Abstract
Intraductal papillary mucinous neoplasms (IPMNs) are epithelial neoplasms treated with surgical resection when appropriate. We present a 79-year-old man with jandice refractory to endoscopic stenting. Biliary radiofrequency ablation (RFA) with cholangioscopy was used as palliation of obstructive jaundice due to a mucin-producing pancreatic IPMN with fistulous biliary communication. Clinical improvement permitted surgery, and he returned to pre-illness status at 17 months. The use of cholangioscopy in the setting of mucinous filling defects can guide over-the-wire RFA for palliation and may be a bridge to surgery.
Introduction
Intraductal papillary mucinous neoplasms (IPMNs) are potentially malignant epithelial neoplasms that are composed of mucin-producing columnar epithelium that show papillary proliferation, cyst formation, and varying degrees of cellular atypia. They may be in communication with the main pancreatic duct, branch ducts, or both. The true incidence is not known; however, an 2.6% incidence of pancreatic cysts was reported from a large series, most of which were believed to be IPMNs.1 Stigmata indicating increased risk for malignancy include cyst size 3 cm or larger, obstructive jaundice with a pancreatic head lesion, a solid enhancing component, and a main pancreatic duct diameter of 10 mm or larger. Treatment is surgical resection in appropriate candidates.
Radiofrequency ablation (RFA) is a technique that has been utilized during endoscopic retrograde cholangiopancreatography (ERCP) for palliation of locally advanced biliary malignancies. RFA utilizes radiofrequency waves to heat and create tissue necrosis. This has been shown to be beneficial in a variety of tumors, including malignant biliary tumors, by reducing epithelial proliferation and tumor growth.2 Therefore, IPMNs are believed to be susceptible to thermal ablation via RFA, given that they are exocrine tumors comprised of mucin-containing neoplastic cells possibly linked to overexpression of mucin-producing genes.3 Prior series with short-term follow-up have demonstrated technically and clinically successful RFA for maintaining stent patency.4-6 Safety and efficacy of the Habib endoscopic ultrasound (EUS)-RFA catheter (EMcision, Montreal, Canada) for pancreatic cystic neoplasms and NET has also been reported.7 To our knowledge, however, endoscopic over-the-wire biliary RFA has not yet been reported as therapy for palliation of obstructive jaundice due to a mucin-producing tumor.
Case Report
A 79-year-old man was admitted to an outside hospital with 2 weeks of fatigue, abdominal discomfort, and jaundice. Physical exam revealed a frail man with jaundice and tenderness in the right upper quadrant and epigastrium. Laboratory tests showed WBC 16.8 x 109/L, platelets 461 x 109/L, INR 3.4, albumin 2.2 g/dL, total bilirubin 24.9 mg/dL, direct bilirubin 14 mg/dL, alkaline phosphatase 207 U/L, AST 59 U/L, ALT 43 U/L, and CA 19-9 51,763 unit/mL. Computed tomography (CT) revealed a pancreatic head cystic mass with biliary and pancreatic ductal dilatation. EUS-FNA revealed IPMN without dysplasia. A plastic stent was placed via ERCP, and he was referred due to persistent jaundice and failure to thrive.
At our institution, CT demonstrated a dilated pancreatic duct (16 mm), multiloculated pancreatic cystic head/uncinate mass (6 cm), biliary dilation (18 mm), and narrowing of the portosplenic confluence. Due to poor functional status and CT findings, palliative options were pursued along with additional tissue sampling to confirm suspected malignancy. Repeat EUS and ERCP revealed gaping biliary and pancreatic orifices (Figure 1). ERCP revealed mucinous filling defects in bile duct with marked dilatation (Figure 2). After forceps biopsy, 2 overlapping fully covered self-expanding metal stents (Boston Scientific, Natick, MA) were placed. Histology revealed mucinous epithelium with moderate dysplasia. The patient's bilirubin improved within 1 week but worsened to 22.6 mg/dL, and CT demonstrated stent migration to the rectum, which then passed.
Figure 1.
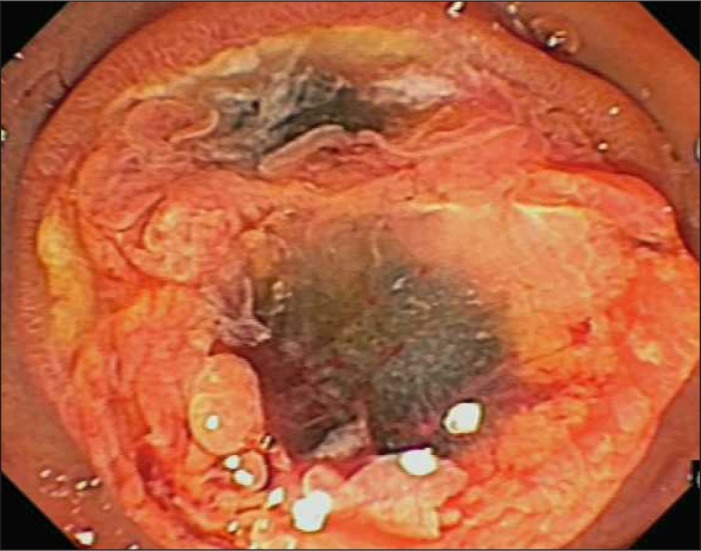
Ampullary image of gaping orifices of the biliary and pancreatic ducts.
Figure 2.
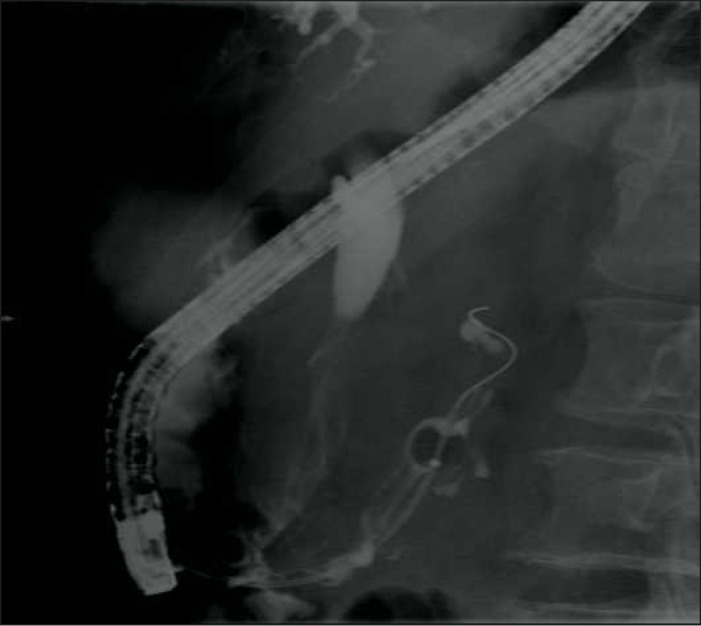
ERCP showing mucinous filling defects in both ducts.
ERCP with biliary RFA was pursued. The mucinous filling defects on ERCP obscured the upper and lower margins of the tumor. Cholangioscopy (SpyGlass DS SystemTM, Boston Scientific, Natick, MA) guidance to fluoroscopically mark the villous tumor burden revealed a fish-egg and villous-appearing mass with a pancreaticobiliary fistula (Figure 3 and Video 1). The 8.5-F Habib endocatheter (EMcision, Montreal, Canada) was advanced over a .035-inch wire (Boston Scientific, Natick, MA) to perform 3 ablations (8 W, effect 8, 90 sec/site) using the reference fluoroscopic spot films. Three side-by-side plastic stents were placed. Seven weeks later, his jaundice, anorexia, and weight had improved. ERCP revealed a subjective decline in the degree of mucinous filling defects. A second RFA session under cholangioscopy guidance included 2 stations followed by stent exchange.
Figure 3.

Fish-egg appearance of IPMN as seen by cholangioscopy within the bile duct.
Video 1.
Cholangioscopy showing a fish-egg and villous-appearing mass with a pancreaticobiliary fistula. Watch the video:
Three weeks later, his CA 19-9 had dropped to 142 U/mL, total bilirubin to 1.3 mg/dL, and albumin rose to 3.1 g/dL. Appetite, functional status, and weight improved. CT suggested an improved surgical plane between the cystic mass and major vessels, and the patient underwent a classic Whipple's resection with portal vein reconstruction. Pathology revealed IPMN with high-grade dysplasia and negative margins of the bile duct and portal vein with non-dysplastic IPMN at the neck margin (Figure 4). He remains at pre-illness functional status 17 months post-operatively.
Figure 4.
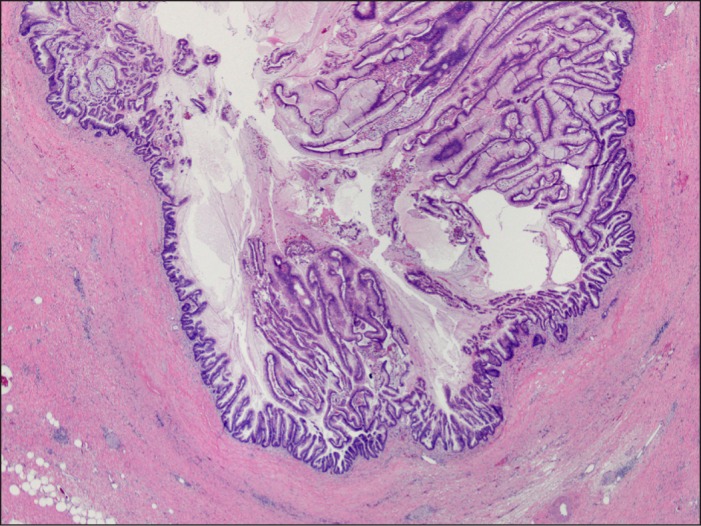
Pancreaticoduodenectomy pathology of the IPMN in the pancreatic duct with abundant luminal mucin (20x magnification).
Discussion
The incidence of IPMN is estimated at approximately 2.6%.4 Invasive biliary IPMN is a relatively rare phenomenon and often manifests as pancreaticobiliary fistulae.8,9 Self-expandable metal stents are standard therapy for the palliation of unresectable extrahepatic malignant biliary obstruction.10,11 However, our patient's IPMN and obstructive jaundice was refractory to both plastic and metal stenting due to marked mucinous burden that would not permit sustained biliary drainage.
Biliary RFA has been shown to be safe and effective in improving the caliber of malignant biliary strictures, and, as a result, stent patency in patients with unresectable biliary malignancies.5,6,12,13 To our knowledge, we describe the first case in which cholangioscopy to determine fluoroscopic tumor margins prior to RFA was successful not only as an intended palliation, but as a bridge to surgery. Prior to RFA sessions, the patient was not an operative candidate due to poor functional status from refractory obstructive jaundice and fat malabsorption.14 Following 2 biliary RFA sessions, clinical and CT improvement permitted successful pancreaticoduodenectomy. Increased recognition of this therapeutic option may enhance management of this complex, albeit rare, patient group.
Disclosures
Author contributions: NG Brown wrote the manuscript. J. Camilo and M. McCarter revised the manuscript. RJ Shah critically revised the manuscript and is the article guarantor.
Financial disclosure: Dr. Shah is on the medical advisory board a consultant for Boston Scientific, Inc.
Informed consent was obtained for this case report.
References
- 1.Laffan T, Horton KM, Klein AP, et al. . Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J of Roentgenol. 2008;191(3):802–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Figueroa-Barojas P, Bakhru MR, Habib NA, et al. . Safety and efficacy of radiofrequency ablation in the management of unresectable bile duct and pancreatic cancer: A novel palliation technique. J Oncol. 2013;2013:910897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Machado NO, Al Qadhi H, Al Wahibi K.. Intraductal papillary mucinous neoplasm of pancreas. N Am J Med Sci. 2015:7(5):160–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alis H, Sengoz C, Gonenc M, et al. . Endobiliary radiofrequency ablation for malignant obstruction. Hepatobiliary Pancreat Dis Int. 2013;12(4):423–7. [DOI] [PubMed] [Google Scholar]
- 5.Rossi S, Viera F, Ghittoni G, et al. . Radiofrequency ablation of pancreatic neuroendocrine tumors: A pilot study of feasibility, efficacy, and safety. Pancreas. 2014;43(6):938–45. [DOI] [PubMed] [Google Scholar]
- 6.Steel A, Postgate A, Khorsandi S, et al. . Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endos. 2011;73(1):149–153. [DOI] [PubMed] [Google Scholar]
- 7.Pai M, Habib N, Senturk H, et al. . Endoscopic ultrasound guided radiofrequency ablation for pancreatic cystic neoplasms and neuroendocrine tumors. World J Gastrointest Surg. 2015;7(4):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim J, Jang KT, Choi D. Biliary intraductal papillary-mucinous neoplasm manifesting only as dilatation of the hepatic lobar or segmental bile ducts: Imaging featuresin six patients. AJR Am J Roentgenol. 2008;191(3):778–82. [DOI] [PubMed] [Google Scholar]
- 9.Okada K, Furuuchi T, Tamada T, et al. . Pancreatobiliary fistula ssociated with an intraductal papillary-mucinous pancreatic neoplasm manifesting as obstructive jaundice: Report of a case. Surg Today. 2008;38(4):371–6. [DOI] [PubMed] [Google Scholar]
- 10.Glättli A, Stain S, Baer H, et al. . Unresectable malignant biliary obstruction: Treatment by self-expandable biliary endoprostheses. HPB Surg. 1993;6(3):175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaw M, Singh S, Gagneja H. Clinical outcome of simultaneous self-expandable metal stents for palliation of malignant biliary and duodenal obstruction. Surg Endosc. 2003;17(3):457–61. [DOI] [PubMed] [Google Scholar]
- 12.Hu B, Gao D, Wu J, et al. . Intraductal radiofrequency ablation for refractory benign biliary stricture: Pilot feasibility study. Dig Endosc. 2014;26(4):581–5. [DOI] [PubMed] [Google Scholar]
- 13.Tal A, Vermehren J, Friedrich-Rust M, et al. . Intraductal endoscopic radiofrequency ablation for the treatment of hilar non-resectable malignant bile duct obstruction. World J Gastrointest Endosc. 2014;6(1):13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guardino JM. Primo Gastro. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]


