Abstract
Metastasis of colon adenocarcinoma is commonly found in the lung, liver, or peritoneum. Common bile duct (CBD) tumors related to adenomas from familial adenomatous polyposis metastasizing from outside of the gastrointestinal tract have been reported. We report a case of biliary colic due to metastatic colon adenocarcinoma to the CBD. Obstructive jaundice with signs of acalculous cholecystitis on imaging in a patient with a history of colon cancer should raise suspicion for metastasis to CBD.
Introduction
Metastasis of colon adenocarcinoma are commonly found in the lung, liver, or peritoneum.1 There are case reports of common bile duct (CBD) tumors related to other processes in the gastrointestinal tract.2-4
Case Report
A 57-year-old man with a history of metastatic rectosigmoid adenocarcinoma presented for evaluation of abdominal pain. He was diagnosed with rectosigmoid cancer in 2011 and had a lower anterior resection without chemotherapy or radiation. In 2013, he had local recurrence with metastasis to the liver. At that time, he received chemotherapy of FOLFOX and bevacizumab for 4 cycles, and then he required dose reduction for 3 more cycles due to leukopenia and thrombocytopenia. He received bevacizumab alone for 3 cycles before undergoing a bone marrow biopsy, which showed no evidence of myelodysplasia. He was changed to FOLFIRI and bevacizumab for 3 cycles in preparation for radiation and surgery before being lost to follow-up. At the time of our presentation, he was having pain associated with food intake for 3 weeks, which led to 13.6 kg weight loss. He had associated jaundice but an otherwise unremarkable physical examination.
On admission, liver function tests showed AST 115 U/L, ALT 51 U/L, alkaline phosphatase 714 U/L, and total bilirubin 2.0 U/L. Right upper quadrant ultrasound showed gallbladder wall thickening with likely sludge and a 1-cm CBD. Abdominal/pelvic computed tomography (CT) showed probable pericholecystic sludge and a distended gallbladder as well as progression of liver metastasis. A pre-cholecystectomy endoscopic retrograde cholangiopancreatography (ERCP) revealed a main bile duct stricture and gallstones with sludge. A sphincterotomy was performed and stones were removed with retrievable balloon (Figure 1). Multiple pathology specimens showed moderately differentiated adenocarcinoma consistent with colonic origin, including CDX-2 and CK20 expression (Figure 2). One week later, a repeat ERCP was performed. Contrast was injected into the entire biliary tree, which showed a 4-cm CBD stricture with proximal dilation. A 10 mm x 6 cm uncovered metal stent was placed, and the previously successful chemotherapy regimen was restarted.
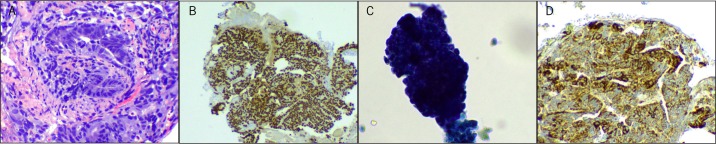
Figure 1.
(A) Ampulla of lower third CBD stricture post-sphincterotomy. (B) Stones and debris removed from the bile duct with a retrieval balloon.
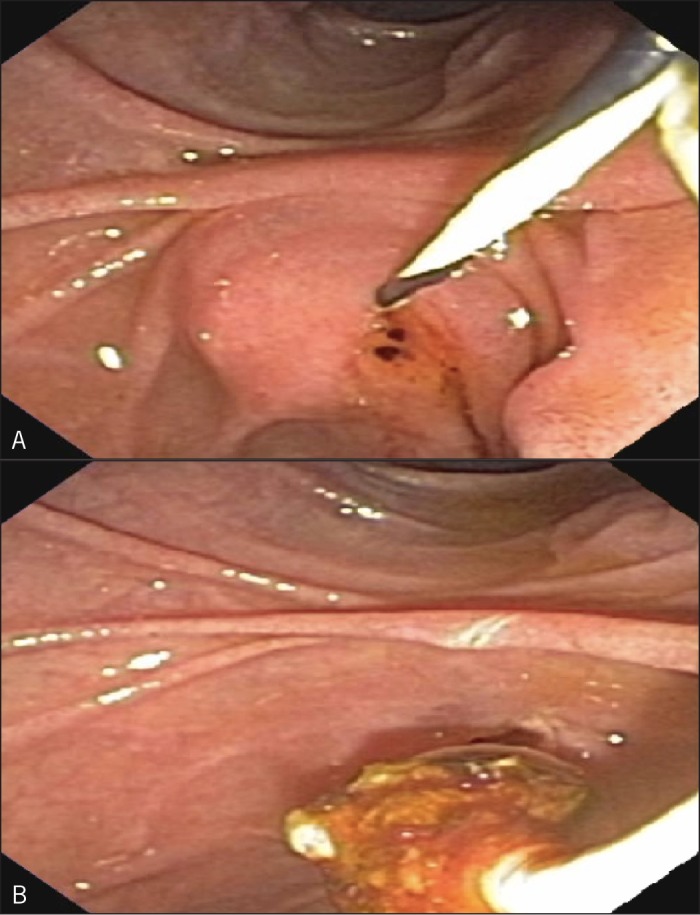
Figure 2.
All slides at 100x magnification. (A) H&E stain showing a moderately-differentiated adenocarcinoma within the submucosal stroma of the biliary duct. It lacks the typical “dirty necrosis” of rectosigmoid adenocarcinoma, and no intraepithelial dysplasia is identified in the surrounding duct epithelium. (B) Immunoperoxidase staining for CDX-2 antigen demonstrates robust nuclear staining. (C) Immunoperoxidase staining for CK20 antigen is expressed in typical cytoplasmic pattern. Together, CDX-2 and CK20 expression confirm middle to lower alimentary tract origination, favoring a colonic or rectal primary. (D) Immunoperoxidase staining for p504s (AMACR) antigen is positive, further favoring origination in the colon or rectum rather than the intestine.
Discussion
Colon cancer is the third most common cancer in the United States. The most common sites of colon metastasis are lung, liver, and peritoneum.1 Some case reports have described patients with abdominal pain due to primary adenocarcinoma of the CBD or adenomas from FAP.2-4 Some cases have been reported involving metastasis to the CBD from the lung and kidney.5,6 Usually, colon cancer metastasizes to the liver, causing intrahepatic obstruction and jaundice.7 Some patients have been identified to have extrahepatic biliary obstruction caused by adenocarcinoma metastasis to lymph nodes adjacent to biliary structures, for which percutaneous drainage has been shown to be effective.8 Self-expandable metal stents have a lower occlusion rate, less failure, and lower cholangitis occurrence when compared to plastic stents for treatment of this condition.9
To our knowledge, the literature contains only 3 reports of of colon cancer metastasis to the CBD.10-11 While uncommon, these metastases have distinct histopathologic morphology and immunohistochemically detectable antigen expression. In contrast to adenocarcinomas arising from the biliary ducts or pancreatic duct, which are often CK7 and CK17 positive (71–100%), ampullary carcinomas arising from intestinal epithelial cells (enterocytes) have variable expression of CK7 and are uncommonly positive for CK17 (18%). Further, intestinal epithelial cells express both CK20 and CDX-2 (91–100%), which are uncommonly expressed in pancreaticobiliary neoplasms (22–46%).12 It is worth noting that well-differentiated adenocarcinomas have more distinct morphology and characteristic antigen expression than poorly differentiated adenocarcinomas. Obstructive jaundice with signs of acalculous cholecystitis on imaging in a patient with a history of colon cancer should raise suspicion for metastasis to the CBD.
Disclosures
Author contributions: All authors contributed equally to the creation of this manuscript. AT Strauss is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Disibio G, French SW. Metastatic patterns of cancer: results from a large autopsy study. Arch Pathol Lab Med. 2008;132(6):931–939. [DOI] [PubMed] [Google Scholar]
- 2.Montalvo-Jave EE, Chablé-Montero F, Toapanta-Yanchapaxi LN, et al. Papillary in situ and intramucosal adenocarcinoma of the lower third of common bile duct: A report and review of the literature. Ann Hepatol. 2015;14(3):425–9. [PubMed] [Google Scholar]
- 3.Yan ML, Pan JY, Bay YN, et al. Adenomas of the common bile duct in familial adenomatous polyposis. World J Gastroenterol. 2015;21(10):3150–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vasiliadisi K, Papavasilliou, Pervana S, et al. Acute pancreatitis as the initial manifestation of an adenocarcinoma of the major duodenal papilla in a patient with familial adenomatous polyposis syndrome: A case report and literature review. Acta Chir Belg. 2013;113(6):463–7. [PubMed] [Google Scholar]
- 5.Ochi N, Goto D, Yamane H, et al. Obstructive jaundice caused by intraductal metastasis of lung sdenocarcinoma. Onco Targets Ther. 2014;7:1847–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haidong W, Jainwei W, Guizhong L. Ampullary tumor caused by metastatic renal cell carcinoma and literature review. Urol J. 2014;11(2):1504–7. [PubMed] [Google Scholar]
- 7.Levine AW, Donegan WL, Irwin M. Adenocarcinoma of the colon with hepatic metastases: Fifteen-year survival. JAMA. 1982;(247):2809–10. [PubMed] [Google Scholar]
- 8.Warshaw AL, Welch JP. Extrahepatic biliary obstruction by metastatic colon carcinoma. Ann Surg. 1978;188(55):593–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sawas T, Al Halabi S, Parsi MA, Vargo JJ. Self-expandable metal stents versus plastic stents for malignant niliary obstruction: A meta-analysis. Gastroinestinal Endosc. 2005;82(2):256–7. [DOI] [PubMed] [Google Scholar]
- 10.Morelli L, Faraci R, Piscioli I, et al. Colon carcinoma metastasis to the intrapancreatic tract of the common biliary duct: A first case report. Scand J Gastroenterol. 2007;42(6):777–8. [DOI] [PubMed] [Google Scholar]
- 11.Sung MW, Bruckner HW, Szabo S, Mitty HA. Extrahepatic obstructive jaundice due to colorectal cancer. Am J Gastroenterol. 1988;(83):267–70. [PubMed] [Google Scholar]
- 12.Chu PG, Schwarz RE, Lau SK,. Immunohistochemical staining in the diagnosis of pancreatobiliary and ampulla of Vater adenocarcinoma: Application of CDX2, CK17, MUC1, and MUC2. Am J Surg Pathol. 2005;29(3):359–67. [DOI] [PubMed] [Google Scholar]