Abstract
Background
Nipple-sparing mastectomy (NSM) is considered an oncologically safe option for select patients. As many patients are candidates for nipple-sparing or skin-sparing mastectomy (SSM), reliable patient-reported outcome data are crucial for decision-making. The objective of this study was to determine whether patient satisfaction and/or health-related quality of life (HRQOL) were improved by preservation of the nipple with NSM compared to SSM and nipple reconstruction.
Methods
Subjects were identified from a prospectively maintained database of patients who completed the BREAST-Q following mastectomy and breast reconstruction between March and October 2011 at Memorial Sloan Kettering Cancer Center. Fifty-two patients underwent NSM followed by immediate expander-implant reconstruction. A comparison group consisted of 202 patients who underwent SSM followed by immediate expander-implant reconstruction and later nipple reconstruction. HRQOL and satisfaction domains as measured by BREAST-Q scores were compared in multivariate linear regression analyses that controlled for potential confounding factors.
Results
NSM patients reported significantly higher scores in the psychosocial (p=0.01) and sexual well-being (p=0.02) domains compared to SSM patients. There was no significant difference in the BREAST-Q physical well-being, satisfaction with breast, or satisfaction with outcome domains between the NSM and SSM groups.
Conclusions
NSM is associated with higher psychosocial and sexual well-being compared to SSM and nipple reconstruction. Preoperative discussion of such HRQOL outcomes with patients may facilitate informed decision-making and realistic postoperative expectations.
Keywords: nipple-sparing mastectomy, breast reconstruction, implant reconstruction, health-related quality of life, BREAST-Q
INTRODUCTION
The nipple areola complex (NAC) is a vital component and focal point of the breast. Reconstruction of the NAC following total mastectomy and breast mound reconstruction has been shown to enhance a woman's body image and health-related quality of life (HRQOL) and render the breast reconstruction complete (1,2). Despite this, outcomes following NAC reconstruction remain variable, with factors such as nipple projection, color match, shape, and sensitivity contributing most frequently to patient dissatisfaction (3-6).
Nipple-sparing mastectomy (NSM) may offer an appealing alternative from both an aesthetic and psychological point of view. Born out of efforts to lessen disfigurement and improve cosmesis following mastectomy, NSM is increasingly sought after and performed by patients and surgeons, respectively (7,8). While still somewhat controversial, NSM has become recognized as an oncologically safe option for carefully selected patients (9-13). Numerous studies have reviewed the oncologic safety and surgical complications of NSM, and critics of the procedure often cite poor preservation of vascularity and sensation to the NAC as factors that detract from the end result (14,15). Few studies, in contrast, have examined the impact of nipple preservation on HRQOL following mastectomy and reconstruction, particularly psychological and sexual functioning (16,17). The increased demand for NSM underscores the need for objective evaluation of these HRQOL outcomes. Such data will allow clinicians to counsel patients on realistic outcomes following NSM and will assist patients in making decisions regarding a still-controversial procedure.
The objective of this study was to determine how HRQOL is impacted by NAC preservation. We compared women undergoing NSM and implant reconstruction with women undergoing skin-sparing mastectomy (SSM), implant reconstruction, and delayed NAC reconstruction using the BREAST-Q, a validated patient-reported outcome (PRO) instrument developed specifically for breast reconstruction patients (18,19).
METHODS
Patient Selection
With institutional review board approval, institutional databases were retrospectively reviewed from September 2005 to October 2011 to identify all patients who underwent unilateral or bilateral NSM followed by immediate expander/implant reconstruction at Memorial Sloan Kettering Cancer Center. This population was then cross-referenced with a prospectively maintained database of patients who completed the BREAST-Q reconstruction module at a minimum of five months following their final reconstruction surgery as part of routine clinical care.
Patients deemed eligible for NSM at Memorial Sloan Kettering Cancer Center were females 18 years of age or older undergoing mastectomy for prophylaxis or stage IIB disease or less, with the tumor >1cm from the areolar margin. Furthermore, these patients were deemed suitable for immediate reconstruction as determined by the operative plastic surgeon. Exclusion criteria included patients with disease greater than stage IIB, tumor <1cm from the areolar margin, retroareolar tissue biopsy positive for invasive or intraductal carcinoma, clinical evidence of NAC involvement (i.e., induration, retraction, ulceration, bloody discharge), Paget's disease, previous invasive breast cancer treated with breast-conserving surgery, grade 3 nipple ptosis, or any medical comorbidity known to negatively impact wound healing such as uncontrolled diabetes mellitus or constitute an unwarranted surgical risk. Patients undergoing either unilateral or bilateral NSM were eligible for inclusion in this study.
A comparison group was identified from patients who underwent unilateral or bilateral SSM, immediate expander/implant reconstruction, and later NAC reconstruction and/or tattooing, and similarly completed the BREAST-Q reconstruction module a minimum of five months following their last reconstructive surgery during the same time interval as the identified NSM patients (March-October 2011).
Surgical technique
NSM was performed by the breast surgeon leaving the dermis and epidermis of the NAC but removing the major ducts, with the goal of leaving a NAC flap of at least 3-5mm in thickness. The ductal tissue was sent as a separate surgical specimen or marked with a suture if it was not separated from the mastectomy specimen for definitive pathologic examination. If the final pathology revealed in situ or invasive carcinoma of the ductal tissue, the NAC was removed in a second procedure. Once the breast was removed, the NAC was assessed clinically for viability by the plastic surgeon. If viable, breast reconstruction was carried out using either tissue expanders or permanent prostheses.
In the comparison group, SSM was performed by the breast surgeon, removing the entire breast including the NAC. Reconstruction of the breast mound was then performed by the plastic surgeon using tissue expanders or permanent prostheses. NAC reconstruction was carried out in a subsequent procedure using either the modified skate (20) or C-V flap technique following successful reconstruction of the breast mound. A small number of patients elected to have NAC tattooing only.
Patient-reported outcomes
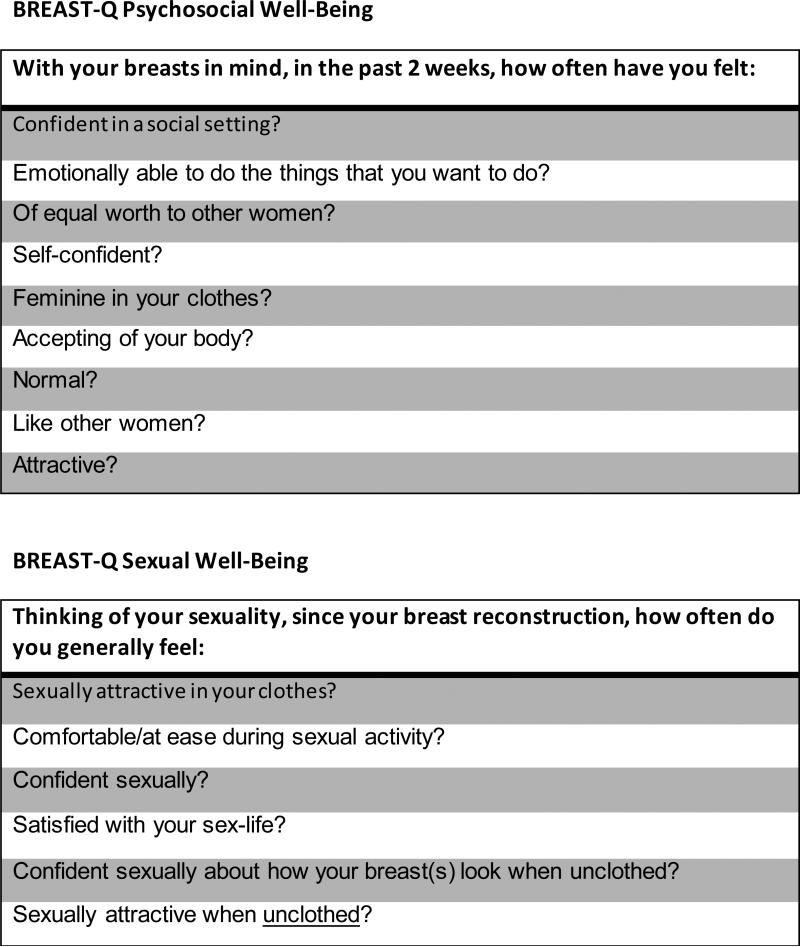
Patients were asked to complete the BREAST-Q postoperatively at a minimum of five months after their final reconstructive surgery. All questionnaires were completed electronically via email. The BREAST-Q is a validated PRO instrument designed to measure HRQOL and patient satisfaction regarding breast reconstruction (18,19). The questionnaire evaluates three HRQOL domains: physical, psychosocial, and sexual well-being, and three satisfaction domains: satisfaction with breast, overall outcome, and process of care. All BREAST-Q scores are transformed onto a scale from 0 to 100, with higher scores representing better outcome. Questions from the psychosocial and sexual well-being scales are shown in Figure 1.
Figure 1.
BREAST-Q psychosocial and sexual well-being scales.
Data Acquisition and Statistical Analysis
Chart review was performed for NSM and SSM patients eligible for study inclusion. Demographic and clinical characteristics captured included age at mastectomy, BMI, time from final surgery to completion of BREAST-Q, marital status, ethnicity, original cup size, smoking status, medical comorbidities, cancer stage, receipt of adjuvant chemotherapy or radiation, implant type, type (therapeutic or prophylactic) and laterality of mastectomy, receipt of contralateral symmetry procedure or NAC reconstruction, and presence of one or more significant surgical complications. Significant surgical complications were considered infection requiring intravenous antibiotics, hematoma or seroma requiring drainage, full-thickness mastectomy flap necrosis, and partial or total nipple loss.
Continuous variables (age at mastectomy, BMI, time from final surgery to BREAST-Q completion) were analyzed for normality, and comparisons between NSM and SSM patients for continuous variables were made using Student's t-test. Pearson's chi-square was used for categorical variables: ethnicity (white, non-white/Hispanic), original cup size (AA-C, D-EEE), smoking status (present/past smoker, non-smoker), presence of comorbidities (hypertension/type 2 diabetes, no comorbidities), implant type (saline, silicone), mastectomy type (therapeutic [unilateral or bilateral disease], bilateral prophylactic), presence of surgical complications (none or ≥1). Fischer's exact test was used for dichotomous variables: marital status (married/living with a partner, single/divorced/separated/widowed), cancer stage (stage 0/I/II, stage III/IV), radiation therapy (yes, no), chemotherapy (yes, no), receipt of contralateral symmetry procedure or NAC reconstruction (yes, no).
BREAST-Q satisfaction and HRQOL domains were compared between the NSM and SSM groups using Student's t-test. Domains in which there was a significant difference between the two groups were identified for further analysis as dependent variables. Univariate linear regression analysis was used to identify demographic and clinical variables that were associated with each dependent variable. Multivariate linear regression models were then constructed to identify independent predictors of HRQOL. The independent variables were incorporated into a multivariate linear regression model to control for differences between the two groups. Only significant variables identified in the univariate analysis and clinical factors known to impact post-mastectomy sexual and psychosocial well-being were included in the model. Statistical analyses were performed using SPSS v22.0 (IBM, Armonk, NY). All p-values were two-tailed, and values of p ≤ 0.05 were considered statistically significant.
RESULTS
Comparison of NSM and SSM Patients
A total of 254 patients eligible for the study were identified from the institutional databases: 52 NSM patients and 202 SSM patients. Mean age of the NSM and SSM patients was 44.9 ± 9.4 years and 45.7 ± 7.9 years, respectively. Demographic and clinical characteristics of the two groups are shown in Table 1. Compared to women undergoing SSM, women who had NSM had a significantly lower BMI, smaller original cup size, and were more likely to complete the BREAST-Q questionnaire sooner after their final reconstructive surgery. The incidence of bilateral prophylactic mastectomy also differed significantly between the two groups.
Table 1.
Demographic and clinical characteristics of NSM and SSM patients
| Variable | NSM n =52 | SSM n = 202 | p-value |
|---|---|---|---|
| Mean Age in years (±SD) (range) | 44.9 (±9.4) (23-64) | 45.7 (±7.9) (23-72) | 0.526 |
| Mean BMI (±SD) (range) | 22.9 (±3.8) (17-35) | 25.0 (±4.7) (16-40) | 0.003 |
| Time from reconstruction to Breast-Q completion in months | 18.3 (±17) (5-83) | 32.9 (±21) (5-84) | <0.001* |
| Marital status | 0.588 | ||
| Married/living with partner | 41 (78.8%) | 152 (75.2%) | |
| Single/divorced/widowed | 11 (21.2%) | 50 (24.8%) | |
| Ethnicity | 0.264 | ||
| White | 50 (96.2%) | 182 (90.5%) | |
| Non-white/Hispanic | 2 (3.8%) | 19 (9.5%) | |
| Original Cup Size | 0.007* | ||
| AA-C | 49 (94.2%) | 157 (77.7%) | |
| D-EEE | 3 (5.8%) | 45 (22.3%) | |
| History of smoking | 16 (30.8%) | 61 (30.2%) | 0.936 |
| Comorbidities (HTN, DM) | 4 (7.7%) | 16 (7.9%) | 0.956 |
| Breast Cancer Stage | 0.594 | ||
| Early Stage (0, I, II) | 40 (100%) | 182 (96.8%) | |
| Late Stage (III, IV) | 0 | 6 (3.2%) | |
| Radiation Therapy | 6 (11.8%) | 15 (7.4%) | 0.391 |
| Adjuvant Chemotherapy | 16 (30.8%) | 77 (38.1%) | 0.327 |
| Implant Type | 0.419 | ||
| Saline | 6 (11.8%) | 33 (16.3%) | |
| Silicone | 45 (88.2%) | 169 ( 83.7%) | |
| Unknown | 1 (1.9%) | ||
| Laterality | |||
| Unilateral | 15(29%) | 70 (35%) | 0.431 |
| Bilateral | 37(71%) | 132 (65%) | |
| Mastectomy Type | <0.001* | ||
| Therapeutic (U/L or B/L disease) | 40 (76.9%) | 194 ( 96.0%) | |
| B/L prophylactic | 12 (23.1%) | 8 (4.0%) | |
| Contralateral Symmetry Procedure | 9 (17.3%) | 53 (26.2%) | 0.204 |
| NAC reconstruction | - | 195 (96.5%)** | |
| Surgical Complication | 0.207 | ||
| None | 43 (82.7%) | 180 (89.1%) | |
| ≥1 complication | 9 (17.3%) | 22 (10.9%) | |
NSM, nipple-sparing mastectomy; SSM, skin-sparing mastectomy; SD, standard deviation; BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; U/L, unilateral; B/L, bilateral
statistically significant p-value
7 patients underwent nipple-areolar tattooing only, without flap reconstruction
Surgical complications following the mastectomy and reconstructive procedures included infection requiring intravenous antibiotics, hematoma or seroma requiring drainage, full-thickness mastectomy flap necrosis, and partial or total NAC loss (Table 2). No significant difference in the incidence of surgical complications was found between the two groups. The most common complication among both the NSM and SSM patients was full-thickness mastectomy flap necrosis. In all cases, mastectomy flap necrosis was successfully managed with local wound care and healing by secondary intention was achieved.
Table 2.
Complications following NSM or SSM and immediate expander-implant reconstruction
| NSM n = 52 | SSM n = 202 | p-value | |
|---|---|---|---|
| None | 43 (82.7%) | 180 (89.1%) | 0.062 |
| Seroma requiring drainage | 0 | 4 (2.0%) | |
| Hematoma requiring return to OR | 1 (1.9%) | 4 (2.0%) | |
| Infection requiring antibiotics | 1 (1.9%) | 2 (1.0%) | |
| Full thickness mastectomy flap necrosis | 4 (7.7%) | 12 (5.9%) | |
| Partial NAC loss | 2 (3.8%) | 0 | |
| Total NAC loss | 0 | 0 |
NSM, nipple-sparing mastectomy; SSM, skin-sparing mastectomy
BREAST-Q Results
BREAST-Q scale scores were compared for NSM and SSM patients (Table 3). Women who underwent NSM were found to have a significantly higher mean score on both the psychosocial and sexual well-being scale than women who had SSM. No significant differences were found in the physical well-being, satisfaction with breast, or satisfaction with overall outcome domains between the two groups.
Table 3.
Comparison of BREAST-Q© score by scale: NSM vs SSM patients
| BREAST-Q scale | NSM Mean score (±SD) (range) | SSM Mean score (±SD) (range) | Mean score differencea | p-value |
|---|---|---|---|---|
| Psychosocial well-being | 83.2 (±20.8) (26-100) | 75.5 (±18.8) (28-100) | 7.7 | 0.01* |
| Sexual well-being | 65.5 (±23.6) (0-100) | 57.4 (±21.1) (0-100) | 8.1 | 0.02* |
| Physical well-being | 80.0 (±14.2) (50-100) | 77.2 (±14.1) (31-100) | 2.8 | 0.23 |
| Satisfaction with breast | 66.2 (±18.5) (11-100) | 65.6 (±18.8) (0-100) | 0.6 | 0.85 |
| Satisfaction with outcome | 76.6 (±20.5) (27-100) | 76.4 (±19.4) (21-100) | 0.935 | 0.94 |
NSM, nipple-sparing mastectomy; SSM, skin-sparing mastectomy; SD, standard deviation
statistically significant p-value
unadjusted scores
In the multivariate regression analysis, NSM was found to be a significant predictor of higher psychosocial as well as sexual well-being after adjusting for BMI, original cup size, time between surgery and BREAST-Q completion, adjuvant radiotherapy, and prophylactic mastectomy (Table 4). No other variables were found to predict higher or lower psychosocial or sexual well-being in the analysis.
Table 4.
Multivariate analysis for predictors of psychosocial and sexual well-being.
| Psychosocial well-being | Sexual well-being | |||||
|---|---|---|---|---|---|---|
| Variable | β | 95% CI | p-value | β | 95% CI | p-value |
| NSM | 6.8 | 0.12, 13.46 | 0.05* | 7.5 | 0.04, 14.89 | 0.05* |
| Months from reconstruction to Breast-Q completion | −0.04 | −0.16, 0.08 | 0.51 | −0.12 | −0.26, 0.01 | 0.07 |
| Original cup size (D-EEE) | −2.23 | −9.06, 4.60 | 0.52 | 1.34 | −6.64, 8.57 | 0.80 |
| Radiation therapy | 8.26 | −0.58, 17.12 | 0.07 | 8.23 | −1.23, 18.50 | 0.09 |
| BMI | −0.52 | −1.11, 0.06 | 0.08 | −0.30 | −0.95, 0.36 | 0.38 |
| B/L prophylactic mastectomy | 2.16 | −7.19, 11.51 | 0.65 | 8.23 | −2.18, 18.63 | 0.12 |
NSM, nipple-sparing mastectomy; BMI, body mass index; β, beta coefficient; SE, standard error; B/L, bilateral
statistically significant p-value
Dependent variable: Psychosocial well-being, adjusted R2 =0.027, observed power (corrected model)=0.95
Dependent variable: Sexual well-being, adjusted R2 =0.040, observed power (corrected model)=0.95
DISCUSSION
The demand for NSM among patients seeking therapeutic or prophylactic treatment for breast cancer has increased dramatically over the last ten years. NSM has become accepted as an oncologically safe option for carefully selected patients; however, there remains a need for data regarding HRQOL outcomes following the procedure to help guide preoperative counseling and decision-making. This study uses a validated, patient-reported outcome metric to compare HRQOL among women undergoing NSM or SSM with NAC reconstruction. Our results show that women who have their nipples preserved report significantly higher psychosocial and sexual well-being compared to women who have NAC reconstruction. However, physical well-being, satisfaction with the reconstructed breast, and satisfaction with overall outcome are similar among women who have NSM or SSM.
Very few reports in the literature address the psychological impact of the nipple on breast reconstruction outcomes. Wellisch et al first examined the effect of adding a nipple to the breast mound in 1987 (2). They found that patients who underwent NAC reconstruction reported higher satisfaction not only with the nude appearance of the reconstructed breast, but also with its size, softness, and sexual sensitivity. The finding that patients had greater satisfaction with factors not obviously affected by the addition of a nipple suggested that the nipple adds a dimension to the breast reconstruction beyond just the physical. Didier et al in 2009 investigated the effect of nipple preservation on patient satisfaction and found that NSM had a positive impact with regard to nipple appearance and sensitivity, body image, and feelings of mutilation (16). They did not find that NSM had a significant effect on sexuality compared to control patients undergoing NAC reconstruction.
Our findings complement the conclusions in these studies. The higher psychosocial well-being score in NSM patients suggests that preserving the nipple may help patients maintain a greater sense of normalcy and self-confidence compared to patients undergoing NAC reconstruction. Furthermore, NSM patients feel more sexually attractive and fulfilled than patients who have NAC reconstruction, as indicated by their higher sexual well-being score. Interestingly, we found no difference between the NSM and SSM groups in the satisfaction with breast domain, which addresses physical qualities of the reconstruction such as softness of the reconstructed breast and symmetry with the contralateral side. This further supports the idea that preservation of the nipple contributes elements to the breast reconstruction that extend beyond the physical appraisal of the breast.
The findings in this study are useful because they suggest that NSM may confer a significant, little-recognized psychological benefit over SSM followed by breast and NAC reconstruction. Satisfaction with aesthetic outcomes of NSM have generally been reported as high in the literature (16, 21-24), and compare favorably with total mastectomy and nipple reconstruction (16). Nipple sensitivity, however, is almost universally rated fair to poor (22-25), and the utility of sparing a nipple that will ultimately be insensate has been questioned (14). Studies have nonetheless demonstrated that overall patient satisfaction following NSM is high (21, 23-25) and that the majority of patients would elect to have NSM again, presumably because of the aesthetic outcomes (24). The results of this study suggest that NSM can provide HRQOL advantages from both a psychosocial and sexual standpoint despite poor return of nipple sensation.
We acknowledge several limitations of this study, one being the relatively small number of NSM patients included in the study. Although the study was adequately powered to reach significance at a p value of 0.05, the inclusion of a greater number of patients would strengthen this analysis and future studies with greater power will be required to confirm our findings. Another limitation is selection bias, as patients were not randomized to have NSM or SSM. Not all patients are good candidates for NSM, and thus patients were offered NSM or SSM based on a combination of factors including tumor characteristics, breast size, degree of nipple ptosis, and patient preference. Although we attempted to control for potential confounding factors using multivariate regression analysis, we recognize the potential for selection bias in non-randomized groups of study subjects. A significantly higher percentage of patients in the NSM group underwent bilateral prophylactic mastectomy compared to the SSM group. Bilateral prophylactic mastectomy and reconstruction is generally associated with high patient satisfaction (26-28), however some studies have found negative effects on body image and sexuality in substantial numbers of patients (29-31). Our results did not show bilateral prophylactic mastectomy to impact psychosocial or sexual well-being (Table 4). Similarly, a study on contralateral prophylactic mastectomy and satisfaction as measured by the BREAST-Q found that contralateral prophylactic mastectomy is associated with higher satisfaction with breasts, but does not affect other domains including psychosocial or sexual well-being (32).
Additional limitations of this study include the lack of preoperative BREAST-Q score comparisons between the NSM and SSM groups, representing another variable in which the two groups may have differed. The lack of matching between NSM and SSM patients with respect to the time elapsed from final surgery to BREAST-Q completion represents another potential source of bias. Implant reconstructions change with time, with increased rates of capsular contracture and asymmetry with the contralateral natural breast as time progresses. The group with longer follow-up is thus more likely to be affected by these potential complications and sources of dissatisfaction. The SSM group in our study had a significantly greater mean follow-up time than the NSM group, however there was no significant difference in satisfaction with breasts or overall outcome between the two groups, suggesting that the differences observed in psychosocial and sexual well-being are real. Finally, as the BREAST-Q is designed to assess outcomes only from the patient's perspective, we did not include any objective assessment of aesthetic or sensory outcomes in this study. Future studies investigating the correlation between clinician-rated and patient-reported outcomes will offer further insights that may be useful in the preoperative counseling of patients considering NSM.
CONCLUSION
The surgical management of breast cancer has undergone tremendous change over the past 40 years and has come to focus increasingly on enhancing cosmesis and HRQOL. As the population of breast cancer patients seeking NSM grows, an improved understanding of the surgical, aesthetic, and quality of life outcomes becomes paramount. This study suggests that NSM positively impacts patient psychosocial and sexual well-being following breast reconstruction compared to conventional mastectomy and nipple reconstruction techniques. The growing body of literature on outcomes following NSM should be an integral part of shared medical decision-making between patients and providers, and is essential to provide patients with accurate quality of life expectations following surgery.
Acknowledgments
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnotes
Disclosures: Andrea L. Pusic, M.D., M.H.S. and Anne F. Klassen, D.Phil. are co-developers of the BREAST-Q and receive a share of licensing revenues when the instrument is used in industry-sponsored clinical trials. The BREAST-Q is jointly owned by the Memorial Sloan Kettering Cancer Center and the University of British Columbia, and is provided free of charge for academic research and clinical care.
REFERENCES
- 1.Little JW. Nipple-areola reconstruction. Clin Plast Surg. 1984;11:351. [PubMed] [Google Scholar]
- 2.Wellisch DK, Schain WS, Noone RB. The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg. 1987;80:699–704. doi: 10.1097/00006534-198711000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Jabor MA, Shayani P, Collins DR, Karas T, Cohen BE. Nipple-areola reconstruction: satisfaction and clinical determinants. Plast Reconstr Surg. 2002;110:457–463. doi: 10.1097/00006534-200208000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Goh SC, Martin NA, Pandya AN, Cutress RI. Patient satisfaction following nipple-areolar complex reconstruction and tattooing. J Plast Reconstr Aesthet Surg. 2011;64:360–363. doi: 10.1016/j.bjps.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Harcourt D, Russell C, Hughes J, White P, Nduka C, Smith R. Patient satisfaction in relation to nipple reconstruction: the importance of information provision. J Plast Reconstr Aesthet Surg. 2011;64:494–499. doi: 10.1016/j.bjps.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Momoh AO, Colakoglu S, de Blacam C, Yueh JH, Lin SJ, Tobias AM, Lee BT. The impact of nipple reconstruction on patient satisfaction in breast reconstruction. Ann Plast Surg. 2012;69:389–393. doi: 10.1097/SAP.0b013e318246e572. [DOI] [PubMed] [Google Scholar]
- 7.Coopey SB, Tang R, Lei L, et al. Increasing eligibility for nipple-sparing mastectomy. Ann Surg Oncol. 2013;20:3218–3222. doi: 10.1245/s10434-013-3152-x. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal S, Agarwal S, Neumayer L, Agarwal JP. Therapeutic nipple-sparing mastectomy: trends based on a national cancer database. Am J Surg. 2014;208:93–98. doi: 10.1016/j.amjsurg.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 9.Chung AP, Sacchini V. Nipple-sparing mastectomy: where are we now? Surg Oncol. 2008;17:261–266. doi: 10.1016/j.suronc.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Etienne CA, Cody HS, Disa JJ, Cordeiro P, Sacchini V. Nipple-sparing mastectomy: initial experience at the Memorial Sloan-Kettering Cancer Center and a comprehensive review of the literature. Breast J. 2009;15:440–449. doi: 10.1111/j.1524-4741.2009.00758.x. [DOI] [PubMed] [Google Scholar]
- 11.Rusby JE, Smith BL, Gui GPH. Nipple-sparing mastectomy. Br J Surg. 2010;97:305–316. doi: 10.1002/bjs.6970. [DOI] [PubMed] [Google Scholar]
- 12.Endara M, Chen D, Verma K, Nahabedian MY, Spear SL. Breast reconstruction following nipple-sparing mastectomy: a systematic review of the literature with pooled analysis. Plast Reconstr Surg. 2013;132:1043–1054. doi: 10.1097/PRS.0b013e3182a48b8a. [DOI] [PubMed] [Google Scholar]
- 13.Mallon P, Feron JG, Couturaud B, et al. The role of nipple-sparing mastectomy in breast cancer: a comprehensive review of the literature. Plast Reconstr Surg. 2013;131:969–984. doi: 10.1097/PRS.0b013e3182865a3c. [DOI] [PubMed] [Google Scholar]
- 14.Opatt D, Morrow M. The dual role of nipple preservation. J Support Oncol. 2006;4:233–234. [PubMed] [Google Scholar]
- 15.Murthy V, Chamberlain R. Defining a place for nipple-sparing mastectomy in modern breast care: an evidence-based review. Breast J. 2013;19:571–581. doi: 10.1111/j.1524-4741.2011.01220.x. [DOI] [PubMed] [Google Scholar]
- 16.Didier F, Radice D, Gandini S, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat. 2009;118:623–633. doi: 10.1007/s10549-008-0238-4. [DOI] [PubMed] [Google Scholar]
- 17.Peled AW, Duralde E, Foster RD, Fiscalini AS, Esserman LJ, Hwang ES, Sbitany H. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg. 2014;72(Suppl 1):S48–52. doi: 10.1097/SAP.0000000000000020. [DOI] [PubMed] [Google Scholar]
- 18.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 19.Cano SJ, Klassen AF, Scott AM, Cordeiro PG, Pusic AL. The Breast-Q: further validation in independent clinical samples. Plast Reconstr Surg. 2012;129:293–302. doi: 10.1097/PRS.0b013e31823aec6b. [DOI] [PubMed] [Google Scholar]
- 20.Zhong T, Antony A, Cordeiro P. Surgical outcomes and nipple projection using the modified skate flap for nipple-areolar reconstruction in a series of 422 implant reconstructions. Ann Plast Surg. 2009;62:591–595. doi: 10.1097/SAP.0b013e31819fb1c9. [DOI] [PubMed] [Google Scholar]
- 21.Mosahebi A, Ramakrishnan V, Gittos M, Collier DS. Envelope mastectomy and immediate reconstruction (EMIR), improving outcome without oncological compromise. J Plast Reconstr Aesthet Surg. 2006;59:1025–1030. doi: 10.1016/j.bjps.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 22.Petit JY, Veronesi U, Orecchia R, et al. Nipple sparing mastectomy with nipple areola intraoperative radiotherapy: one thousand and one cases of a five year experience at the European institute of oncology of Milan (EIO). Breast Cancer Res Treat. 2009;117:333–338. doi: 10.1007/s10549-008-0304-y. [DOI] [PubMed] [Google Scholar]
- 23.Yueh JH, Houlihan MJ, Slavin SA, Lee BT, Pories SE, Morris DJ. Nipple-sparing mastectomy: evaluation of patient satisfaction, aesthetic results, and sensation. Ann Plast Surg. 2009;62:586–590. doi: 10.1097/SAP.0b013e31819fb1ac. [DOI] [PubMed] [Google Scholar]
- 24.Djohan R, Gage E, Gatherwright J, Pavri S, Firouz J, Bernard S, Yetman R. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg. 2010;125:818–829. doi: 10.1097/PRS.0b013e3181ccdaa4. [DOI] [PubMed] [Google Scholar]
- 25.Nahabedian MY, Tsangaris TN. Breast reconstruction following subcutaneous mastectomy for cancer: a critical appraisal of the nipple-areola complex. Plast Reconstr Surg. 2006;117:1083–1090. doi: 10.1097/01.prs.0000202103.78284.97. [DOI] [PubMed] [Google Scholar]
- 26.Metcalfe KA, Semple JL, Narod SA. Satisfaction with breast reconstruction in women with bilateral prophylactic mastectomy: a descriptive study. Plast Reconstr Surg. 2004;114:360–366. doi: 10.1097/01.prs.0000131877.52740.0e. [DOI] [PubMed] [Google Scholar]
- 27.Spear SL, Schwarz KA, Venturi ML, Barbosa T, Al-Attar A. Prophylactic mastectomy and reconstruction: clinical outcomes and patient satisfaction. Plast Reconstr Surg. 2008;122:1–9. doi: 10.1097/PRS.0b013e318177415e. [DOI] [PubMed] [Google Scholar]
- 28.Gahm J, Jurell G, Edsander-Nord A, Wickman M. Patient satisfaction with aesthetic outcome after bilateral prophylactic mastectomy and immediate reconstruction with implants. J Plat Reconstr Aesthet Surg. 2010;63:332–338. doi: 10.1016/j.bjps.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 29.Brandberg Y, Sandelin K, Erikson S, et al. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol. 2008;26:3943–3949. doi: 10.1200/JCO.2007.13.9568. [DOI] [PubMed] [Google Scholar]
- 30.den Heijer M, Seynaeve C, Timman R, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer. 2012;48:1263–1268. doi: 10.1016/j.ejca.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Gopie JP, Mureau MA, Seynaeve C, et al. Body image issues after bilateral prophylactic mastectomy with breast reconstruction in healthy women at risk for hereditary breast cancer. Fam Cancer. 2013;12:479–87. doi: 10.1007/s10689-012-9588-5. [DOI] [PubMed] [Google Scholar]
- 32.Koslow S, Pharmer LA, Scott AM, et al. Long-term patient-reported satisfaction after contralateral prophylactic mastectomy and implant reconstruction. Ann Surg Oncol. 2013;20:3422–3429. doi: 10.1245/s10434-013-3026-2. [DOI] [PubMed] [Google Scholar]