Case Report
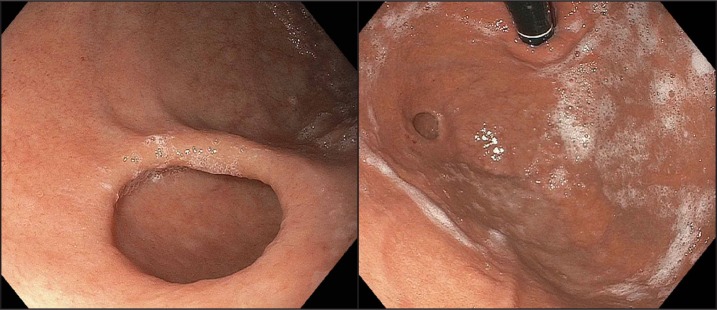
A 54-year-old white woman with a past medical history of gastroesophageal reflux disease (GERD) presented to the outpatient gastroenterology clinic with the complaint of persistent pyrosis despite proton pump inhibitor (PPI) therapy. Her symptoms were described as progressively worsening over 4 years. She also reported intermittent nausea and localized epigastric burning pain. The symptoms occurred more often in the evening and were unchanged with meals. She noted no symptomatic improvement with omeprazole 40 mg orally up to twice daily, and a switch to pantoprazole 40 mg twice daily was also ineffective. Complete laboratory studies were unremarkable. An upper endoscopy showed a 1-cm diverticulum in the gastric fundus (Figure 1), confirming a similar finding from an upper endoscopy performed 4 years prior. Biopsy specimens revealed mild esophagitis, mild chronic gastric inflammation without evidence of Helicobacter pylori, and 2 fundic gland polyps. The mucosa in the diverticulum appeared normal. An upper gastrointestinal series to characterize diverticular morphology was not performed, but would be encouraged preoperatively should she choose to pursue elective diverticular resection in the future.
Figure 1.
Endoscopic views of gastric diverticulum in the gastric fundus.
Gastric diverticula is the rarest form of gastrointestinal diverticula, with a reported prevalence of 0.01–0.11%.1 It occurs equally in men and women, most commonly in the fifth and sixth decades of life.1 Gastric diverticula are similar to colonic, duodenal, and jejunal diverticula, ranging in size from 1 to 11 cm.2-4 Gastric diverticula can be congenital (true), typically located on the posterior side of the cardia and containing all wall layers, or acquired (false), forming in association with weakened gastric wall musculature and without involvement of the muscularis propria. False gastric diverticula are less common, but most commonly occur near the greater curvature of the gastric antrum in the pars pylorica of the stomach and are usually asymptomatic. Symptomatic patients may present with a variety of clinical manifestations, including epigastric or lower chest pain, nausea, non-bilious emesis, dyspepsia, weight loss, iron deficiency anemia, bowel obstruction, bleeding, or even gastric perforation.4-6
Gastric diverticula have been reported as air- or contrast-filled suprarenal masses and have been mistakenly reported as necrotic adrenal masses on CT imaging.5 They may not be appreciated on barium contrast studies without lateral views. Juxtacardiac diverticula are best appreciated on retroflexed view during endoscopy. No treatment is needed for incidentally-discovered proximal diverticula. Symptomatic patients may be treated conservatively with H2-receptor blockers or PPIs.1,7 As distal gastric diverticula have been associated with malignancy, surgical management with amputation, segmental resection, or invagination is advised.5 Diverticulectomy is required in settings of perforation or malignancy and has been suggested in the presence of bleeding refractory to endoscopic therapy or diverticular size >4 cm.2,7 As much of our knowledge pertaining to gastric diverticula is derived from case reports, further outcome studies on excised diverticula may prove useful.2, 8-11
Disclosures
Author contributions: BT Moy and RM Marchioni Beery wrote and revised the manuscript and performed the literature search. JW Birk revised the manuscript and is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Rashid F, Aber A, Iftikhar SY. A review on gastric diverticulum. World J Emerg Surg. 2012;7(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marano L, Reda G, Porfidia R, et al. Large symptomatic gastric diverticula: Two case reports and a brief review of literature. World J Gastroenterol. 2013;19(36):6114–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen JH, Su WC, Chang CY, et al. Education and imaging: Gastrointestinal bleeding gastric diverticulum. J Gastroenterol Hepatol. 2008;23(2):336. [DOI] [PubMed] [Google Scholar]
- 4.Rodeberg DA, Zaheer S, Moir CR, Ishitani MB. Gastric diverticulum: A series of four pediatric patients. J Pediatr Gastroenterol Nutr. 2002;34(5):564–7. [DOI] [PubMed] [Google Scholar]
- 5.Jeyarajan HA, Harford WV, Jeyarajan DR. Diverticula of the pharynx, esophagus, stomach, and small intestine. In: Feldman M, Friedman LS, Brandt LJ, eds Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 9th ed Philadelphia, PA: Saunders Elsevier; 2010:375–6. [Google Scholar]
- 6.Ward WW, Oca CF, Carty CB. Massive hemoperitoneum due to gastric diverticulum. JAMA. 1966;196(9):798–9. [PubMed] [Google Scholar]
- 7.Hajini FF, Husain M, Bhat A, Bukhari SI, et al. Gastric diverticulum a rare endoscopic finding. BMJ Case Rep. 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palmer ED. Gastric diverticula. Int Abstr Surg. 1951;92(5):417–28. [PubMed] [Google Scholar]
- 9.Fine A. Laparoscopic resection of a large proximal gastric diverticulum. Gastrointest Endosc. 1998;48(1):93–5. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Lee SW, Choi WJ, et al. Laparoscopic resection of gastric diverticulum. J Laparoendosc Adv Surg Tech A. 1999;9(1):87–91. [DOI] [PubMed] [Google Scholar]
- 11.Vogt DM, Curet MJ, Zucker KA. Laparoscopic management of gastric diverticula. J Laparoendosc Adv Surg Tech A. 1999;9(5):405–10. [DOI] [PubMed] [Google Scholar]