Abstract
Background
In 2011, the Centers for Disease Control and Prevention and the New Jersey Department of Health used the New Jersey Behavioral Risk Factor Survey (NJBRFS), a state component of the national Behavioral Risk Factor Surveillance System (BRFSS) to pilot a travel health module designed to collect population-based data on New Jersey residents travelling internationally. Our objective was to use this population-based travel health information to serve as a baseline to evaluate trends in US international travellers.
Methods
A representative sample of New Jersey residents was identified through a random-digit-dialing method and administered the travel health module, which asked five questions: travel outside of USA during the previous year; destination; purpose; if a healthcare provider was visited before travel and any travel-related illness. Additional health variables from the larger NJBRFS were considered and included in bivariate analyses and multiple logistic regression; weights were assigned to variables to account for survey design complexity.
Results
Of 4029 participants, 841 (21%) travelled internationally. Top destinations included Mexico (10%), Canada (9%), Dominican Republic (6%), Bahamas (5%) and Italy (5%). Variables positively associated with travel included foreign birth, ≥$75 000 annual household income, college education and no children living in the household. One hundred fifty (18%) of 821 travellers with known destinations went to high-risk countries; 40% were visiting friends and relatives and only 30% sought pre-travel healthcare. Forty-eight (6%) of 837 responding travellers reported travel-related illness; 44% visited high-risk countries.
Conclusions
Approximately one in five NJBRFS respondents travelled internationally during the previous year, a sizeable proportion to high-risk destinations. Few reported becoming ill as a result of travel but almost one-half of those ill had travelled to high-risk destinations. Population-based surveillance data on travellers can help document trends in destinations, traveller type and disease prevalence and evaluate the effectiveness of disease prevention programmmes.
Keywords: US international travel, population-based surveillance, BRFSS, travellers’ health, New Jersey, travel epidemiology
Background
International travel volume has grown substantially during the past two decades. In 2013, US residents made >61 million trips with at least one night outside US borders, an approximate 33% increase since 1994.1, 2 Not only are more people travelling but also more are travelling to the developing world and returning ill to their country of residence. For example, in 2011, 1920 cases of malaria were diagnosed in US travellers returning from trips overseas, the highest number in 40 years.3 Travellers returning home sick can also have an impact on the domestic US population. A total of 23 measles outbreaks occurred in USA in 2014, amounting to 648 cases, the most in USA since the disease was declared eliminated in 2000 [Centers for Disease Control and Prevention (CDC), unpublished data, 2015]. All 23 outbreaks resulted from importations from travel from foreign countries, including a large, widely reported measles outbreak involving a popular amusement park in California.4
Despite the impact of travel-related illnesses, few population-based data exist describing the travel characteristics, pre-travel health preparation and health-related behaviours of US international travellers. Much of the literature on which guidance for travellers is based comes from limited airport surveys, clinic-based convenience samples and case studies.5-11 As the world’s largest ongoing telephone health survey,12 the Behavioral Risk Factor Surveillance System (BRFSS) is the gold standard for behavioural surveillance in USA. The Travellers’ Health Branch of the CDC and the New Jersey Department of Health (NJDOH) piloted a set of travel health questions with existing health modules in the 2011 New Jersey Behavioral Risk Factor Survey (NJBRFS), a state component of the national BRFSS. The aim was to use the variables in the NJBRFS and the travel health module to collect data on a variety of potential demographic and socioeconomic indicators for international travel as well as the decision to seek pre-travel care. This baseline population-based data on travellers can help document trends in destinations, traveller type and disease prevalence and evaluate the effectiveness of disease prevention programmmes.
Methods
BRFSS is a system of telephone surveys that collects data on health-related risk behaviours, chronic health conditions and preventive health service utilization from a representative sample of civilian non-institutionalized adults (≥18 years) in each of the 50 states, the District of Columbia and three US territories. Post-stratification weights are used to adjust for non-response, non-coverage and uneven selection of the population to generate demographic distributions that closely match the state population. A detailed description of the survey design, random sampling procedures and validity of measures are available elsewhere.13-15
Travel Health Module
The NJDOH and CDC inserted five travel health questions (travel health module) into the 2011 NJBRFS; the five questions were asked to a subset of randomly assigned persons from eligible respondents in the landline sample of the 2011 NJBRFS. To include as many health subjects in the survey as possible while keeping a robust sample size to maintain data quality, approximately one-quarter of the landline sample was administered the module. The five questions were regarding whether respondents travelled outside of USA during the previous 12 months, the travel destination, the travel purpose, whether they visited a healthcare provider prior to travelling and whether they became sick during, or upon returning from, their trip. Only interviewees who were asked whether they travelled outside of USA were administered the additional questions in the travel health module. If respondents travelled to more than one country during the 12 months, they were asked to state the country in which they spent the most amount of travel time. All interviewees who answered ‘don’t know’ or ‘refused’ for a question in the NJBRFS were excluded from the analysis for that particular question.
A destination risk assignment (high, medium or low) was based on the specific country to which the respondent travelled and categorized based on the United Nations Human Development Index (HDI). The HDI was used as a proxy for explaining differences in risk a traveller may face depending on their specific travel destination. In general, destinations with lower human development can present more challenges to the health and well-being of international travellers than destinations with high human development. Some destinations were not included in the HDI; these places were assigned a risk category that was deemed most appropriate, based, in part, by geographic relationships to other countries in the HDI as well as by the World Bank classification for country income. More information regarding the HDI and the World Bank classification can be found elsewhere.16, 17
Other NJBRFS Variables
We included other variables in the NJBRFS, specifically demographics (age, sex, race, country of birth), socioeconomic (income, education level, current employment, marital status, number of children living in the home), health and health access (current healthcare coverage, current disability, health problem requiring special equipment) and health behaviour (smoking, binge drinking, seatbelt use, risky behaviours for HIV in the past 12 months, physical activity in past 30 days, influenza vaccine received in the past 12 months) variables. We also examined several specific health conditions, including high blood pressure, myocardial infarction, angina/coronary heart disease, stroke, cancers, chronic obstructive pulmonary disease (COPD)/emphysema/chronic bronchitis, depression, anxiety, rheumatic diseases (arthritis/rheumatoid arthritis/gout/lupus/fibromyalgia), asthma and diabetes. Binge drinking was defined as four drinks per day for women and five drinks per day for men, ≥1 day per month. Risky behaviours for HIV included intravenous ≥ drug use, treatment for a sexually transmitted infection, exchanging money/drugs for sex or vice versa and anal sex without a condom. A current disability was defined as anything physical, mental or emotional that limited the person’s activities in any way.
Data Analysis
We calculated variable frequencies, and bivariate analyses were performed for the outcome of international travel and, for high-risk destination travellers, a dichotomous outcome of pre-travel care. To account for the complexity of the survey–sample design, post-stratification weights were assigned to all variables for the bivariate analysis. The methodology for assigning post-stratification weights in the landline sample of the 2011 BRFSS data is described elsewhere.13 A two-sample t-test was used to calculate the difference in means for age and a chi-square test was used for categorical variables to calculate odds ratios (OR). Two logistic regression models were used to determine factors associated with international travel and the seeking of pre-travel care for travellers to high-risk destinations. Demographic variables of interest that were found to be significant in the bivariate analysis as well as others that were considered to be contributing factors a priori based on the literature were included in the models. Statistical significance was determined at the two-sided 0.05 level. SAS Enterprise Guide v5.1 (SAS Institute, Cary, NC) was used for all analyses.
Results
Characteristics of Travellers
Of 15 383 NJBRFS interviews conducted in 2011, 4029 respondents (26%) were asked whether or not they travelled outside USA in the past 12 months. Of 4029, 841 (21%) had travelled internationally, 3177 (79%) did not travel internationally and 11 (0.2%) refused or did not know. Of 841 international travellers, 493 (59%) were female and had a mean age of 52 years [standard error (SE) = 0.6] (range 18–88 years). Among 831 travellers who reported their race, 646 (78%) were Caucasian, 67 (8%) African–American, 61 (7%) Asian and 57 (7%) other or mixed race. Twenty-six percent were born outside of USA. Approximately two-thirds (65%) of travellers were employed, 62% had four or more years of college, 60% made ≥$75 000 per year and 67% had no children currently living in their household. Eight hundred one travellers (95%) had current health coverage in the form of health insurance, prepaid plans such as Health Maintenance Organizations (HMOs) or government plans such as Medicare or Indian Health Services.
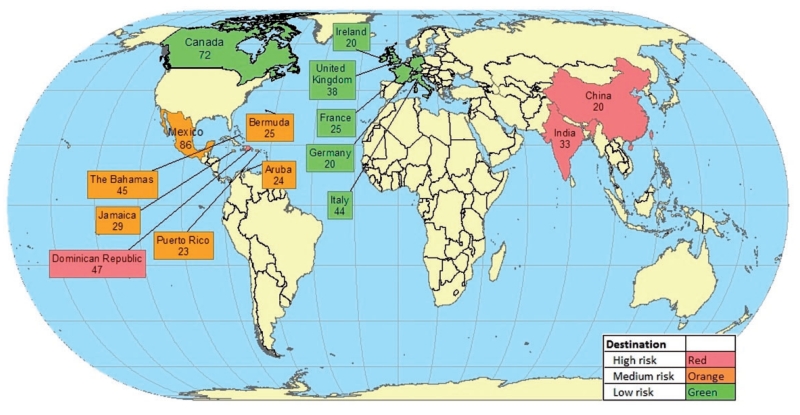
The primary purpose of travel for the 841 international travellers was vacation (71%) followed by visiting friends and relatives [(VFR) 18%] and business (8%); the remaining 3% travelled for health/medical treatment, volunteer/missionary work or another reason (Table 1). Of the 841 travellers, 821 (98%) specified their destination country; of these, 320 (39%) went to a low-risk country, 351 (43%) to a medium-risk country and 150 (18%) to a high-risk country (Table 1). The top 15 overall destinations included six low-risk countries, six medium-risk countries and three high-risk countries (Figure 1). Among all high-risk destinations, the most frequently reported were the Dominican Republic (31%), India (22%), China (13%), the Philippines (4%) and South Africa (3%).
Table 1.
Travel characteristics of the internationally travelling population of New Jersey, 2011
| n (%) | |
|---|---|
| Participated in a pre-travel health visit (n = 838) | 117 (14) |
| Purpose of travel (n = 839) | |
| Vacation/leisure | 595 (71) |
| Visiting friends or relatives | 149 (18) |
| Business | 69 (8) |
| Othera | 26 (3) |
| Acquired illness during travelb(n = 837) | 48 (6) |
| Risk of destination (n = 821) | |
| High-risk country | 150 (18) |
| Medium-risk country | 351 (43) |
| Low-risk country | 320 (39) |
| Top high-risk destinations visited (n = 150) | |
| Dominican Republic | 47 (31) |
| India | 33 (22) |
| China | 20 (13) |
| Philippines | 6 (4) |
| South Africa | 5 (3) |
Includes those travelling for volunteer/missionary purposes, health/medical treatment, research/study or another purpose.
Includes those who began experiencing symptoms within 7 days after return to USA.
Figure 1.
Top 15 destinations among New Jersey international travellers, by destination risk category, NJBRFS, 2011. Numbers listed for each country refer to the number of travellers who indicated the country as their primary travel destination in the previous year
Characteristics of International Travellers vs Non-Travellers
On average, international travellers were slightly younger than non-travellers (52.3 vs 55.3 years, P < 0.0001, Table 2). In the bivariate analysis, those who were male, employed, married, foreign-born, had four or more years of college education, or made at least $75 000 were more likely to travel internationally (P < 0.0001). In a multiple regression model, being foreign-born (P < 0.0001), making at least $75 000 per year (P < 0.0001), having four or more years of college education (P < 0.0001) and having no children living in the household (P = 0.0016) were all independently associated with international travel.
Table 2.
Demographic characteristics of international travellers and non-travellers, New Jersey, 2011
| Demographic characteristics | International travel mean (SE) or n (row %) |
|||
|---|---|---|---|---|
| Yes (n = 841) | No (n = 3177) | cORa (95% Confidence Interval [CI]) | P | |
| Mean age, years (SE) | 52.3 (0.6) | 55.3 (0.3) | - | <0.0001 |
| Sex | ||||
| Male (n = 1479) | 348 (24) | 1131 (76) | 1.47 (1.23, 1.75) | <0.0001 |
| Female (n = 2539) | 493 (19) | 2046 (81) | ||
| Race | ||||
| Non-white (n = 789) | 185 (23) | 604 (77) | 1.19 (0.97, 1.46) | 0.09 |
| White (n = 3166) | 646 (20) | 2520 (80) | ||
| Location of birthb | ||||
| Foreign-born (n = 622) | 222 (36) | 400 (64) | 2.5 (2.04, 3.07) | <0.0001 |
| US-born (n = 3394) | 619 (18) | 2775 (82) | ||
| Employment | ||||
| Working (n = 2137) | 544 (25) | 1593 (75) | 1.72 (1.44, 2.06) | <0.0001 |
| Not working (n = 1869) | 296 (16) | 1573 (84) | ||
| Educationb | ||||
| ≥4 years of college (n = 1712) | 519 (30) | 1193 (70) | 2.53 (2.12, 3.02) | <0.0001 |
| < 4 years of college (n = 2300) | 320 (14) | 1980 (86) | ||
| Annual Incomeb | ||||
| ≥$75 000 (n = 1438) | 441 (31) | 997 (69) | 2.42 (2.00, 2.92) | <0.0001 |
| < $75 000 (n = 2049) | 296 (14) | 1753 (86) | ||
| Marital status | ||||
| Married (n = 2199) | 544 (25) | 1655 (75) | 1.61 (1.35, 1.93) | <0.0001 |
| Not married (n = 1802) | 293 (16) | 1509 (84) | ||
| Children living in householdb | ||||
| Yes (n = 1227) | 274 (22) | 953 (78) | 1.04 (0.87, 1.26) | 0.65 |
| No (n = 2704) | 552 (20) | 2152 (80) | ||
Crude odds ratio.
In a multiple logistic regression model, these factors were all associated with international travel.
Those who reported having the following conditions were significantly less likely to travel than those without the conditions (Table 3): high blood pressure, asthma, depression, anxiety, diabetes, chronic lung disease (COPD/emphysema/chronic bronchitis), rheumatic disease (arthritis/rheumatoid arthritis/gout/lupus/fibromyalgia) and angina/coronary heart disease. In addition, those who had ever previously been told that they had suffered a myocardial infarction or stroke, had a health problem that required special treatment or had a current physical, mental or emotional disability were significantly less likely to travel internationally. Those with current health coverage were twice as likely to travel compared with those without health coverage (OR = 2.05, P = 0.0002). Those who engaged in physical activity or in binge drinking at least once during the 30 days before being interviewed were significantly more likely to travel internationally than those who did not. Non-smokers were significantly more likely to travel internationally than smokers.
Table 3.
Pre-existing health conditions, health characteristics and health risk behaviours of international travellers and non-travellers, New Jersey 2011
| International travel mean (SE) or n (row %) |
||||
|---|---|---|---|---|
| Health conditions | Yes (n = 841) | No (n = 3177) | cORa (95% CI) | P |
| High blood pressure | ||||
| Yes (n = 1548) | 277 (18) | 1271 (82) | 0.68 (0.57, 0.82) | <0.0001 |
| No (n = 2463) | 563 (23) | 1900 (77) | ||
| Asthma | ||||
| Yes (n = 509) | 84 (17) | 425 (83) | 0.64 (0.48, 0.85) | 0.0018 |
| No (n = 3494) | 754 (22) | 2740 (78) | ||
| Depressive disorder | ||||
| Yes (n = 493) | 78 (16) | 415 (84) | 0.63 (0.47, 0.84) | 0.0016 |
| No (n = 3502) | 760 (22) | 2742 (78) | ||
| Anxiety disorder | ||||
| Yes (n = 430) | 63 (15) | 367 (85) | 0.61 (0.45, 0.83) | 0.0017 |
| No (n = 3567) | 775 (22) | 2792 (78) | ||
| Diabetes | ||||
| Yes (n = 486) | 62 (13) | 424 (87) | 0.56 (0.41, 0.78) | 0.0004 |
| No (n = 3529) | 779 (22) | 2750 (78) | ||
| COPD/emphysema/chronic bronchitis | ||||
| Yes (n = 287) | 38 (13) | 249 (87) | 0.60 (0.40, 0.88) | 0.0088 |
| No (n = 3711) | 800 (22) | 2911 (78) | ||
| Arthritis/rheumatoid arthritis/gout/lupus/fibromyalgia | ||||
| Yes (n = 1265) | 209 (17) | 1056 (83) | 0.65 (0.53, 0.79) | <0.0001 |
| No (n = 2732) | 628 (23) | 2104 (77) | ||
| Angina/coronary heart disease | ||||
| Yes (n = 232) | 32 (14) | 200 (86) | 0.52 (0.32, 0.84) | 0.0071 |
| No (n = 3753) | 805 (21) | 2948 (79) | ||
| Myocardial infarction | ||||
| Yes (n = 216) | 23 (11) | 193 (89) | 0.44 (0.26, 0.76) | 0.0027 |
| No (n = 3788) | 816 (22) | 2972 (78) | ||
| Stroke | ||||
| Yes (n = 135) | 18 (13) | 117 (87) | 0.49 (0.26, 0.90) | 0.0184 |
| No (n = 3875) | 819 (21) | 3056 (79) | ||
| Kidney disease | ||||
| Yes (n = 102) | 16 (16) | 86 (84) | 0.71 (0.38, 1.33) | 0.2892 |
| No (n = 3908) | 824 (21) | 3084 (79) | ||
| Skin cancer | ||||
| Yes (n = 316) | 68 (22) | 248 (78) | 1.16 (0.84, 1.59) | 0.3749 |
| No (n = 3692) | 772 (21) | 2920 (79) | ||
| Other types of Cancer | ||||
| Yes (n = 347) | 79 (23) | 268 (77) | 1.19 (0.88, 1.60) | 0.2493 |
| No (n = 3660) | 758 (21) | 2902 (79) | ||
| Health characteristics | ||||
| Current health coverageb | ||||
| Yes (n = 3686) | 801 (22) | 2885 (78) | 2.05 (1.39, 3.03) | 0.0002 |
| No (n = 320) | 38 (12) | 282 (88) | ||
| Current physical mental or emotional disability | ||||
| Yes (n = 984) | 148 (15) | 836 (85) | 0.59 (0.47, 0.74) | <0.0001 |
| No (n = 3018) | 692 (23) | 2326 (77) | ||
| Health problem requiring special equipment | ||||
| Yes (n = 368) | 28 (8) | 340 (92) | 0.25 (0.16, 0.40) | <0.0001 |
| No (n = 3649) | 813 (22) | 2836 (78) | ||
| Health risk behaviours | ||||
| Any physical activity in last 30 days | ||||
| Yes (n = 2917) | 688 (24) | 2229 (76) | 1.77 (1.43, 2.20) | <0.0001 |
| No (n = 1094) | 152 (14) | 942 (86) | ||
| Binge drinking | ||||
| ≥1 time/month (n = 492) | 149 (30) | 343 (70) | 1.36 (1.05, 1.76) | 0.0213 |
| Not at all (n = 1872) | 445 (24) | 1427 (76) | ||
| Smoking | ||||
| Do not smoke (n = 1271) | 267 (21) | 1004 (79) | 1.60 (1.18, 2.18) | 0.0026 |
| Smoke (n = 576) | 75 (13) | 501 (87) | ||
| How often use seatbelt | ||||
| Always (n = 3663) | 786 (21) | 2877 (79) | 1.45 (1.00, 2.10) | 0.0476 |
| Not always (n = 326) | 52 (16) | 274 (84) | ||
| Engaged in risky behaviours for HIV | ||||
| Yes (n = 68) | 21 (31) | 47 (69) | 1.68 (0.92, 3.08) | 0.0904 |
| No (n = 3932) | 817 (21) | 3115 (79) | ||
| Flu vaccine in last 12 months | ||||
| Yes (n = 1813) | 397 (22) | 1416 (78) | 1.06 (0.89, 1.27) | 0.493 |
| No (n = 2198) | 444 (20) | 1754 (80) | ||
Crude odds ratio.
Includes health insurance, prepaid plans such as HMOs or government health plans such as Medicare or Indian Health Services.
Those who were vaccinated for influenza were statistically as likely to travel internationally as those who were not vaccinated (22 vs 20%, P = 0.49). Having been vaccinated for influenza was inversely proportional to destination risk category: 170 (53%) of 320 travellers to low-risk destinations received influenza vaccine vs 164 (47%) of 351 to medium-risk destinations and 54 (36%) of 150 to high-risk destinations.
Travellers to High-Risk Destinations
Of the 149 travellers who went to high-risk destinations and reported their reason for travel, the primary purpose of travel was vacation/leisure (46%), followed by VFR (40%) and business (10%). Overall, 85 (57%) travellers to high-risk destinations were foreign-born and only 30% sought pre-travel healthcare. Only 19 (28%) of 68 vacation/leisure travellers, 16 (27%) of 60 VFR travellers and seven (47%) of 15 business travellers to high-risk destinations sought pre-travel care (Table 4). A similar proportion of US-born travellers sought pre-travel care (31%) compared with foreign-born travellers (29%) going to high-risk destinations (Table 4). Those who made at least $75 000 per year had more than twice the odds of seeking pre-travel care than those who made <$75 000 per year (OR = 2.26, P = 0.05). Age (P = 0.44), sex (P = 0.58), being a VFR traveller (P = 0.17), education level (P = 0.42), having children living in the household (P = 0.30) and being currently employed (P = 0.66) were not associated with seeking pre-travel care. Among travellers to high-risk destinations, there was no association between travellers who received pre-travel care and whether they had received influenza vaccination (P = 0.16). No variables were found to be statistically significantly associated with pre-travel care in the multiple regression model.
Table 4.
Demographic and health characteristics among travellers to high-risk countries who did or did not seek pre-travel care, New Jersey, 2011
| Pre-travel care mean (SE) or n (row %) |
||||
|---|---|---|---|---|
| Demographic characteristics | Yes (n = 45) | No (n = 104) | cORa (95% CI) | P |
| Mean age, years (SE) | 48.4 (2.3) | 50.7 (1.5) | - | 0.44 |
| Sex | ||||
| Female (n = 83) | 24 (29) | 59 (71) | 0.81 (0.37, 1.74) | 0.58 |
| Male (n = 66) | 21 (32) | 45 (68) | ||
| Purpose of travel | ||||
| Vacation/leisure (n = 68) | 19 (28) | 49(72) | - | 0.35 |
| VFRb (n = 60) | 16 (27) | 44 (73) | ||
| Business (n = 15) | 7 (47) | 8 (53) | ||
| Otherc (n = 6) | 3 (50) | 3 (50) | ||
| Location of birth | ||||
| Foreign-born (n = 85) | 25 (29) | 60 (71) | 1.01 (0.46, 2.24) | 0.97 |
| US-born (n = 64) | 20 (31) | 44 (69) | ||
| Employment | ||||
| Not currently working (n = 46) | 16 (35) | 30 (65) | 1.2 (0.53, 2.70) | 0.66 |
| Working (n = 93) | 29 (28) | 74 (72) | ||
| Education | ||||
| ≥4 years of college (n = 95) | 32 (34) | 63 (66) | 1.4 (0.61, 3.18) | 0.42 |
| <4 years of college (n = 54) | 13 (24) | 41 (76) | ||
| Income | ||||
| ≥75 000 (n = 78) | 28 (36) | 50 (64) | 2.26 (0.99, 5.1) | 0.05 |
| <75 000 (n = 60) | 15 (25) | 45 (75) | ||
| Children | ||||
| Children (n = 68) | 23 (34) | 45 (66) | 1.51 (0.68, 3.33) | 0.31 |
| No children (n = 79) | 22 (28) | 57 (72) | ||
| Health characteristics | ||||
| Current health coveraged | ||||
| Yes (n = 137) | 43 (31) | 94 (69) | 3.45 (0.69, 17.17) | 0.11 |
| No (n = 12) | 2 (17) | 10 (83) | ||
| Current physical, mental or emotional disability | ||||
| Yes (n = 19) | 8 (42) | 11 (58) | 1.64 (0.55, 4.90) | 0.37 |
| No (n = 130) | 37 (28) | 93 (72) | ||
| Acquired illness abroad | ||||
| Yes (n = 21) | 6 (29) | 15 (71) | 0.56 (0.18, 1.80) | 0.32 |
| No (n = 128) | 39 (30) | 89 (70) | ||
| Flu vaccine in last 12 months | ||||
| Yes (n = 53) | 19 (36) | 34 (64) | 1.76 (0.79, 3.95) | 0.16 |
| No (n = 96) | 26 (27) | 70 (73) | ||
Crude odds ratio.
The purpose of travel variable was also dichotomized into VFRs and non-VFRs. An additional bivariate analysis and multiple logistic regression model were assessed, P = 0.17 and 0.14, respectively.
Includes those travelling for volunteer/missionary purposes (3), health/medical treatment (1), research/study (1) or another purpose (1).
Includes health insurance, prepaid plans such as HMOs, or government health plans such as Medicare or Indian Health Services.
Reported Illness among Travellers
Forty-eight (6%) of 837 travellers reported that they acquired an illness during travel or within 7 days of returning to USA. Twenty-one (44%) of the 48 with illness visited high-risk destinations; these 21 comprised 14% of all travellers to high-risk destinations. Those who became ill had travelled to the Dominican Republic (6), India (4), China (4), Philippines (3), El Salvador (1), Guyana (1), Vietnam (1) and Sub-Saharan Africa (1) (data not shown). Among the 21 travellers to high-risk destinations who reported an illness, six (29%) received pre-travel care.
Discussion
We found that approximately one-fifth of New Jersey residents interviewed travelled internationally during the previous year. This pilot study is the first population-based study that uses the BRFSS to describe specific variables related to international travel and health. These data were obtained in New Jersey, a state with one of the largest internationally travelling populations in USA and a state that accounted for 10% of all US resident international travel in 2010.18 As more US residents travel overseas, and with increasing numbers going to higher-risk destinations, information on travel patterns, associated illnesses and related healthcare utilization will be increasingly valuable to medical and public health professionals.
In our study, few travellers reported becoming ill as a result of their travel. However, almost one-half of those who reported travel-associated illness travelled to high-risk destinations, accounting for 14% of all travellers to high-risk destinations. This number is slightly lower compared with cohort studies that assessed travel-related illness in travellers to the developing world; in these studies the proportion of travellers who experienced an illness during travel ranged from 15–70%.19-25 Although a pre-travel health consultation cannot guarantee a traveller’s health and safety, a well-organized and -executed consultation using counselling, education and administration of vaccines and prescriptions can help reduce and manage the risk of illness and injury during travel.26 In addition, the pre-travel consultation creates awareness of preventable health risks and may reduce the risk of infected travellers importing travel-related diseases into the local population of the home country. Despite these benefits, we found that only 14% of travellers overall sought pre-travel care before going abroad; alarmingly, only 30% of those going to high-risk destinations sought pre-travel care. This latter number was similar to that found in a 2003 study of American travellers leaving John F. Kennedy International Airport: 36% of travellers going to high-risk destinations reported seeking health advice,6 suggesting that the trend of low participation in seeking pre-travel care has not changed.
Overall, we found proportionally lower numbers of VFR travellers among our respondents than was found in other studies.6, 8, 27 However, VFRs in our study accounted for 40% of travellers to high-risk destinations. VFRs remain a particular concern since they have been shown to have disproportionate infectious disease risk compared with other types of travellers.26 For example, of the 908 cases of imported malaria in USA in 2012 among US citizens for which purpose of travel was known, 603 (66%) were VFRs.28 Likely reasons for disproportionate disease risk in VFRs include, but are not limited to, the belief that they are immune to diseases in their destination country, propensity of travel to higher-risk destinations such as staying in homes and living the local lifestyle that often includes lack of safe food and water and cultural and language barriers with healthcare providers.26 Interestingly, we found a similarly low proportion of pre-travel care among VFR (27%) and vacation/leisure travellers (28%) going to high-risk destinations, suggesting more needs to be done to reach all travellers to high-risk destinations.
Our data indicated that compared with non-travellers, international travellers tended to be healthier overall, engaged in many positive health behaviours, including physical activity, and not smoking. Travellers were less likely to have health conditions such as arthritis, asthma, depression or anxiety or previous health complications such as a myocardial infarction, stroke or diabetes. However, there were some conditions of note among international travellers. Approximately one-fifth of travellers had a current physical, mental or emotional disability and one-third of those who travelled reported high blood pressure. Studies by LaRocque et al.,7 and Hochberg et al.29 found the proportion of international travellers with underlying health conditions to be 59 and 18% respectfully; however, all travellers in these studies attended pre-travel health consultations where medical histories were verified by clinicians.
Less than one-half of travellers received an influenza vaccination in the 12 months prior to departing USA. Further, the proportion of international travellers vaccinated for influenza was inversely proportional by destination risk, with the largest proportion of those vaccinated going to low-risk destinations and the smallest proportion of those vaccinated going to high-risk destinations. International travel does not necessarily increase one’s risk of getting influenza; however, travel to tropical countries, or countries in the Southern Hemisphere, and contact with people from these countries, can put one at risk for influenza, outside of the regular influenza season in USA.30 Although we were unable to determine the nature of the travel-related illnesses, 48 (6%) travellers reported illness abroad or within 7 days of returning to USA; those who became ill were no more likely to have received the influenza vaccine than those who did not become ill. Influenza vaccination may be a viable protective measure depending on these factors as well as the health profile of the individual patient.26 Clinicians can use the pre-travel health consultation as an opportunity to suggest influenza vaccination to travellers who may not have already received the vaccine.
Almost all of those interviewed had current health insurance. However, those with health coverage were more than twice as likely to travel internationally. Although this is encouraging, many insurance carriers do not provide coverage when policy holders are travelling abroad. International travellers should be reminded by clinicians to carefully check their policies before travel and, if necessary, purchase supplementary travel, travel-health or medical-evacuation insurance.26
This study had several limitations. First, BRFSS information is self-reported, which could result in recall error or bias, especially since some questions asked participants to recall events up to 1 year prior to the interview. Second, the state-added questions for travel health were included in the landline-only version of the 2011 NJBRFS; therefore, the data were limited to a random-digit dialing method that excluded households without landline telephones or that have only cellular telephone coverage.31 As a result, a sizeable portion of the New Jersey population that did not have a landline phone was not included in this analysis. A proxy was used to estimate destination risk, and the low, medium and high categories defined in this study may not accurately represent the true risk of infectious disease or injury. Though we were able to collect data on the occurrence of travel-related illness, we were unable to collect data on the specific illnesses experienced or their impact during the trip or upon returning home. Finally, the results of this study reflect the internationally travelling population of New Jersey in 2011 and may not be representative of the entire internationally travelling population of USA.
This pilot study of the travel health module provides valuable baseline surveillance data on US international travellers. In addition to data on general travel health characteristics from the module, the NJBRFS allowed us to collect data on a variety of potential demographic and socioeconomic indicators for international travel as well as the decision to seek pre-travel care. Using these data as a baseline for comparison for future BRFSS travel health studies will also allow us to examine trends over time and evaluate the effectiveness of prevention programmmes. Additional travel health studies with the BRFSS, including expanding the travel health module to new states and incorporating additional questions on travel-related syndromes experienced and emerging topics (e.g. medical tourism), could help federal, state and local health authorities and providers identify and quantify new high-risk subpopulations within this large and rapidly growing demographic, helping to support policies and programmmes designed to assist them.
Acknowledgements
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors acknowledge Kenneth O’Dowd, the New Jersey state BRFSS coordinator, for his technical assistance. They also acknowledge Susan Redd and Allison Maiuri of CDC’s National Center for Immunization and Respiratory Diseases, Division of Viral Diseases and R. Ryan Lash of the Division of Global Migration and Quarantine for their expertise.
Footnotes
The findings of this study were presented at the 14th Conference of the International Society of Travel Medicine, Quebec City, Canada in May, 2015.
Conflict of interest: None declared.
References
- 1.International Trade Administration. U.S. Department of Commerce [5 January 2015, date last accessed];United States Resident Travel Abroad. 2013 2013 http://travel.trade.gov/outreachpages/download_data_table/2013_US_Travel_Abroad.pdf.
- 2.International Trade Administration. U.S. Department of Commerce [5 January 2015, date last accessed];Top Destinations for U.S. Travelers 1995/1994. 1994 http://travel.trade.gov/view/f-3/freeab23.html.
- 3.Cullen KA, Arguin PM. Division of Parasitic Diseases, Centers for Disease Control and Prevention. Malaria surveillance–United States, 2011. MMWR Surveill Summ. 2013;62:1–17. [PubMed] [Google Scholar]
- 4.National Center for Immunization and Resiratory Diseases. Division of Viral Diseases. Centers for Disease Control and Prevention [18 March 2015, date last accessed];U.S. Multi-state Measles Outbreak 2014—2015. 2015 http://www.cdc.gov/measles/multi-state-outbreak.html.
- 5.Dahlgren AL, DeRoo L, Steffen R. Prevention of travel-related infectious diseases: knowledge, practices and attitudes of Swedish travellers. Scand J Infect Dis. 2006;38:1074–80. doi: 10.1080/00365540600868354. [DOI] [PubMed] [Google Scholar]
- 6.Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11:23–6. doi: 10.2310/7060.2004.13577. [DOI] [PubMed] [Google Scholar]
- 7.Larocque RC, Rao SR, Lee J, et al. Global TravEpiNet: a national consortium of clinics providing care to international travelers–analysis of demographic characteristics, travel destinations, and pre-travel healthcare of high-risk US international travelers, 2009-2011. Clin Infect Dis. 2012;54:455–62. doi: 10.1093/cid/cir839. [DOI] [PubMed] [Google Scholar]
- 8.LaRocque RC, Rao SR, Tsibris A, et al. Pre-travel health advice-seeking behavior among US international travelers departing from Boston Logan International Airport. J Travel Med. 2010;17:387–91. doi: 10.1111/j.1708-8305.2010.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharp TM, Pillai P, Hunsperger E, et al. A cluster of dengue cases in American missionaries returning from Haiti, 2010. Am J Trop Med Hyg. 2012;86:16–22. doi: 10.4269/ajtmh.2012.11-0427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Herck K, Van Damme P, Castelli F, et al. Knowledge, attitudes and practices in travel-related infectious diseases: the European airport survey. J Travel Med. 2004;11:3–8. doi: 10.2310/7060.2004.13609. [DOI] [PubMed] [Google Scholar]
- 11.Harvey K, Esposito DH, Han P, et al. Surveillance for travel-related disease–GeoSentinel Surveillance System, United States, 1997-2011. MMWR Surveill Summ. 2013;62:1–23. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention [9 September 2014, date last accessed];Behavioral Risk Factor Surveillance System. 2013 http://www.cdc.gov/brfss/about/about_brfss.htm.
- 13.Centers for Disease Control and Prevention [9 September 2014, date last accessed];Behavioral Risk Factor Surveillance System 2011 Landline Questionnaire Use of Data. 2012 http://www.cdc.gov/brfss/annual_data/2011/2011_landline_data_modules.pdf.
- 14.Centers for Disease Control and Prevention [30 October 2014, date last accessed];Overview: BRFSS 2011. 2011 http://www.cdc.gov/brfss/annual_data/2011/overview_11.pdf.
- 15.Nelson DE, Holtzman D, Bolen J, et al. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Soz Praventivmed. 2001;46(Suppl 1):S3–42. [PubMed] [Google Scholar]
- 16.United Nations Development Programme. Human Development Index (HDI) [20 February 2012, date last accessed]; http://hdr.undp.org/en/content/human-development-index-hdi.
- 17.The World Bank Group [5 January 2012, date last accessed];World DataBank World Development Indicators. 2012 http://databank.worldbank.org/data/views/variableselection/selectvariables.aspx?source=world-development-indicators.
- 18.International Trade Administration. U.S. Department of Commerce [10 January 2011, date last accessed];Profile of U.S. resident travelers visiting overseas destinations: 2010 outbound. 2010 http://tinet.ita.doc.gov/outreachpages/download_data_table/2010_Outbound_Profile.pdf.
- 19.Ahlm C, Lundberg S, Fesse K, et al. Health problems and self-medication among swedish travellers. Scand J Infect Dis. 1994;26:711–7. doi: 10.3109/00365549409008640. [DOI] [PubMed] [Google Scholar]
- 20.Hill DR. Health problems in a large cohort of americans traveling to developing countries. J Travel Med. 2000;7:259–66. doi: 10.2310/7060.2000.00075. [DOI] [PubMed] [Google Scholar]
- 21.Kendrick MA. Study of illness among Americans returning from international travel, July 11–August 24, 1971. (preliminary data) J Infect Dis. 1972;126:684–5. doi: 10.1093/infdis/126.6.684. [DOI] [PubMed] [Google Scholar]
- 22.Reid D, Dewar RD, Fallon RJ, et al. Infection and travel: the experience of package tourists and other travellers. J Infect. 1980;2:365–70. doi: 10.1016/s0163-4453(80)92864-9. [DOI] [PubMed] [Google Scholar]
- 23.Scoville SL, Bryan JP, Tribble D, et al. Epidemiology, preventive services, and illnesses of international travelers. Mil Med. 1997;162:172–8. [PubMed] [Google Scholar]
- 24.Steffen R, Rickenbach M, Wilhelm U, et al. Health problems after travel to developing countries. J Infect Dis. 1987;156:84–91. doi: 10.1093/infdis/156.1.84. [DOI] [PubMed] [Google Scholar]
- 25.Ryan ET, Kain KC. Health advice and immunizations for travelers. N Engl J Med. 2000;342:1716–25. doi: 10.1056/NEJM200006083422306. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention . CDC Health Information For International Travel 2014. United States Department of Health and Human Services, Public Health Service; Atlanta, GA: 2014. [Google Scholar]
- 27.Behrens RH, Alexander N. Malaria knowledge and utilization of chemoprophylaxis in the UK population and in UK passengers departing to malaria-endemic areas. Malar J. 2013;12:461. doi: 10.1186/1475-2875-12-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cullen KA, Arguin PM. Division of Parasitic Diseases, Centers for Disease Control and Prevention. Malaria surveillance–United States, 2012. MMWR Surveill Summ. 2014;63:1–22. [PubMed] [Google Scholar]
- 29.Hochberg NS, Barnett ED, Chen LH, et al. International travel by persons with medical comorbidities: understanding risks and providing advice. Mayo Clinic proceedings. 2013;88:1231–40. doi: 10.1016/j.mayocp.2013.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention [3 November 2014, date last accessed];Flu (Influenza) 2014 http://wwwnc.cdc.gov/travel/diseases/influenza-seasonal-zoonotic-and-pandemic.
- 31.Hu SS, Pierannunzi C, Balluz L. Integrating a multimode design into a national random-digit-dialed telephone survey. Prev Chronic Dis. 2011;8:A145. [PMC free article] [PubMed] [Google Scholar]