Abstract
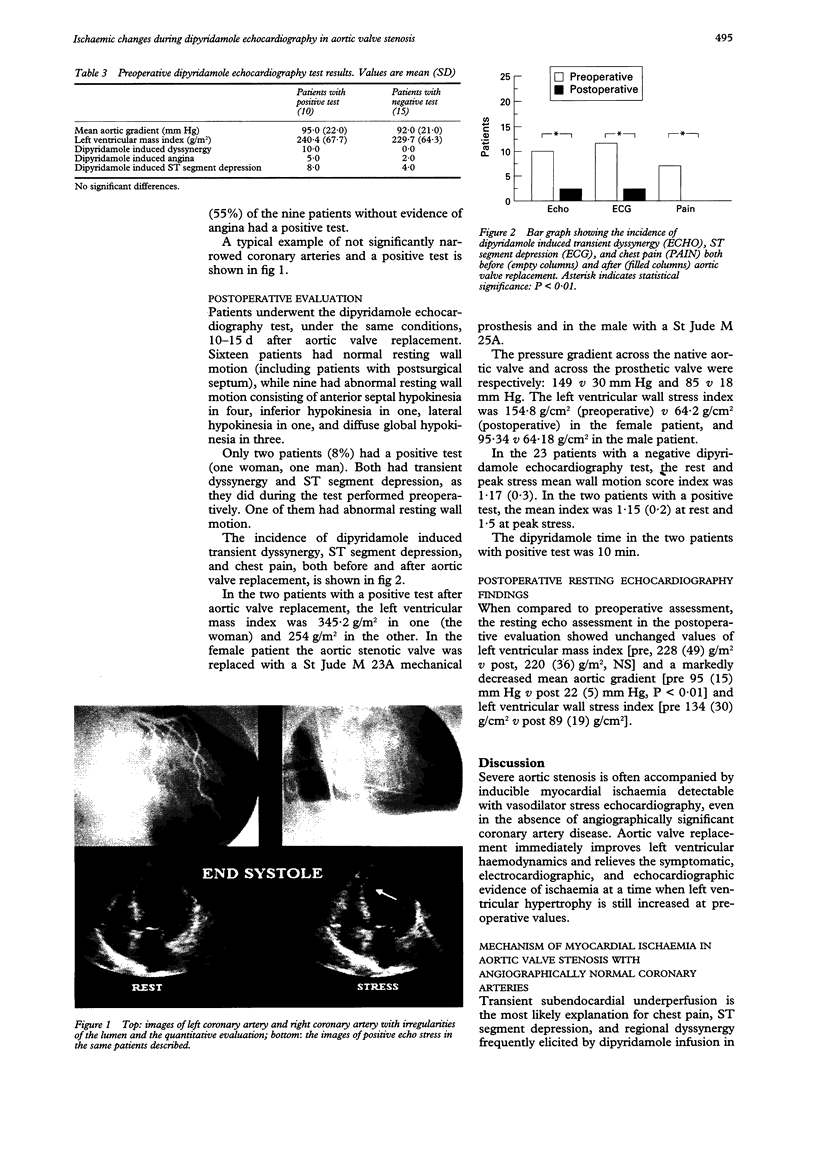
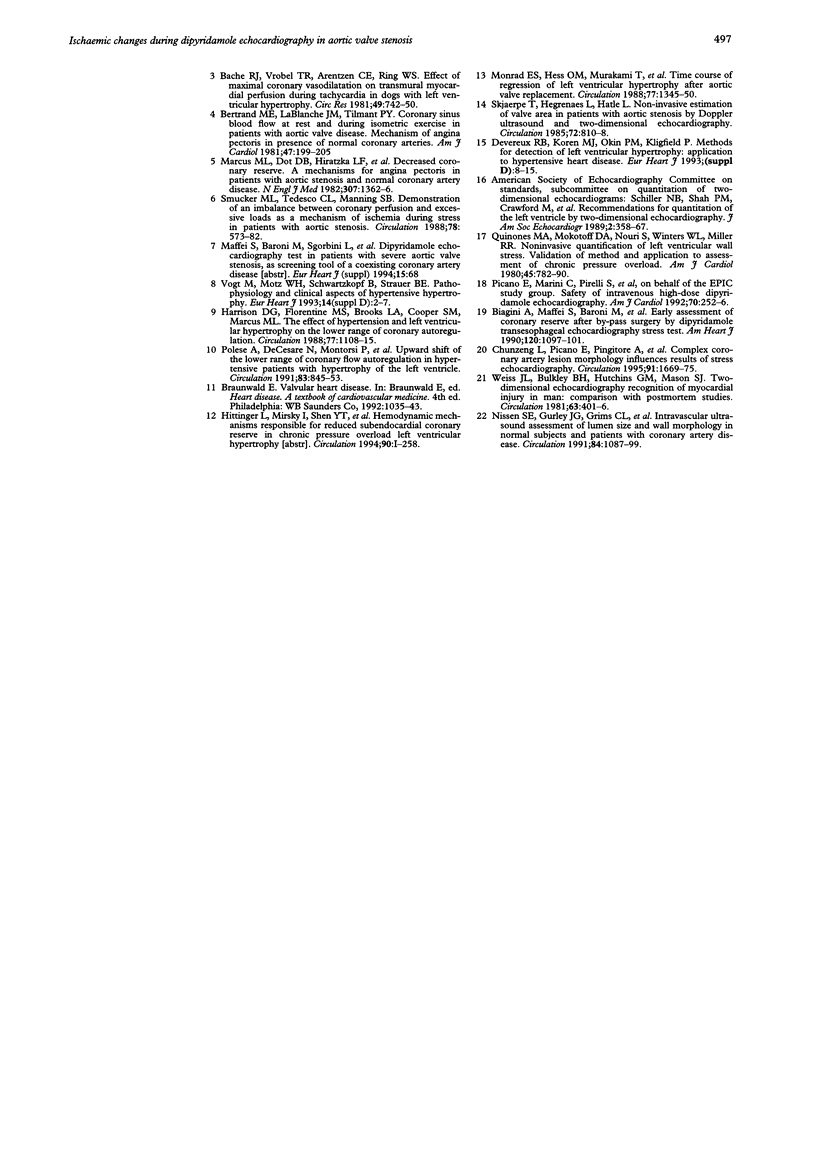
OBJECTIVE: Vasodilator stress echocardiography can cause myocardial ischaemia in patients with severe aortic valve stenosis and angiographically normal coronary arteries. The aim of the study was to determine the mechanism of ischaemia in this clinical model. METHODS: The study group comprised patients with severe aortic valve stenosis and normal coronary arteries: 25 patients (17 males, eight females; age 63 (SD 11) years) underwent a high dose (up to 0.84 mg/kg over 10 min) dipyridamole echocardiography test both before (2-4 d) and after (10-15 d) aortic valve replacement. Mean aortic pressure gradient was 96 (15) mm Hg, with a left ventricular mass index of 228 (49) g/m2. The dipyridamole echocardiography test was well tolerated and interpretable in all patients. RESULTS: Dipyridamole infusion induced chest pain in seven patients before and in no patient after surgery (28 v 0%, P < 0.01), ST segment depression in 12 patients before and two after surgery (48 v 8%, P < 0.01), and a transient regional dyssynergy in 10 patients before and two after surgery (40 v 8%, P < 0.01). In the preoperative evaluation, patients with an echocardiographically positive dipyridamole echocardiography test were comparable with patients with negative test as far as left ventricular mass index [240 (67) v 230 (64) g/m2, NS] and mean aortic pressure gradient [95 (22) v 92 (21) mm Hg, NS] were concerned. When compared to the preoperative assessment, the resting echo assessment in the postoperative evaluation showed unchanged values of left ventricular mass index [pre 228 (49) g/m2 v post 220 (36) g/m2, NS], but markedly decreased values of mean aortic gradient [pre 95 (15) mm Hg v post 22 (5) mm Hg, P < 0.01] and left ventricular wall stress index [pre 134 (30) g/cm2 v post 89 (19) g/cm2]. CONCLUSIONS: Dipyridamole echocardiography is a suitable clinical technique for assessing the ischaemic vulnerability of the left ventricle in severe aortic valve stenosis with angiographically normal coronary arteries. The frequent disappearance of the ischaemic response early after aortic valve replacement suggests that haemodynamic factors such as compressive diastolic wall stress or afterload reduction are important components of myocardial ischaemic vulnerability under these circumstances.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anand I. S., Ferrari R., Kalra G. S., Wahi P. L., Poole-Wilson P. A., Harris P. C. Edema of cardiac origin. Studies of body water and sodium, renal function, hemodynamic indexes, and plasma hormones in untreated congestive cardiac failure. Circulation. 1989 Aug;80(2):299–305. doi: 10.1161/01.cir.80.2.299. [DOI] [PubMed] [Google Scholar]
- Bache R. J., Vrobel T. R., Arentzen C. E., Ring W. S. Effect of maximal coronary vasodilation on transmural myocardial perfusion during tachycardia in dogs with left ventricular hypertrophy. Circ Res. 1981 Sep;49(3):742–750. doi: 10.1161/01.res.49.3.742. [DOI] [PubMed] [Google Scholar]
- Bertrand M. E., LaBlanche J. M., Tilmant P. Y., Thieuleux F. P., Delforge M. R., Carré A. G. Coronary sinus blood flow at rest and during isometric exercise in patients with aortic valve disease. Mechanism of angina pectoris in presence of normal coronary arteries. Am J Cardiol. 1981 Feb;47(2):199–205. doi: 10.1016/0002-9149(81)90384-2. [DOI] [PubMed] [Google Scholar]
- Biagini A., Maffei S., Baroni M., Levantino M., Comite C., Russo V., Salerno L., Borzoni G., Piacenti M., Salvatore L. Early assessment of coronary reserve after bypass surgery by dipyridamole transesophageal echocardiographic stress test. Am Heart J. 1990 Nov;120(5):1097–1101. doi: 10.1016/0002-8703(90)90122-e. [DOI] [PubMed] [Google Scholar]
- Harrison D. G., Florentine M. S., Brooks L. A., Cooper S. M., Marcus M. L. The effect of hypertension and left ventricular hypertrophy on the lower range of coronary autoregulation. Circulation. 1988 May;77(5):1108–1115. doi: 10.1161/01.cir.77.5.1108. [DOI] [PubMed] [Google Scholar]
- Lenfant C. NHLBI funding policies. Enhancing stability, predictability, and cost control. Circulation. 1994 Jul;90(1):1–1. doi: 10.1161/01.cir.90.1.1. [DOI] [PubMed] [Google Scholar]
- Lu C., Picano E., Pingitore A., Sicari R., Tongiani R., Baratto M., Palmieri C., Marzilli M., L'Abbate A. Complex coronary artery lesion morphology influences results of stress echocardiography. Circulation. 1995 Mar 15;91(6):1669–1675. doi: 10.1161/01.cir.91.6.1669. [DOI] [PubMed] [Google Scholar]
- Marcus M. L., Doty D. B., Hiratzka L. F., Wright C. B., Eastham C. L. Decreased coronary reserve: a mechanism for angina pectoris in patients with aortic stenosis and normal coronary arteries. N Engl J Med. 1982 Nov 25;307(22):1362–1366. doi: 10.1056/NEJM198211253072202. [DOI] [PubMed] [Google Scholar]
- Monrad E. S., Hess O. M., Murakami T., Nonogi H., Corin W. J., Krayenbuehl H. P. Time course of regression of left ventricular hypertrophy after aortic valve replacement. Circulation. 1988 Jun;77(6):1345–1355. doi: 10.1161/01.cir.77.6.1345. [DOI] [PubMed] [Google Scholar]
- Nakano K., Corin W. J., Spann J. F., Jr, Biederman R. W., Denslow S., Carabello B. A. Abnormal subendocardial blood flow in pressure overload hypertrophy is associated with pacing-induced subendocardial dysfunction. Circ Res. 1989 Dec;65(6):1555–1564. doi: 10.1161/01.res.65.6.1555. [DOI] [PubMed] [Google Scholar]
- Nissen S. E., Gurley J. C., Grines C. L., Booth D. C., McClure R., Berk M., Fischer C., DeMaria A. N. Intravascular ultrasound assessment of lumen size and wall morphology in normal subjects and patients with coronary artery disease. Circulation. 1991 Sep;84(3):1087–1099. doi: 10.1161/01.cir.84.3.1087. [DOI] [PubMed] [Google Scholar]
- Picano E., Marini C., Pirelli S., Maffei S., Bolognese L., Chiriatti G., Chiarella F., Orlandini A., Seveso G., Colosso M. Q. Safety of intravenous high-dose dipyridamole echocardiography. The Echo-Persantine International Cooperative Study Group. Am J Cardiol. 1992 Jul 15;70(2):252–258. doi: 10.1016/0002-9149(92)91284-b. [DOI] [PubMed] [Google Scholar]
- Polese A., De Cesare N., Montorsi P., Fabbiocchi F., Guazzi M., Loaldi A., Guazzi M. D. Upward shift of the lower range of coronary flow autoregulation in hypertensive patients with hypertrophy of the left ventricle. Circulation. 1991 Mar;83(3):845–853. doi: 10.1161/01.cir.83.3.845. [DOI] [PubMed] [Google Scholar]
- Quinones M. A., Mokotoff D. M., Nouri S., Winters W. L., Jr, Miller R. R. Noninvasive quantification of left ventricular wall stress. Validation of method and application to assessment of chronic pressure overload. Am J Cardiol. 1980 Apr;45(4):782–790. doi: 10.1016/0002-9149(80)90122-8. [DOI] [PubMed] [Google Scholar]
- Schiller N. B., Shah P. M., Crawford M., DeMaria A., Devereux R., Feigenbaum H., Gutgesell H., Reichek N., Sahn D., Schnittger I. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989 Sep-Oct;2(5):358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- Skjaerpe T., Hegrenaes L., Hatle L. Noninvasive estimation of valve area in patients with aortic stenosis by Doppler ultrasound and two-dimensional echocardiography. Circulation. 1985 Oct;72(4):810–818. doi: 10.1161/01.cir.72.4.810. [DOI] [PubMed] [Google Scholar]
- Smucker M. L., Tedesco C. L., Manning S. B., Owen R. M., Feldman M. D. Demonstration of an imbalance between coronary perfusion and excessive load as a mechanism of ischemia during stress in patients with aortic stenosis. Circulation. 1988 Sep;78(3):573–582. doi: 10.1161/01.cir.78.3.573. [DOI] [PubMed] [Google Scholar]
- Weiss J. L., Bulkley B. H., Hutchins G. M., Mason S. J. Two-dimensional echocardiographic recognition of myocardial injury in man: comparison with postmortem studies. Circulation. 1981 Feb;63(2):401–408. doi: 10.1161/01.cir.63.2.401. [DOI] [PubMed] [Google Scholar]



