Abstract
Background
Healthcare workers have an elevated prevalence of asthma and related symptoms associated with the use of cleaning/disinfecting products. The objective of this study was to identify and characterize cleaning/disinfecting tasks and products used among hospital occupations.
Methods
Workers from 14 occupations at five hospitals were monitored for 216 shifts, and work tasks and products used were recorded at five-minute intervals. The major chemical constituents of each product were identified from safety data sheets.
Results
Cleaning and disinfecting tasks were performed with a high frequency at least once per shift in many occupations. Medical equipment preparers, housekeepers, floor strippers/waxers, and endoscopy technicians spent on average 108–177 min/shift performing cleaning/disinfecting tasks. Many occupations used products containing amines and quaternary ammonium compounds for > 100 min/shift.
Conclusions
This analysis demonstrates that many occupations besides housekeeping incur exposures to cleaning/disinfecting products, albeit for different durations and using products containing different chemicals.
Keywords: healthcare workers, cleaning products, cleaning tasks, disinfecting chemicals, asthma
INTRODUCTION
Cleaning and disinfecting activities in hospitals are critical for preventing healthcare associated infections [Denton et al., 2004; Dancer, 2009; Carling and Huang, 2013]. However, performance of cleaning tasks is associated with increased risk of asthma and respiratory symptoms among healthcare workers [Delclos et al., 2007; Mirabelli et al., 2007; Arif et al., 2009; Liss et al., 2011; Arif and Delclos, 2012] and professional cleaners in non-healthcare settings [Karjalainen et al., 2002]. Relevant cleaning tasks include using spray products, waxing floors, spot-cleaning floors, stripping wax off floors, and cleaning tiles [Zock et al., 2007; Obadia et al., 2009; Le Moual et al., 2012].
Cleaning and disinfecting products are complex mixtures of chemicals which often contain respiratory sensitizers such as quaternary ammonium compounds or monoethanolamine and/or irritants such as chlorinated compounds, ammonia, or acids [Wolkoff et al., 1999; Nazaroff and Weschler, 2004; Quirce and Barranco, 2010; AOEC, 2012]. Studies have reported an association between work-related asthma (WRA) or respiratory symptoms and use of general purpose cleaning products such as ammonia and/or chlorine [Arif and Delclos, 2012]; chemicals used for cleaning and sterilizing instruments [Vizcaya et al., 2011; Arif and Delclos, 2012]; chemicals used for floor stripping and waxing [Wieslander and Norbäck, 2010]; groups/classes of chemicals such as volatile organic compounds (VOCs) [Zock et al., 2007; Wieslander and Norbäck, 2010; Vizcaya et al., 2011; Arif and Delclos, 2012]; and detergent enzymes [Adisesh et al., 2011]. Most of these studies utilized qualitative exposure metrics for cleaning products, often based on self-reports.
Simulated activities in laboratories and at work sites have provided more detailed information about exposures associated with cleaning tasks and products. Laboratory-based studies of cleaning product and air freshener use suggest that the chemical emissions vary by type of product and cleaning activity [Zhu et al., 2001; Singer et al., 2006]. Bello et al. [2009, 2010] used a controlled environment to simulate cleaning tasks and determined that these activities yielded high airborne concentrations of total VOCs and that the chemicals remained in the air after completion of cleaning tasks. A study of floor polishing in a hospital revealed high levels of glycol ether during polish application that declined rapidly after the application was completed [Wieslander and Norbäck, 2010]. Actual workplace exposure levels may differ from these simulated results because of variability in several factors, including the type, duration, and frequency of cleaning and disinfecting tasks; types and amounts of products used; and environmental conditions.
Hand dermatitis is a concern among healthcare workers because they frequently perform “wet work” (i.e., activities involving wet hands or glove use), which is shown to vary by occupation and location [Jungbauer et al., 2004a,b, 2005; Anveden et al., 2006]. In addition, research indicates that direct observation rather than self-reports are needed to obtain an accurate assessment of wet work activities performed by workers [Jungbauer et al., 2005; Anveden et al., 2006].
Exposure to chemicals in cleaning products in healthcare facilities has not been well studied because of the chemical complexity of cleaning products and the difficulty in conducting personal exposure monitoring for multiple chemicals in this work environment. As such, current knowledge of the types of tasks performed, products used, and exposures among occupations are incomplete. To address these deficiencies, we systematically observed and documented cleaning and disinfecting activities of healthcare workers while concurrently measuring personal airborne exposures; the results of the airborne exposures are presented elsewhere [LeBouf et al., 2014]. As part of a larger project, the objective of this paper is to characterize the cleaning and disinfecting tasks performed by different occupations in hospitals, including the use of cleaning products and their application methods.
MATERIALS AND METHODS
Study Description
Exposure assessment studies were conducted from 2009 to 2011 at five facilities (three government general hospitals and two university teaching hospitals) with participants from 14 occupations. Four of the facilities were located in the South East and one in the North East of the United States. Over 230,000 annual outpatient visits were reported in all facilities. The 14 occupations were selected based on: (i) higher prevalence of WRA reported in the literature for the occupations, and/or (ii) their potential for exposure to cleaning and disinfecting chemicals. Supervisors identified potential participants from these occupations, and research staff obtained verbal consent from individual workers. The exposure assessment studies were exempted from National Institute of Occupational Safety and Health (NIOSH) Internal Review Board review.
The 144 workers who participated in the study were monitored for two shifts on average (range: 1–3 shifts) within a two-week period. The total number of shifts observed was the sum of shifts over all workers. The Occupational Information Network code (O*NET code), the number of shifts monitored, and the duration of the observations are summarized for each occupation in Table I. O*NET codes are standardized occupational codes developed under the sponsorship of the U.S. Department of Labor Employment and Training Administration and have been used in the development of job exposure matrices (JEMs) [Cifuentes et al., 2010]. Our goal was to monitor three to four workers from each of the 14 occupations within each facility on at least two occasions; however, this approach was not always feasible because of a lack of workers on shift, lack of volunteers to participate, and/or limited staff members from whom to select. Work sampling was conducted by trained NIOSH research technicians who used a standardized data collection form to record observations at five-minute intervals on tasks and activities, products used, tools used, control technologies (including personal protective equipment), as well as tasks conducted and products used by other workers in the same area (bystander exposures).
TABLE I.
List of Occupations and Number of Shifts, Workers, and Hospitals Monitored and Sampling Time
| Occupation | O*NET code | # Shifts monitored |
# Workers monitored |
# Hospitals monitored |
Mean (range) sampling time (mins) |
|---|---|---|---|---|---|
| Housekeepers | 37–2012.00 | 52 | 31 | 5 | 312 (187–467) |
| Floor strippers/waxers | 37–2012.00 | 13 | 13 | 4 | 404 (351–450) |
| Registered nurses | 29–1141.00 | 44 | 34 | 4 | 427 (354–500) |
| Licensed practical nurses | 29–2061.00 | 9 | 5 | 3 | 422 (380–483) |
| Nursing assistants | 31–1014.00 | 8 | 8 | 3 | 432 (338–490) |
| Medical appliance technician | 51–9082.00 | 2 | 2 | 1 | 397 (373–422) |
| Medical equipment preparers | 31–9093.00 | 13 | 7 | 4 | 442 (366–492) |
| Endoscopy technicians | 31–9099.02 | 19 | 11 | 4 | 432 (335–484) |
| Dental assistants | 31–9091.00 | 11 | 4 | 3 | 410 (404–415) |
| Dental laboratory technicians | 51–9081.00 | 11 | 4 | 3 | 418 (380–475) |
| Respiratory therapists | 29–1126.00 | 12 | 8 | 3 | 461 (403–472) |
| Medical and clinical laboratory techs | 12 | 8 | 2 | 440 (396–490) | |
| Medical and Clinical Laboratory Technicians | 29–2099.00 | ||||
| Medical and Clinical Laboratory Technologists | 29–2011.00 | ||||
| Pharmacists/Pharmacy Technicians | 8 | 6 | 3 | 438 (374–470) | |
| Pharmacists | 29–1051.00 | ||||
| PharmacyTechnicians | 29–2052.00 | ||||
| Surgical Technologists | 29–2055.00 | 2 | 2 | 1 | 393 (361–425) |
Note: Floor strippers / waxers are sometimes grouped with housekeepers, though in our study they were considered as a separate occupation because of their distinct job tasks. Pharmacists and pharmacy technicians were combined together as were medical and clinical laboratory technicians and technologists due to the small number of participants available for monitoring in these occupations.
Identification of Chemicals From SDS
A total of 185 safety data sheets (SDS) of products used by hospital workers during monitoring were reviewed. The chemical composition of each cleaning and disinfecting product was identified and the constituent chemicals were further grouped into 27 categories based on their common physical (e.g., phases) and chemical properties (e.g., functional groups): acid, acrylate, alcohol, aldehyde, alkane, amide, amine, ammonia, aromatic, base, carboxylic acid, enzyme, ester, ether, fragrance, glycol ether, halogenated compound, metal, metal salt, metalloid, oxidizer, phenolic, quaternary ammonium compounds, salt, surfactant, terpene, and others.
Data Analyses
All data analyses were conducted in SAS 9.2 (SAS Institute Inc., Cary, NC). Cleaning and disinfecting tasks (cleaning tasks associated with the use of liquids or chemical products) were identified from a complete list of over 100 tasks performed, and were categorized based on types of activities (equipment cleaning, floor cleaning, etc.). The frequency (or probability) and duration of cleaning and disinfecting tasks, chemicals in products and tools used were summarized by each occupation and location (wards, pharmacy, operating room, etc.). Frequency was calculated by dividing the number of shifts an activity was performed during the observation period by the total number of shifts the occupation was monitored, and converted to a percentage. The duration (in minutes) of cleaning tasks performed, products used, and tools used by a worker per shift was calculated as the amount of time an activity of interest was observed per worker per shift. The durations of activities of interest were summarized by calculating the means, medians, and percentiles for each occupation.
RESULTS
Overall, cleaning and disinfecting tasks were performed at least once per shift (5 min) for 169 out of 216 total shifts, and varied by occupation (range: 0–100% of shifts). All occupations except for medical appliance technicians performed cleaning and disinfecting tasks at least once per shift. Occupations with high frequency (in % of shifts) of cleaning and disinfecting tasks included: floor strippers/waxers (100%), endoscopy technicians (100%), dental assistants (100%), housekeepers (98%), certified nursing assistants (88%), and medical equipment preparers (85%). Moderate frequency was observed for licensed practical nurses (78%), respiratory therapists (75%), and registered nurses (66%). For the remainder of the occupations, cleaning and disinfecting tasks were performed during less than 50% of their shifts.
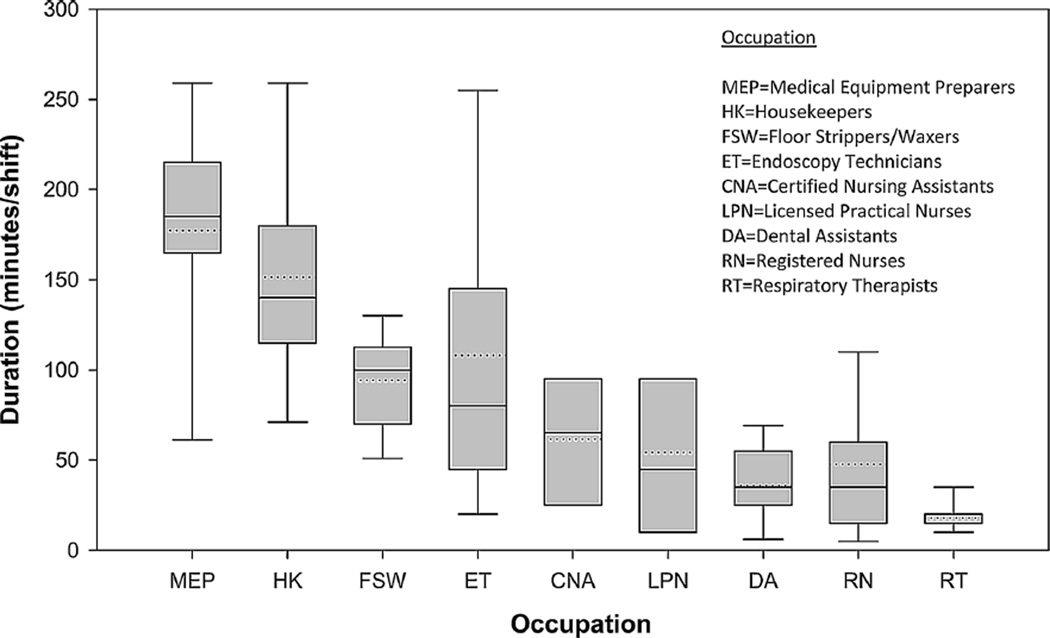
Figure 1 shows a box plot summary of time spent (duration in minutes per shift) performing cleaning and disinfecting tasks by occupation. The mean duration was the highest for medical equipment preparers (177 min/shift), followed by housekeepers (151 min/shift), endoscopy technicians (108 min/shift), and floor strippers/waxers (94 min/ shift). Notably, licensed practical nurses, certified nursing assistants, and dental assistants had moderate durations of cleaning and disinfecting tasks (mean range: 36–61 min/ shift). Other occupations such as pharmacy technicians, clinical laboratory technicians, and dental laboratory technicians spent on average less than 25 min/shift performing cleaning and disinfecting tasks.
FIGURE 1.
Duration (min/shift) in cleaning and disinfecting tasks by occupation. Center line in each box indicates median, top and bottom edges of the box represents 75-percentile and 25-percentile, error bars indicates 90-percentile and 10-percentile, and the dotted line indicates mean. Medical Appliance Technicians were not observed performing cleaning and disinfecting tasks during data collection; Surgical Technologists, Pharmacist/Pharmacy Technicians, Medical and Clinical Laboratory Techs, and Dental Laboratory Technicians were observed completing fewer than five cleaning and disinfecting tasks; therefore these occupations were not included in the figure.
Workers in several different occupations may simultaneously perform jobs in the same location or ward (e.g., dialysis unit). Analysis of the duration and frequency of cleaning and disinfecting tasks revealed variation by location: central supply (sterilization) had the longest mean duration of cleaning and disinfecting tasks (177 min/shift), followed by wards (112 min/shift), operating rooms (102 min/shift), and emergency rooms (99 min/shift). The frequency of cleaning and disinfecting tasks in these units was high (range: 82–90% of shifts). Although high frequencies (% of shifts) of cleaning and disinfecting tasks were observed in dental (100%), dialysis (100%), and critical care (79%) units, the mean durations of such tasks were short in these units (35, 61, and 56 min/shift, respectively). In pharmacy, clinical laboratory, and dental laboratory, workers spent on average less than 12.5 min/shift on cleaning and disinfecting tasks.
Table II summarizes by occupation, the frequency, and duration of five broad categories of cleaning and disinfecting tasks. Two additional types of cleaning tasks were observed, personal cleaning (e.g., hand washing) and patient care (e.g., swabbing with alcohol), but are not reported in the table because they were either very short-lived (lasting a few seconds) or were mostly observed in a few occupations (e.g., nursing assistant and respiratory therapist). Registered nurses, licensed practical nurses, medical equipment preparers and endoscopy technicians performed all categories of cleaning tasks except floor cleaning. Housekeepers and floor strippers/ waxers performed all cleaning categories except for instrument cleaning. The remaining occupations performed tasks in one or two of these categories. Most occupations performed equipment cleaning, with the highest frequency (% of shifts) being among dental assistant (91%), medical equipment preparers (77%), and endoscopy technicians (53%). The mean duration of equipment cleaning was the longest in medical equipment preparers (131 min/shift) followed by endoscopy technicians (58 min/shift). For the remainder of the occupations, the frequency of equipment cleaning was less than 50% of shifts and the mean duration was shorter than 40 min/shift. Although fixed surface cleaning was reported among many occupations, the actual frequency was generally low (7–39% of shifts) except for housekeepers (96% of shifts). Floor cleaning was performed by floor strippers/waxers (100% of shifts with a mean duration of 84 min) and housekeepers (87% of shifts with a mean duration of 61 min/shift). Instrument cleaning which involves the use of high-level disinfectants was most frequently done by endoscopy technicians and medical equipment preparers, but also by registered nurses, licensed practical nurses, and dental laboratory technicians.
TABLE II.
Frequency and Duration of Cleaning and Disinfecting Tasks by Occupation*
| Equipment cleaning |
Floor cleaning |
Instrument cleaning |
Fixed surface cleaning |
Mixing cleaning products |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Occupation | % of shifts |
Mean minutes (min-max) |
% of Shifts |
Mean minutes (min-max) |
% of shifts |
Mean minutes (min-max) |
% of Shifts |
Mean minutes (min-max) |
% of Shifts |
Mean minutes (min-max) |
| Housekeepers | 8 | 23 (5–75) | 87 | 61 (10–205) | 96 | 94 (15–305) | 42 | 8 (5–20) | ||
| Floor strippers/waxers | 15 | 8 (5–10) | 100 | 84 (25–125) | 39 | 9 (5–20) | 54 | 10 (5–20) | ||
| Registered nurses | 23 | 13 (5–20) | 2 | 25 (25) | 7 | 10 (5–15) | 5 | 10 (5–15) | ||
| Licensed practical nurses | 33 | 37 (20–50) | 22 | 90 (85–95) | 11 | 10 (10) | 11 | 20 (20) | ||
| Nursing assistants | 13 | 15 (15) | ||||||||
| Medical equipment preparers |
77 | 131 (5–260) | 69 | 54 (5–100) | 8 | 115 (115) | 23 | 13 (10–15) | ||
| Endoscopy Technicians | 53 | 58 (10–170) | 68 | 73 (5–255) | 32 | 34 (5–60) | 5 | 10 (10) | ||
| Dental assistants | 91 | 35 (5–70) | 27 | 17 (5–40) | ||||||
| Dental laboratory technicians |
18 | 8 (5–10) | ||||||||
| Respiratory therapists | 33 | 10 (5–15) | ||||||||
| Clinical laboratory technicians |
42 | 12 (5–30) | ||||||||
| Pharmacists/pharmacy technicians |
25 | 13 (10–15) | ||||||||
Note: Equipment cleaning: cleaning equipment surfaces, cleaning interior of equipment, and disinfecting machines, e.g., dialysis; Floor cleaning: mopping, preparing buffer and buffing, and waxing and stripping floors; Instrument cleaning: flushing contaminants from scopes, preparing, and operating scope cleaning machine, and wiping instrument; Fixed surface cleaning: cleaning beds, furniture, counters, walls, windows, and mirrors; Mixing products: mixing cleaning products.
Min, minimum; Max, maximum.
Medical Appliance Technicians were not observed completing cleaning and disinfecting tasks during data collection; Surgical Technologists were observed completing only two cleaning and disinfecting tasks.
Workers in the same occupation may perform different cleaning and disinfecting tasks or the same tasks for different durations at different locations, reflecting types of shifts. A summary of cleaning and disinfecting tasks for occupations that were performed in multiple locations showed that some tasks are performed in one location only (e.g., instrument cleaning), whereas other tasks can be performed in multiple locations for varying durations (e.g., floor and fixed surface cleaning) (Supplemental Table SI).
We also investigated the chemical composition of products used by laboratory and clinical support occupations and cleaning and disinfecting occupations (Supplemental Table SII) and by patient-care occupations (Supplemental Table SIII). The number of products used varied by occupation and hospital: housekeepers (range: 6–16), floor strippers and waxers (range: 1–6), patient-care occupations (range: 1–5, depending on occupation and hospital), laboratory and clinical support occupations (range: 1–2), medical equipment preparers and endoscopy technicians (range: 2–9).
Products containing alcohols were used with the highest frequency in cleaning and disinfecting occupations and patient-care occupations (67–100% of shifts), as well as among clinical laboratory technicians (58% of shifts). Housekeepers most frequently used products containing alcohol and quaternary ammonium compounds (90% of shifts) with the mean duration of 117 and 115 min/shift, respectively. The other occupations also used products that contained quaternary ammonium compounds, but the mean durations were much shorter than that of housekeepers (range: 5–70 min/shift). Housekeepers frequently used products that contained bases, salts, ethers, carboxylic acids, or amines (all >50% of shifts) for mean durations of 82– 122 min/shift. Floor strippers/waxers frequently used products containing aromatic, alcohol, ether, amine, and glycol ether, but the mean duration was short (24 min/shift for alcohol) to moderate (83 min/shift for glycol ether).
Although a wide variety of chemicals were reported for products used by endoscopy technicians and medical equipment preparers, only a few products were used with a frequency of greater than 50% of shifts: alcohol among endoscopy technicians (84% of shifts with a mean duration of 65 min/shift) and alcohol and surfactant among medical equipment preparers (frequency: 77% and 61% of shifts; mean duration: 94 and 99 min/shift, respectively). Nevertheless, these occupations used products containing several different chemicals (acids, amines, amides, bases, carboxylic acids, enzymes, etc.) for mean duration of greater than 30 min/shift.
Among all patient-care occupations, registered nurses were observed using products containing the widest variety of chemicals. Besides alcohol-containing products, registered nurses frequently used salt-containing products (40% of shifts) with a mean duration of 47 min/shift, while the longest average duration was reported for acrylate-containing products (118 min/shift among registered nurses). Licensed practical nurses used products that contained carboxylic acids for a mean duration of 99 min/shift and frequency of 50% of shifts; they used products containing salts, aldehydes, enzymes, and surfactants for more than 80 min/shift on average, but the frequency of use was low (22% of shifts). Dental assistants used products containing alcohol (100% of shifts), glycol ether (100% of shifts), and quaternary ammonium compounds (73% of shifts) albeit for a short mean duration (less than 26 min/shift for all chemicals).
Table III lists chemicals that are classified as potential sensitizers or irritants (asthmagens) by the Association of Occupational and Environmental Clinics (AOEC) and other sources [Bernstein et al., 2006; Anderson et al., 2010; AOEC, 2012] along with healthcare occupations that use products containing these chemicals. Quaternary ammonium compounds and ethanolamines were commonly present in a wide variety of cleaning products. Many potential sensitizers were present in products used in dental and clinical laboratory procedures (e.g., acrylates, metals, and formaldehyde), products used in floor stripping and finishing (e.g., ethanolamines), as well as in products used for high-level instrument disinfection (e.g., ortho-phthaldehyde—OPA).
TABLE III.
Selection of Observed Asthmagens in Products Used by Participants and the Corresponding Usage in the Healthcare Setting
| Asthmagens | Chemical group | In products used by |
|---|---|---|
| Methacrylatesa | Acrylate | Dental and clinical laboratory technicians during laboratory procedures; dental assistants when performing procedures on patients |
| Acrylatesb | Acrylate | Dental laboratory technicians during laboratory procedures |
| Quaternary ammonium compoundsc | Quats | Dental assistants and laboratory technicians, registered nurses, licensed practical nurses, certified nursing assistants, endoscopy technicians, medical equipment preparers, floor strippers /waxers, and housekeepers for general cleaning of surfaces, furniture, and equipment |
| Ethanolaminesd | Amine | Certified nursing assistants, endoscopy technicians, medical equipment preparers, for instrument cleaning; floor strippers/waxers and housekeepers for general cleaning of surface, furniture, and equipment |
| Acidse | Carboxylic acid Acid oxidizer | Registered and licensed practical nurses when working in dialysis units; registered and licensed practical nurses, dental assistants, endoscopy technicians, and medical equipment preparers for cleaning, sterilizing, and high-level disinfecting medical instruments |
| Aluminum oxide | Metal | Dental laboratory technicians during laboratory procedures |
| Ammonium hydroxide | Base | Housekeepers for general cleaning of surfaces |
| Ethylene oxide | Ether | Medical equipment prepares when sterilizing and high-level disinfecting medical instruments |
| Eugenol | Other | Dental assistants when performing procedures on patients |
| Formaldehyde | Aldehyde | Clinical laboratory technicians during laboratory procedures |
| Ortho-phthalaldehydef | Aldehyde | Licensed practical nurses and endoscopy technicians for cleaning, sterilizing, and high-level disinfecting medical instruments |
| Subtilisin | Enzyme | Licensed practical nurses, endoscopy technicians and medical equipment preparers for cleaning instruments |
| Sodium hypochzlorite | Oxidizer | Registered and licensed practical nurses, respiratory therapists, clinical laboratory technicians, and housekeepers for general surface cleaning |
| Ammonia | Ammonia | Floor strippers/waxers for stripping and finishing floors |
Note: Classification as asthmagen based on Asthma in the Workplace 3rd Edition [Bernstein et al., 2006] and the Association of Occupational and Environmental Clinics Exposure Code Lookup webpage [AOEC, 2012] unless otherwise noted. Product usage based on field observations during data collection and information from manufacturers and material safety data sheets.
Includes 2-(acetoacetoxy) ethyl methacrylate, methyl methacrylate, poly methyl methacrylate.
Includes ethyl cyanoacrylate, ethyl-2 cyanoacrylate.
Includes alkyl (60% C14, 30% C16, 5% C12, 5% C18) dimethyl benzyl ammonium chloride, alkyl (68% C12, 32% C14) dimethyl ethylbenzyl ammonium chloride, benzyl-C12-16 alkyl dimethyl ammonium chloride, didecyl dimethyl ammonium chloride, dioctyl dimethyl ammonium chloride, N-alkyl (C14 50%, C12 40%, C16 10%) dimethyl benzyl ammonium chloride, octyldecyldimethylammonium chloride, quaternary ammonium chloride.
Includes monoethanolamine, triethanolamine.
Includes acetic acid, hydrochloric acid, sulfuric acid.
Classification as a sensitizer based on evidence from other literature [Anderson et al., 2010].
Many occupations used tools such as brushes, sponges/ rags/wipes, sprays, etc., to perform cleaning tasks. The frequency and duration of the use of tools varied among occupations. Some notable examples include the use of sprays by dental assistants (frequency: 55% of shifts; mean duration: 13 min/shift) and housekeepers (frequency: 54% of shifts; mean duration: 52 min/shift), and the use of sponges/ rags/wipes by housekeepers (frequency: 96% of shifts; mean duration: 91 min/shift) and medical equipment preparers (frequency: 77% of shifts; mean duration: 146 min/shift).
Glove use while performing cleaning and disinfecting tasks varied among occupations. The frequency (% of shifts) of glove use was highest among endoscopy technicians (90%), followed by medical equipment preparers (84%), dental assistants (79%) and housekeepers (80%), and lowest among floor strippers/waxers (48%), licensed practical nurses (68%), and registered nurses (41%). Some of the cleaning and disinfecting tasks may not require glove use.
DISCUSSION
Characteristics of Cleaning Tasks Among Occupations and Locations
Our results demonstrate a wide variation in the frequency (% of shifts) and duration (minutes per shift) of cleaning and disinfecting tasks among 14 hospital occupations. As expected, cleaning and disinfecting occupations were observed to have a higher frequency and longer duration of these tasks. Other occupations that require performing multiple tasks as part of their jobs (e.g., nurses) also performed cleaning and disinfecting tasks albeit with lower frequency and for shorter durations. Other investigators have reported a higher frequency of exposure to cleaning and disinfecting agents during patient care (64%), instrument cleaning (42%) and building surface cleaning (78%) among patient-care professions (nurses, occupational therapists, physicians, and respiratory therapists) based on responses to a questionnaire survey [Delclos et al., 2009]. Note that our results are not directly comparable to results based on questionnaire surveys, as the latter yield the proportion of participants responding yes to questions on using cleaning products in the past 12 months; our results are based on workers having performed a task or used a product on a shift during our observations (most workers were observed for 1–2 shifts), which is likely to yield lower frequencies. Based on expert assessment, Dumas et al. [2012] reported that 81% of female hospital workers performed cleaning/disinfecting tasks; their study constituted 76.5% of personal care workers (nurses, physicians, and others) and 23.6% of helpers and cleaners. In our study, the occupational distribution included: cleaners and helpers (30%), personal care workers (39%), and laboratory workers and technicians (31%). Nevertheless, the findings from the two studies are similar in the high frequency of cleaning and disinfecting tasks.
Variation in tasks within the same occupation may be explained by each worker’s assigned unit or location. For example, registered nurses in the operating room or in the dialysis unit often perform equipment and instrument cleaning tasks while registered nurses in the emergency room primarily perform cleaning tasks on patients. Jungbauer et al. [2005] reported substantial differences in average duration of “wet work” tasks among hospital wards, with the longest duration in the intensive care unit (24% of the morning shift), followed by dialysis unit (16%) and regular wards (9%). We observed the longest mean duration of cleaning and disinfecting tasks in regular wards, followed by dialysis and critical care units. However, our study included a high number of housekeepers in regular wards while Jungbauer et al. [2005] only included nurses. Moreover, Jungbauer et al. [2005] defined wet work to include any glove-used activities, which makes comparison to our study difficult as we defined cleaning and disinfecting tasks as those conducted in conjunction with the use of cleaning and disinfecting products.
The frequency and duration of tasks or products used that were reported in our study provide useful insights into the differences in the potential for exposure to cleaning and disinfecting agents between and within healthcare occupations. However, the actual values may not be generalized to other samples of the same occupations due to differences among hospitals or departments/units in job duties, training, safety culture, individual knowledge, and other factors.
Inhalation and Dermal Routes of Exposure
The lists of chemicals presented in Table III and Table in the supplementary tables demonstrate that many cleaning products contain chemicals with a range of volatility. Inhalation risk may be the biggest concern for highly and moderately volatile chemicals (such as ammonia, alcohols, and glycol ethers). Product application methods (e.g., spraying) will affect the emission levels of all chemical constituents of a product. According to a study conducted by Singer et al. [2006], the use of spray and wipe to apply cleaning chemicals results in a higher rate of VOC emission into the air than the use of scrub and rinse or mops. The study also reported that the use of spray applicators results in longer suspension of chemicals in the air than other forms of application. An epidemiological study of domestic cleaners reported increased risk of asthma associated with the use of sprays for cleaning [Zock et al., 2007]. In the present study, we observed a high frequency of use of sprays to apply cleaning products among multiple occupations (housekeepers, floor strippers/waxers, dental assistants, surgical technologists, pharmacists/pharmacy technicians, endoscopy technicians, and clinical laboratory technicians) suggesting a higher risk of exposure; such activities can be targeted for change in application methods, including training workers on best practices to minimize exposures.
Healthcare workers may be exposed to cleaning chemicals through direct skin contact. Use of alcohol-based hand sanitizers is common practice among many occupations in hospitals (though difficult to capture during observations as the activity usually lasts < 30 sec). Their use raises the question of whether frequent contact with alcohol results in deterioration of the skin barrier (dryness, cracking, etc.). Results from a study of nurses and housekeepers suggest that, at least in one hospital, limited use of alcohol-based hand sanitizers did not dry skin [Ahmed-Lecheheb et al., 2012]. During observations, we noticed most workers in cleaning and disinfecting occupations wore gloves during their cleaning tasks, while a lower proportion of workers in the non-cleaning and disinfecting occupations wore gloves during their cleaning tasks. Glove use itself may lead to occlusion of skin and possibly dermatitis if moisture builds up in the glove or allergic reactions to glove materials such as latex and other natural proteins occur [Abraham et al., 2005; Jungbauer et al., 2005].
Cleaning Products Use and Potential Exposures
Many cleaning and disinfecting products contain alcohol as a solvent, and as a result, many hospital workers are exposed to alcohols when they use cleaning products. Our finding is consistent with Dumas et al. [2012] who reported 84% of hospital workers were exposed to alcohol. Although alcohol is not associated with respiratory health outcomes, it may be a suitable surrogate of exposure to cleaning and disinfecting chemicals.
Quaternary ammonium compounds are one of the most common active ingredients in general cleaners. Although the frequency and duration of use varied by occupation, quaternary ammonium compounds are widely used by hospital occupations during various cleaning tasks. Dumas et al. [2012] reported that 71% of female hospital workers used quaternary ammonium compounds, supporting the finding of high frequency of use of quaternary ammonium compounds among hospital workers. These compounds were introduced as a replacement for phenols because of their lower volatility. However, quaternary ammonium compounds are identified as asthmagens by the AOEC [AOEC, 2012] thus raising questions about their role as a preferred substitution choice. Recent epidemiological studies indicate increased risk of WRA among hospital workers, especially among nurses exposed to quaternary ammonium compounds [Gonzalez et al., 2014]. Although etiology remains unclear, clinical cases of asthma associated with exposure to quaternary ammonium compounds continue to be reported [Purohit et al., 2000; Health, 2012,]. Quaternary ammonium compounds, in general, have low volatility and thus may not be easily aerosolized and detected by air sampling for vapors. However, use of quaternary ammonium compounds-containing products in spray form may lead to high inhalation exposures. In addition, quaternary ammonium compounds can be absorbed onto particles, which may be resuspended in the air and may result in inhalation exposures. For such cases, non-detection by conventional air sampling does not necessary mean absence of an inhalation risk. Furthermore, low volatile quaternary ammonium compounds may persist for a long time on surfaces, potentially leading to dermal exposure. A reliable analytical method for quaternary ammonium compounds is needed for an accurate dermal/ inhalation exposure assessment.
Hospital workers come into daily contact with cleaning and disinfecting products, and the cleaning manufacturers have started labeling their products as “green,” non-toxic, or natural; however, criteria for their claims vary widely by manufacturers, and are often questionable as green product claims are not tightly regulated in the United States [Dahl, 2010]. There are over 300 green label or eco-label certifications of cleaning materials in the world, but not all labels are reliable. One of the most recognized labels for cleaning products is Green Seal [Dahl, 2010]. To be certified by Green Seal, products must meet toxicity criteria set by the organization and must not contain carcinogens, mutagens, reproductive toxic agents, sensitizers, corrosive agents, nor be listed as asthmagens by the AOEC [GreenSeal, 2013]. The Environmental Protection Agency also has a program for labeling products called “design for the environment” (DfE) [EPA, 2012]. One of the hospitals surveyed in our study adopted the use of “green” cleaning products by replacing some cleaning products with less toxic products over time. Although encouraging, the actual reduction in health risk from the use of green cleaning products is not known. Furthermore, due to the difficulties of identifying “green” products (as the labels were not included in product SDSs), the actual use of “green” products was not assessed in this study.
Product SDSs may not be completely reliable for identifying potential exposures to asthmagens as chemicals listed in SDSs are not always identified as asthmagens. For example, quaternary ammonium compounds, monoethanolamine, and 2-butoxyethanol are listed in SDSs without indication of asthmagen or sensitizer status, although all of them are classified as asthmagens by AOEC [AOEC, 2012]. Presently, companies can omit listing potential sensitizing agents in SDSs because they are not classified as toxic substances [Bernstein, 2002]. Quirce and Barranco [2010] reported that fragrances may contain sensitizing agents but chemical components of fragrances are often indicated as proprietary. Similarly, chemical components of surfactants are also commonly not listed. One of the limitations of our study is that we identified chemicals in products as present or absent, and were not able to get the actual percent of the constituent. Although multiple products contain the same chemicals, the amounts of the chemicals may be different. Therefore, actual chemical exposures may vary by choice of products as well as amount used and the manner in which it is used.
Implications for Epidemiologic Studies
Epidemiological studies have reported increased risk of WRA and respiratory symptoms among hospital workers who perform cleaning tasks [Delclos et al., 2007; Mirabelli et al., 2007; Arif et al., 2009] or use cleaning products such as general cleaners, disinfectants, and sterilizers [Donnay et al., 2011; Arif and Delclos, 2012; Dumas et al., 2012]. Cleaning and disinfecting tasks are very common among hospital workers, and involve the use of products containing asthmagens. Information on the frequency and duration of tasks performed and products and tools used provide valuable information on the probability or likelihood of exposure for a Job/Task Exposure Matrix (J/TEM) and can also be used to develop occupational exposure modules for questionnaires used in epidemiologic studies. For example, JEMs generally do not account for within-job differences stemming from work practices or workplace conditions (as everyone in the cell is assigned the same exposure); however, relevant worker-specific information (e.g., tasks performed, products used or control measures) collected using a detailed occupational questionnaire can be incorporated into JEMs [Kromhout and Vermeulen, 2001; Semple et al., 2004]. Thus, the exposure measures within the cells of a J/TEM can be refined to reflect worker-specific exposure circumstances.
The task and product use information reported in this study provides needed understanding of the variability of cleaning and disinfecting tasks and product use among various hospital workers and occupations. This information on the frequency and duration of tasks, products use, and tools use for the different occupations was used to develop occupational modules that were incorporated into questionnaires for ongoing epidemiological studies of asthma among healthcare workers. These modules elicit worker specific information on cleaning and disinfecting tasks performed and the type and amount of cleaning and disinfecting products the worker used during each cleaning task.
CONCLUSIONS
Our observations revealed that in addition to cleaning and disinfecting occupations, most of the 14 occupations that we monitored also performed tasks that use cleaning and disinfecting products, albeit with different frequencies and durations, and containing different chemical constituents. Most products used by these 14 occupations contained potential irritants or sensitizers. Many workers used a wide variety of cleaning tools with sponges/rags/wipes and sprays being the most common. Cleaning and disinfecting occupations such as housekeepers, floor strippers/waxers, medical equipment preparers, and endoscopy technicians spent the longest duration on cleaning and disinfecting tasks though patient-care occupations and laboratory and clinical support occupations also performed cleaning and disinfecting tasks. Our observational study provides important information on the frequency and duration of cleaning and disinfecting tasks and products used by various occupations, which may provide useful insights when developing questionnaires for epidemiologic studies of the health effects of cleaning and disinfecting products. These results suggest that information on both the frequency and duration is required to get a complete understanding of the activity and the potential for exposure.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Gretchen White and Dr. Brent Donney for their comments and suggestions; Matt Duling, Brent Lawrence, Randy Boylstein, Mike Beaty, Thomas Jefferson, Sook Ja Cho, Ji Young Park, Betsy Shogren, and Chris Piacitelli for field sampling efforts; Brian Tift for database development and management; hospital safety staff and department supervisors in each hospital for coordinating the data collection; and all workers for participating in the study. The authors would also like to acknowledge the VHA Staff who coordinated access to the VA Medical Centers and assisted the authors in the collection of the samples used in this study: Douglas Dulaney MSEH, MHA, Director, Office of Occupational Safety, Health, and GEMS Programs Veterans Health Administration, Washington, DC; Craig Brown CIH, CSP, Industrial Hygienist, Office of Occupational Safety, Health, and GEMS Programs Veterans Health Administration, Washington, DC; Margaret Engwer, Safety Manager, VA Medical Center, Pittsburgh, PA; Steven Baker, Industrial Hygienist, VA Medical Center, Pittsburgh, PA; and Jessica Proctor, Industrial Hygienist, VA Medical Center, Clarksburg, WV.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of any commercial products or trade names does not constitute endorsement by the Centers for Disease Control and Prevention/ National Institute for Occupational Safety and Health.
Footnotes
Additional supporting information may be found in the online version of this article at the publisher’s web-site.
Disclosure Statement: The authors report no conflicts of interests.
REFERENCES
- Abraham EK, Ramesh P, Joseph R, Mohanan P, Remakumari V. Release of dithiocarbamates into sweat from natural rubber latex surgical gloves. Rubber Chem Technol. 2005;78:674–681. [Google Scholar]
- Adisesh A, Murphy E, Barber CM, Ayres JG. Occupational asthma and rhinitis due to detergent enzymes in healthcare. Occup Med. 2011;61:364–369. doi: 10.1093/occmed/kqr107. [DOI] [PubMed] [Google Scholar]
- Ahmed-Lecheheb D, Cunat L, Hartemann P, Hautemaniere A. Prospective observational study to assess hand skin condition after application of alcohol-based hand rub solutions. Am J Infect Control. 2012;40:160–164. doi: 10.1016/j.ajic.2011.04.323. [DOI] [PubMed] [Google Scholar]
- Anderson SE, Umbright C, Sellamuthu R, Fluharty K, Kashon M, Franko J, Jackson LG, Johnson VJ, Joseph P. Irritancy and allergic responses induced by topical application of ortho-phthalaldehyde. Toxicol Sci. 2010;115:435–443. doi: 10.1093/toxsci/kfq054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anveden I, Lidén C, Alderling M, Meding B. Self-reported skin exposure—Validation of questions by observation. Contact Dermatitis. 2006;55:186–191. doi: 10.1111/j.1600-0536.2006.00907.x. [DOI] [PubMed] [Google Scholar]
- Arif AA, Delclos GL. Association between cleaning-related chemicals and work-related asthma and asthma symptoms among healthcare professionals. Occup Environ Med. 2012;69:35–40. doi: 10.1136/oem.2011.064865. [DOI] [PubMed] [Google Scholar]
- Arif AA, Delclos GL, Serra C. Occupational exposures and asthma among nursing professionals. Occup Environ Med. 2009;66:274–278. doi: 10.1136/oem.2008.042382. [DOI] [PubMed] [Google Scholar]
- Association of Occupational and Environmental Clinics (AOEC) Exposure code lookup. 2012 http://www.aoecdata.org/ExpCodeLookup.aspx.
- Bello A, Quinn MM, Perry MJ, Milton DK. Characterization of occupational exposures to cleaning products used for common cleaning tasks—A pilot study of hospital cleaners. Environ Health. 2009;8:11. doi: 10.1186/1476-069X-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bello A, Quinn MM, Perry MJ, Milton DK. Quantitative assessment of airborne exposures generated during common cleaning tasks: A pilot study. Environ Health. 2010;9:76. doi: 10.1186/1476-069X-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein JA. Material safety data sheets: Are they reliable in identifying human hazards? J Allergy Clin Immunol. 2002;110:35–38. doi: 10.1067/mai.2002.124891. [DOI] [PubMed] [Google Scholar]
- Bernstein DI, Chan-Yeung M, Malo J-L, Bernstein IL. Asthma in the workplace. Third. New York, NY: Taylor & Francis Group; 2006. [Google Scholar]
- Carling PC, Huang SS. Improving healthcare environmental cleaning and disinfection: Current and evolving issues. Infect Control Hosp Epidemiol. 2013;34:507–513. doi: 10.1086/670222. [DOI] [PubMed] [Google Scholar]
- Cifuentes M, Boyer J, Lombardi DA, Punnett L. Use of O*NET as a job exposure matrix: A literature review. Am J Ind Med. 2010;53:898–914. doi: 10.1002/ajim.20846. [DOI] [PubMed] [Google Scholar]
- Dahl R. Green washing: Do you know what you’re buying? Environ Health Perspect. 2010;118:A246–A252. doi: 10.1289/ehp.118-a246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dancer SJ. The role of environmental cleaning in the control of hospital-acquired infection. J Hosp Infect. 2009;73:378–385. doi: 10.1016/j.jhin.2009.03.030. [DOI] [PubMed] [Google Scholar]
- Delclos GL, Gimeno D, Arif AA, Benavides FG, Zock J-P. Occupational exposures and asthma in health-care workers: Comparison of self-reports with a workplace-specific job exposure matrix. Am J Epidemiol. 2009;169:581–587. doi: 10.1093/aje/kwn387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delclos GL, Gimeno D, Arif AA, Burau KD, Carson A, Lusk C, Stock T, Symanski E, Whitehead LW, Zock J-P. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007;175:667–675. doi: 10.1164/rccm.200609-1331OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton M, Wilcox MH, Parnell P, Green D, Keer V, Hawkey PM, Evans I, Murphy P. Role of environmental cleaning in controlling an outbreak of Acinetobacter baumannii on a neurosurgical intensive care unit. J Hosp Infect. 2004;56:106–110. doi: 10.1016/j.jhin.2003.10.017. [DOI] [PubMed] [Google Scholar]
- Donnay C, Denis M-A, Magis R, Fevotte J, Massin N, Dumas O, Pin I, Choudat D, Kauffmann F, Le Moual N. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Environ Med. 2011;68:611–617. doi: 10.1136/oem.2010.061671. [DOI] [PubMed] [Google Scholar]
- Dumas O, Donnay C, Heederik DJ, Hery M, Choudat D, Kauffmann F, Le Moual N. Occupational exposure to cleaning products and asthma in hospital workers. Occup Environ Med. 2012;69:883–889. doi: 10.1136/oemed-2012-100826. [DOI] [PubMed] [Google Scholar]
- EPA. EPA’s DfE standard for safer products (DfE standard) 2012 http://www.epa.gov/dfe/pubs/projects/gfcp/standard-for-safer-products.pdf.
- Gonzalez M, Jégu J, Kopferschmitt MC, Donnay C, Hedelin G, Matzinger F, Velten M, Guilloux L, Cantineau A, Blay F. Asthma among workers in healthcare settings: Role of disinfection with quaternary ammonium compounds. Clin Exp Allergy. 2014;44:393–406. doi: 10.1111/cea.12215. [DOI] [PubMed] [Google Scholar]
- GreenSeal. GS-37 Cleaning products for industrial and institutional use. 2013 http://www.greenseal.org/GreenBusiness/Standards.aspx?vid=ViewStandardDetail&cid=2&sid=23.
- Health TNIfOSa. Work-related lung disease surveillance system (eWoRLD) 2012 http://www2.cdc.gov/drds/WorldReportData/SectionDetails.asp?ArchiveID=1&SectionTitleID=9.
- Jungbauer FH, Lensen GJ, Groothoff JW, Coenraads PJ. Exposure of the hands to wet work in nurses. Contact Dermatitis. 2004a;50:225–229. doi: 10.1111/j.0105-1873.2004.0314.x. [DOI] [PubMed] [Google Scholar]
- Jungbauer FH, Steenstra FB, Groothoff JW, Coenraads PJ. Characteristics of wet work in nurses. Int Arch Occup Environ Health. 2005;78:248–251. doi: 10.1007/s00420-004-0561-y. [DOI] [PubMed] [Google Scholar]
- Jungbauer FH, Van Der Harst JJ, Schuttelaar ML, Groothoff JW, Coenraads PJ. Characteristics of wet work in the cleaning industry. Contact Dermatitis. 2004b;51:131–134. doi: 10.1111/j.0105-1873.2004.00421.x. [DOI] [PubMed] [Google Scholar]
- Karjalainen A, Martikainen R, Karjalainen J, Klaukka T, Kurppa K. Excess incidence of asthma among Finnish cleaners employed in different industries. Eur Respir J. 2002;19:90–95. doi: 10.1183/09031936.02.00201002. [DOI] [PubMed] [Google Scholar]
- Kromhout H, Symanski E, Rappaport SM. A comprehensive evaluation of within—and between—Worker components of occupational exposure to chemical agents. Ann Occup Hyg. 1993;37:253–270. doi: 10.1093/annhyg/37.3.253. [DOI] [PubMed] [Google Scholar]
- Kromhout H, Vermeulen R. Application of job-exposure matrices in studies of the general population-some clues to their performance. Eur Respir Rev. 2001;11:80–90. [Google Scholar]
- LeBouf R, Virji MA, Saito R, Henneberger P, Simcox N, Stefaniak A. Exposures to volatile organic compounds in healthcare settings. Occup Environ Med. 2014;71:642–650. doi: 10.1136/oemed-2014-102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Moual N, Varraso R, Siroux V, Dumas O, Nadif R, Pin I, Zock J-P, Kauffmann F. Domestic use of cleaning sprays and asthma activity in females. Eur Respir J. 2012;40:1381–1389. doi: 10.1183/09031936.00197611. [DOI] [PubMed] [Google Scholar]
- Liss GM, Buyantseva L, Luce CE, Ribeiro M, Manno M, Tarlo SM. Work-related asthma in health care in Ontario. Am J Ind Med. 2011;54:278–284. doi: 10.1002/ajim.20935. [DOI] [PubMed] [Google Scholar]
- Mirabelli MC, Zock JP, Plana E, Anto JM, Benke G, Blanc PD, Dahlman-Hoglund A, Jarvis DL, Kromhout H, Lillienberg L, et al. Occupational risk factors for asthma among nurses and related healthcare professionals in an international study. Occup Environ Med. 2007;64:474–479. doi: 10.1136/oem.2006.031203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazaroff WW, Weschler CJ. Cleaning products and air fresheners: Exposure to primary and secondary air pollutants. Atm Environ. 2004;38:2841–2865. [Google Scholar]
- Obadia M, Liss GM, Lou W, Purdham J, Tarlo SM. Relationships between asthma and work exposures among non-domestic cleaners in Ontario. Am J Ind Med. 2009;52:716–723. doi: 10.1002/ajim.20730. [DOI] [PubMed] [Google Scholar]
- Purohit A, Kopferschmitt-Kubler MC, Moreau C, Popin E, Blaumeiser M, Pauli G. Quaternary ammonium compounds and occupational asthma. Int Arch Occup Environ Health. 2000;73:423–427. doi: 10.1007/s004200000162. [DOI] [PubMed] [Google Scholar]
- Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol. 2010;20:542–550. [PubMed] [Google Scholar]
- Semple SE, Dick F, Cherrie JW. Exposure assessment for a population-based case-control study combining a job-exposure matrix with interview data. Scand J Work Environ Health. 2004;30:241–248. doi: 10.5271/sjweh.785. [DOI] [PubMed] [Google Scholar]
- Singer BC, Destaillats H, Hodgson AT, Nazaroff WW. Cleaning products and air fresheners: Emissions and resulting concentrations of glycol ethers and terpenoids. Indoor Air. 2006;16:179–191. doi: 10.1111/j.1600-0668.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- Vizcaya D, Mirabelli MC, Anto JM, Orriols R, Burgos F, Arjona L, Zock JP. A workforce-based study of occupational exposures and asthma symptoms in cleaning workers. Occup Environ Med. 2011;68:914–919. doi: 10.1136/oem.2010.063271. [DOI] [PubMed] [Google Scholar]
- Wieslander G, Norbäck D. A field study on clinical signs and symptoms in cleaners at floor polish removal and application in a Swedish hospital. Int Arch Occup Environ Health. 2010;83:585–591. doi: 10.1007/s00420-010-0531-5. [DOI] [PubMed] [Google Scholar]
- Wolkoff P, Clausen PA, Wilkins CK, Hougaard KS, Nielsen GD. Formation of strong airway irritants in a model mixture of (+)-α-pinene/ozone. Atm Environ. 1999;33:693–698. [Google Scholar]
- Zhu J, Cao XL, Beauchamp R. Determination of 2-butoxyethanol emissions from selected consumer products and its application in assessment of inhalation exposure associated with cleaning tasks. Environ Int. 2001;26:589–597. doi: 10.1016/s0160-4120(01)00046-0. [DOI] [PubMed] [Google Scholar]
- Zock JP, Plana E, Jarvis D, Anto JM, Kromhout H, Kennedy SM, Kunzli N, Villani S, Olivieri M, Toren K, et al. The use of household cleaning sprays and adult asthma: An international longitudinal study. Am J Respir Crit Care Med. 2007;176:735–741. doi: 10.1164/rccm.200612-1793OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.