Abstract
Background
Early intervention with medical and/or coronary revascularization treatment approaches remains the cornerstone of the management of patients hospitalized with acute myocardial infarction (AMI). However, several patient groups, especially the elderly, are known to delay seeking prompt medical care after onset of AMI‐associated symptoms. Current trends, and factors associated with prolonged prehospital delay among elderly patients hospitalized with AMI, are incompletely understood.
Methods and Results
Data from a population‐based study of patients hospitalized at all 11 medical centers in central Massachusetts with a confirmed AMI on a biennial basis between 2001 and 2011 were analyzed. Information about duration of prehospital delay after onset of acute coronary symptoms was abstracted from hospital medical records. In patients 65 years and older, the overall median duration of prehospital delay was 2.0 hours, with corresponding median delays of 2.0, 2.1, and 2.0 hours in those aged 65 to 74 years, 75 to 84 years, and in patients 85 years and older, respectively. There were no significant changes over time in median delay times in each of the age strata examined in both crude and multivariable adjusted analyses. A limited number of patient characteristics were associated with prolonged delay in this patient population.
Conclusions
The results of this community‐wide study demonstrate that delay in seeking prompt medical care continues to be a significant problem among elderly patients hospitalized with AMI. The lack of improvement in the timeliness of patients’ care‐seeking behavior during the years under study remains of considerable clinical and public health concern.
Keywords: acute myocardial infarction, elderly, prehospital delay
Subject Categories: Acute Coronary Syndromes, Epidemiology, Cardiovascular Disease, Secondary Prevention
Introduction
Older individuals are at greatest risk for developing and dying from coronary heart disease, particularly acute myocardial infarction (AMI).1, 2 The growing number of elderly patients who are hospitalized for AMI are also more likely to present with atypical symptoms of acute coronary disease, with multiple cardiovascular and noncardiovascular comorbidities, and are less likely to receive evidence‐based cardiac medications and coronary reperfusion strategies compared to younger individuals.3, 4, 5 Older individuals are also significantly more likely to delay seeking medical care after onset of AMI symptoms, which may, in part, contribute to the overall poorer outcomes noted in these high‐risk individuals, even after aggressive management for AMI.3, 6
Although several studies have examined trends in, and factors associated with, duration of prehospital delay in all patients who present with an AMI, few studies have examined the extent of, and relatively recent trends in, prehospital delay in seeking acute medical care among the high‐risk subgroup of elderly persons who are hospitalized with an AMI.7, 8, 9 In addition, few studies have examined the characteristics associated with prolonged delay in elderly patients experiencing an AMI and whether these factors differ among those in various age strata among persons 65 years and older.
The purpose of this population‐based study was to describe the magnitude of, and relatively contemporary decade long trends (2001–2011) in, extent of prehospital delay in elderly patients hospitalized with AMI as well as among those in three age strata of the elderly (eg, 65–74, 75–84, and ≥85 years). A secondary study goal was to examine the association between various patient characteristics with extent of prehospital delay and determine whether these factors differed among the young‐old (65–74 years), moderately old (75–84 years), and oldest‐old (≥85 years) patients hospitalized with an AMI.
Methods
The Worcester Heart Attack Study is an ongoing population‐based investigation that is examining long‐term trends in the incidence and case‐fatality rates of AMI among residents of central Massachusetts hospitalized at all 16 medical centers in metropolitan Worcester, Massachusetts, on an essentially biennial basis attributed to the availability of federal funding support.10, 11, 12, 13 Fewer hospitals (n=11) have been included during recent study years because of hospital closures, mergers, and conversion to chronic care facilities. Among these 11 hospitals, 8 were community medical centers and 3 were tertiary care medical centers; among the latter centers, 2 had percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) capability.14 For purposes of the present study, to describe relatively contemporary decade long trends in prehospital delay, we included residents of central Massachusetts who were 65 years and older at the time of their hospitalization for an AMI on a biennial basis between 2001 and 2011 at all 11 participating medical centers in central Massachusetts.
The details of this study have been described previously.10, 11, 12, 13 In brief, computerized printouts of patients discharged from all greater Worcester hospitals with possible AMI during the years under study were obtained, and International Classification of Disease (ICD) codes for possible AMI (ICD‐9 codes 410–414, 786.5) were reviewed for purposes of sample selection. In the city of Worcester, if a patient is suspected of having an ST‐segment elevation AMI, the PCI lab at appropriate city of Worcester hospitals is activated from the field. At the community level, paramedics can send the 12‐lead electrocardiogram to an emergency room (ER) physician for interpretation, who can then activate the appropriate cardiac catheterization/PCI capable lab as needed.
Cases of possible AMI treated at all greater Worcester medical centers were independently validated according to predefined criteria for AMI, which included a suggestive clinical history, serum enzyme/biomarker elevations, and serial electrocardiographic findings during hospitalization.10, 11, 12, 13, 15 Patients who satisfied at least 2 of these 3 criteria, and were residents of central Massachusetts given that this study is population based, were included in this investigation. Patients who developed symptoms of AMI after hospital admission, or after an interventional procedure or surgery, were excluded as were patients with an imprecise and/or unknown time of acute symptom onset.
Data Collection
Information about patients’ demographic characteristics, medical history, prehospital treatment regimens, clinical presentation, development of acute clinical complications, and hospital discharge status was abstracted from the hospital medical records of patients with confirmed AMI by trained nurse and physician reviewers. Prehospital delay was defined as the time interval between onset of symptoms suggestive of AMI and arrival time in the emergency department.7, 16, 17 This information was collected by our trained data abstractors who reviewed any information they could find in hospital medical records and emergency medical service reports that described extent of prehospital delay from emergency personnel, nurses, and physicians notes. Information on prehospital delay was collected in minutes or hours as a continuous variable. This variable was further categorized according to cutpoints that had been commonly utilized in the published literature, based on the distribution of our data, and according to what we considered to be clinically meaningful cutpoints of prehospital delay. The delay times for patients who delayed seeking medical care by more than 24 hours after onset of their acute symptoms (n=32) were truncated at 24 hours.
Candidate variables considered as potential confounders of the association between age and extent of prehospital delay were chosen based on findings from previous studies, including study year, sex, race (white vs nonwhite), marital status, insurance status, comorbidities (eg, heart failure, diabetes), prehospital medications and interventional procedures (eg, cardiac catheterization, PCI), mode of hospital transport, day of hospital admission (weekday vs weekend), time of day (12 am–5:59 am, 6 am–11:59 am, 12 pm–5:59 pm, and 6 pm–11:59 pm), AMI order (initial vs previous), and whether the AMI was a non‐ST‐segment elevation myocardial infarction (NSTEMI) or an ST‐segment elevation myocardial infarction (STEMI).13, 18
Statistical Analysis
Differences in various baseline demographic and clinical characteristics overall, and in our 3 age strata, were examined using chi‐square tests for categorical variables and ANOVA for continuous variables. Differences in average prehospital delay times by study year, overall and in our 3 elderly age strata, were compared using analysis of variance.
Categorical data were compared between patients who delayed <2 and ≥2 hours using the chi‐square test of statistical significance. Wilcoxon sum‐rank tests were used to compare differences in selected continuous variables according to extent of delay as defined at our cutpoint of 2 hours.
Prehospital delay was missing in 57% of confirmed cases of AMI during the years under study. Using chi‐square tests and Wilcoxon sum‐rank tests, we determined significant differences in the characteristics of those missing medical record information about prehospital delay from those who had such data available. Because of the potential bias, these differences might create for our complete‐case analysis, we simultaneously employed an inverse probability weighted (IPW) analysis to weight each complete case according to the probability of nonmissing prehospital delay information.19 Weights were stabilized as the overall probability of being observed (0.43) (eg, having delay time data available) divided by the predicted probability of being observed for each person to minimize the effects of the artificial inflation of precision as a result of the increased N used in the weighted analysis.
We examined the possible association between age and extent of prehospital delay using a logistic regression model to examine the association between age with duration of prehospital delay (<2 or ≥2 hours) as well as trends over time. In both the complete‐case sample and the IPW sample analyses, a series of regression models were used to examine the association between several demographic characteristics, comorbidities, and clinical presentation with extent of prehospital delay in the total study population and in the 3 elderly age strata examined. The first regression model calculated the crude odds ratios (ORs) and 95% CIs for each of the 3 age strata examined. The second regression model controlled for patient sex, marital status, medical history of various comorbidities, receipt of past cardiac medications and cardiovascular procedures, and presenting symptoms at the time of admission to the hospital. The third regression model adjusted for additional variables, including patient hemodynamic status at time of arrival to the hospital and early complications experienced by patients within 24 hours of admission for AMI (see footnotes to each table for the list of controlling variables). This medical record review study was approved by the institutional review board at the University of Massachusetts Medical School (Worcester, MA). Consent was not required, given that no patients were directly contacted as part of this study. All data analyses were performed using SAS software (version 9.1; SAS Institute Inc., Cary, NC).
Results
During the 10‐year period under study (2001–2011), which consisted of 6 biennial study years, a total of 3593 patients 65 years and older were admitted to all 11 hospitals in central Massachusetts with a confirmed diagnosis of AMI. Of these, information regarding prehospital delay was available in the hospital medical records of 1542 patients (43%) who formed the basis of the present report. The proportion of patient medical records with sufficient documentation of information to calculate extent of prehospital delay remained relatively stable during the decade‐long period under study (45% in 2001–2003; 41% in 2009–2011).
In terms of possible differences in selected baseline characteristics between patients with and without available information in hospital medical records on the approximate time of onset of acute coronary symptoms, patients without information on duration of prehospital delay were slightly older (mean age=79.0 years [SD=7.7] vs 78.0 years [SD=7.7]) and were more likely to be female (53.2% vs 45.8%), single or widowed (45.9% vs 39.9%), have a history of heart failure (32.1% vs 20.8%) or diabetes (40.4% versus 36.6%), to have had a do‐not‐resuscitate (DNR) order in their medical records (34.6% vs 26.1%), and to have developed an NSTEMI during their index hospitalization (79.3% vs 67.1%; all P<0.05) than elderly patients with information available on extent of prehospital delay.
Study Population Characteristics
The average age of our study population in whom information about extent of prehospital delay was available was 78 years, 45.9% were women, and in 59% of patients it was their first AMI.
In examining differences in our 3 elderly patient subgroups (Table 1), patients in the oldest old‐age group (≥85 years) were more likely to be female, white, widowed, have Medicare insurance, and to have an active DNR status at the time of hospital admission; they were less likely to be obese, however, when compared with those in the youngest old‐age group (65–74 years). Patients in the oldest old‐age group were also more likely to have arrived by ambulance to greater Worcester hospitals and to have been previously diagnosed with angina, atrial fibrillation, heart failure, hypertension, and/or stroke, but were less likely to have had a history of diabetes, when compared with those in the youngest old‐age stratum. Patients in the oldest old‐age group were also less likely to be on lipid‐lowering medications or to have previously undergone cardiac interventional procedures in comparison with the youngest old‐age patients (Table 1).
Table 1.
Baseline Characteristics of Elderly Patients With Acute Myocardial Infarction Further Stratified According to Age
| Characteristic | Age, y | ||||
|---|---|---|---|---|---|
| ≥65 (n=1542) | 65 to 74 (n=549) | 75 to 84 (n=668) | ≥85 (n=325) | P Value | |
| Demographics | |||||
| Age, mean (y) | 78.0 | 69.6 | 79.8 | 88.6 | <0.001 |
| Female (%) | 45.9 | 34.1 | 48.4 | 60.6 | <0.001 |
| White (%) | 91.2 | 87.7 | 92.1 | 95.1 | <0.001 |
| Body mass index ≥30 (%) | 25.8 | 37.2 | 22.4 | 12.5 | <0.001 |
| DNR order (%) | 26.1 | 9.7 | 25.0 | 56.3 | <0.001 |
| Marital status (%) | |||||
| Single | 9.1 | 9.7 | 7.4 | 11.4 | |
| Married | 52.9 | 63.5 | 54.1 | 32.6 | |
| Divorced | 6.2 | 10.6 | 4.9 | 1.5 | <0.001 |
| Widowed | 30.8 | 15.2 | 32.9 | 52.6 | |
| Medical history (%) | |||||
| Angina | 20.8 | 18.4 | 20.7 | 25.2 | 0.019 |
| Atrial fibrillation | 18.2 | 10.0 | 20.7 | 26.8 | <0.001 |
| Diabetes | 36.6 | 41.9 | 36.5 | 28.0 | <0.001 |
| Heart failure | 28.0 | 19.5 | 29.8 | 38.8 | <0.001 |
| Hypertension | 81.8 | 79.4 | 81.9 | 85.5 | 0.025 |
| Stroke | 13.2 | 10.2 | 15.0 | 14.8 | 0.028 |
| Medication history (%) | |||||
| Aspirin | 52.9 | 50.3 | 54.0 | 55.1 | 0.137 |
| Beta‐blockers | 54.7 | 52.3 | 55.1 | 58.2 | 0.089 |
| Lipid‐lowering agents | 46.6 | 52.1 | 47.6 | 35.7 | <0.001 |
| ACE inhibitors/ARBs | 45.7 | 45.7 | 45.5 | 46.2 | 0.922 |
| Procedure history (%) | |||||
| PCI | 23.1 | 27.3 | 22.9 | 16.3 | <0.001 |
| CABG surgery | 17.2 | 18.9 | 18.0 | 12.6 | 0.025 |
| Insurance status (%) | |||||
| Medicare | 46.9 | 40.0 | 48.6 | 55.3 | <0.001 |
| HMO | 41.0 | 44.2 | 41.3 | 35.1 | |
| Medicaid | 0.9 | 1.6 | 0.8 | 0.0 | |
| Blue Cross/private insurance | 9.0 | 10.8 | 8.0 | 8.1 | |
| Private payment/other | 2.2 | 3.5 | 1.4 | 1.6 | |
| Ambulance transport (%) | 75.6 | 66.5 | 76.4 | 89.2 | <0.001 |
| Presenting symptoms (%) | |||||
| Abdominal pain | 7.3 | 5.1 | 7.9 | 9.9 | 0.007 |
| Chest pain | 82.0 | 86.7 | 81.9 | 74.2 | <0.001 |
| Diaphoresis | 34.0 | 38.3 | 32.6 | 29.5 | 0.006 |
| Fatigue | 13.9 | 13.3 | 12.9 | 17.2 | 0.157 |
| Nausea | 31.5 | 36.4 | 27.5 | 31.4 | 0.042 |
| Palpitations | 8.0 | 9.1 | 7.2 | 8.0 | 0.448 |
| Shortness of breath | 56.4 | 55.2 | 56.1 | 58.8 | 0.323 |
| Symptom onset (%) | |||||
| 12 am to 5:59 am | 26.7 | 27.2 | 24.4 | 30.3 | |
| 6 am to 11:59 am | 27.1 | 25.7 | 27.1 | 28.9 | 0.497 |
| 12 pm to 5:59 am | 20.8 | 24.2 | 20.5 | 16.6 | |
| 6 pm to 11:59 pm | 25.5 | 22.9 | 28.0 | 24.3 | |
| ER weekend visit (%) | 27.1 | 26.6 | 26.4 | 29.5 | 0.406 |
| Admission laboratory findings, mean | |||||
| Cholesterol, mg/dL | 166.0 | 168.0 | 162.5 | 169.9 | 0.087 |
| eGFR, mL/min | 53.6 | 59.0 | 52.6 | 46.7 | <0.001 |
| Glucose, mg/dL | 177.9 | 178.1 | 175.2 | 183.0 | 0.324 |
| Vital signs, mean | |||||
| Diastolic blood pressure, mm Hg | 76.5 | 79.5 | 76.7 | 70.7 | <0.001 |
| Heart rate | 86.4 | 84.2 | 86.6 | 89.7 | 0.003 |
| Systolic blood pressure, mm Hg | 144.6 | 146.0 | 144.9 | 141.5 | 0.141 |
| STEMI (%) | 32.9 | 39.3 | 32.5 | 22.8 | <0.001 |
| Early hospital complications (%) | |||||
| Atrial fibrillation | 17.0 | 11.3 | 18.0 | 24.6 | <0.001 |
| Cardiac arrest | 2.6 | 3.3 | 2.1 | 2.5 | 0.364 |
| Cardiogenic shock | 3.7 | 4.6 | 3.1 | 3.4 | 0.296 |
| Heart failure | 31.3 | 25.3 | 32.9 | 37.9 | <0.001 |
| Stroke | 0.7 | 0.6 | 0.5 | 1.2 | 0.292 |
| Ventricular fibrillation | 2.2 | 3.8 | 2.0 | 0.3 | <0.001 |
| Ventricular tachycardia | 9.4 | 10.0 | 9.0 | 9.2 | 0.642 |
| Hospital length of stay, mean (days) | 5.3 | 5.2 | 5.6 | 4.8 | 0.052 |
| Death (%) | 8.6 | 5.8 | 9.0 | 12.6 | <0.001 |
ACE indicates angiotensin‐converting enzyme; ARBs, angiotensin receptor blockers; CABG, coronary artery bypass graft; DNR, do‐not‐resuscitate; eGFR, estimated glomerular filtration rate; ER, emergency room; HMO, health maintenance organization; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
The youngest old‐age patients were more likely to have presented with more‐typical symptoms of AMI, such as chest pain, nausea, and diaphoresis, whereas the oldest old‐age patients were more likely to have presented with atypical symptoms, such as abdominal pain (Table 1). At the time of hospital admission, the oldest old‐age patients were more likely to have poorer kidney function, a higher heart rate but lower diastolic blood pressure findings, and were more likely to have presented with an NSTEMI in comparison with the youngest old‐age patients. Patients in the oldest old‐age stratum were also more likely to have experienced early clinical complications (within 24 hours of admission), including atrial fibrillation and/or heart failure, whereas the youngest old‐age patients were more likely to have developed ventricular fibrillation within 24 hours of admission. Finally, the oldest old‐age AMI patients were more likely to have died during their acute hospitalization when compared with those in the youngest old‐age stratum.
Magnitude of Prehospital Delay
During the 10‐year study period, the overall median duration of prehospital delay in our study population was 2.0 hours (mean=3.7 hours). Median durations of prehospital delay were 1.9, 2.1, and 1.9 hours in the youngest old‐age, intermediate old‐age, and oldest old‐age strata, respectively. Corresponding mean durations of delay in the 3 elderly age strata were 3.5, 4.0, and 3.4 hours, respectively (Table 2). Approximately 47% of the study population presented to all hospitals in central Massachusetts within 2 hours of acute symptom onset, an additional 37% presented between 2 and 6 hours of symptom onset, and 16% presented more than 6 hours after onset of AMI symptoms. Similar distributions of prehospital delay were noted in the 3 elderly age strata examined.
Table 2.
Magnitude of Prehospital Delay, and Distribution According to Age, in Elderly Patients Hospitalized With Acute Myocardial Infarction
| Age, y | ||||
|---|---|---|---|---|
| ≥65 | 65 to 74 | 75 to 84 | ≥85 | |
| Median, hours | 2.0 | 2.0 | 2.1 | 2.0 |
| Mean, hours (SE) | 3.7 (±0.12) | 3.5 (±0.19) | 4.0 (±0.19) | 3.4 (±0.25) |
| Distribution (%) | ||||
| <2 hours | 46.7 | 49.0 | 43.9 | 48.6 |
| 2 to 5.9 hours | 37.5 | 35.7 | 37.4 | 38.9 |
| 6 to 11.9 hours | 8.9 | 9.8 | 10.0 | 4.9 |
| 12 to 23.9 hours | 4.8 | 3.8 | 6.3 | 3.4 |
| ≥24 hours | 2.1 | 1.7 | 2.3 | 2.2 |
Among patients with an STEMI, the median and mean durations of prehospital delay were 1.9 and 3.6 hours, whereas among patients with an NSTEMI, these times were 2.1 and 3.8 hours, respectively. Among patients with an STEMI, the median durations of prehospital delay were 1.7, 2.0, and 1.8 hours in the youngest old‐age, intermediate old‐age, and oldest old‐age strata, respectively. Among patients with an NSTEMI, the median durations of prehospital delay were 2.0, 2.2, and 2.0 hours, respectively, in these 3 age groups.
Trends in Prehospital Delay
A total of 747 elderly patients were hospitalized with a confirmed AMI in 2001–2003, 466 in 2005–2007, and 329 in 2009–2011. In 2001–2003, there were 248 patients 65 to 75 years old, 316 who were 75 to 84 years old, and 183 who were 85 years and older; these numbers were 145, 219, and 102, respectively in 2005–2007 and 156, 133, and 40 in 2009–2011, respectively.
During the decade‐long period under study, median duration of prehospital delay among elderly patients hospitalized with AMI remained stable at 2.0 hours (2.0 hours in 2001–2003; 2.0 hours in 2009–2011). Among the 3 different age groups examined, median duration of prehospital delay changed marginally from 2.0, 2.2, and 2.0 hours in 2001–2003 to 1.9, 2.0, and 1.8 hours during 2009–2011 in those ages 65 to 74, 75 to 84, and ≥85 years, respectively (Figure 1). Mean duration of prehospital delay, however, decreased from 3.9 hours in 2001–2003 to 3.2 hours in 2009–2011 (P=0.08). The corresponding average durations of prehospital delay decreased from 4.0, 4.1, and 3.3 hours, respectively, in 2001–2003 to 3.2, 3.5, and 2.5 hours, respectively, in 2009–2011, among patients 65 to 74, 75 to 84, and 85 years and older (Figure 2). The proportion of elderly patients who reached the hospital within 2 hours of acute symptom onset during the years under study remained relatively stable (45.8% in 2001–2003; 48.9% in 2009–2011), with similar patterns noted when we used a 6‐hour cutpoint to denote early from late care seekers as well.
Figure 1.
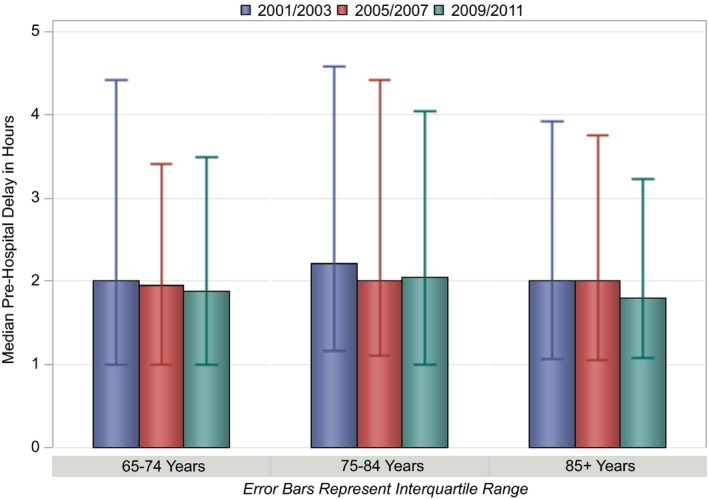
Trends in median duration of prehospital delay in elderly patients hospitalized with acute myocardial infarction according to age strata.
Figure 2.
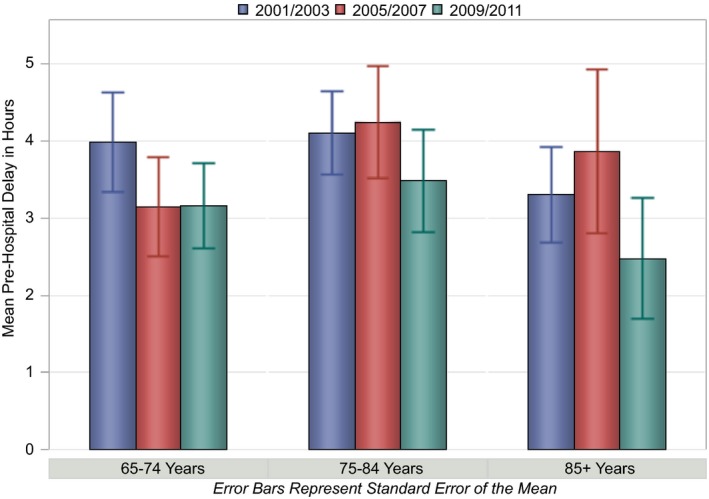
Trends in mean duration of prehospital delay in elderly patients hospitalized with acute myocardial infarction according to age strata.
A number of patient characteristics were also examined for possible changes during the decade‐long period under study (Table 3). Patients admitted during recent years were relatively younger, more likely to be male, Caucasian, married, and without an active DNR order at the time of hospital admission. Elderly patients hospitalized during the most recent study years were less likely to have had a history of angina or to have previously undergone cardiac revascularization procedures such as PCI or CABG surgery; on the other hand, these patients were more likely to have been previously prescribed several beneficial cardiac medications (aspirin, beta‐blockers, lipid‐lowering agents, and angiotensin‐converting enzyme [ACE] inhibitors/angiotensin receptor blockers [ARBs]) before their index hospitalization. They were less likely to present using the ambulance for transportation and were less likely to have symptoms such as shortness of breath, palpitations, or diaphoresis compared with those admitted during earlier study years. At the time of hospital admission, patients admitted during recent years had lower heart rate and serum cholesterol findings and poorer renal function and were less likely to have developed various clinical complications compared with elderly patients admitted during earlier study years (Table 3). Similar trends were also observed in the 3 individual age strata examined.
Table 3.
Trends in Patient Characteristics Over Time
| Characteristic | Study Year | |||
|---|---|---|---|---|
| 2001/2003 (n=747) | 2005/2007 (n=466) | 2009/2011 (n=329) | P Value | |
| Demographics | ||||
| Age, mean (y) | 78.8 | 78.5 | 75.7 | <0.001 |
| Female (%) | 47.9 | 47.9 | 38.3 | 0.008 |
| White (%) | 88.9 | 93.1 | 96.4 | 0.001 |
| Body mass index ≥30 (%) | 23.0 | 27.7 | 28.3 | 0.311 |
| DNR order (%) | 29.3 | 27.7 | 16.7 | <0.001 |
| Marital status (%) | ||||
| Single | 9.5 | 9.0 | 8.2 | |
| Married | 51.1 | 52.0 | 58.1 | |
| Divorced | 4.1 | 9.0 | 7.0 | <0.001 |
| Widowed | 35.1 | 29.5 | 23.1 | |
| Medical history (%) | ||||
| Angina | 30.3 | 16.3 | 5.8 | <0.001 |
| Atrial fibrillation | 17.8 | 18.9 | 17.9 | 0.887 |
| Diabetes | 33.9 | 38.0 | 41.0 | 0.061 |
| Heart failure | 28.1 | 29.6 | 25.5 | 0.449 |
| Hypertension | 81.1 | 82.0 | 83.0 | 0.761 |
| Stroke | 12.3 | 13.5 | 14.9 | 0.503 |
| Medication history (%) | ||||
| Aspirin | 50.2 | 53.0 | 59.0 | 0.029 |
| Beta‐blockers | 49.0 | 59.9 | 60.5 | <0.001 |
| Lipid‐lowering agents | 37.9 | 48.5 | 64.1 | <0.001 |
| ACE inhibitors/ARBs | 40.0 | 51.1 | 51.1 | <0.001 |
| Procedure history (%) | ||||
| PCI | 17.0 | 23.8 | 35.9 | <0.001 |
| CABG surgery | 14.9 | 17.0 | 22.8 | 0.006 |
| Ambulance transport (%) | 76.8 | 77.5 | 71.7 | <0.001 |
| Presenting symptoms (%) | ||||
| Abdominal pain | 7.2 | 7.3 | 7.6 | 0.976 |
| Chest pain | 80.7 | 82.2 | 84.5 | 0.328 |
| Diaphoresis | 41.4 | 34.6 | 16.4 | <0.001 |
| Fatigue | 14.7 | 12.9 | 13.7 | 0.656 |
| Nausea | 33.6 | 29.6 | 29.5 | 0.232 |
| Palpitations | 10.6 | 5.4 | 6.1 | 0.001 |
| Shortness of breath | 61.2 | 56.4 | 45.3 | <0.001 |
| ER weekend visit (%) | 28.4 | 26.0 | 25.9 | 0.551 |
| Admission laboratory findings, mean | ||||
| Cholesterol, mg/dL | 177.3 | 163.4 | 153.0 | <0.001 |
| eGFR, mL/min | 53.8 | 55.0 | 51.3 | 0.027 |
| Glucose, mg/dL | 178.3 | 181.0 | 172.5 | 0.306 |
| Vital signs, mean | ||||
| Diastolic blood pressure, mm Hg | 77.3 | 75.5 | 76.2 | 0.283 |
| Heart rate | 87.0 | 87.6 | 83.2 | 0.017 |
| Systolic blood pressure, mm Hg | 146.0 | 144.1 | 142.1 | 0.185 |
| STEMI (%) | 35.1 | 31.6 | 29.8 | 0.179 |
| Early hospital complications (%) | ||||
| Atrial fibrillation | 18.3 | 19.5 | 10.3 | 0.001 |
| Cardiac arrest | 2.8 | 2.8 | 1.8 | 0.611 |
| Cardiogenic shock | 4.0 | 4.3 | 2.1 | 0.228 |
| Heart failure | 36.1 | 29.8 | 22.2 | <0.001 |
| Stroke | 0.9 | 0.4 | 0.3 | 0.383 |
| Ventricular fibrillation | 1.7 | 3.4 | 1.8 | 0.129 |
| Ventricular tachycardia | 13.0 | 5.2 | 7.3 | <0.001 |
| Hospital length of stay, mean (days) | 5.9 | 4.9 | 4.7 | <0.001 |
| Death (%) | 9.9 | 8.4 | 6.1 | 0.116 |
ACE indicates angiotensin‐converting enzyme; ARBs, angiotensin receptor blockers; CABG, coronary artery bypass graft; DNR, do‐not‐resuscitate; eGFR, estimated glomerular filtration rate; ER, emergency room; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
After controlling for a number of potentially confounding factors in a multivariable adjusted logistic regression model, as well as in a multivariable adjusted IPW logistic regression model (Table 4), there were no significant trends observed during the years under study in the proportion of patients who presented to all central Massachusetts medical centers during the first 2 hours of AMI‐related symptoms. We also reran similar multivariable adjusted models using an ordinal year variable and did not find any of the trends observed to be statistically significant.
Table 4.
Crude and Multivariable Adjusted Odds Ratios of Prehospital Delay Greater Than 2 Hours Among Elderly Patients Hospitalized With Acute Myocardial Infarction With Complete‐Case Analysis and IPW Analysis
| Age, y | ||||||||
|---|---|---|---|---|---|---|---|---|
| ≥65 | 65 to 74 | 75 to 84 | ≥85 | |||||
| 2005/2007 (n=466) | 2009/2011 (n=329) | 2005/2007 (n=145) | 2009/2011 (n=156) | 2005/2007 (n=219) | 2009/2011 (n=133) | 2005/2007 (n=102) | 2009/2011 (n=40) | |
| Model 1 | ||||||||
| Complete case | 0.97 (0.77, 1.22)a | 0.88 (0.68, 1.14)a | 0.83 (0.55, 1.25) | 0.82 (0.55, 1.23) | 0.98 (0.69, 1.39) | 0.93 (0.62, 1.40) | 1.13 (0.70, 1.84) | 0.88 (0.44, 1.74) |
| IPW | 0.98 (0.78, 1.23) | 0.81 (0.63, 1.05) | 0.88 (0.57, 1.35) | 0.76 (0.50, 1.14) | 0.91 (0.65, 1.29) | 0.91 (0.62, 1.35) | 1.23 (0.77, 1.95) | 0.64 (0.34, 1.19) |
| Model 2 | ||||||||
| Complete case | 0.94 (0.74, 1.19) | 0.80 (0.61, 1.07) | 0.84 (0.55, 1.27) | 0.78 (0.50, 1.20) | 0.95 (0.66, 1.36) | 0.80 (0.51, 1.25) | 0.98 (0.58, 1.64) | 0.75 (0.35, 1.63) |
| IPW | 0.93 (0.74, 1.19) | 0.73 (0.55, 0.96) | 0.86 (0.55, 1.34) | 0.71 (0.45, 1.11) | 0.90 (0.62, 1.29) | 0.78 (0.51, 1.21) | 1.15 (0.69, 1.91) | 0.54 (0.26, 1.11) |
| Model 3 | ||||||||
| Complete case | 0.94 (0.73, 1.19) | 0.82 (0.62, 1.10) | 0.85 (0.55, 1.32) | 0.70 (0.45, 1.11) | 0.91 (0.63, 1.32) | 0.80 (0.53, 1.35) | 1.05 (0.61, 1.79) | 0.79 (0.35, 1.79) |
| IPW | 0.93 (0.73, 1.19) | 0.74 (0.56, 0.99) | 0.86 (0.54, 1.37) | 0.63 (0.39, 1.00) | 0.86 (0.59, 1.25) | 0.84 (0.53, 1.32) | 1.24 (0.73, 2.12) | 0.60 (0.28, 1.27) |
Referent period=2001–2003. Model 1: Crude odds ratio. Model 2: Adjusted for sex, marital status, medical history, past cardiac medications and procedures, and acute presenting symptoms. Model 3: Adjusted for sex, marital status, medical history, past cardiac medications and procedures, acute presenting symptoms, vital signs, and early hospital complications.
IPW indicates inverse probability weighted.
95% CIs.
Similarly, there were no significant changes observed in the care‐seeking behavior of each of our elderly subgroups of different ages after adjusting for multiple factors possibly associated with patient care‐seeking behavior (Table 4).
Patient Characteristics Associated With Duration of Prehospital Delay
In examining possible differences in the characteristics of patients who presented to all hospitals in central Massachusetts early after onset of acute symptoms (within 2 hours) as compared with those who presented at a later time (greater than 2 hours) to the hospital, patients who presented at a later time were more likely to have initially experienced their acute symptoms between 6 pm and 5:59 am and were more likely to have presented to the hospital with atypical symptoms, such as abdominal pain and/or palpitations, when compared with those who presented at an earlier time (Table 5). Patients who sought care earlier were more likely to have been diagnosed with an STEMI and were more likely to have developed early in‐hospital complications compared with those who presented at a later time (Table 5).
Table 5.
Patient Characteristics According to Extent of Prehospital Delay
| Characteristic | Age, y | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≥65 | 65 to 74 | 75 to 84 | ≥85 | |||||||||
| Delay, Hours | <2 (n=720) | ≥2 (n=822) | P Value | <2 (n=269) | ≥2 (n=280) | P Value | <2 (n=293) | ≥2 (n=375) | P Value | <2 (n=158) | ≥2 (n=167) | P Value |
| Demographics | ||||||||||||
| Age, mean (y) | 77.9 | 78.1 | 0.74 | 69.5 | 69.6 | 0.61 | 79.7 | 79.8 | 0.74 | 89.0 | 88.3 | 0.07 |
| Female (%) | 45.0 | 46.6 | 0.53 | 31.6 | 36.4 | 0.23 | 49.8 | 47.2 | 0.50 | 58.9 | 62.3 | 0.53 |
| White (%) | 91.9 | 90.7 | 0.43 | 89.1 | 86.4 | 0.38 | 92.0 | 92.1 | 0.97 | 96.0 | 94.2 | 0.49 |
| Body mass index ≥30 (%) | 25.3 | 26.2 | 0.43 | 37.6 | 36.7 | 0.93 | 20.8 | 23.6 | 0.23 | 10.7 | 14.0 | 0.70 |
| DNR order (%) | 25.4 | 26.8 | 0.54 | 8.2 | 11.1 | 0.25 | 22.5 | 26.9 | 0.19 | 60.1 | 52.7 | 0.18 |
| Marital status (%) | ||||||||||||
| Single | 9.7 | 8.6 | 10.5 | 9.0 | 7.3 | 7.5 | 12.7 | 10.2 | ||||
| Married | 52.7 | 53.1 | 0.40 | 62.3 | 64.6 | 0.60 | 54.5 | 53.8 | 0.52 | 32.9 | 32.3 | 0.25 |
| Divorced | 7.3 | 5.3 | 11.2 | 10.1 | 6.3 | 3.8 | 2.5 | 0.6 | ||||
| Widowed | 29.3 | 32.1 | 14.6 | 15.9 | 30.9 | 34.4 | 51.3 | 53.9 | ||||
| Medical history (%) | ||||||||||||
| Angina | 22.8 | 19.1 | 0.08 | 21.6 | 15.4 | 0.06 | 20.8 | 20.5 | 0.93 | 28.5 | 22.2 | 0.19 |
| Atrial fibrillation | 18.3 | 18.0 | 0.87 | 10.0 | 10.0 | 0.99 | 22.2 | 19.5 | 0.39 | 25.3 | 28.1 | 0.56 |
| Diabetes | 36.0 | 37.2 | 0.61 | 36.8 | 46.8 | <0.05 | 38.9 | 34.7 | 0.26 | 29.1 | 27.0 | 0.66 |
| Heart failure | 28.2 | 27.9 | 0.88 | 16.0 | 22.9 | <0.05 | 32.4 | 27.7 | 0.19 | 41.1 | 36.5 | 0.39 |
| Hypertension | 82.5 | 81.1 | 0.49 | 80.7 | 78.2 | 0.48 | 82.6 | 81.3 | 0.67 | 85.4 | 85.6 | 0.96 |
| Stroke | 13.5 | 13.0 | 0.79 | 7.1 | 13.2 | <0.05 | 16.7 | 13.6 | 0.26 | 18.4 | 11.4 | 0.08 |
| Insurance status (%) | ||||||||||||
| Medicare | 49.4 | 44.8 | 0.32 | 39.9 | 40.0 | 0.32 | 54.1 | 44.4 | 0.12 | 56.7 | 53.9 | 0.95 |
| HMO | 38.2 | 43.5 | 41.0 | 47.1 | 37.7 | 44.1 | 34.2 | 35.9 | ||||
| Medicaid | 1.0 | 0.9 | 2.2 | 1.1 | 0.3 | 1.1 | 0 | 0 | ||||
| Blue Cross/private insurance | 9.1 | 8.9 | 12.7 | 8.9 | 6.5 | 9.1 | 7.7 | 8.4 | ||||
| Private payment/other | 2.4 | 2.0 | 4.1 | 2.9 | 1.4 | 1.3 | 1.3 | 1.8 | ||||
| Ambulance transportation (%) | 78.1 | 74.0 | 0.31 | 68.3 | 65.0 | 0.45 | 80.2 | 73.3 | <0.05 | 89.2 | 89.2 | 1.0 |
| Type of AMI (%) | ||||||||||||
| NSTEMI | 63.6 | 70.2 | <0.01 | 55.0 | 66.1 | <0.01 | 65.5 | 69.1 | 0.33 | 74.7 | 79.6 | 0.28 |
| Presenting symptoms (%) | ||||||||||||
| Abdominal pain | 6.0 | 8.5 | 0.05 | 4.1 | 6.1 | 0.29 | 6.5 | 9.1 | 0.22 | 8.2 | 11.4 | 0.34 |
| Chest pain | 80.7 | 83.1 | 0.22 | 85.9 | 87.5 | 0.57 | 80.9 | 82.7 | 0.55 | 71.5 | 76.7 | 0.29 |
| Diaphoresis | 35.7 | 32.5 | 0.18 | 41.3 | 35.4 | 0.15 | 34.1 | 31.5 | 0.46 | 29.1 | 29.9 | 0.87 |
| Fatigue | 12.8 | 15.0 | 0.22 | 13.4 | 13.2 | 0.95 | 8.9 | 16.0 | <0.01 | 19.0 | 15.6 | 0.41 |
| Nausea | 30.0 | 32.9 | 0.23 | 35.7 | 37.1 | 0.72 | 25.9 | 28.8 | 0.41 | 27.9 | 34.7 | 0.18 |
| Palpitations | 6.5 | 9.4 | <0.05 | 8.2 | 10.0 | 0.46 | 5.8 | 8.3 | 0.22 | 5.1 | 10.8 | 0.05 |
| Shortness of breath | 55.1 | 57.4 | 0.37 | 57.9 | 52.4 | 0.2 | 55.0 | 57.1 | 0.58 | 60.1 | 57.5 | 0.63 |
| Medication and procedure history (%) | ||||||||||||
| Aspirin | 52.6 | 53.2 | 0.84 | 49.4 | 51.1 | 0.70 | 52.6 | 55.2 | 0.50 | 58.2 | 52.1 | 0.27 |
| Beta‐blockers | 52.8 | 56.5 | 0.15 | 53.5 | 51.1 | 0.56 | 52.2 | 57.3 | 0.19 | 52.5 | 63.5 | <0.05 |
| Lipid‐lowering agents | 46.1 | 47.2 | 0.67 | 52.8 | 51.4 | 0.75 | 47.4 | 47.7 | 0.94 | 32.3 | 38.9 | 0.21 |
| ACE inhibitors/ARBs | 46.3 | 45.3 | 0.70 | 45.7 | 45.7 | 1.0 | 47.4 | 44.0 | 0.38 | 44.9 | 47.3 | 0.67 |
| PCI | 22.8 | 23.4 | 0.79 | 28.3 | 26.4 | 0.63 | 21.5 | 24.0 | 0.45 | 15.8 | 16.8 | 0.82 |
| CABG surgery | 15.8 | 18.4 | 0.19 | 16.4 | 21.4 | 0.13 | 17.1 | 18.7 | 0.59 | 12.7 | 12.6 | 0.98 |
| Acute symptom onset (%) | ||||||||||||
| 12 am to 6 am | 25.3 | 28.0 | 24.9 | 29.4 | 22.4 | 26.0 | 30.7 | 29.9 | ||||
| 6 am to 12 pm | 30.1 | 24.4 | 28.0 | 23.5 | 29.7 | 25.0 | 33.6 | 24.5 | ||||
| 12 pm to 6 pm | 22.0 | 19.7 | 25.9 | 22.6 | 22.8 | 18.7 | 15.3 | 17.7 | ||||
| 6 pm to 12 am | 22.6 | 28.0 | <0.05 | 21.2 | 24.5 | 0.48 | 25.0 | 30.3 | 0.24 | 20.4 | 27.9 | 0.27 |
| ER weekend visit (%) | 27.6 | 26.6 | 0.66 | 27.5 | 25.7 | 0.63 | 27.2 | 25.3 | 0.57 | 32.3 | 27.0 | 0.29 |
| Hospital vital signs, mean | ||||||||||||
| Diastolic blood pressure, mm Hg | 76.3 | 76.7 | 0.69 | 79.9 | 79.2 | 0.68 | 75.9 | 77.4 | 0.33 | 70.7 | 70.8 | 0.96 |
| Heart rate, bpm | 86.4 | 86.3 | 0.91 | 83.5 | 84.8 | 0.47 | 86.2 | 86.9 | 0.72 | 92.0 | 87.5 | 0.09 |
| Systolic blood pressure, mm Hg | 143.2 | 145.8 | 0.12 | 146.0 | 146.1 | 0.97 | 142.8 | 146.5 | 0.14 | 139.2 | 143.7 | 0.22 |
| Admission laboratory findings, mean | ||||||||||||
| Cholesterol | 164.6 | 167.3 | 0.34 | 168.0 | 168.0 | 0.98 | 160.1 | 164.3 | 0.32 | 166.2 | 173.4 | 0.31 |
| eGFR | 53.5 | 53.7 | 0.84 | 60.6 | 57.5 | 0.07 | 50.4 | 54.4 | <0.01 | 47.5 | 45.9 | 0.44 |
| Glucose | 176.6 | 179.0 | 0.55 | 175.1 | 180.9 | 0.40 | 176.4 | 174.2 | 0.70 | 179.5 | 186.4 | 0.43 |
| STEMI (%) | 36.4 | 29.8 | <0.01 | 45.0 | 33.9 | <0.01 | 34.5 | 30.9 | 0.33 | 25.3 | 20.4 | 0.29 |
| Early hospital complications | ||||||||||||
| Atrial fibrillation | 16.0 | 17.9 | 0.32 | 11.2 | 11.4 | 0.92 | 17.8 | 18.1 | 0.90 | 20.9 | 28.1 | 0.13 |
| Cardiac arrest | 3.6 | 1.7 | 0.01 | 4.1 | 2.5 | 0.29 | 3.8 | 0.8 | <0.01 | 2.5 | 2.4 | 0.94 |
| Cardiogenic shock | 5.4 | 2.2 | <0.01 | 6.3 | 2.9 | 0.05 | 4.4 | 2.1 | 0.09 | 5.7 | 1.2 | <0.05 |
| Heart failure | 28.9 | 33.3 | 0.06 | 21.9 | 28.6 | 0.07 | 32.1 | 33.6 | 0.68 | 34.8 | 40.7 | 0.27 |
| Stroke | 0.6 | 0.7 | 0.67 | 0.7 | 0.4 | 0.54 | 0.7 | 0.3 | 0.43 | 0.0 | 2.4 | <0.05 |
| Ventricular fibrillation | 2.6 | 2.0 | 0.36 | 4.5 | 3.2 | 0.45 | 2.4 | 1.6 | 0.47 | 0.0 | 0.6 | 0.25 |
| Death (%) | 8.8 | 8.5 | 0.87 | 4.8 | 6.8 | 0.33 | 9.9 | 8.3 | 0.47 | 13.3 | 12.0 | 0.72 |
| Hospital length of stay, mean (days) | 5.5 | 5.2 | 0.28 | 5.4 | 5.1 | 0.30 | 5.9 | 5.5 | 0.35 | 4.8 | 4.9 | 0.84 |
ACE indicates angiotensin‐converting enzyme; AMI, acute myocardial infarction; ARBs, angiotensin receptor blockers; CABG, coronary artery bypass graft; DNR, do‐not‐resuscitate; eGFR, estimated glomerular filtration rate; ER, emergency room; HMO, health maintenance organization; NSTEMI, non‐ST‐elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
In examining possible differences in selected characteristics between patients who sought medical care soon after onset of acute symptoms versus those who sought care at a later time in each of the 3 age strata examined (Table 5), the youngest old‐age patients who delayed more than 2 hours after acute symptom onset were more likely to have had a history of previously diagnosed heart failure, stroke, and/or diabetes and to have developed an NSTEMI compared with those who presented at an earlier time; on the other hand, these patients were less likely to have developed early cardiogenic shock during their index hospitalization. Similarly, patients in the intermediate old‐age group who delayed more than 2 hours after acute symptom onset were more likely to have presented with atypical symptoms, such as fatigue, and were less likely to have arrived at participating medical centers by ambulance. These patients had better renal function and were less likely to have developed in‐hospital cardiac arrest than those who presented earlier. Finally, patients in the oldest old‐age stratum who presented to the hospital 2 or more hours after onset of acute coronary symptoms were more likely to have presented with atypical symptoms, to have previously been on beta‐blocker medications, and were more likely to have developed an acute stroke, but less likely to have developed cardiogenic shock, as an early complication during hospitalization for AMI when compared with those who presented earlier for hospital care. Appropriate caution needs to be exercised, however, in the interpretation of these findings given the multiplicity of comparisons carried out.
Discussion
The results of this population‐based observational study showed that the median as well as distribution of prehospital delay patterns in elderly patients who were hospitalized for an AMI at all medical centers in central Massachusetts were substantial and failed to improve during the decade long period under study (2001–2011). The relatively few factors associated with prolonged delay in this patient population included onset of acute symptoms between 6 pm and 5:59 am, presence of previously diagnosed multiple comorbidities, hospital presentation with atypical symptoms of AMI, and diagnosis of an NSTEMI.
Magnitude of Prehospital Delay in the Elderly
Although the majority of studies that have examined extent of prehospital delay among patients presenting with AMI in the United States have found median delays of ≈2 to 3 hours7, 8, 17, 20, 21, 22, 23 with most of these studies showing higher delay times in elderly than in younger patients,8, 24 few studies have examined the magnitude of, and factors associated with, prolonged delay in seeking medical care after onset of acute coronary symptoms in elderly patients presenting with AMI.9 Furthermore, we were unable to find any published studies that examined the extent of prehospital delay within different age strata of elderly patients hospitalized with an AMI. Many studies have, however, included varying proportions of elderly patients in their study population and observed median prehospital delays ranging from 2.2 to 2.8 hours in these patients.7, 8, 9, 25
Whereas the overall median duration of prehospital delay of 2 hours, and mean of 3.7 hours, observed in our study were comparable with observations from several previous studies on elderly patients in the community setting,7, 8, 9 they were generally lower in comparison with the findings from several international studies, where average delay times in the setting of AMI have ranged from 1.6 to 42.4 hours and median delays have ranged from 1.7 to 8 hours.22, 26, 27 However, mean and median delay times observed among elderly patients in our study were notably longer compared with elderly patients enrolled in clinical trials of fibrinolytic agents, where patients 75 years and older were typically excluded and patients also had to satisfy additional inclusion criteria.28 Our finding that nearly half of elderly patients who presented to all 11 central Massachusetts medical centers during the years under study within 2 hours of acute symptom onset was also comparable with the findings from other studies carried out in the United States.22, 24, 25
These collective findings suggest that the extent of prehospital delay observed in our patient population was comparable to several past studies in the United States and other countries, although it was notably better than that observed in many European and Asian countries. It is not clear, however, whether this is attributed to differences in health literacy or knowledge, type and extent of health insurance coverage, behavioral factors, severity of acute symptoms, access to care, and/or attributed to other sociodemographic characteristics and health care system–associated factors in various countries.
Irrespective of the underlying reasons, it is clear that a large proportion of elderly patients experiencing signs and symptoms of AMI delay seeking acute medical care in a timely manner. We also failed to find any appreciable differences in the care‐seeking behavior of patients who developed an STEMI as compared with those who developed an NSTEMI during the years under investigation. These findings reinforce the importance of monitoring contemporary trends in the care‐seeking behavior of these high‐risk patients and for the development of educational intervention strategies to better inform and encourage the public to seek care in a timely manner should they be experiencing signs or symptoms of a possible AMI. Moreover, several large‐scale and multidisciplinary community‐based campaigns, including the Rapid Early Action for Coronary Treatment trial,29 which were designed to reduce delay in seeking medical care among patients with signs and symptoms of acute coronary disease, have been largely unsuccessful, highlighting the complexities involved in addressing the problem of prehospital delay, especially in the elderly.
Decade Long Trends in Prehospital Delay
Our earlier studies, which examined trends in prehospital delay in patients admitted for AMI, irrespective of age, to all central Massachusetts medical centers between 1986 and 2005, failed to observe any significant changes in the extent of prehospital delay during the years under study, remaining relatively constant at a median of 2.0 hours.7, 17 The present study also found that the median duration of prehospital delay among elderly patients experiencing an AMI between 2001 and 2011 had not changed, although there was a suggestion of some decline in average delay times in patients hospitalized during the most recent years under study, especially among those in the oldest old‐age stratum. These findings suggest that the extent of prehospital delay may have plateaued during the years under study, at least in this large Northeast community of elderly patients presenting with AMI, and require verification in other US communities for better characterization of this important clinical and public health problem at a national level.
Patient Characteristics Associated With Prolonged Prehospital Delay
Investigators and clinicians have previously ascribed the observation of prolonged care‐seeking behavior in the elderly to the presence of atypical symptoms, which could cause difficulties in early recognition by both patients and their caregivers. Furthermore, relatively diminished chest pain sensation in the elderly, relatively high frequency of cognitive impairment, presence of multiple cardiovascular and noncardiovascular comorbidities, and social situations of the elderly further challenge their ability to seek care earlier.8, 24
Findings from the multinational Global Registry of Acute Coronary Events (GRACE) study had previously demonstrated that advanced age, presence of various comorbidities, failure to use an ambulance for acute care transportation, and absence of more‐typical AMI‐associated symptoms were associated with delays in seeking medical care in a timely manner.23 Smaller retrospective studies, such as the Minnesota Clinical Comparison and Assessment Program performed in the early 1990s, found that AMI patients who were at higher risk for delay in seeking acute medical care were the elderly, women, those with a history of hypertension, and those who presented in the evening or early morning hours.24
In our large, observational study of 1542 elderly patients, a limited number of sociodemographic and clinical factors were related to extent of prehospital delay.9 In univariate analyses, elderly patients experiencing atypical symptoms, symptoms during the late evening and early morning hours, and those who were eventually diagnosed with an NSTEMI were more likely to have delayed seeking timely medical care than respective comparison groups. Patients who experienced significant cardiac complications, such as cardiogenic shock and cardiac arrest, who were presumably more sick, were more likely to seek care early.
The use of emergency medical services (EMS) transport has been associated with declines in treatment delays30; however, between 40% and 80% of patients with signs and symptoms of an acute coronary event do not use EMS, with especially lower rates of usage observed in minority populations.30, 31, 32
Our previous article on community trends in utilization of EMS by residents of the Worcester metropolitan area who were hospitalized for AMI (not limited to the elderly) had observed encouraging increases in utilization of EMS over time,33 but there were differences in demographic and clinical characteristics of patients transported by ambulance versus those who did not activate the emergency transport system. In the current study, ambulance usage appeared to decline in the elderly over time, but did not demonstrate any consistent patterns in the 3 age strata examined.
Changes in the EMS preactivation infrastructure, and protocols employed in the community and their accompanying impact on prehospital delay times, especially among the elderly, remain unclear. A secondary analysis in our study also demonstrated a general, albeit nonsignificant, tendency for reduced delay times among elderly patients who were transported by ambulance during recent study years, suggesting the potentially positive impact of changes made in EMS transport protocols over time.
It is unclear why duration of prehospital delay has not changed during the decade‐long period under study, although several reasons could be postulated. Previous attempts at altering the care‐seeking behavior of patients experiencing signs and symptoms of acute coronary disease have been less than successful,29, 34, 35 despite being based on sound behavior modification principles. These and related findings suggest the need for better understanding of the psychosocial, contextual, and other personal variables, which are often given lesser importance in structuring intervention programs to enhance patient's critical care‐seeking behavior. The lack of appreciable improvement over time in the use of ambulance services by several high‐risk groups, including the elderly, and the role of changing sociodemographic and risk profiles in influencing the magnitude of prehospital delay, should also be examined further. Given the magnitude of prehospital delay in the setting of AMI among elderly patients, and the high morbidity and mortality experienced by these patients, there remains an important need for further in‐depth qualitative and quantitative studies to identify the reasons leading to prolonged care‐seeking behavior in these patients and identification of potentially modifiable barriers before devising and implementing more‐effective and targeted interventions in the future.
Study Strengths and Limitations
The strengths of the present study include the use of a population‐based design and the inclusion of elderly patients who were admitted to all 11 hospitals in central Massachusetts with a validated AMI during the years under study, thus offering a “real‐world” perspective to the problem of prehospital delay in the elderly. Furthermore, we studied different age groups of elderly patients hospitalized with AMI.
There are, however, several limitations of the present investigation that need to be considered in interpreting our findings. Our observational study included both patients with their first admission for AMI as well as those with recurrent admission for AMI, thus suggesting the possibility of a few patients being included more than once in this study. We only examined the patterns of care‐seeking behavior of elderly patients who presented to the hospital and were unable to study patients with AMI who died before hospital presentation. Additionally, whereas more than half of elderly patients with AMI did not have adequate documentation available in their hospital medical records about duration of prehospital delay, we observed similar factors to be associated with extent of prehospital delay in our different regression modeling approaches. Improved measures need to be taken for better documentation of time of acute symptom onset, which would not only help in guiding in‐hospital management, but also for future epidemiological studies examining the problem of prehospital delay. This is a difficult construct to measure and systematically record in hospital charts and is subject to potential problems with patient recall and information bias. We did not have information available about other factors that may be associated with patient care‐seeking behavior, including their socioeconomic status, distance from the hospital, and psychosocial factors, including their knowledge of the signs and symptoms of acute coronary disease and their cognition. Finally, because of the exploratory nature of this descriptive observational study, appropriate caveats need to be exercised in the interpretation of the present findings given that a large number of individual hypothesis tests were performed and multiple testing on the same data set could have resulted in an inflation of the type 1 error rate. Adjustment for multiple testing was beyond the scope of this investigation and caution needs to be exercised by the reader in interpreting the results of tests with nominal significance. Further studies in different population settings are needed to validate a number of the findings observed in the present study.
Conclusions
The results of this decade‐long observational study suggest that prolonged delay in seeking care after onset of AMI symptoms continues to be a vexing problem among the elderly, with no evidence for improving trends noted during the years under study.
Significant advances have been made in the management of AMI in the elderly in recent years, but the full benefits of these coronary reperfusion and revascularization procedures can only be achieved if the extent of prehospital delay is minimized as well. Further efforts need to be taken to better understand the reasons and situational factors responsible for delays in the seeking of timely acute medical care in the elderly, and in the identification of high risk groups that are particularly vulnerable for delay, before initiating more broad‐based and coordinated systems‐based strategies and educational interventions for improving patients’ acute care‐seeking behavior among those with signs and symptoms of AMI.
Sources of Funding
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434 and R56 HL035434). Partial salary support for Drs Gore and Goldberg was provided for by National Institutes of Health grant 1U01HL105268‐01.
Disclosures
None.
Acknowledgments
We are indebted to the physicians and nurses who have worked on the Worcester Heart Attack Study for the past several decades.
(J Am Heart Assoc. 2016;5:e002664 doi: 10.1161/JAHA.115.002664)
References
- 1. Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. [DOI] [PubMed] [Google Scholar]
- 2. Desai MM, Zhang P, Hennessy CH. Surveillance for morbidity and mortality among older adults–United States, 1995–1996. MMWR CDC Surveill Summ. 1999;48:7–25. [PubMed] [Google Scholar]
- 3. Barakat K, Wilkinson P, Deaner A, Fluck D, Ranjadayalan K, Timmis A. How should age affect management of acute myocardial infarction? A prospective cohort study Lancet. 1999;353:955–959. [DOI] [PubMed] [Google Scholar]
- 4. Mehta RH, Rathore SS, Radford MJ, Wang Y, Wang Y, Krumholz HM. Acute myocardial infarction in the elderly: differences by age. J Am Coll Cardiol. 2001;38:736–741. [DOI] [PubMed] [Google Scholar]
- 5. Rathore SS, Mehta RH, Wang Y, Radford MJ, Krumholz HM. Effects of age on the quality of care provided to older patients with acute myocardial infarction. Am J Med. 2003;114:307–315. [DOI] [PubMed] [Google Scholar]
- 6. Carro A, Kaski JC. Myocardial infarction in the elderly. Aging Dis. 2011;2:116–137. [PMC free article] [PubMed] [Google Scholar]
- 7. Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FA, Goldberg RJ. Age and sex differences and 20‐year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3:590–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3:82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sheifer SE, Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Breall JA, Schulman KA. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102:1651–1656. [DOI] [PubMed] [Google Scholar]
- 10. Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 11. Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): the Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. [DOI] [PubMed] [Google Scholar]
- 12. Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two‐decades (1975 to 1995) long experience in the incidence, in‐hospital and long‐term case‐fatality rates of acute myocardial infarction: a community‐wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. [DOI] [PubMed] [Google Scholar]
- 13. Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30‐year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cardiac Study Hospital Sites. Available at: http://www.massdac.org/index.php/public-outreach/cardiac-study-hospital-sites/. Accessed January 27, 2016.
- 15. Tunstall‐Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary‐event rates to changes in coronary heart disease mortality: 10‐year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353:1547–1557. [DOI] [PubMed] [Google Scholar]
- 16. Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade‐long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. [DOI] [PubMed] [Google Scholar]
- 17. Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Goldberg RJ. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study). Am J Cardiol. 2008;102:1589–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horvitz D. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc. 1952;47:663–685. [Google Scholar]
- 20. Dracup K, Moser DK. Treatment‐seeking behavior among those with signs and symptoms of acute myocardial infarction. Heart Lung. 1991;20(5 Pt 2):570–575. [PubMed] [Google Scholar]
- 21. Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med. 1995;40:379–392. [DOI] [PubMed] [Google Scholar]
- 22. Ho MT. Delays in the treatment of acute myocardial infarction: an overview. Heart Lung. 1991;20(5 Pt 2):566–570. [PubMed] [Google Scholar]
- 23. Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry). Am J Cardiol. 2002;89:791–796. [DOI] [PubMed] [Google Scholar]
- 24. Gurwitz JH, McLaughlin TJ, Willison DJ, Guadagnoli E, Hauptman PJ, Gao X, Soumerai SB. Delayed hospital presentation in patients who have had acute myocardial infarction. Ann Intern Med. 1997;126:593–599. [DOI] [PubMed] [Google Scholar]
- 25. Ridker PM, Manson JE, Goldhaber SZ, Hennekens CH, Buring JE. Comparison of delay times to hospital presentation for physicians and nonphysicians with acute myocardial infarction. Am J Cardiol. 1992;70:10–13. [DOI] [PubMed] [Google Scholar]
- 26. Gartner C, Walz L, Bauernschmitt E, Ladwig KH. The causes of prehospital delay in myocardial infarction. Dtsch Arztebl Int. 2008;105:286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ottesen MM, Kober L, Jorgensen S, Torp‐Pedersen C. Determinants of delay between symptoms and hospital admission in 5978 patients with acute myocardial infarction. The TRACE Study Group. Trandolapril Cardiac Evaluation. Eur Heart J. 1996;17:429–437. [DOI] [PubMed] [Google Scholar]
- 28. White HD, Barbash GI, Califf RM, Simes RJ, Granger CB, Weaver WD, Kleiman NS, Aylward PE, Gore JM, Vahanian A, Lee KL, Ross AM, Topol EJ. Age and outcome with contemporary thrombolytic therapy. Results from the GUSTO‐I trial. Global Utilization of Streptokinase and TPA for Occluded coronary arteries trial. Circulation. 1996;94:1826–1833. [DOI] [PubMed] [Google Scholar]
- 29. Luepker RV, Raczynski JM, Osganian S, Goldberg RJ, Finnegan JR Jr, Hedges JR, Goff DC Jr, Eisenberg MS, Zapka JG, Feldman HA, Labarthe DR, McGovern PG, Cornell CE, Proschan MA, Simons‐Morton DG. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: the Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;284:60–67. [DOI] [PubMed] [Google Scholar]
- 30. Mathews R, Peterson ED, Li S, Roe MT, Glickman SW, Wiviott SD, Saucedo JF, Antman EM, Jacobs AK, Wang TY. Use of emergency medical service transport among patients with ST‐segment‐elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry‐Get With The Guidelines. Circulation. 2011;124:154–163. [DOI] [PubMed] [Google Scholar]
- 31. McGinn AP, Rosamond WD, Goff DC Jr, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987‐2000. Am Heart J. 2005;150:392–400. [DOI] [PubMed] [Google Scholar]
- 32. Henderson SO, Magana RN, Korn CS, Genna T, Bretsky PM. Delayed presentation for care during acute myocardial infarction in a Hispanic population of Los Angeles County. Ethn Dis. 2002;12:38–44. [PubMed] [Google Scholar]
- 33. Goldberg RJ, Lamusta J, Darling C, DeWolf M, Saczynski JS, Lessard D, Ward J, Gore JM. Community trends in the use and characteristics of persons with acute myocardial infarction who are transported by emergency medical services. Heart Lung. 2012;41:323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dracup K, McKinley S, Riegel B, Moser DK, Meischke H, Doering LV, Davidson P, Paul SM, Baker H, Pelter M. A randomized clinical trial to reduce patient prehospital delay to treatment in acute coronary syndrome. Circ Cardiovasc Qual Outcomes. 2009;2:524–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kainth A, Hewitt A, Sowden A, Duffy S, Pattenden J, Lewin R, Watt I, Thompson D. Systematic review of interventions to reduce delay in patients with suspected heart attack. Emerg Med J. 2004;21:506–508. [DOI] [PMC free article] [PubMed] [Google Scholar]


