Abstract
With new breast conserving oncological surgical techniques, accurate identification of specimen margins is important to allow for the re-excision of margins. The accurate identification of margins is crucial is the success of the patients treatment if further margins are required. NHS Breast Screening Programme (NHSBSP) guidelines recommend the excised specimen is labelled accurately to correctly identify the margins and allow for X-ray examination.
This method has been proven to be cheap, it uses equipment and materials readily available in the operating theatre. Furthermore, if any of the methods fails as there is more than one way to identifying your margins. For example if a clip were to fall off, the type/length of suture and the orientation on the board will still allow you to identify the correct margin. If the sample was to fall off the board, the sutures and clips will still allow the pathologist to orientate the sample.
In summary this method is easy to apply, logical and uses equipment readily available within the theatre, i.e. silk sutures, and the needle protection board. It ensures all relevant radiological and surgical criteria are met for enabling orientation of the specimen when removed from the breast tissue. It is an easily taught technique that is easy to remember. A national survey showed a lack and wide variation of specimen orientation protocols. (Volleamere et al., 2013) This technique could be used as the national standard for breast specimen marking and as a national marking system for the NHS.
Keywords: Breast, Wide local excision, Re-excision of margins, Breast specimen, Breast cancer
Highlights
-
•
There is a variation in the techniques used to mark breast specimens.
-
•
There is no national standard to how specimens should be marked.
-
•
The identification of margins is essential if re-excision of margins is required.
-
•
Specimen marking should be compatible for both radiological and pathological analysis.
-
•
The technique should be easy to remember and easily taught and understood by clinicians.
A technique for marking oncological breast tissue samples in wide local excisions: a solution to the lack of national protocols and variation in techniques.
With new breast conserving oncological surgical techniques used in breast conserving surgery, accurate identification of specimen margins is important to allow for the re-excision of margins. The accurate identification of margins is crucial is the success of the patients treatment if further margins are required. NHS Breast Screening Programme (NHSBSP) guidelines recommend the excised specimen is labelled accurately to correctly identify the margins and allow for X-ray examination.
Using a foam board, clips and a silk suture we have developed a technique that fulfils this criteria and provides reassurances with the accuracy of marking margins.
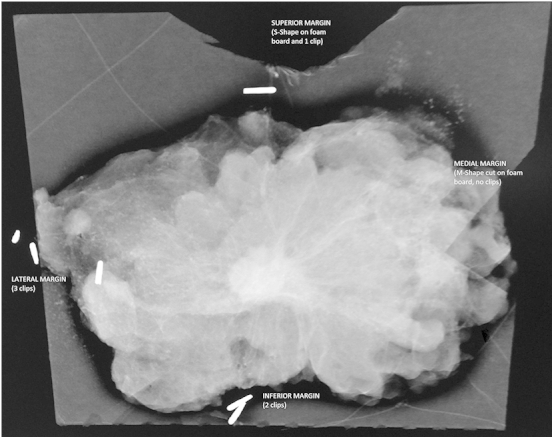
The board is pre-cut with an S shape on the Superior margin and an M-shape for the Medial margin. The specimen is then fixed with the posterior surface lying on the board, using a silk stitch. The Superior margin is secured using a Short suture, the Lateral margin with a Long suture and the inferior or Ductal margin with Double knots. Metallic clips are then placed on the silk sutures to avoid infringing on the specimen and on the pathologists blades. One clip is used on the superior edge with a short suture and it short so can only fit one clip. Two clips are used on the inferior or ductal margin, as the inferior margin has a double (two) knots and finally, three clips are used on the lateral margin, it's longest suture and can fit the most clips. The technique follows a logical sequence that can be easily taught to surgeons. The superior and lateral markings are static where as the ductal margin is variable depending on upper or lower half lesions. In inferior lesions the ductal marking would clash with the superior marking and therefore made this transferable with the inferior margin. So easy memorable markings as S cut = Short Stitch = Single knot = Single clip (x1), M cut = Medial, Long stitch = Lateral = x3 clips, Double stitch knot = Ductal/inferior = Double clips (x2).
The benefit of this technique is that the margins and orientation can be visualised using the faxtron or x-ray machine independent to the intensity of the image. The pathologist is also able to examine the specimen without any infringement on the specimen and able to accurately orientate the specimen.
This method has been proven to be cheap and uses equipment and materials readily available in the operating theatre. Furthermore, if any of the methods fails, there is more than one way to identifying your margins, providing a safe back up system. For example if a clip were to fall off, the type/length of suture and the orientation on the board will still allow you to identify the correct margin. If the sample was to fall off the board, the sutures and clips will still allow the pathologist to orientate the sample.
In summary this method is easy to apply, logical and uses equipment readily available within the theatre, i.e. silk sutures and the needle protection board. It ensures all relevant radiological and surgical criteria are met for enabling orientation of the specimen when removed from the breast. It is an easily taught technique that is easy to remember. A recent national survey showed a lack or a wide variation of specimen orientation protocols. (Volleamere et al, 2013) This technique could be used as the national standard for breast specimen marking and as a national marking system for the National Health Service.
Ethical approval
None.
Sources of funding
None.
Author contribution
Jaison Patel – paper written by Stephanie Jenkins – consultant that uses the technique described.
Conflicts of interest
None.
Guarantor
Jaison Patel.
Contributor Information
Jaison Patel, Email: jaison.patel@nhs.net.
Stephanie Jenkins, Email: Stephanie.jenkins@pah.nhs.uk.


