Abstract
Backgrounds and Aim:
Cancer process is a traumatic period for both patients and their caregivers. Caregivers of the patients use various coping methods to minimize the effects of anxiety-creating negativities in their daily lives. The present study aimed to examine the coping attitudes adopted by the patients and caregivers and the effects of this process upon the quality of life (QoL) of caregivers.
Methods:
The cross-sectional study was conducted on three groups of (i) 74 patients consisting of those hospitalized in the department of medical oncology in tertiary care hospital or coming to the health center for chemotherapy treatment as cancer outpatients and (ii) 46 caregivers of patients; and control group 46 healthy individuals. Face-to-face interviews were conducted with the study patients to administer a short sociodemographic questionnaire, coping attitudes assessment scale (COPE), and Short Form-36 (SF-36) QoL scale.
Results:
Statistically significant differences were recorded among patients, caregivers, and control groups in terms of “problem-focused coping” and “dysfunctional coping” the COPE scale (P = 0.001, P = 0.017). According to scores taken from the SF-36 scale, there was a statistically significant difference between caregivers and control groups in all parameters (P < 0.05).
Conclusion:
Patients and caregivers should be encouraged to use the coping methods related to the source of the problem rather than the dysfunctional coping methods. Evaluation of the QoL indicators of not only the patients but also their caregivers enables to formulate a more integrated approach and detection of the expectations of the caregivers.
Keywords: Cancer patients, Caregivers, Coping attitudes, Quality of life
INTRODUCTION
Cancer is a severe health problem with high mortality rate unless diagnosed and treated at early phases. Cancer constitutes 25% of the mortality and ranks second after the ischemic heart disease, particularly in the developed countries.[1] Cancer is not personal experience; rather, it is a concomitant health process caregivers.[2] Responsibilities of caregiving bring about complicated physical and psychological support, the economic burden, decision-making skill, and care coordination.[3,4]
As seen all chronic diseases, the cancer process is a stressful period for both patients and their caregivers. In this regard, it is unavoidable to use some coping methods to minimize and eliminate the negative effects of the anxiety-creating problems. In definition, “coping” refers to the resistance shown by the individual against the stressing events or factors and the sum of all cognitive, emotional, and behavioral reactions given by the individual to resist to these events or factors.[5] Coping attitudes are unique to each and differ on the basis of multiple factors such as gender, age, culture, and disease.[6]
In general, coping methods aimed to overcome the issues are classified into solution-focused and emotion-focused methods.[7] The solution-focused method includes the attitudes related to the malfunctioning underlying the problem, and the emotion-focused method includes the attitudes related to coping with the emotional effects created by this malfunctioning. From this aspect, coping methods can be classified into two sections: Those which are adaptation-focused and which are not.[8] There is a statistically significant relationship between the adoption of the coping methods aimed at reducing emotional stress rather than the adaptation-focused active coping methods in regards to psychopathological findings. Detection of the coping attitudes adopted by the individual against the negativity-creating problem provides beneficial in setting and monitoring the appropriate medical and psychological treatment targets.[5,9]
While the early diagnosis and the developments in scanning and treatment options span the life period; treatment-related problems create the main effect on the quality of life (QoL) of the caregivers. Caregiving responsibility undertaken in this process impairs both mental and physiological wellbeing of caregivers and increases his/her psychological burden and negatively affects upon his/her QoL.[10]
Literature review conducted made in the scope of the present study revealed limited or no previous study analyzing the cancer patients and their caregivers together. The present study aimed to examine the coping methods used by the cancer patients and their caregivers in the diagnosis and treatment phases of cancer process full of psychological difficulties and the effects of this process on the life quality of the caregivers of these patients.
METHODS
This observational, cross-sectional study was conducted at the medical oncology clinic of tertiary care hospital. Patients who were hospitalized or treated as cancer outpatients for chemotherapy treatment and their caregivers (patients' relatives) were included in the study. Terminal phase patients who had cognitive function disorders, patients with all kinds of acute infections, pregnant, and those having any inflammatory diseases were excluded from the present study. Almost all of the caregivers were the first-degree relatives of the patients. They were the ones fulfilling patients' needs about their medical healthcare and daily life. Patients and caregivers were informed about the scope of the study. While 74 patients and 46 caregivers who signed the consent form were classified into the experimental groups, 46 individuals with no psychiatric or chronic diseases were enrolled into the control group randomly. Required permit related to the compliance of the study with the ethical rules was obtained from the Local Board of Ethics.
A pretested structured questionnaire was administered to the study participants via face-to-face interviews conducted by trained physicians. The questionnaire was composed sections on sociodemographic information, coping attitudes assessment scale (COPE) scale and. Short Form-36 (SF-36) QoL scale. Questionnaire results were evaluated with the help of a psychiatrist.
Coping attitudes assessment scale
COPE is a 60-item validated scale developed by Carver et al. in 1989.[11] Ağargün et al. declared that COPE was a reliable and validated instrument for assessing coping strategies in Turkish study sample. It is composed of 15 subscales, each including 4 items.[6] Each of 15 subscales informs about a specific coping attitude such as positive reinterpretation and growth and behavioral disengagement. Minimum and maximum possible scores to be taken from each subscale are 4 and 16 points, respectively. Sum of the first 5 subscale scores constitutes the problem-focused coping score; sum of the 6th–10th subscale scores refer to the emotion-focused coping score; and the sum of the remaining 5 subscale scores point out the dysfunctional coping score.
Short Form-36 quality of life scale
It was developed and brought into use by Rand Corporation in 1992.[12] The 36-item questionnaire is composed of physical and mental components. Physical component consists of the subscales of general health (GH), physical function (FF), etc.; the mental component consists of the subscales of mental health (MH), role limitations related to the emotional function (ER), liveliness/vitality/energy, and social function (SF). Subscales assess health in 0–100 score range, where “0” points out bad health. The scale offers items about the health change perception within the last 4 weeks and the last 1 week. Validity and reliability studies of the Turkish version of the SF-36 scale were conducted by Koçyiğit et al.[13]
Data analysis was performed on SPSS version 22.00 (SPSS Inc., Chicago, IL., USA). Frequencies, percentages, mean scores, and standard deviations were calculated to define the descriptive statistics. Compliance of the active coping attitudes with the normal distribution in terms of descriptive statistics was tested via Kolmogorov–Smirnov test. Multiple-group comparisons were made by one-way ANOVA and the post hoc comparisons by Bonferroni test for the parameters complying with the normal distribution. Parameters noncomplying with the normal distribution were tested by Kruskal–Wallis test, and then the further pair comparisons were assessed by Bonferroni-adjusted Mann–Whitney U-test. Statistical significance was set at P ≤ 0.05.
RESULTS
The study was designed to recruit 100 cancer patients and same number of their caregivers. After taking consents, 74 cancer patients, 46 caregivers (experimental groups), and 46 healthy individuals (control group) were enrolled in the study. Females were 36.5% (n = 27) of the patient group; 50% (n = 23) of the caregivers group; and 47.8% (n = 22) of the control group; whereas males constituted 63.5% (n = 47) of the patient group; 50% (n = 23) of the caregivers group; and 52.2% (n = 24) of the control group. Mean age of the patient group was 37.30 ± 15.30; of the caregivers group was 44.65 ± 11.62; and of the control group was 33.83 ± 8.52. The relationship between the patients and their caregivers is figured out in Figure 1.
Figure 1.

Distribution of relationship in caregiver group
Half of the cancer patients (50%, n = 37) were married while 93.5% (n = 43) of the caregivers were married. On the other hand, 89.1% (n = 41) of the control group participants were married. Statistically significance was detected between groups in terms of marital status (P< 0.001). About 5.5% (n = 4) of the cancer patients were literate, and about 36.5% (n = 27) of them had 15 years of educational background. Educational background status of the caregivers was as follows: 30.5% (n = 14) of them had 8 years, 19.6% (n = 9) of them 11 years, and 50% (n = 23) of them 15 years of educational background. About 4.3% (n = 2) of the control group participants had 8 years, 50% (n = 23) of them 11 years, and 45.7% (n = 21) of them 15 years of educational background. Comparison of the educational backgrounds of the study groups demonstrated a statistically significant difference (P< 0.001). This difference may have arisen from the lower educational background of the patient and caregivers groups compared to the control group. Mean scores of the study groups from the main and subgroups of the COPE scale are presented in Table 1.
Table 1.
Intergroup comparison of the coping attitudes assessment scale scores
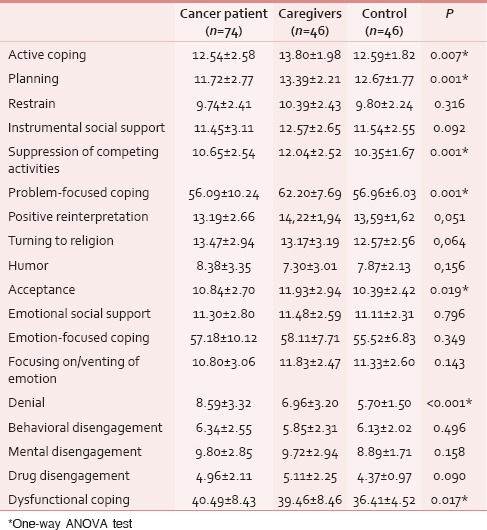
Comparison of the scores getting from the main groups of the COPE scale among study groups (patient, caregiver, and control groups) demonstrated a statistically significant difference in the “problem-focused coping” and “dysfunctional coping” scores (P = 0.001, P = 0.017, respectively). The difference detected in terms of problem-focused coping method was established between caregiver group and groups of patients and control, which originated from the higher mean scores of the caregivers group compared to the other two groups. Statistical difference in the “dysfunctional coping” scores was recorded between the patient group and control group, which was induced by the higher score of the patient group compared to the control group. However, no statistically significant difference was found out between the study groups in terms of “emotion-focused coping” scores (P = 0.349).
A statistically significant difference was recorded between the scores taken from “active coping,” “planning,” and “suppression of competing activities” of which are the three subgroups of the “problem-focused coping” main group of the COPE scale (P = 0.007, P = 0.001, P = 0.001, respectively). Statistically significant difference in the “active coping” scores was detected among the caregiver group on one hand and the patient and control groups on the other; in the “planning” scores between the caregiver and patient groups; in the “suppression of competing activities” score between the caregivers group on one hand, and the patient and control groups on the other. A statistically significant intergroup difference was detected in the “acceptance” subgroup of the “emotion-focused coping” main group of the COPE scale (P = 0.019). This difference was determined between the caregiver and control groups, which resulted from higher scores of the caregiver group compared to the control group. A statistically significant difference was found out in terms of scores taken from the “denial” subgroup of the “dysfunctional coping” main group among the study groups (P ≤ 0.001). This difference originated from the higher scores of patients compared to scores of caregiver and control groups.
Examination of the gender-based COPE scores of the cancer patients group revealed a statistically significant difference in the subgroups of “acceptance,” “positive reinterpretation,” and “focusing on and venting of emotion” (P = 0.029, P = 0.040, P = 0.006, respectively). This difference was produced by the high scores of females from these subgroups [Table 2]. Comparison of the gender-based COPE scores of the caregivers group revealed a statistically significant difference in the “mental disengagement” and “dysfunctional coping” methods (P = 0.007, P = 0.048, respectively). This difference was associated with the higher scores of female caregivers from these two subgroups [Table 3].
Table 2.
Distribution of significant coping attitudes assessment scale subgroups regarding to gender difference in the cancer patient group (n=74)
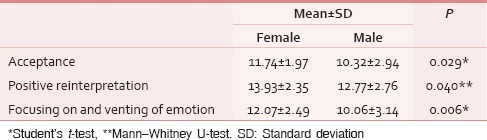
Table 3.
Distribution of significant coping attitudes assessment scale subgroups regarding to gender difference in the caregivers group (n=46)
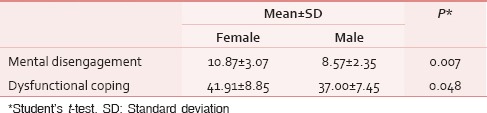
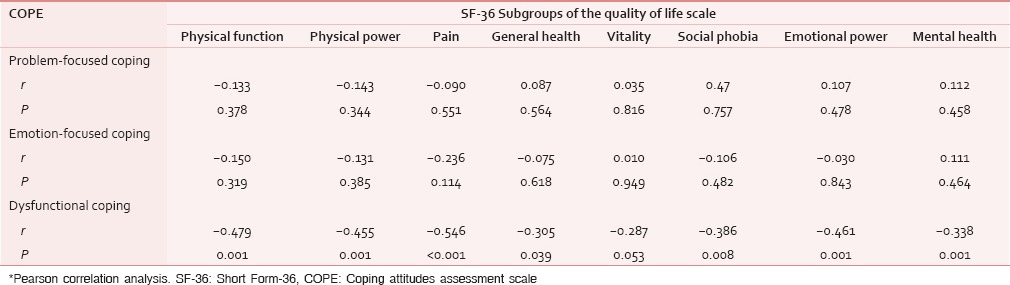
Table 4 presents the scores for the caregivers and control groups from the SF-36 QoL Scale. Comparison between these two groups on the basis of SF-36 scores produced a statistically significant difference in all parameters (P< 0.05), with the highest difference in the physical role and emotional role level. Gender-based comparison between the SF-36 scores of the caregivers group revealed a statistically significant difference in the subgroups of pain, vitality, SF, and emotional role; with the highest difference in the vitality subgroup [Table 5]. The present study established a statistically significant difference and negative correlation between the scores taken from all subgroups of the SF-36 scale which contain physical and mental components (except for the vitality subgroup) and from the “dysfunctional coping” main group of the COPE scale [Table 6].
Table 4.
Analysis and group distribution of the SF-36 scores
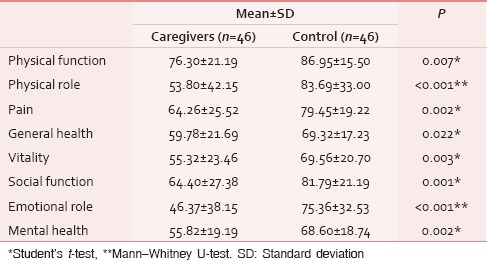
Table 5.
Analysis and gender-based distribution of the Short Form-36 scores of the caregivers group (n=46)
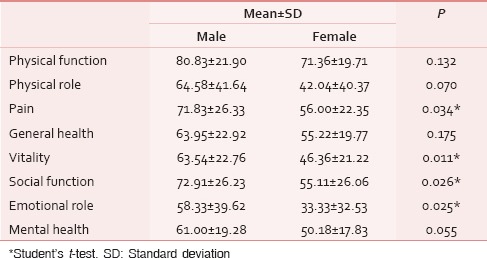
Table 6.
Relationship between the Short Form-36 subgroups and the coping attitudes assessment scale
DISCUSSION
The coping attitudes developed by the patients with various types of cancer and their caregivers against cancer were examined in this cross-sectional study. Group-based evaluations showed that caregivers used mainly the “acceptance” method among the “emotional coping” methods and gender-based evaluations revealed that females caregivers adopted mainly the “dysfunctional coping” method and “mental disengagement.” Group-based study evaluations, on the other hand, pointed out that cancer patients group used the dysfunctional coping methods and the method of denial among the subgroups. Female cancer patients were recorded to utilize “acceptance” and “positive reinterpretation” methods (included in the main group of the “emotion-focused coping”) and “focusing on and venting of emotion” (included in the main group of “dysfunctional coping”) more frequently than the male cancer patients.
In a study conducted by Manna et al. on 44 women with breast cancer, the patients were found out to use emotion-focused coping methods more frequently than the other coping methods.[14] The present study showed that female cancer patients used acceptance and positive reinterpretation methods (included in the main group of “emotion-focused coping”) more than the male cancer patients [Table 2]. Use of such emotional coping methods by the female cancer patients may result from the more sensitive attitudes they develop against stressing situations. Considering on the group basis, caregivers were found to prefer acceptance method (included in the main group of “emotion-focused coping”). Adoption of this coping method by the caregivers may be interpreted in such way that individuals who are afraid to lose their beloved ones avoid using cognitive problem-solving skills and tend to accept the illness. In the study by Manna et al., breast cancer group was found to adopt dysfunctional coping methods more (not at a statistically significant level though) than the control group. Study group comparisons made within the scope of the present study also showed that mainly the dysfunctional coping methods and (as a subgroup) denial method were used by the patient group. Utilization of such coping methods by the cancer patients may be explained by the groups that cancer patients have difficulty in overcoming this chronic process and tend to deny their problems by leaving them aside. Since it reduces anxiety, denial is known to be beneficial in improving problem-coping skill. Unless the anxiety-creating factor is successfully ignored, denial method may bring no benefit but some extra problems.
It seems that there are alterations in perception of cancer diagnoses and caregiving experiences based on gender differences. Kim and Givenstated that females were inclined to accept the caregiving character and more likely to reflect their emotions comparing to males.[15] In another study, it was found out male caregivers of patients with breast and gynecological cancer were more likely to have interconnected physical, cognitive, and psychological problems after the period exceeding 1 year.[16] Moreover, gender-based comparisons made within the scope of the present study stated that the method of “focusing on and venting of emotion” (included in the main group of “dysfunctional coping”) was more frequently used by the female cancer patients. Utilization of this method reflects the tendency of the individual to focus on the negativities she/he suffers from and to disclose how she/he feels in this process. It should be noted that responding to some situations by using dysfunctional coping methods may either be functional or prevent the adaptation process. Caregivers group of the present study used mainly “the dysfunctional coping method” and “mental disengagement.” Usage of this method may be interpreted such that it is quite difficult for the female caregivers to carry the psychological burden of the diseases and that they no more regard this process.
Many studies have been conducted on the QoL levels perceived by the cancer patients during the diagnosis and treatment processes. However, there are only a limited number of studies aimed to assess the QoL of the individuals who give care to and who meet the needs of the cancer patients (most of the caregivers being the first-degree relatives).[17,18,19] Therefore, future studies are warranted on the psychological state and QoL of the caregivers, which are impaired in this chronic process.
In a study on 212 cancer patients receiving chemotherapy and on their caregivers found out that the scores of the caregivers from the subgroups of FF, physical role, and GH (of the physical component group) were nearly as high as the scores of the healthy control group. One of the surprising results of the concerned studies was that the scores of the caregivers group from the subgroup of MH were lower than those of the patients whom they cared and whose needs they met.[20] Klassen et al. revealed that parents giving care for their children with cancer (411 children) got significantly lower scores from all physical and psychological parameters of the QoL compared to the healthy individuals.[21] The present study also recorded that caregivers got statistically significant lower scores from all physical and mental component subgroups of the SF-36 scale compared to the control group. These results suggest that caregivers are equally stressed (physically and emotionally) as that of cancer patients.
Several studies indicated gender-based differences in favor of women in such psychological diagnosis as anxiety and depressive disorder.[22] However, only a few studies have been able to find out whether this difference also exists in terms of the QoL of the caregivers of the cancer patients. In a study on caregivers of 49 breast and 47 prostate cancer patients revealed that caregivers of both types of cancer patients had statistically significant lower scores from the MH, vitality, and SF subgroups of the SF-36 scales compared to the healthy individuals. Mean emotional power scores of the male caregivers were lower than healthy individuals at the statistically significant level. Physical function subgroup scores of the caregiving females were statistically significantly higher than healthy individuals. However, no such statistically significant difference was recorded between the caregivers and the control group in the other three subgroups reflecting the physical component.[17] Examination of the scores of the caregivers group of the present study from the SF-36 scale showed that female caregivers had statistically significantly lower scores than the male caregivers in the subgroups of pain, vitality, SF and emotional role. This difference may have originated from being more sensitive attitudes of women toward to their inner world experiences.
Based on our literature search, there is no or limited evidence available regarding the correlation between SF-36 QoL scale and the COPE Scale. The present study, on the other hand, assumed a relationship between the method adopted in the disease coping process and the quality of daily life of the individuals affected by the chronic disease processes. This study revealed a statistically significant difference and negative correlation between the dysfunctional coping scores and all subgroups of the SF-36 scale, which contain physical and mental components (except for the vitality subscale). This statistically significant difference may be explained because the individuals whose QoL has diminished tend to develop dysfunctional coping attitudes.
Study limitations
Some limitations of our study merit emphasis. First, the present study had a small sample size of participants. Moreover, this cross-sectional study does not offer a cause and effect relationship; rather, it reflects the current situation. Most important reason for this limitation is the long treatment and prognosis periods of the most cancer types. Future studies should be conducted using larger sample size including both the patients and their caregivers in national centers monitoring oncology patients. Second, based on a limitation about small sample size, we could not have a chance to assess the statistical association between coping styles and phases of the diagnosis and treatment both in patients and caregivers groups. Third, the mean age of the control group was approximately 4 years younger than the patient group. This slight difference may have an impact on coping scores of both groups. Further studies need to be conducted on any possible change in the coping attitudes during the cancer treatment processes.
CONCLUSION
The present study pointed out that caregivers utilized mainly the “acceptance” method among the “emotional coping” methods, while cancer patients utilized the dysfunctional coping methods and the method of denial among the subgroups. In addition, caregivers had lower scores within all physical and mental component subgroups of the SF-36 scale compared to the control group. Moreover, a statistically significant difference and negative correlation between the dysfunctional coping scores and all subgroups of the SF-36 scale (except for the vitality subscale) was determined.
In accordance with literature, the present study demonstrated that psychological support should be given to the patients and their caregivers to use the coping methods oriented at the source of the problem rather than the dysfunctional coping methods. Integration of the QoL indicators in the relationship with not only the patients but also their caregivers would offer a more integrated approach and meet the needs of the caregivers. One of the most important responsibilities of the primary health care providers is to ensure and maintenance of the functional coping methods by the cancer patients and their caregivers in the scope of the medical and psychological supportive treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lepore SJ, Coyne JC. Psychological interventions for distress in cancer patients: A review of reviews. Ann Behav Med. 2006;32:85–92. doi: 10.1207/s15324796abm3202_2. [DOI] [PubMed] [Google Scholar]
- 2.Çivi S, Kutlu R, Çelik HH. Depression status and the factors affecting the quality of life in the relatives of the patients with cancer. Gulhane Med J. 2011;53:248–53. [Google Scholar]
- 3.Hudson PL, Remedios C, Thomas K. A systematic review of psychosocial interventions for family carers of palliative care patients. BMC Palliat Care. 2010;9:17. doi: 10.1186/1472-684X-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaugler JE, Eppinger A, King J, Sandberg T, Regine WF. Coping and its effects on cancer caregiving. Support Care Cancer. 2013;21:385–95. doi: 10.1007/s00520-012-1525-5. [DOI] [PubMed] [Google Scholar]
- 5.Dempster M, McCorry NK, Brennan E, Donnelly M, Murray LJ, Johnston BT. Psychological distress among family carers of oesophageal cancer survivors: The role of illness cognitions and coping. Psychooncology. 2011;20:698–705. doi: 10.1002/pon.1760. [DOI] [PubMed] [Google Scholar]
- 6.Ağargün MY, Beşiroğlu L, Kıran Ü, Özer Ö, Kara H. The psychometric properties of the COPE inventory in Turkish sample: A preliminary research. Anatolian Journal of Psychiatry. 2005;6:221–26. [Google Scholar]
- 7.Li XM, Sun YQ. A correlation study between hope and coping style for nasopharyngeal cancer patients during radiotherapy. Chin J Prev Control Chronic Dis. 2011;19:422–3. [Google Scholar]
- 8.Rohde P, Lewinsohn PM, Tilson M, Seeley JR. Dimensionality of coping and its relation to depression. J Pers Soc Psychol. 1990;58:499–511. doi: 10.1037//0022-3514.58.3.499. [DOI] [PubMed] [Google Scholar]
- 9.Han Y, Hu D, Liu Y, Caihong Lu, Luo Z, Zhao J, et al. Coping styles and social support among depressed Chinese family caregivers of patients with esophageal cancer. Eur J Oncol Nurs. 2014;18:571–7. doi: 10.1016/j.ejon.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Given BA, Given CW, Sherwood P. The challenge of quality cancer care for family caregivers. Semin Oncol Nurs. 2012;28:205–12. doi: 10.1016/j.soncn.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989;56:267–83. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 12.Bowling A. Measuring Health: A Review of Quality of Life Measurement Scales. 2nd ed. Philadelphia: Open University Press; 1997. [Google Scholar]
- 13.Koçyiğit H, Aydemir Ö, Fişek G, Ölmez N, Memiş A. Kısa Form 36 (KF–36)'nın Türkçe versiyonunun güvenilirliği ve geçerliliği. Ilaç ve tedavi dergisi. 1999;12:102–6. (Article in Turkish) [Google Scholar]
- 14.Manna G, Foddai E, Di Maggio MG, Pace F, Colucci G, Gebbia N, et al. Emotional expression and coping style in female breast cancer. Ann Oncol. 2007;18(Suppl 6):vi77–80. doi: 10.1093/annonc/mdm231. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: Across the trajectory of the illness. Cancer. 2008;112(11 Suppl):2556–68. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 16.Lopez V, Copp G, Molassiotis A. Male caregivers of patients with breast and gynecologic cancer: Experiences from caring for their spouses and partners. Cancer Nurs. 2012;35:402–10. doi: 10.1097/NCC.0b013e318231daf0. [DOI] [PubMed] [Google Scholar]
- 17.Grov EK, Dahl AA, Moum T, Fosså SD. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. 2005;16:1185–91. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- 18.Wagner CD, Bigatti SM, Storniolo AM. Quality of life of husbands of women with breast cancer. Psychooncology. 2006;15:109–20. doi: 10.1002/pon.928. [DOI] [PubMed] [Google Scholar]
- 19.Shakeri J, Kamangar M, Ebrahimi E, Aznab M, Shakeri H, Arman F. Association of coping styles with quality of life in cancer patients. Indian J Palliat Care. 2015;21:298–304. doi: 10.4103/0973-1075.164890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papadopoulos A, Vrettos I, Kamposioras K, Anagnostopoulos F, Giannopoulos G, Pectasides D, et al. Impact of cancer patients' disease awareness on their family members' health-related quality of life: A cross-sectional survey. Psychooncology. 2011;20:294–301. doi: 10.1002/pon.1731. [DOI] [PubMed] [Google Scholar]
- 21.Klassen AF, Klaassen R, Dix D, Pritchard S, Yanofsky R, O'Donnell M, et al. Impact of caring for a child with cancer on parents' health-related quality of life. J Clin Oncol. 2008;26:5884–9. doi: 10.1200/JCO.2007.15.2835. [DOI] [PubMed] [Google Scholar]
- 22.Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158:1091–8. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]


