Abstract
Objective:
Pharmacy-driven medication history (MH) programs have been shown to reduce the number of serious or potentially life-threatening (S/PLT) medication discrepancies (MDs) in many settings, but not Intensive Care Units (ICUs).
Methods:
MHs were repeated over a 6-week period. Demographics, number, and nature of MDs were documented. Discrepancy severity was graded using a previously published method. Primary outcome was the proportion of MHs containing >1 S/PLT MDs.
Findings:
Sixty-three MHs were repeated. Pharmacy MHs were less likely to contain ≥1 S/PLT MDs (0% vs. 50%, P < 0.001).
Conclusion:
Pharmacy MHs contained fewer S/PLT MDs in this small sample. S/PLT MDs on admission and home medication lists were common in patients admitted to the medical ICU. Pharmacy-driven medication reconciliation (MR) reduced the number and frequency of these discrepancies. Further research is required to improve current MR procedures.
Keywords: Critical care, medication reconciliation, intensive care unit
INTRODUCTION
Medication errors are a common cause of harm in hospitalized patients.[1] Accurate medication reconciliation (MR) has been shown to reduce medication errors, but has not been extensively studied in Intensive Care Units (ICUs).[1] Considering this population's complexity of illness, systematic evaluation of MR and pharmacy's impact on the process are required. This study's purpose was to characterize medication discrepancies (MDs) in medical ICU (MICU) patients. The primary endpoint was the proportion of medication histories (MHs) containing at least one serious or potentially life-threatening discrepancy (S/PLTD). We hypothesized that MHs performed by pharmacy personnel would contain fewer S/PLTDs than nonpharmacy personnel.
METHODS
This quality improvement study met the criteria for exemption from the Institutional Review Board. A convenience sample of adult MICU patients was reviewed over a 6-week period. A sample size was not predetermined, but patients admitted to the MICU were selected from a convenience sample to be screened for inclusion after initial MHs were completed by either pharmacy or nonpharmacy personnel upon admission. Patients not taking any medications before admission and patients for whom an accurate MH could not be obtained were excluded, as described in Figure 1. A single reviewer, trained in MR, repeated MHs in included patients by utilizing patients’ caregivers, pharmacies, and past admission records as sources of information. Demographics, professional designation of initial MH (pharmacy or nonpharmacy personnel), number of discrepancies, and discrepancy nature were recorded. Three reviewers independently and subjectively determined discrepancy severity using a pre-established severity-of-error scale, published by Kalb et al., based on how likely the discrepancy was to cause minor, moderate, or S/PLT discomfort or clinical deterioration [Table 1].[2] The reviewers later discussed all discrepancies and came to a consensus if there was any disagreement concerning discrepancy severity. An MH was considered accurate if it was >90% correct when compared to the repeat reconciliation.[3]
Figure 1.
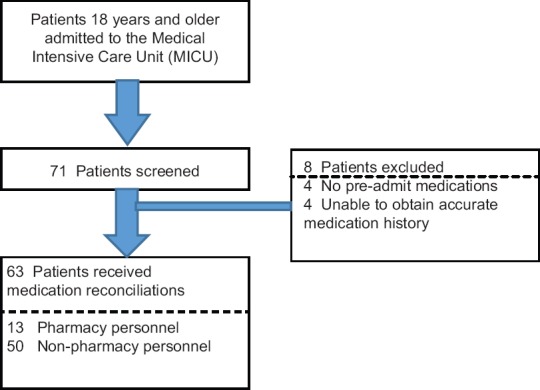
Study design
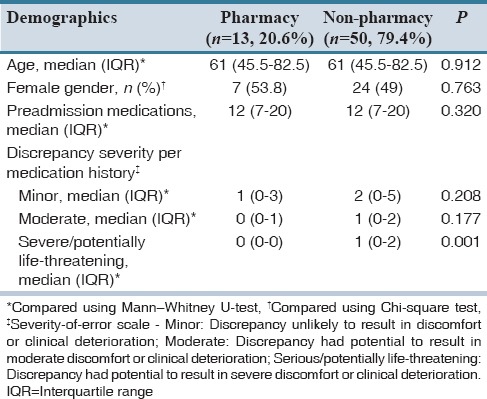
Table 1.
Demographics and discrepancy severity from pharmacy and non-pharmacy medication histories
The primary outcome was the proportion of MHs performed by pharmacy versus nonpharmacy personnel containing at least one S/PLTD. Secondary outcomes were the incidence of MDs and the accuracy of MHs performed by pharmacy versus nonpharmacy personnel.
Descriptive statistics including median and interquartile range (IQR) were used to describe the central tendency and data spread; Mann-Whitney U-test was used for the comparison of continuous data; and Chi-square test/Fisher's exact test was used for categorical data. All statistical tests were two-tailed, and P < 0.05 was considered statistically significant. All statistics were performed using IBM SPSS version 22.0 (Released 2013. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp.).
RESULTS
Over a period of 6 weeks, 63 MHs were repeated in adult patients admitted to the MICU. Thirteen and 50 MHs were completed by pharmacy and nonpharmacy personnel, respectively. Demographics are summarized in Table 1 and were similar between groups.
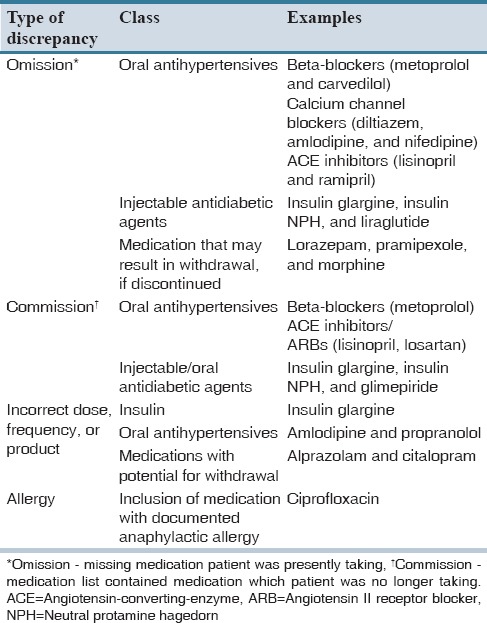
In total, 292 discrepancies were identified. Omissions and commissions were most common, accounting for 36.6% (107/292) and 33.9% (99/292) of identified discrepancies, respectively [Figure 2]. Of 292 total discrepancies, 50 (17.1%) were classified as S/PLT. Examples of S/PLTDs included omissions or commissions of diabetes medications such as insulin, omissions, or commissions of cardiovascular medications such as beta-blockers and omission of medications that have the potential to cause serious withdrawal such as benzodiazepines [Table 2].
Figure 2.
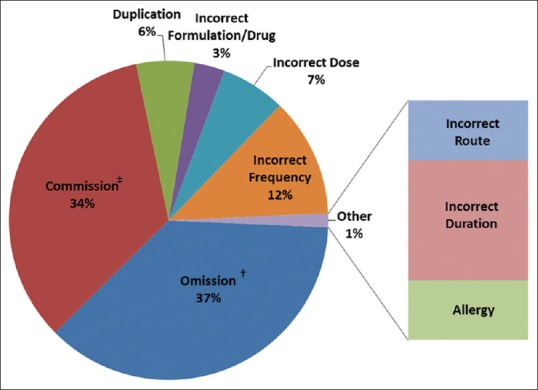
Types of discrepancies (n = 292)*. *No statistical difference in discrepancy type between pharmacy and nonpharmacy personnel, †Omission - missing medication patient was presently taking, ‡Commission - medication list contained medication which patient was no longer taking
Table 2.
Examples of serious/potentially life-threatening discrepancies
There was no statistical difference in the total number of minor and moderate discrepancies contained within MHs initially obtained by pharmacy versus nonpharmacy personnel (minor, n [%]: 24 (64.9) vs. 152 (59.6), P = 0.593; moderate, n [%]: 13 (35.1) vs. 53 (20.8), P = 0.051). The proportion of MHs containing at least one S/PLTD was also significantly lower in those completed by pharmacy versus nonpharmacy personnel (0% vs. 50%, P < 0.001); [Table 3].
Table 3.
Primary and secondary outcomes in medication histories performed by pharmacy verses nonpharmacy personnel
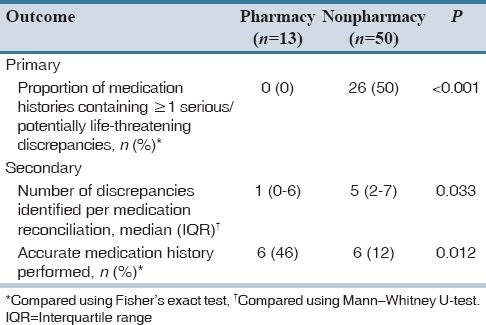
MDs in general were less common when MHs were completed by pharmacy personnel (median [IQR]: 1 [0-6] vs. 5 [2-7], P = 0.033); [Table 3]. Pharmacy personnel were also more likely to produce accurate MHs than nonpharmacy personnel (46% vs. 12%, P = 0.012); [Table 3].
DISCUSSION
Overall, S/PLTDs were common in the MICU, occurring in 18% of MHs. In a study using a similar severity-of-error scale, 17% of discrepancies found were classified as having the potential to cause severe discomfort and clinical deterioration, which is consistent with our findings.[2] More than 85% of patients in our study had discrepancies in their MHS; similar to the findings of studies completed upon admission to emergency departments (EDs).[4] Only about 20% of patients had accurate MHs on admission (using a benchmark of >90% accuracy).[1] About 80% of patients did not have MHs completed by pharmacy personnel; however, our results indicate that MHs completed by pharmacy personnel appeared to be more accurate.
Other studies comparing the standard of care (MHs completed by nursing and medical staff) to pharmacy-acquired MHs have demonstrated similar outcomes.[1,4] Several recent studies aiming to assess the potential impact of pharmacy-driven MR programs in EDs and internal medicine teams have found that pharmacists, student pharmacists, and pharmacy technicians were able to identify a higher number of discrepancies and complete more accurate MHs than nonpharmacy personnel.[4,5,6] Lancaster and Grgurich used a strict set of inclusion and exclusion criteria to include only “high-risk,” communicative patients in their study of patients admitted to an internal medicine team, thereby excluding over half of potential patients.[6] Lancaster's study and a study by Provine et al. who evaluated patients admitted to a general pediatrics service were limited by the lack of characterization of discrepancies in terms of clinical significance.[6,7] We attempted to reduce several limitations from previous studies by not excluding noncommunicative patients (which would have excluded many MICU patients, as intubation and sedation are common) and classifying discrepancies according to a pre-established severity-of-error scale to help place value on the clinical significance of the discrepancies.[2]
Illness severity is a strong predictor of adverse drug events and medication errors, which places MICU patients at an increased risk for harm.[3] Accurate MR has been shown to reduce medication errors, but has not been extensively studied in critically ill patients. This study characterized both the frequency and severity of medication errors found within home medication lists in a population that has not been previously defined in terms of MR.
Limitations of this study include small sample size, single-center study, as well as several barriers to obtaining accurate MRs. Such barriers include, but are not limited to the lack of knowledge on the part of families and caregivers regarding patients’ medications. Sedation, intubated, and critically ill patients were often unable to be utilized as a source of information, and the use of multiple pharmacies complicated the MR process. The results of this study may not be generalizable to other institutions, based on its single-center design and small sample size.
The impact of pharmacy-driven MR has been previously studied and noted in a variety of settings. However, despite widespread acceptance that MHs obtained by pharmacy personnel have been shown to be more accurate than those obtained by nursing and medical staff, the concept of utilizing pharmacy personnel to help reduce potential medication errors has yet to be universally applied. Anecdotal reports indicate that many institutions have begun to implement pharmacy-driven MR protocols in selected areas of patient care.[3,4,7] Our institution, for example, currently utilizes certified pharmacy technicians to complete MHs in the ED during peak hours. Nursing and medical staff predominantly obtain MHs throughout the rest of the institution and are expected to perform MR. Based on the findings of this quality improvement study, future research directions will include implementation and systematic evaluation of a pharmacy-driven protocol in MR.
The results of this study identified areas for potential improvement in our current procedures. The percentage of accurate MHs performed by pharmacy personnel was 46% (compared to 12% of MHs completed by nonpharmacy personnel), which is lower than previous studies completed in the ED of our institution. It is important to note that this study involved a different population of patients, ICU patients specifically. While some ICU patients may be admitted through the ED, it is not uncommon for ICU patients to be admitted in a state where it is difficult to obtain a completely accurate MH. Although many patients may have a home pharmacy on file in their electronic medical record, information regarding the use of additional pharmacies might not be obtained until further questioning of caregivers and family members can be completed.
This quality improvement study demonstrates that S/PLTDs are prevalent in the MICU population. The degree of S/PLTDs revealed suggest that medication histories obtained via pharmacy personnel compared to non -pharmacy personnel are more accurate and further supports the benefit of pharmacy personnel involvement in MR.
AUTHORS’ CONTRIBUTION
Wills, Brittany M., PharmD Student, Wilkes University Nesbitt School of Pharmacy, Wilkes-Barre, PA. Darko, William, BPharm, PharmD, Upstate University Hospital, Syracuse, NY. Seabury, Robert, PharmD, BCPS, Upstate University Hospital, Syracuse, NY. Probst, Luke A., PharmD, BCPS, Upstate University Hospital, Syracuse, NY. Miller, Christopher D., PharmD, BCPS, Upstate University Hospital, Syracuse, NY. Cwikla, Gregory M., PharmD, Upstate University Hospital, Syracuse, NY.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Moyen E, Camiré E, Stelfox HT. Clinical review: Medication errors in critical care. Crit Care. 2008;12:208. doi: 10.1186/cc6813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalb K, Shalansky S, Legal M, Khan N, Ma I, Hunte G. Unintended medication discrepancies associated with reliance on prescription databases for medication reconciliation on admission to a general medical ward. Can J Hosp Pharm. 2009;62:284–9. doi: 10.4212/cjhp.v62i4.809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith SB, Mango MD. Pharmacy-based medication reconciliation program utilizing pharmacists and technicians: A process improvement initiative. Hosp Pharm. 2013;48:112–9. doi: 10.1310/hpj4802-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Becerra-Camargo J, Martínez-Martínez F, García-Jiménez E. The effect on potential adverse drug events of a pharmacist-acquired medication history in an emergency department: A multicentre, double-blind, randomised, controlled, parallel-group study. BMC Health Serv Res. 2015;15:337. doi: 10.1186/s12913-015-0990-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hart C, Price C, Graziose G, Grey J. A program using pharmacy technicians to collect medication histories in the emergency department. P T. 2015;40:56–61. [PMC free article] [PubMed] [Google Scholar]
- 6.Lancaster JW, Grgurich PE. Impact of students pharmacists on the medication reconciliation process in high-risk hospitalized general medicine patients. Am J Pharm Educ. 2014;78:34. doi: 10.5688/ajpe78234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Provine AD, Simmons EM, Bhagat PH. Establishment and evaluation of pharmacist-managed admission medication history and reconciliation process for pediatric patients. J Pediatr Pharmacol Ther. 2014;19:98–102. doi: 10.5863/1551-6776-19.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]


