Abstract
Polycystic disease of the pancreas is a very rare entity with very few cases reported in the literature. We report a symptomatic case of polycystic pancreas associated with pheochromocytoma that was treated surgically.
Introduction
Polycystic disease of the pancreas is a rare entity with an unknown incidence. Polycystic disease of the pancreas or dysontogenetic cysts of the pancreas can occur with other cysts, especially those of the kidneys, liver, central nervous system, and spleen. Pancreatic cysts are found in 10% of patients with polycystic kidney disease, which suggests an etiologic connection between the different cyst types.1 The tail or neck of the pancreas (62%) is the most common site for true cysts. Pancreatic cysts can be classified as retention cysts, proliferative cysts, cystic adenoma, cystic epitheliomata, hydatid cysts, congenital cysts, hemorrhagic cysts, or pseudocysts.2
Case Report
A 32-year-old woman presented with a painless epigastric lump that had progressively grown over 8 years to a size of 9 x 10 x 2 cm. She complained of early satiety, severe loss of appetite, and a 7-kg weight loss. She was recently diagnosed with diabetes mellitus and was on insulin. Transabdominal ultrasound revealed a diffuse atrophic pancreas with dilated main pancreatic duct, along with a 13.5 x 12.8-cm walled-off cystic collection near the pancreatic head, suggestive of a large pseudocyst. It also revealed a simple left thin-walled ovarian cyst (4.5 x 2.5 cm). Abdominal computed tomography (CT) with angiogram revealed a bulky pancreas with variably sized cystic lesions and multiple calcifications. A 3.5 x 2.9 x 4.7-cm partially necrotic lesion was detected in the right adrenal gland. Abdominal magnetic resonance imaging (MRI) showed innumerable cystic lesions of variable sizes diffusely involving the pancreas, almost completely replacing the parenchyma (Figure 1). The largest cystic lesion was exophytic, measuring 11 x 8.3 x 10 cm (Figure 2). The lesions resulted in compression and the displacement of the stomach and duodenum. The right adrenal mass was heterogenous and contained nodular irregular cystic/necrotic areas, highly suggestive of pheochromocytoma. There was no evidence of concomitant polycystic kidney disease. Brain CT was normal, and no family history of Von Hippel Lindau disease was reported.
Figure 1.
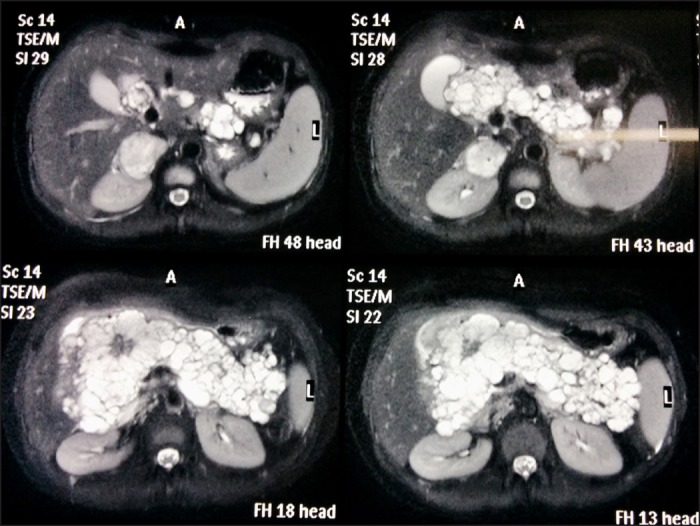
Abdominal MRI showing innumerable cystic lesions of variable sizes diffusely involving the pancreas, almost completely replacing the parenchyma.
Figure 2.
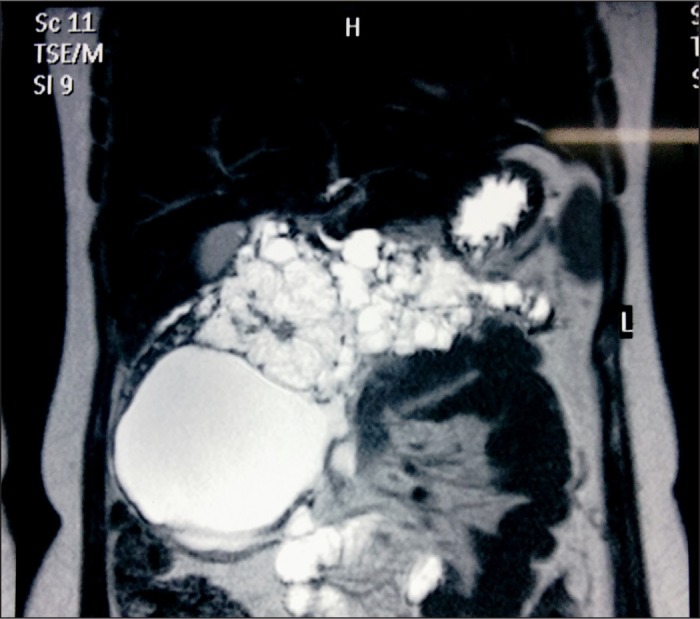
Abdominal MRI showing the largest cystic lesion (11 x 8.3 x 10 cm), which was exophytic.
Liver values, renal values, serum carcino-embryonic antigen (CEA), CA 19-9 levels, and plasma level of free metanephrines were normal. Her 24-hour urinary noradrenaline and 24-hour urinary vinyl mandellic acid values were elevated at 237.8 µg and 82 mg, respectively. Fluid resulting from transabdominal ultrasound-guided percutaneous fluid aspiration of the cysts revealed normal amylase, CEA, and CA 19-9 levels, and cytology was negative for malignancy. A gastroscopy revealed extrinsic compression over the stomach and duodenum with significant gastric residue and distorted gastric anatomy. An endoscopic retrograde cholangiopancreatography (ERCP) revealed an irregular pancreatic duct without connection to the cysts.
She underwent right adrenalectomy and deroofing of the pancreatic cysts (Figure 3). Histopathology of the pancreatic cyst wall revealed multiple cystic spaces with benign epithelial lining suggestive of polycystic disease of the pancreas (Figure 4). Histopathological examination of the 30-g right adrenal mass revealed pheochromocytoma. Her hospital recovery was uneventful and she was asymptomatic at 6-month follow-up.
Figure 3.
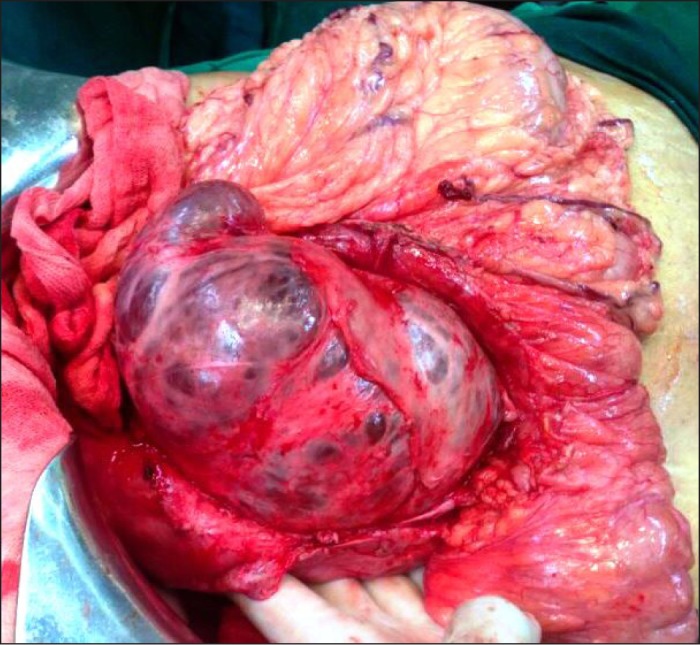
Surgical specimen of the large polycystic lesion.
Figure 4.
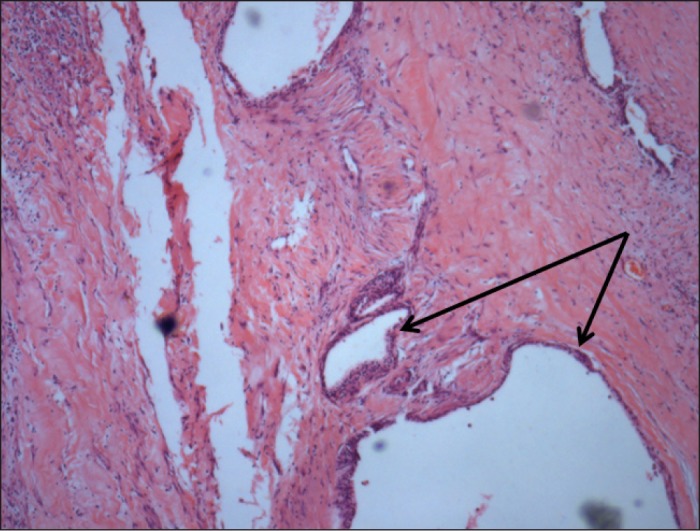
H&E stain of the pancreatic cyst wall showing multiple cystic spaces with benign epithelial lining (arrow) suggestive of polycystic disease of the pancreas (100x magnification).
Discussion
Polycystic disease of the pancreas is a very rare entity with very few cases reported in the literature. Bile and pancreatic secretions are transported to the gut lumen by widespread and complex networks of ducts in the liver and pancreas. The endoderm germ layer lining the primitive gut gives rise to the epithelial cells that form the ductal trees. Anomalous development of these duct systems (ducts with dramatically enlarged lumen and multiple cysts) can lead to polycystic disease in both liver and pancreas. True cysts develop as a result of developmental defects that cause sequestration of primitive pancreatic ducts. It was recently demonstrated that Forkhead box-containing protein, O-subfamily (FoxO1) gain of function in the pancreas can lead to diabetes, polycystic pancreas, and islet hypervascularization.3
Detailed histopathology of the cyst lining shows a lack of the primary cilia that are normally found on pancreatic ductal epithelial cells. This is comparable to the absent cilia seen in polycystic kidney disease. Molecular analysis shows that in a hepatocyte nuclear factor 6 (HNF-6)-deficient pancreas, the intra- and interlobular ducts were abnormal, causing multilayered epithelia with atypical cellular polarity, absence of primary cilia, and development of cysts.4 Ciliopathy has been thus associated with cyst formation in various organs including kidney, liver, and pancreas.
Congenital pancreatic cysts are largely asymptomatic, but can present with abdominal distension, vague abdominal pain, vomiting, jaundice, or pancreatitis.5-7 Ultrasonography is particularly valuable for cystic/solid differentiation, and a color Doppler flow can demonstrate the vascular nature of lesions.8 Cross-sectional imaging is eventually important in the characterization and localization of the cysts. MRI is preferred over CT as it can establish the relationship between a cyst and surrounding tissues, along with extensions of a cyst.
Distinguishing between congenital and acquired cysts can be difficult. Clinical history in addition to radiological, and histopathological features can facilitate this differentiation. Solitary congenital cysts are rare. Multiple congenital pancreatic cysts are usually associated with other congenital anomalies, frequently polycystic kidney disease and cysts of the liver, lung, and central nervous system. Congenital cysts can be differentiated from the more common pseudocysts by the existence of a true columnar or cuboidal epithelial lining. Pseudocysts often follow bouts of acute pancreatitis, and the cyst fluid is rich in pancreatic enzymes.
Preoperative assessment by MRI or CT can help differentiate benign from malignant pancreatic cysts. Characteristics suspicious of malignancy include peripheral calcification, thick irregular cyst wall, main pancreatic duct dilatation, mural nodules, and enlarged nodes. Benign cysts are characterized by thin walls (unless infected) and usually spare the pancreatic duct. Unfortunately, there is no way to precisely distinguish these lesions radiologically.9 Symptomatic cysts, advanced age, and rapidly increasing size of the cysts are indicators for surgical intervention.10
Disclosures
Author contributions: AD Sonavane gathered the data, wrote the manuscript, and is the article guarantor. DN Amarapurkar edited the manuscript. AD Amarapurkar provided the histopathological image.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Nygaard KK, Walters W. Polycystic disease of the pancreas (dysontogenetic cysts): Report of a case with partial pancreatectomy. Ann Surg. 1937;106(1):49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stillman A. Surgery of the pancreas at hospital from 1918 to 1928. Ann Surg. 1929;90(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kikuchi O, Kobayashi M, Amano K, et al. FoxO1 gain of function in the pancreas causes glucose intolerance, polycystic pancreas, and islet hypervascularization. PLoS One. 2012;7(2):e32249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaestner KH. Of cilia and cysts: Modeling pancreatic polycystic disease. Gastroenterology. 2006;130(3):926–8. [DOI] [PubMed] [Google Scholar]
- 5.Dhar DA, Suchi T, Garg S, Dixit VK. A rare isolated polycystic pancreatic disease. Radiation free diagnostic protocol in selected cases. India J Endocrinol Metab. 2012;16(6):1054–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rowe MI, O'Neill JA Jr, Grosfeld JL, et al. , eds Disorders of the Pancreas. Essentials of Pediatric Surgery. St. Louis, MO: Mosby Year Book; 1995:663–74. [Google Scholar]
- 7.Daher P, Diab N, Melki I, et al. Congenital cyst of the pancreas: Antenatal diagnosis. Eur J Pediatr Surg. 1996;6(3):180–2. [DOI] [PubMed] [Google Scholar]
- 8.Casadei R, Campione O, Greco VM, Marrano D. Congenital true pancreatic cysts in young adults: Case report and literature review. Pancreas. 1996;12(4):419–21. [DOI] [PubMed] [Google Scholar]
- 9.Sahani DV, Kambadakone A, Macari M, et al. Diagnosis and management of cystic pancreatic lesions. Am J Roentgenol. 2013;200(2):343–354. [DOI] [PubMed] [Google Scholar]
- 10.Spinelli KS, Fromwiller TE, Daniel RA, et al. Cystic pancreatic neoplasms: Observe or operate. Ann Surg. 2004;239(5):651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]


