the suture of the postoperative tracheal fistula reinforced with muscle flaps. Asvide 2016;3:202. Available online: http://www.asvide.com/articles/958
- 2.Pearse RM, Moreno RP, Bauer P, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet 2012;380:1059-65. 10.1016/S0140-6736(12)61148-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmidt U, Eikermann M. Organizational aspects of difficult airway management: think globally, act locally. Anesthesiology 2011;114:3-6. 10.1097/ALN.0b013e318201c6ff [DOI] [PubMed] [Google Scholar]
- 4.Das P, Zhu H, Shah RK, et al. Tracheotomy-related catastrophic events: results of a national survey. Laryngoscope 2012;122:30-7. 10.1002/lary.22453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waldron J, Padgham ND, Hurley SE. Complications of emergency and elective tracheostomy: a retrospective study of 150 consecutive cases. Ann R Coll Surg Engl 1990;72:218-20. [PMC free article] [PubMed] [Google Scholar]
- 6.Connelly NR, Ghandour K, Robbins L, et al. Management of unexpected difficult airway at a teaching institution over a 7-year period. J Clin Anesth 2006;18:198-204. 10.1016/j.jclinane.2005.08.011 [DOI] [PubMed] [Google Scholar]


