Abstract
Background:
Attritional bone loss in patients with recurrent anterior instability has successfully been treated with a bone block procedure such as the Latarjet. It has not been previously demonstrated whether cortical or cancellous screws are superior when used for this procedure.
Purpose:
To assess the strength of stainless steel cortical screws versus stainless steel cannulated cancellous screws in the Latarjet procedure.
Study Design:
Controlled laboratory study.
Methods:
Ten fresh-frozen matched-pair shoulder specimens were randomized into 2 separate fixation groups: (1) 3.5-mm stainless steel cortical screws and (2) 4.0-mm stainless steel partially threaded cannulated cancellous screws. Shoulder specimens were dissected free of all soft tissue and a 25% glenoid defect was created. The coracoid process was osteomized, placed at the site of the glenoid defect, and fixed in place with 2 parallel screws.
Results:
All 10 specimens failed by screw cutout. Nine of 10 specimens failed by progressive displacement with an increased number of cycles. One specimen in the 4.0-mm screw group failed by catastrophic failure on initiation of the testing protocol. The 3.5-mm screws had a mean of 274 cycles (SD, ±171 cycles; range, 10-443 cycles) to failure. The 4.0-mm screws had a mean of 135 cycles (SD, ±141 cycles; range, 0-284 cycles) to failure. There was no statistically significant difference between the 2 types of screws for cycles required to cause failure (P = .144).
Conclusion:
There was no statistically significant difference in energy or cycles to failure when comparing the stainless steel cortical screws versus partially threaded cannulated cancellous screws.
Clinical Relevance:
Latarjet may be performed using cortical or cancellous screws without a clear advantage of either option.
Keywords: shoulder instability, Latarjet, biomechanics, general sports trauma, glenoid bone loss
Recurrent instability of the shoulder occurs 67% of the time after arthroscopic soft tissue stabilization when significant attritional glenoid bone loss is present.10,21 In these patients, osseous procedures are more effective at restoring glenohumeral stability than soft tissue procedures.2,3 Glenoid bone defects can be reconstructed with iliac crest autograft,17,22 allograft, or coracoid transfer. Biomechanical studies have noted superiority of coracoid transfer procedures such as the Bristow and Latarjet procedures compared with purely structural grafts due to the advantage conveyed by the soft tissue attachments to the coracoid tip.6,7,24
Latarjet13 first described coracoid bone transfer in 1954 to address glenoid bone loss in patients with recurrent anterior instability of the shoulder. This involves transferring the coracoid process to the anteroinferior margin of the glenoid. Fixation of the graft is typically obtained with 2 screws. Stability is imparted via 2 mechanisms: the soft tissue sling composed of the conjoint tendon and the osseous augmentation of the glenoid contour with the coracoid graft. Prior biomechanical studies have demonstrated the importance and relative contribution of the surrounding soft tissues in the native and reconstructed shoulder.15,23,26 While often successful, complications have been described after the Latarjet procedure and may be due to malunion or nonunion of the graft as well as hardware complications.28 A variety of screws can be used for fixation during the Latarjet procedure, but the strength of fixation for each type of screw is still unknown. In this study, we aim to determine the strength and modes of failure of 2 types of screws used for the Latarjet procedure. As cortical screws have a higher pitch thread compared with the cancellous screws, theoretically resulting in greater purchase of the far cortex, we hypothesize that 3.5-mm cortical screws will be biomechanically stronger than 4.0-mm cannulated screws.
Methods
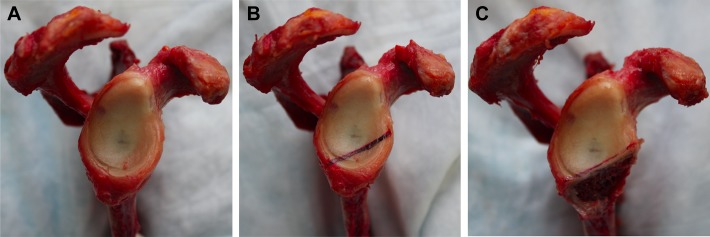
Ten fresh-frozen matched-pair shoulder specimens from 3 male and 2 female cadavers (mean age, 56.6 years; range, 32-67 years at time of death) were randomized to undergo the Latarjet procedure via 1 of 2 separate fixation techniques: (1) two 3.5-mm stainless steel cortical screws or (2) two 4.0-mm cannulated cancellous stainless screws. All shoulder specimens had a bone densitometry performed prior to preparation (mean, 0.516 mg/cm2; range, 0.396-0.657 mg/cm2). Shoulder specimens were dissected free of all soft tissue, and the glenoid was osteotomized. As previously described by Itoi et al,10 an osteotomy was performed to replicate a 25% glenoid and typical attritional bone loss (Figure 1). The individualized template was placed on top of each glenoid, and line 2 was used to mark a 25% glenoid defect. The coracoid process was osteotomized proximal to its angle and then fixed flush with its long axis parallel to the glenoid defect using two 0.62-mm Kirschner wires for provisional fixation using the congruent arc method.5
Figure 1.
(A) Glenoid dissected free of all soft tissue. (B) Osteotomy depicting 25% attritional bone loss as previously described by Itoi et al.10 (C) Glenoid after completion of osteotomy.
For specimens in group 1 (3.5-mm screw; Stryker Orthopaedics), a 3.5-mm drill bit was used to over-drill the near cortex (coracoid graft) in a parallel fashion to the provisional Kirschner wires and a 2.5-mm-diameter drill bit was used to drill the far cortex (glenoid neck). Both screw types were self-tapping and hence did not require tapping prior to placement. The screws were subsequently advanced using a 2-finger tightening technique to achieve bicortical fixation through the far cortex of the glenoid neck and to decrease the risk of fixation failure (Figure 2). To prevent rotational displacement, both Kirschner wires were removed once the screws were fully advanced. For specimens in group 2 (4.0-mm screw; Stryker Orthopaedics), two 0.62-mm Kirschner wires were initially placed parallel to each other, bicortically through the far cortex of the glenoid neck. The near and far cortices were over-drilled with a 2.7-mm cannulated drill bit. The 4.0-mm cannulated screws were placed over each of the 2 Kirschner wires and advanced until bicortical fixation was achieved through the far cortex of the glenoid neck.
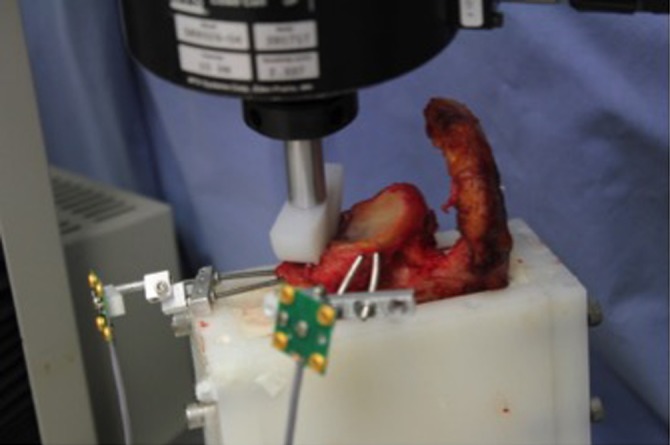
Figure 2.
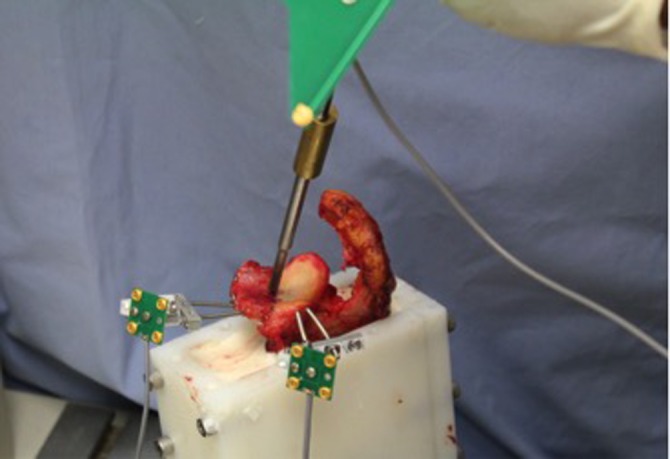
Points along the interface between the graft and the glenoid surface were obtained using a digitizing probe. Two infrared emitting targets can be seen: one attached to the graft and the other to the glenoid of the potted specimen.
Once the specimens were prepared, the scapula was potted into a rectangular plastic container using polymethylmethacrylate. The fixture holding the embedded glenoid was rigidly attached to the T-slot metal base plate of the material testing machine (MTS Insight; MTS Corp). Infrared emitting targets were rigidly attached to both the coracoid graft and the native glenoid. A probe and an optoelectronic motion measurement system (Optotrak Certus; Northern Digital Inc) were used to digitize points along the interface between the graft and glenoid at the level of the articular surface (Figure 2). The position of the points of the graft-glenoid interface relative to the infrared emitting targets rigidly attached to the glenoid and coracoid graft was determined after the digitizing process. Postexperiment data analysis was used to calculate graft-glenoid interface positions during the experiment using the experimentally measured motion of the 2 targets and the position of the digitized interface points relative to the targets. Any relative motion between the 2 targets produced a relative difference in calculated graft-glenoid interface positions. Graft migration was calculated by finding the maximum relative difference in calculated graft-glenoid interface position. This calculation technique is similar to the “interface displacement” calculation described by Giles et al.8 Custom Matlab programs (MathWorks Inc) were used to calculate graft migration.
The cadaveric specimens were tested immediately following completion of the Latarjet procedure. The humerus was positioned to mimic maximum abduction and external rotation to maximize the load applied to the graft. The load was applied in the medial direction, transverse to the glenoid surface representing a worst-case loading scenario (Figure 3). Cyclic loading protocol ensued at a rate of 0.25 mm/s with a load amplitude of 300 N in an attempt to keep the load rate low, however not to prolong the duration of testing. An initial maximum load of 325 N was applied to the graft based on low estimates of lowest glenohumeral contact force in abduction.1 A 25-N initial minimum load was chosen to ensure contact was maintained between the graft and the simulated humeral head. The minimum and maximum loads were increased by 25 N every 20 cycles until the end of testing was triggered by the operator based on visual assessment of graft migration. Applied load and the motion of the infrared markers were continuously recorded during testing. To standardize loading across specimens, a 12.7-mm-thick (0.5 inches) plastic hemidisk cut from 44.5-mm-diameter (1.75 inches) impact-resistant ultra-high–molecular weight polyethylene was used to apply force directly to the coracoid (Figure 4), as this would concentrate the entire force on the graft simulating a worst-case loading scenario. Failure was categorized as: (1) visible loosening of coracoid graft, (2) fracture of the coracoid graft, (3) pull out of screw, (4) screw breakage, or (5) coracoid graft migration 7 mm or more relative to the glenoid. Seven millimeters of relative displacement was selected as this magnitude of migration is twice the diameter of the smallest screws used in this study. The number of cycles, highest load, and total input energy at point of failure were determined from the load displacement data.
Figure 3.
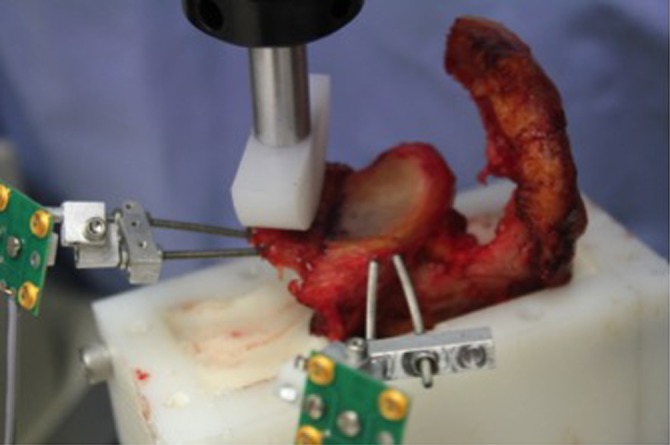
The graft was loaded using a hemispherical plastic piece acting as a simulation of the humeral head. The graft was directly loaded to mimic maximum abduction and external rotation of the arm.
Figure 4.
The experiment proceeded until 1 of the 5 defined failure points was reached. Note the medial displacement of coracoid graft.
Statistical Analysis
A power analysis was completed prior to conducting our experiment. Twenty-one specimens were required in each group (42 total specimens) to have an 80% power to detect a mean difference. A Wilcoxon Mann-Whitney test was used for statistical analysis.
Results
All 10 specimens in both groups failed by screw cut out (Figure 4). Nine of 10 specimens failed by progressive displacement with an increased number of cycles. One specimen in the 4.0-mm partially threaded stainless steel cannulated screw group and no specimens in the 3.5-mm stainless steel cortical screw group exhibited catastrophic failure on initiation of the testing protocol. It is possible the catastrophic failure may have been due to inadequate bony purchase during specimen preparation.
The 3.5-mm screws had a mean 274.2 cycles (SD, ±170.9 cycles; range, 10-443 cycles) to failure, and the 4.0-mm screws had a mean 135 cycles (SD, ±140.8 cycles; range, 0-284 cycles) to failure (P = .144).
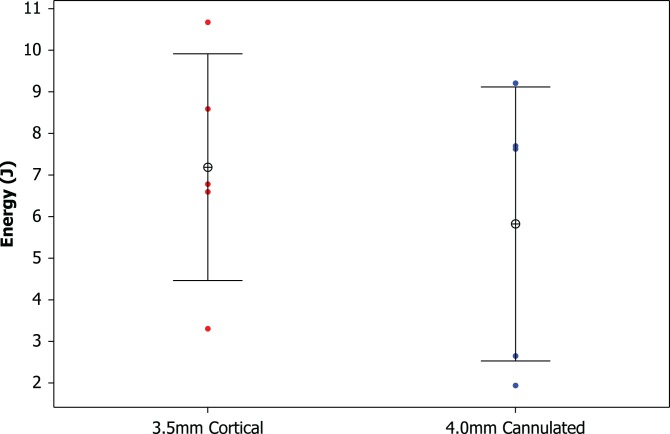
As each specimen was tested and the number of cycles increased, there was an increase in the loading force at 11 time points throughout the entire testing cycle. The increased loading force at the different time points assessed the energy required to cause screw failure. The 3.5-mm screws required a mean 7.19 J (1 J = 1 Nċm) to failure (SD ±2.73 J; range, 3.30-10.67 J). The 4.0-mm screws required a mean 5.82 J to failure (SD ±3.29 J; range, 1.94-9.21 J) (P = .676) (Figure 5). We performed a separate analysis with the exclusion of the catastrophic failure specimen to see if this would create a statistically significant difference. Despite the exclusion of the catastrophically failed specimen, no statistically significant difference was identified between the 2 screw types.
Figure 5.
Individual plot of energy comparing 3.5-mm cortical screws with 4.0-mm cannulated screws.
Discussion
The Latarjet procedure is being increasingly used for patients with recurrent shoulder instability and glenoid bone deficiency. Clinically, the Latarjet procedure has been successful in treating the young, high-demand athlete with glenoid deficit or hyperlaxity.2,3 Both the osseous block and the soft tissue sling contribute to the stability conveyed by the Latarjet procedure, and previous studies have demonstrated their relative effects.26 However, methods of fixation of the bony block have not been evaluated. The purpose of this study was to isolate the osseous block and examine the biomechanical strength of solid versus cannulated screws for fixation of the coracoid graft for the Latarjet procedure.
The current study failed to show a difference in the mean number of cycles to failure or energy to failure between the 2 screw types. Our testing protocol was devised in an attempt to provide uniform loading of the coracoid graft to replicate a worst-case scenario so that any differences in fixation strength between the groups could be quantified. As suggested by Shah et al,19 there may be other factors, such as smoking and workers’ compensation status, that may have contributed to failure and recurrent instability in their series. Although we noted no difference in load to failure, it was concerning that in our study 1 of the specimens in the cannulated fixation group failed catastrophically immediately on initiation of testing.
When the Latarjet procedure is performed with 2 parallel metal screws as an open procedure it has excellent long-term results with coracoid graft healing and low recurrence of instability.11,16 However graft malpositioning was the greatest contributor to repeat episodes of instability.14 Positioning of the coracoid graft is important to prevention of recurrent instability and allowing the graft to successfully unite. Inappropriate positioning can lead to inadvertent screw paths. If the graft is placed too far superiorly, the anterior screw may potentially injure the suprascapular nerve,12,20 and conversely, if the graft is placed too inferior then the inferior screw may have insufficient purchase to provide adequate stability to the graft.9,25 Intraoperative fractures may also occur because of screws being placed too close to the periphery of the graft or too close to each other.20 An argument can be made that cannulated screws may make screw placement easier in being able to first achieve preliminary fixation via a guide wire while also confirming trajectory and minimizing loss of positioning.14 Some studies have found cortical screws to be biomechanically stronger than cannulated systems4,27 while others have demonstrated similar pullout strength with the 2 screw types.14 Additionally, a recent study by Shah et al19 reported a complication rate of 25% after the Latarjet procedure and noted that all of their cases of recurrent instability utilized cannulated screws for fixation of the coracoid graft. Our study suggests that either screw type may be used for the Latarjet procedure without significant difference in the number of cycles or energy to failure. The Latarjet procedure relies on adequate bony healing that occurs over a period of time, and in our study in cadaveric specimens, we were only able to test the procedure at time zero. It is possible that with adequate time and protection of the repair with immobilization, both screw types may result in healing of the coracoid graft to the glenoid.
Limitations of the present study were those inherent to a cadaveric study. The mean age of specimens in our study was 57 years with dual-energy x-ray absorptiometry (DEXA) results within normal ranges; however, shoulder stabilization procedures are typically performed in younger patients than our sample. The mean bone mineral density in a non-Hispanic white male is 1.21 g/cm2.18 Strength of internal fixation over time is supplemented and replaced as osseous healing occurs, and this is impossible to replicate in a cadaveric model. In efforts to isolate the graft to glenoid fixation strength, soft tissues were removed, hence eliminating the advantage offered by the soft tissue sling stabilizers of the in vivo Latarjet procedure. Conversely, if the conjoint tendon remains attached to the coracoid graft in vivo, contraction of this muscle may cause micromotion at the graft/glenoid fixation site, which may interfere with healing. Despite attempting to simulate physiologic loading, conditions of the native shoulder cannot be fully replicated. The cadaveric model makes it impossible to test other factors thought to influence outcome, including smoking, workers’ compensation status, and compliance with postoperative immobilization. Additionally, despite an attempt to mimic worst-case scenario when the humeral head directly loads the coracoid graft, we were likely testing a nonphysiologic situation.
Strengths of the present study include its use of a uniform surgical technique. Biomechanical testing was performed immediately after fixation, and testing was designed to simulate a worst-case scenario where the coracoid graft was exclusively loaded under maximal humeral abduction and external rotation. Cadavers were matched pairs and thus controlled for bone density in hopes of eliminating bone quality as a variable. Nonetheless, there was a large variance in the cycle to failure within each group, potentially indicating that minor differences in technique, including screw trajectory and bone purchase, may affect fixation strength and ultimately cycles and energy to failure.
Conclusion
This study failed to identify a difference in the fixation strength between stainless steel cortical screws and partially threaded cannulated cancellous screws. The surgeon should choose the implant for fixation that they feel the most comfortable with while keeping in mind that proper graft preparation and positioning are likely crucial for success.
Acknowledgment
The authors thank Robert Havey and Dr Avinash Patwardhan for their help and assistance in the setup, testing, and analysis of the specimens.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A Northwestern University Department of Orthopaedic Surgery institutional department research grant of $5000 was received for this cadaveric study. M.D.S. receives royalties from Tornier and is a paid consultant for Tornier and Medacta. G.M. receives royalties from and is a paid consultant for Zimmer.
References
- 1. Bergmann G, Graichen F, Bender A, Kaab M, Rohlmann A, Westerhoff P. In vivo glenohumeral contact forces—measurements in the first patient months postoperatively. J Biomech. 2007;40:2139–2149. [DOI] [PubMed] [Google Scholar]
- 2. Bessiere C, Trojani C, Carles M, Mehta SS, Boileau P. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res. 2014;472:2345–2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bessiere C, Trojani C, Pelegri C, Carles M, Boileau P. Coracoid bone block versus arthroscopic Bankart repair: a comparative paired study with 5-year follow-up. Orthop Traumatol Surg Res. 2013;99:123–130. [DOI] [PubMed] [Google Scholar]
- 4. Colgan SA, Hecker AT, Kirker-Head CA, Hayes WC. A comparison of the Synthes 4.5-mm cannulated screw and the Synthes 4.5-mm standard cortex screw systems in equine bone. Vet Surg. 1998;27:540–546. [DOI] [PubMed] [Google Scholar]
- 5. de Beer JF, Roberts C. Glenoid bone defects—open Latarjet with congruent arc modification. Orthop Clin North Am. 2010;41:407–415. [DOI] [PubMed] [Google Scholar]
- 6. Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22:821–827. [DOI] [PubMed] [Google Scholar]
- 7. Giles JW, Degen RM, Johnson JA, Athwal GS. The Bristow and Latarjet procedures: why these techniques should not be considered synonymous. J Bone Joint Surg Am. 2014;96:1340–1348. [DOI] [PubMed] [Google Scholar]
- 8. Giles JW, Puskas G, Welsh M, Johnson JA, Athwal GS. Do the traditional and modified Latarjet techniques produce equivalent reconstruction stability and strength? Am J Sports Med. 2012;40:2801–2807. [DOI] [PubMed] [Google Scholar]
- 9. Gupta A, Delaney R, Petkin K, Lafosse L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med. 2015;8:59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. [DOI] [PubMed] [Google Scholar]
- 11. Joshi MA, Young AA, Balestro JC, Walch G. The Latarjet-Patte procedure for recurrent anterior shoulder instability in contact athletes. Orthop Clin North Am. 2015;46:105–111. [DOI] [PubMed] [Google Scholar]
- 12. Ladermann A, Denard PJ, Burkhart SS. Injury of the suprascapular nerve during Latarjet procedure: an anatomic study. Arthroscopy. 2012;28:316–321. [DOI] [PubMed] [Google Scholar]
- 13. Latarjet M. A propos du traitement des luxations re’cidivante de l’e’paule. Lyon Chir. 1954;49:994–1003. [PubMed] [Google Scholar]
- 14. Leggon R, Lindsey RW, Doherty BJ, Alexander J, Noble P. The holding strength of cannulated screws compared with solid core screws in cortical and cancellous bone. J Orthop Trauma. 1993;7:450–457. [DOI] [PubMed] [Google Scholar]
- 15. Malicky DM, Soslowsky LJ, Blasier RB, Shyr Y. Anterior glenohumeral stabilization factors: progressive effects in a biomechanical model. J Orthop Res. 1996;14:282–288. [DOI] [PubMed] [Google Scholar]
- 16. Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23:1691–1699. [DOI] [PubMed] [Google Scholar]
- 17. Montgomery WH, Wahl M, Hettrich C, Itoi E, Lippitt SB, Matsen FA. Anteroinferior bone-grafting can restore stability in osseous glenoid defects. J Bone Joint Surg Am. 2005;87:1972–1977. [DOI] [PubMed] [Google Scholar]
- 18. Sezer A, Altan L, Özdemir Ö. Multiple comparison of age groups in bone mineral density under heteroscedasticity. Biomed Res Int. 2015;2015:426847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. [DOI] [PubMed] [Google Scholar]
- 20. Shishido H, Kikuchi S. Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elbow Surg. 2001;10:372–376. [DOI] [PubMed] [Google Scholar]
- 21. Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A:878–884. [DOI] [PubMed] [Google Scholar]
- 22. Warner JJ, Gill TJ, O’Hollerhan J D, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34:205–212. [DOI] [PubMed] [Google Scholar]
- 23. Wellmann M, de Ferrari H, Smith T, et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012;132:377–386. [DOI] [PubMed] [Google Scholar]
- 24. Wellmann M, Petersen W, Zantop T, et al. Open shoulder repair of osseous glenoid defects: biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med. 2009;37:87–94. [DOI] [PubMed] [Google Scholar]
- 25. Weppe F, Magnussen RA, Lustig S, Demey G, Neyret P, Servien E. A biomechanical evaluation of bicortical metal screw fixation versus absorbable interference screw fixation after coracoid transfer for anterior shoulder instability. Arthroscopy. 2011;27:1358–1363. [DOI] [PubMed] [Google Scholar]
- 26. Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am. 2013;95:1390–1397. [DOI] [PubMed] [Google Scholar]
- 27. Yang SW, Kuo SM, Chang SJ, et al. Biomechanical comparison of axial load between cannulated locking screws and noncannulated cortical locking screws. Orthopedics. 2013;36:e1316–e1321. [DOI] [PubMed] [Google Scholar]
- 28. Young DC, Rockwood CA., Jr Complications of a failed Bristow procedure and their management. J Bone Joint Surg Am. 1991;73:969–981. [PubMed] [Google Scholar]